Abstract
OBJECTIVE: To determine the sensitivity and specificity of ligase chain reaction (LCR) analysis of cervical and urine specimens from women compared with cell culture of cervical and urethral specimens for the diagnosis of genitourinary chlamydial infection. METHODS: Women (n = 624) attending the Genitourinary Medicine Clinic at University College London Hospitals, were enrolled. Patients who had received antibiotics within the previous two weeks were excluded. Specimens were obtained from the urethra and cervix for chlamydial culture, and from the cervix for LCR. A specimen of first void urine was also obtained for LCR. Discrepancies were resolved by direct immunofluorescence or a major outer membrane protein targeted LCR, or both. RESULTS: The prevalence of Chlamydia trachomatis in 600 patients, using an expanded standard of a positive cell culture or two confirmed positive non-culture tests, was 13.2% (79/600). Cervical culture detected 68.4% and urethral culture 62% of all positive results compared with 81% detected by cervical LCR and 69% by urine LCR. Cervical and urethral culture combined detected 87.3% whereas cervical and urine LCR combined detected 91.1% of positive cases. Specificity of LCR was 100% in the cervix and 99.8% in urine. CONCLUSION: This study demonstrates that LCR analysis of cervical and urine specimens is a reliable method for the diagnosis of chlamydial genital infection in women. However, the study also demonstrates that no single test will detect all chlamydial infections. Conventional non-culture tests and cell culture may grossly underestimate the prevalence of chlamydial infection. LCR analysis of a cervical specimen was superior to conventional cell culture without blind passage as a single test for diagnosing chlamydial infection in women, followed by LCR of a urine specimen.
Full text
PDF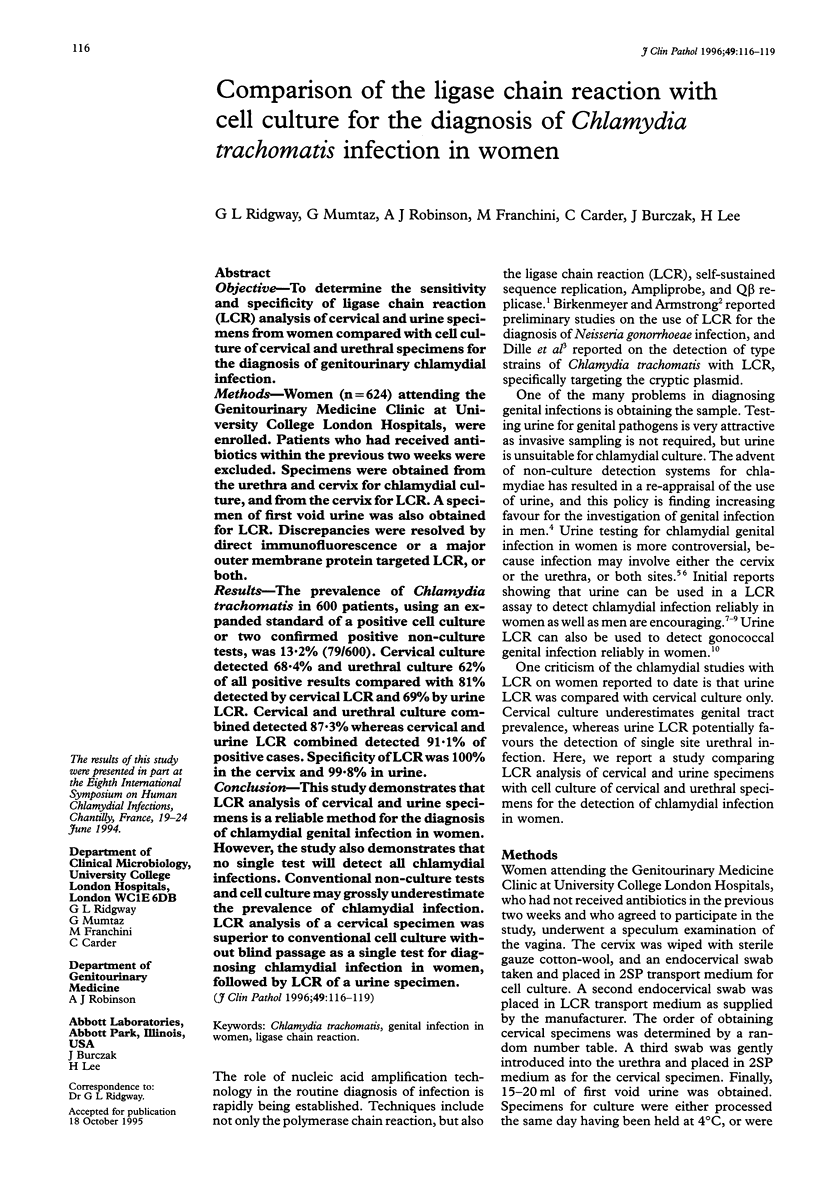


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bassiri M., Hu H. Y., Domeika M. A., Burczak J., Svensson L. O., Lee H. H., Mårdh P. A. Detection of Chlamydia trachomatis in urine specimens from women by ligase chain reaction. J Clin Microbiol. 1995 Apr;33(4):898–900. doi: 10.1128/jcm.33.4.898-900.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birkenmeyer L. G., Mushahwar I. K. DNA probe amplification methods. J Virol Methods. 1991 Nov-Dec;35(2):117–126. doi: 10.1016/0166-0934(91)90127-l. [DOI] [PubMed] [Google Scholar]
- Birkenmeyer L., Armstrong A. S. Preliminary evaluation of the ligase chain reaction for specific detection of Neisseria gonorrhoeae. J Clin Microbiol. 1992 Dec;30(12):3089–3094. doi: 10.1128/jcm.30.12.3089-3094.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chernesky M. A., Jang D., Lee H., Burczak J. D., Hu H., Sellors J., Tomazic-Allen S. J., Mahony J. B. Diagnosis of Chlamydia trachomatis infections in men and women by testing first-void urine by ligase chain reaction. J Clin Microbiol. 1994 Nov;32(11):2682–2685. doi: 10.1128/jcm.32.11.2682-2685.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dille B. J., Butzen C. C., Birkenmeyer L. G. Amplification of Chlamydia trachomatis DNA by ligase chain reaction. J Clin Microbiol. 1993 Mar;31(3):729–731. doi: 10.1128/jcm.31.3.729-731.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay P. E., Thomas B. J., Horner P. J., MacLeod E., Renton A. M., Taylor-Robinson D. Chlamydia trachomatis in women: the more you look, the more you find. Genitourin Med. 1994 Apr;70(2):97–100. doi: 10.1136/sti.70.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R. B., Katz B. P., van der Pol B., Caine V. A., Batteiger B. E., Newhall W. J. Effect of blind passage and multiple sampling on recovery of Chlamydia trachomatis from urogenital specimens. J Clin Microbiol. 1986 Dec;24(6):1029–1033. doi: 10.1128/jcm.24.6.1029-1033.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H. H., Chernesky M. A., Schachter J., Burczak J. D., Andrews W. W., Muldoon S., Leckie G., Stamm W. E. Diagnosis of Chlamydia trachomatis genitourinary infection in women by ligase chain reaction assay of urine. Lancet. 1995 Jan 28;345(8944):213–216. doi: 10.1016/s0140-6736(95)90221-x. [DOI] [PubMed] [Google Scholar]
- Mumtaz G., Clark S., Ridgway G. L., Miller C. J., Johal B., Allason Jones E. Comparison of an enzyme immuno assay (Antigenz Chlamydia) with cell culture for the detection of genital chlamydial infection in high and low risk populations. Genitourin Med. 1993 Apr;69(2):119–122. doi: 10.1136/sti.69.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridgway G. L., Taylor-Robinson D. Current problems in microbiology: 1. Chlamydial infections: which laboratory test? J Clin Pathol. 1991 Jan;44(1):1–5. doi: 10.1136/jcp.44.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schachter J., Stamm W. E., Chernesky M. A., Hook E. W., 3rd, Jones R. B., Judson F. N., Kellogg J. A., LeBar B., Mårdh P. A., McCormack W. M. Nonculture tests for genital tract chlamydial infection. What does the package insert mean, and will it mean the same thing tomorrow? Sex Transm Dis. 1992 Sep-Oct;19(5):243–244. [PubMed] [Google Scholar]
- Smith K. R., Ching S., Lee H., Ohhashi Y., Hu H. Y., Fisher H. C., 3rd, Hook E. W., 3rd Evaluation of ligase chain reaction for use with urine for identification of Neisseria gonorrhoeae in females attending a sexually transmitted disease clinic. J Clin Microbiol. 1995 Feb;33(2):455–457. doi: 10.1128/jcm.33.2.455-457.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]



