Abstract
Background
The literature suggests an association of pancreatic enzymes with systemic inflammation resulting in secondary organ injury and dysfunction following trauma. Elevation in serum enzymes may not always be predictive of pancreatic disease, and can reflect extra pancreatic production.
Objectives
This study was conducted to evaluate the rise in serum pancreatic enzyme levels with the incidence of organ failure following trauma.
Patients and Methods
A retrospective review was performed on critically injured patients from December 2009 to March 2010. Patient’s clinical demographics, routine laboratory investigations along with amylase and lipase levels were also extracted from the patients' records. Patients with pancreatic or duodenal injuries were excluded from the study.
Results
From a total of 296 patients (mean age, 31 years), 85% were males. Blunt injury was seen in 91.6% of the cases and 8.4% had penetrating injury. One hundred and fifty-three patients had single organ failure, 96 had multiple organ failure and 47 had no organ failure. There was a significant difference in lipase levels (P = 0.04), potassium levels (P = 0.05) and hemoglobin levels (P = -0.004), among the three patient groups. There was no significant difference in amylase levels among the three patient groups. The observed independent predictors of mortality included coagulopathy (OR = 1.7), Glasgow coma scale (OR = 1.1, 4.7), pulmonary failure (OR = 0.0004), hepatic failure (OR = 0.048), renal failure (OR = 5.5), organ failure (OR =149.8), lipase levels (OR = 1.3), and infection (OR = 3.0).
Conclusions
There was a significant correlation between elevated lipase levels and the incidence of multiple organ failure. Moreover, No significant association was found between the elevated amylase levels and organ failure. However, on admission, measurement of these enzymes coupled with routine laboratory investigations can be a powerful tool in the early detection of patients progressing towards organ failure.
Keywords: Amylase, Lipase, Organ Failure, Trauma
1. Background
Multiple organ failure (MOF) is the leading cause of posttrauma morbidity and mortality. It is thought to be caused by the systemic inflammatory response syndrome (SIRS) that follows severe trauma and hemorrhagic shock. Multiple organ failure has been defined as progressive dysfunction of two or more organ systems following an acute threat to systemic homeostasis (1, 2). Review of earlier studies depicts an incidence of 5% to 25%. Several organ dysfunction scoring systems have been developed to describe and quantify organ dysfunction/ failure in ICU patients (3-5). There is no gold standard for quantification of the degree of organ damage; however, several scores like multiple organ dysfunctions (MOD) score, and Denver postinjury MOF scores (6) are being utilized.
Available literature suggests that intraluminal pancreatic enzymes stimulate the production of inflammatory mediators by the gut causing uncontrolled systemic inflammation leading to secondary organ injury and dysfunction (7-11).
Increased serum enzyme levels in pancreatic inflammation are not always predictive of pancreatic disease and they may also reflect non-pancreatic or extra-pancreatic production (12-16). This effect is uncertain to predict, whether their direct secretion into the circulation from the pancreas is a part of normal physiology, ischemic pancreatitis, or absorption into the bloodstream through an ischemic intestinal mucosal barrier (17). Detailed information about the prognosis of trauma patients is crucial to improve survival in the intensive care unit (ICU).
2. Objectives
The purpose of this study was to evaluate the prognostic significance of the elevation in serum pancreatic enzyme levels on admission in trauma patients with MOF. We hypothesized that serum amylase and lipase can serve as predictors for the development of MOF in traumatic injury patients.
3. Patients and Methods
A retrospective review was performed on 296 trauma patients presented to the red area of a level-1 trauma center, from December 2009 to March 2010. Data of all the critically injured patients presented during the period of the study, including their demographics, clinical and transfusion data such as age, sex, Glasgow coma score, injury severity score, SOFA score, indication for blood product transfusion, injuries, sepsis, organ failure, coagulopathy and mortality was collected from the computerized patient record system maintained by the institute, or from the individual patient file.
Laboratory investigations namely, complete hemogram (Hb, TLC, and DLC) and coagulation profile (PT, aPTT) were routinely performed on the Sysmex XE-2100 hematology analyzer and STA compact coagulation analyzer, respectively. Biochemistry analysis (liver function test, renal function test, electrolytes) along with amylase and lipase was also routinely performed on the Synchron Cx9 Pro Biochemistry analyzer. Patients with pancreatic or duodenal injuries were excluded from the study group, to ensure that the elevations are due to other intra-abdominal injuries.
The presence of coagulopathy was diagnosed if any of the prothrombin time (PT) or activated partial prothrombin time (aPTT) was > 1.5 times normal and the INR value was > 1.6. Immediate outcome was assessed in terms of hospital length of stay and mortality during the course of the study.
Serum amylase and lipase levels of all traumatic injury patients, who required admission at the trauma care center were assessed and recorded in the emergency department. Trauma scores such as injury severity score (ISS) and Glasgow coma score (GCS) were calculated to assess the severity of injury for the study patients. Elevation in the amylase and lipase levels in the admission day were defined as being > 2 times the upper limit of normal. Normal range for amylase in our laboratory is 30 u/L to 100 u/L, and a value > 200 u/L was considered elevated. The normal range for lipase is 13 u/L to 60 u/L and a value > 120 u/L was considered elevated. The sequential organ failure assessment (SOFA) score was calculated, that quantifies and describes the evolution of organ dysfunction/failure over time, and has been validated in trauma patients. The SOFA score assesses the function of six different organ systems: respiratory [PaO2/FiO2 ratio], cardiovascular (blood pressure, vasoactive drugs), renal (creatinine), hepatic (bilirubin), neurological (Glasgow coma score) and hematological (platelet count) (18).
Multiple organ failure is defined as the occurrence of severe organ failure in two or more organ systems during the ICU stay, either on the same day or on different days.
Statistical analysis was performed using a chi-square test, and two-way ANOVA tests with STATA 11.0 statistical software (USA). Analytical study was done on three different groups of patients namely MOF, single organ failure and no organ failure. The correlation between serum pancreatic enzyme levels and the progression of organ failure was analyzed by comparing the incidence of any one of the following organ system failures in the elevated and non-elevated enzyme groups: cardiac (a requirement for vasopressors, despite adequate volume resuscitation, to maintain adequate organ perfusion), pulmonary (pao2: fio2 <, central venous pressure > 18 mmHg, and bilateral infiltrates on chest radiograph), hepatic (serum total bilirubin > 3 mg/dL and aspartate aminotransferase > 80 IU/L [two times the upper limit of normal]), or renal (serum creatinine > 2 and creatinine clearance < 100 mg/dL), central nervous system (GCS < 8) and hematologic dysfunction (presence of coagulopathy) in the body (19). In this study P < 0.05 has been considered statistically significant.
4. Results
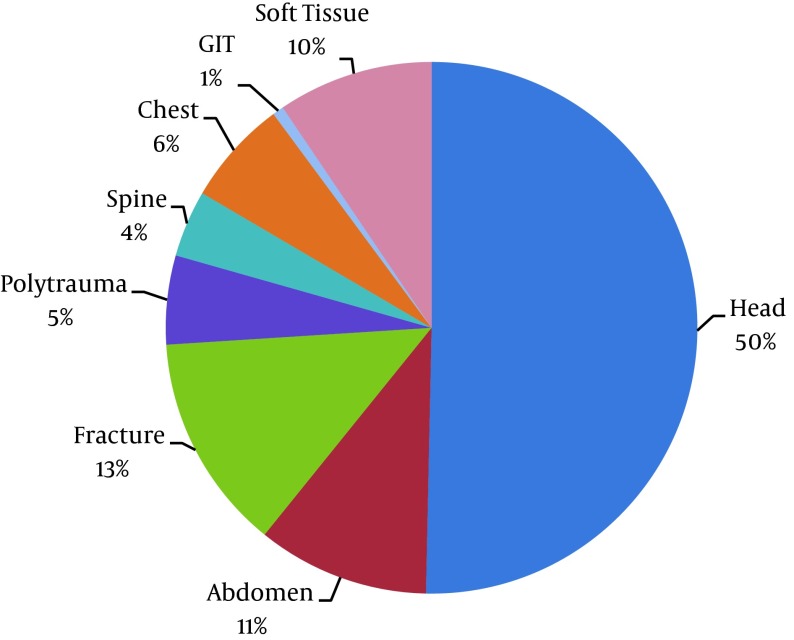
A total of 296 trauma patients from the ICU were enrolled in the study, with the mean age of 31 years, 85% were males and 15% females. Blunt injury was seen in 270 cases (91.6%) and 45 (8.4%) had penetrating injury. (Figure 1) depicts the site of injury. From a total of 296 patients, 153 cases (51.6%) had single organ failure, 96 (32.4%) had MOF and 47 (15.8%) had no organ failure. Of the patients with single organ failure, 1.9% had cardiac failure, 89.5% had pulmonary failure, 7.8% had hepatic failure and 0.6% had renal failure.
Figure 1. Site of Injury.
Univariate analysis of all the laboratory parameters amongst the three patient groups showed varied and significant difference in the lipase level (P = 0.04), prothrombin time (P < 0.001), PaO2 (P < 0.001), PCo2 (P = 0.04), potassium levels (P = 0.05), bilirubin level (P = 0.008) and hemoglobin level (P = 0.004) (Table 1). However, the amylase levels were not found to be significant (Table 1).
Table 1. Patients’ Characteristics in Different Groups of Organ Failure.
| Parameters | Patient Group | SOF vs. No Organ Failure, P Value | No Organ Failure vs. MOF, P Value | SOF vs. MOF, P Value | |||
|---|---|---|---|---|---|---|---|
| No Organ Failure, n = 47 | Single Organ Failure, n = 153 | Multiple Organ Failure, n = 96 | P Value | ||||
| Age, y | 29.3 ± 13.7 | 33.8 ± 17.1 | 30.1 ± 16.1 | 0.11 | 0.29 | 1.00 | 0.25 |
| Sex a | 0.26 | - | - | - | |||
| Male | 38 (80.8) | 136 (88.8) | 80 (83.3) | - | - | - | |
| Female | 9 (19.1) | 17 (11.11) | 16 (16.6) | ||||
| Prothrombin time, sec b | 15.6 ± 2.6 | 16.4 ± 3.8 | 18.6 ± 6.5 | < 0.001 | 0.97 | < 0.001 | < 0.001 |
| Activated partial Thrombin time, sec b | 27.5 ± 7.3 | 26.5 ± 6.1 | 31.0 ± 13.6 | < 0.001 | 1.00 | 0.11 | < 0.001 |
| Coagulopathy a | < 0.001 | - | - | - | |||
| No | 45 (95.7) | 142 (92.8) | 74 (77.0) | ||||
| Yes | 2 (4.26) | 1 (7.1) | 22 (22.9) | ||||
| Blunt injury a | 42 (89.3) | 139 (90.8) | 90 (93.7) | 0.61 | - | - | - |
| Penetrating injury a | 5 (10.6) | 4 (9.10) | 6 (6.2) | ||||
| Glasgow coma scale b | 11.8 ± 4.0 | 11.9 ± 4.3 | 11.10±4.9 | 0.37 | 1.00 | 1.00 | 0.52 |
| Heart rate, /min b | 90.9 ± 13.5 | 92.3 ± 17.2 | 97.9 ± 21.6 | 0.03 | 1.00 | 0.09 | 0.06 |
| Injury a severity score | 0.54 | - | - | ||||
| < 24 | 143 (93.6) | 143 (93.5) | 89 (93.7) | ||||
| > 24 | 16 (6.4) | 10 (6.5) | 6 (6.3) | ||||
| Systolic BP, mmHg b | 116.3 ± 12.7 | 120.9 ± 23.2 | 115.6 ± 16.7 | 0.09 | 0.50 | 1.00 | 0.13 |
| PRBC, units b | 1.08 ± 2.1 | 0.9 ± 1.5 | 1.78 ± 2.1 | 0.002 | 1.00 | 0.11 | 0.002 |
| Pao 2 , mmHg b | 251.7 ± 38.9 | 140.2 ± 57.4 | 133.2 ± 65.1 | < 0.001 | < 0.001 | < 0.001 | 1.000 |
| Pco 2 , mmHg b | 34.7 ± 6.08 | 37.0 ± 6.3 | 43.8 ± 44.6 | 0.065 | 1.00 | 0.14 | 0.13 |
| Hco3, mEq/L b | 21.5 ± 4.2 | 22.7 ± 3.4 | 22.5 ± 4.8 | 0.20 | 0.23 | 0.56 | 1.000 |
| pH b | 7.3 ± 0.1 | 7.3 ± 0.1 | 7.2 ± 0.5 | 0.49 | 1.00 | 1.00 | 0.78 |
| Sodium, meq/L b | 138.6 ± 5.7 | 138.8 ± 5.2 | 138.5 ± 4.9 | 0.89 | 1.00 | 1.00 | 1.000 |
| Potassium, meq/L b | 3.8 ± 0.5 | 3.9 ± 0.76 | 4.1 ± 0. 8 | 0.02 | 0.95 | 0.03 | 0.08 |
| SOFA score b | 4.1 ± 1.2 | 5.5 ± 1.4 | 6.2 ± 1.6 | < 0.001 | < 0.001 | < 0.001 | < 0.002 |
| Bilirubin, mg % b | 0.6 ± 0.3 | 0.7 ± 0.4 | 0.9 ± 0.6 | < 0.001 | 1.00 | 0.02 | 0.01 |
| AST, u/L b | 61.5 ± 102.8 | 62.4 ± 71.2 | 212.4 ± 237.4 | < 0.001 | 1.00 | < 0.001 | < 0.001 |
| Creatinine, meq/L b | 0.6 ± 0.2 | 0.7 ± 0.3z | 0.8 ± 0.6 | 0.01 | 0.83 | 0.01 | 0.05 |
| Urea, meq/L b | 26.4 ± 10.3 | 29.8 ± 14.9 | 37.1 ± 37.4 | 0.01 | 1.00 | 0.04 | 0.06 |
| Hemoglobin, gms/dL b | 11.9 ± 2.2 | 11.6 ± 2.2 | 10.6 ± 2.6 | < 0.001 | 1.00 | 0.005 | 0.003 |
| Hematocrit, % b | 35.7 ± 6.2 | 35.0 ± 6.4 | 32.1 ± 7.8 | < 0.001 | 1.00 | 0.01 | 0.004 |
| Total leukocyte count, x/cu mm b | 14376.5 ± 5865.5 | 14950.3 ± 6627.5 | 16301.0 ± 6789.7 | 0.1 | 1.00 | 1.00 | 1.00 |
| Platelet, /cu mm b | 240.4 ± 118.3 | 233 ± 95.5 | 200.6 ± 84.3 | 0.01 | 1.00 | 0.06 | 0.02 |
| Amylase, U/L b | 93 (31-309) | 89 (9-645) | 89.5 (30 - 1759) | 0.08 | 1.00 | 0.3 | 0.10 |
| Lipase U/L b | 31 (17-190) | 31.5 (4-350) | 33.5 (9 - 526) | 0.05 | 1.00 | 0.16 | 0.09 |
| Length of stay, days b | 5.8 ± 7.4 | 8.4 ± 10.0 | 1 0.1 ± 11.2 | 0.63 | 0.38 | 0.05 | 0.63 |
| Infection a | 0.15 | - | - | ||||
| Yes | 40 (85.11) | 122 (79.7) | 69 (71.8) | ||||
| No | 7 (14.89) | 31 (20.2) | 27 (28.1) | ||||
| Outcome a | < 0.001 | - | - | ||||
| Dead | 45 (95.74) | 146 (95.4) | 35 (36.4) | ||||
| Alive | 2 (4.26) | 7 (4.5) | 61 (63.5) | ||||
aValues expressed as f (%) compared between the different organ failure groups using the chi-square test.
bValues expressed as mean ± SD. compared between the different organ failure groups using analysis of variance-one way ANOVA.
The prevalence of coagulopathy was observed to be significantly higher in patients with MOF (22.9%), 7.1% in patients with single organ failure and 4.2% in patients with no organ failure (P < 0.001) (Table 1).
Incidence of organ failure was also found to be significantly correlated with immediate outcome (dead/alive), (P < 0.001). The mortality rate in case of MOF was 36.4%, 4.5% in patients with single organ failure and 4.2% in patients with no organ failure (Table 1).
To determine if differences exist among three patient groups, one-way analysis of variance (ANOVA) was performed using the mean values of all the laboratory parameters (Table 1). A significant difference was observed in the mean values of PaO2 (P < 0.001) and SOFA score (P < 0.001) for the patients who developed single organ failure when compared to the patients with no organ failure. On comparison of the no organ failure patient group with the patients with MOF, mean values were as follows: for PT (P < 0.001), PaO2 (P < 0.001), SOFA score (P <0.001), potassium (P = 0.03), bilirubin (P = 0.02), AST (P < 0.001), creatinine (P = 0.01), urea (P = 0.04), Hb (P = 0.005), Hct (P = 0.01), length of stay (P = 0.05).
The analysis of variance for the single vs. MOF group showed a significant difference in the mean values of PT (P < 0.001), aPTT (P < 0.001), PRBC transfusion (P = 0.002), SOFA score (P = 0.002), bilirubin (P = 0.01), AST (P < 0.001), creatinine (P = 0.05), Hb (P = 0.003), Hct (P = 0.004) and platelets (P = 0.02) (Tables 2 and 3).
Table 2. [Part 1]. Comparison Between Abnormal and Normal Levels of Lipase and Amylase in Trauma Patients.
| Parameters | Lipase | P Value | Amylase | P Value | ||
|---|---|---|---|---|---|---|
| Normal | Abnormal | Normal | Abnormal | |||
| Sex | 0.06 | 0.67 | ||||
| Male | 197 (83.8) | 56 (93.3) | 192 (85.3) | 62 (87.3) | ||
| Female | 38 (16.1) | 4 (06.6) | 33 (14.6) | 9 (12.6) | ||
| Activated partial Thrombin time | 0.6 | 0.08 | ||||
| Normal (≤ 49.2) | 229 (97.4) | 58 (96.6) | 221 (98.2) | 67 (94.3) | ||
| Abnormal (> 49.2) | 6 (02.5) | 2 (03.3) | 4 (1.70) | 4 (05.6) | ||
| Coagulopathy | 0.02 | 0.12 | ||||
| No | 212 (90.2) | 48 (80) | 202 (89.7) | 59 (83.1) | ||
| Yes | 23 (09.7) | 12 (20) | 23 (10.2) | 12 (16.9) | ||
| Mode of injury | 0.12 | 0.62 | ||||
| Blunt injury | 212 (90.2) | 23 (09.7) | 207 (92) | 64 (90.1) | ||
| Penetrating injury | 58 (96.6) | 2 (03.3) | 18 (08) | 7 (09.8) | ||
| Glasgow coma scale | 0.56 | 0.50 | ||||
| Mild (13 - 15) | 144 (61.2) | 38 (63.3) | 140 (62.2) | 43 (60.5) | ||
| Moderate (9 - 12) | 23 (09.7) | 8 (13.3) | 21 (09.3) | 10 (14.0) | ||
| Severe (1 - 8) | 68 (28.9) | 14 (33.3) | 64 (28.4) | 18 (25.3) | ||
| Injury Severity Score | 0.06 | 0.25 | ||||
| < 24 | 225 (80.9) | 10 (58.8) | 214 (76.7) | 11 (64.7) | ||
| > 24 | 53 (19.1) | 7 (41.2) | 65 (23.3) | 6 (35.3) | ||
| Systolic BP, mmHg | 0.06 | 0.94 | ||||
| Normal (≤ 130) | 207 (88.0) | 47 (78.3) | 194 (86.2) | 61 (85.9) | ||
| Abnormal (> 130) | 28 (11.9) | 13 (21.6) | 31 (13.7) | 10 (14.0) | ||
| PaO 2 , mmHg | 0.24 | 0.62 | ||||
| Normal (80 - 100) | 35 (14.8) | 7 (11.6) | 33 (14.6) | 9 (12.6) | ||
| Abnormal low ( < 80) | 31 (13.1) | 13 (21.6) | 31 (13.7) | 13 (18.3) | ||
| Abnormal high ( > 100) | 169 (71.9) | 40 (66.6) | 161 (71.5) | 49 (69.0) | ||
| PCO 2 , mmHg | 0.4 | 0.92 | ||||
| Normal (35 - 45) | 118 (50.2) | 35 (58.3) | 115 (51.1) | 38 (53.5) | ||
| Abnormal low (> 45) | 25 (10.6) | 7 (11.6) | 25 (11.1) | 8 (11.2) | ||
| Abnormal high ( < 35) | 92 (39.1) | 18 (30.0) | 85 (37.7) | 25 (35.2) | ||
| Hco 3 , mEq/L | 0.63 | 0.6 | ||||
| Normal (24 - 29) | 78 (33.3) | 24 (40.0) | 76 (33.7) | 26 (37.1) | ||
| Abnormal high (> 29) | 8 (03.4) | 1 (01.6) | 8 (03.5) | 1 (01.4) | ||
| Abnormal-low (< 24) | 148 (63.2) | 35 (58.3) | 141 (62.6) | 43 (61.4) | ||
| pH | 0.69 | 0.1 | ||||
| Normal (7.35 - 7.45) | 93 (39.5) | 20 (33.9) | 87 (38.6) | 26 (37.1) | ||
| Abnormal low (< 7.35) | 105 (44.6) | 28 (47.4) | 107(47.5) | 27 (38.5) | ||
| Abnormal high (> 7.45) | 37 (15.7) | 11 (18.6) | 31 (13.7) | 17 (24.2) | ||
| Sodium, mEq/L | 0.3 | 0.26 | ||||
| Normal (135 - 145) | 201 (85.9) | 47 (78.3) | 185 (82.5) | 63 (88.7) | ||
| Abnormal high (> 145) | 11 (04.7) | 4 (06.6) | 11 (04.9) | 4 (05.6) | ||
| Abnormal low (< 135) | 22 (09.4) | 9 (15.0) | 28 (12.5) | 4 (05.6) | ||
| Potassium, mEq/L | 0.1 | 0.14 | ||||
| Normal (3.5 - 5) | 181 (77.0) | 39 (65.0) | 170 (75.5) | 57 (71.8) | ||
| Abnormal-high (> 5) | 17 (07.2) | 5 (08.3) | 13 (05.7) | 9 (12.6) | ||
| Abnormal-low (< 3.5) | 37 (15.7) | 16 (26.6) | 42 (18.6) | 11 (16.4) | ||
Table 3. [Part 2]. Comparison Between Abnormal and Normal Levels of Lipase and Amylase in Trauma Patients.
| Parameters | Lipase | P Value | Amylase | P Value | ||
|---|---|---|---|---|---|---|
| Normal | Abnormal | Normal | Abnormal | |||
| Bilirubin, mg % | 0.16 | 0.22 | ||||
| Normal (up to 1) | 188 (80.0) | 43 (71.6) | 180 (80) | 52 (73.2) | ||
| Abnormal (> 1) | 47 (20.0) | 17 (28.3) | 45 (20) | 90 (26.7) | ||
| Cardiac Failure | 0.15 | 0.71 | ||||
| No | 208 (88.5) | 49 (81.6) | 197 (87.5) | 61 (85.9) | ||
| Yes | 27 (11.4) | 11 (18.3) | 28 (12.4) | 10 (14.0) | ||
| Pulmonary failure | 0.6 | 0.34 | ||||
| No | 58 (24.6) | 13 (21.6) | 51 (22.6) | 20 (28.1) | ||
| Yes | 177 (75.3) | 47 (78.3) | 174 (77.3) | 51 (71.8) | ||
| Hepatic failure | 0.3 | 157 (69.7) | 49 (69.0) | 0.90 | ||
| No | 166 (70.6) | 39 (65.0) | 68 (30.2) | 22 (30.9) | ||
| Yes | 69 (29.3) | 21 (35.0) | ||||
| Renal failure | 0.005 | 0.03 | ||||
| No | 233 (99.1) | 55 (91.6) | 222 (98.6) | 67 (94.3) | ||
| Yes | 2 (08.0) | 5 (08.3) | 3 (01.3) | 4 (05.6) | ||
| Hemoglobin, gms/DL | 0.91 | 0.90 | ||||
| Normal ( ≥ 9) | 201 (85.5) | 51 (85.0) | 192 (85.3) | 61 (85.9) | ||
| Abnormal ( < 9) | 34 (14.4) | 9 (15.0) | 33 (14.6) | 10 (14.0) | ||
| Total leukocyte Count, × 10 ³/cumm | 0.6 | 0.68 | ||||
| Normal (4000 - 10000) | 48 (20.4) | 15 (25.0) | 48 (21.3) | 15 (21.1) | ||
| Abnormal high (> 10000) | 185 (78.7) | 45 (75.0) | 176 (78.2) | 55 (71.4) | ||
| Abnormal low (< 4000) | 2 (0.8) | 0 (0.0) | 1 (00.4) | 1 (01.4) | ||
| Platelet(/cu mm) | 0.005 | 0.51 | ||||
| Normal (1 - 4 lakh) | 224 (95.3) | 51 (85.0) | 211 (93.7) | 65 (91.5) | ||
| Abnormal (< 1 lakh) | 11 (04.6) | 9 (15.0) | 14 (06.2) | 6 (08.4) | ||
| Infection a | 0.01 | 0.26 | ||||
| Yes | 191 (81.2) | 40 (66.6) | 179 (79.5) | 52 (73.2) | ||
| No | 44 (18.7) | 20 (33.3) | 46 (20.4) | 19 (26.7) | ||
| Outcome a | 0.04 | 0.34 | ||||
| Dead | 205 (87.2) | 46 (76.6) | 194 (86.2) | 58 (81.6) | ||
| Alive | 30 (12.7) | 14 (23.3) | 31 (13.7) | 13 (18.3) | ||
| Organ Failure | 0.02 | 0.28 | ||||
| No Organ Failure | 38 (16.1) | 9 (15.0) | 33 (14.6) | 14 (19.7) | ||
| Single Organ Failure | 129 (54.8) | 23 (38.3) | 122 (54.2) | 31 (43.6) | ||
| Multiple Organ Failure | 68 (28.9) | 28 (46.6) | 70 (31.1) | 26 (36.6) | ||
aValues expressed as F (%), compared between the normal abnormal levels using χ2 test.
To compare the lipase and amylase levels within the normal range, and above and beyond the normal range in serum samples, the chi-square test was performed in correlation with the different laboratory parameters. Serum lipase levels were observed to be significantly associated with the platelet count (P = 0.005) of acutely injured patients. Lipase levels were also significantly correlated with coagulopathy (P = 0.02), infection (P = 0.01), immediate outcome (dead/alive) (P = 0.04), and organ failure (P = 0.02). Both amylase and lipase levels were found to be significant in patients with renal failure (P = 0.03, and P = 0.005, respectively) (Table 2).
To determine the comparison between patients with and without organ failure, the univariate logistic regression analysis of the categorical data was performed. Variables that were determined to have statistically significant association with the occurrence of organ failure were evaluated using multivariate regression analysis to determine the independent association of the variable with organ failure (Tables 4 and 5). It was concluded that independent predictors of organ failure were PCo2 (OR = 0.5) and potassium (OR = 4.1).
Table 4. [Part 1]. Analysis of Organ Failure (Univariate and Multivariate Analysis)a.
| Parameters | Organ Failure | P Value | Odds Ratio (95% CI) | Adjusted Odds Ratio (95% CI) | |
|---|---|---|---|---|---|
| No | Yes | ||||
| Sex | 0.29 | ||||
| Male | 38 (80.8) | 216 (86.7) | 1.0 | - | |
| Female | 9 (19.1) | 33 (13.2) | 0.6 (0.2-1.4) | ||
| Activated partial Thrombin time | 0.48 | 1.0 | - | ||
| Normal (≤ 49.2) | 45 (95.7) | 243 (75.0) | 0.5 (0.1-2.8) | ||
| Abnormal (> 49.2) | 2 (4.26) | 6 (02.4) | 1.0 | - | |
| Mode of injury | 0.55 | 0.7 (0.2-2) | |||
| Blunt | 42 (89.3) | 229 (91.9) | |||
| Penetrating | 5 (10.6) | 20 (08.0) | |||
| Glasgow coma scale | 0.62 | 1.0 | - | ||
| Mild (13 - 15) | 30 (63.8) | 153 (61.4) | 1.3 (0.4-4.0) | ||
| Moderate (9 - 12) | 4 (08.5) | 27 (10.8) | |||
| Severe (1 - 8) | 13 (27.6) | 69 (27.7) | 1 (0.5-2.1) | ||
| Injury Severity Score | 0.28 | 1.0 | - | ||
| < 24 | 45 (97.8) | 143 (93.6) | 3.1 (0.4-23.8) | ||
| > 24 | 1 (2.2) | 16 (6.4) | |||
| PCO 2 , mmHg | 0.04 | 1.0 | 1.0 | ||
| Normal (35 - 45) | 20 (42.5) | 133 (53.4) | 2.3 (0.5-11.1) | 2.2 (0.4 - 10.2) | |
| Abnormal-high (>45) | 2 (04.2) | 31 (12.4) | 0.5 (0.2-1.0) | 0.4 (0.2 - 0.90) | |
| Abnormal-low (<35) | 25 (53.1) | 85 (34.1) | |||
| Hco 3, mEq/L | 0.98 | 1.0 | - | ||
| Normal (24 - 29) | 16 (34.0) | 86 (34.6) | |||
| Abnormal high (> 29) | 2 (04.2) | 7 (02.8) | 0.6(0.1-3.4) | ||
| Abnormal-low (< 24) | 29 (61.7) | 155 (62.5) | 0.9 (0.5-1.9) | ||
aValues expressed as f (%).
Table 5. [Part 2]. Analysis of Organ Failure (Univariate and Multivariate Analysis)a.
| Parameters | Organ Failure | P Value | Odds Ratio (95% CI) | Adjusted Odds Ratio(95% CI) | |
|---|---|---|---|---|---|
| No | Yes | ||||
| pH | 0.40 | 1.0 | - | ||
| Normal (7.35 - 7.45) | 15 (31.9) | 98 (31.5) | 0.7(0.3-1.4) | ||
| Abnormal low (< 7.35) | 23 (48.9) | 111 (44.7) | |||
| Abnormal high (> 7.45) | 9 (19.1) | 39 (15.7) | 0.6 (0.2-1.6) | ||
| Sodium, mEq/L | 0.33 | 1.0 | - | ||
| Normal (135 - 145) | 41 (87.2) | 207 (83.4) | 2.7 (0.3-21.6) | ||
| Abnormal high (> 145) | 1 (2.1) | 14 (05.6) | |||
| Abnormal low (< 135) | 5 (10.6) | 27 (10.8) | 1.0 (0.3-2.90) | ||
| Potassium, mEq/L | 0.02 | 1.0 | 1.0 | ||
| Normal (3.5 - 5) | 43 (91.4) | 178 (71.4) | 4.4(0.5-11.1) | 4.2(0.5 - 33.4) | |
| Abnormal-high (> 5) | 1 (2.10) | 21 (08.4) | |||
| Abnormal-low (< 3.5) | 3 (6.30) | 50 (20.0) | 4.1 (1.2-14.0) | 4.0 (1.1 - 14.0) | |
| Bilirubin, mg % | 0.22 | 1.0 | - | ||
| Normal (up to 1) | 40 (17.2) | 192 (82.7) | 1.6 (0.7-3.90) | ||
| Abnormal (> 1) | 7 (10.9) | 57 (89.0) | |||
| Total leukocyte Count, × 10³/cu mm | 0.25 | 1.0 | - | ||
| Normal (4000 - 10000) | 13 (27.6) | 50 (20.0) | 1.5 (0.74-30) | ||
| Abnormal high (> 10000) | 34 (72.3) | 197 (79.1) | 1.0 | ||
| Abnormal low (< 4000) | 0 | 2 ( 0.80) | |||
| Platelet, /cu mm | 0.91 | 1.0 | - | ||
| Normal (1 - 4 lakh) | 44 (93.6) | 232 (93.1) | |||
| Abnormal (< 1 lakh) | 3 (06.3) | 17 (06.8) | 1.0 (0.3-3.8) | ||
| Amylase, U/L | 0.31 | 1.0 | - | ||
| Normal (30 - 130) | 33 (70.2) | 192 (77.1) | 0.6 (0.3-1.3) | ||
| Abnormal-high (> 130) | 14 (29.7) | 57 (22.8) | |||
| Lipase, U/L | 0.82 | 1.0 | - | ||
| Normal (up to 60) | 38 (80.8) | 197 (79.1) | |||
| Abnormal-high (> 60) | 9 (19.1) | 51 (20.4) | 1.9 (0.4-2.4) | ||
aValues expressed as f (%).
The immediate outcome (dead/alive) of the study group was correlated with the clinical and laboratory parameters, and the univariate analysis was performed, followed by multivariate regression analysis of the variables that were determined to be statistically significant (Tables 6 and 7). The observed independent predictors of mortality were coagulopathy (OR = 1.7), Glasgow coma scale (OR = 1.1 , 4.7), sodium (OR = 18.2 ,3.4), potassium (OR = 5.7, 0.3), bilirubin (OR = 0.4), Hb (OR = 1.5), pulmonary failure (OR= 0.0004), hepatic failure (OR = 0.048), renal failure (OR = 5.5), organ failure (OR = 149.8), lipase (OR = 1.3) and infection (OR = 3.0).
Table 6. [Part 1]. Analysis for Outcome (Univariate and Multivariate Analysis).
| Parameters | Outcome | P Value | Odds Ratio (95% CI) | Adjusted Odds Ratio (95% CI) | |
|---|---|---|---|---|---|
| Alive | Dead | ||||
| Sex a | 0.41 | 1.0 1.4 (0.6 - 3.3) | - | ||
| Male | 218 (86.5) | 36 (81.8) | - | ||
| Female | 34 (13.4) | 8 (18.1) | |||
| Activated partial Thrombin time, sec | 0.01 | 1.0 6.2 (1.4 - 25.7) | 1.0 1.0 (0.9 - 1.0) | ||
| Normal (≤ 49.2) | 248 (98.4 | 40 (90.9) | |||
| Abnormal (> 49.2) | 4 (01.5) | 4 (09.0) | - | ||
| Coagulopathy a | < 0.001 | 1.3 3.7 (1.6 - 8.20) | |||
| No | 229 (90.8) | 32 (72.7) | 1.0 | ||
| Yes | 23 (09.1) | 12 (27.2) | - | ||
| Glasgow coma scale a | - | ||||
| Mild (13 - 15) | 168 (66.6) | 15 (34.0) | 1.0 2.6 (0.9 - 7.5) | - | |
| Moderate (9 - 12) | 25 (09.9) | 6 (13.6) | 0.06 | 4.3 (2.1 - 8.9) | - |
| Severe (1 - 8) | 59 (23.4) | 23 (52.2) | < 0.001 | ||
| Injury Severity Score | 0.74 | 1.3 (0.4 - 5.0) | - | ||
| < 24 | 238 (94.4) | 41 (93.2) | |||
| > 24 | 14 (5.7) | 3 (6.8) | |||
| Systolic BP, mmHg a | 0.96 | 1.0 | - | ||
| Normal (≤ 130) | 217 (86.1) | 38 (86.3) | 0.9 (0.3 - 2.4) | - | |
| Abnormal (> 130) | 35 (13.8) | 6 (13.6) | - | ||
| PCO 2 , mmHg | 1.0 | - | |||
| Normal (35 - 45) | 134 (53.1) | 19 (43.1) | - | ||
| Abnormal-high (> 45) | 27 (10.7) | 6 (13.6) | 0.38 | 1.5 (0.5 - 4.2) | - |
| Abnormal-low (< 35) | 91 (36.1) | 19 (43.1) | 0.27 | 1.4 (0.7 - 2.9) | |
| Hco 3, mEq/L | - | ||||
| Normal (24 - 29) | 88 (34.9) | 14 (32.5) | 1.0 | ||
| Abnormal high (> 29) | 6 (02.3) | 6 (13.6) | 0.13 | 3.1 (0.7 - 14) | |
| Abnormal-low (< 24) | 158 (62.7) | 26 (60.4) | 0.92 | 1.0 (0.5 - 2.0) | |
| pH | - | ||||
| Normal (7.35 - 7.45) | 098 (39.0) | 15 (34.0) | 1.0 | ||
| Abnormal low (< 7.35) | 113 (45.0) | 21 (47.7) | 0.59 | 1.2 (0.5 - 2.4) | |
| Abnormal high (> 7.45) | 40 (15.9) | 8 (18.1) | 0.57 | 1.3 (0.5 - 3.3) | |
| Sodium, mEq/L a | - | ||||
| Normal (135 - 145) | 221 (88.0) | 27 (61.3) | 1.0 | 1.0 | |
| Abnormal high (> 145) | 7 (02.9) | 8 (18.1) | < 0.001 | 9.3 (3.1 - 27.8) | 18.2 (2.6 - 124.5) |
| Abnormal low (< 135) | 23 (09.1) | 9 (20.4) | 0.009 | 3.2 (1.3 - 7.60) | 3.4 (0.6 - 17.20) |
aValues expressed as f (%).
Table 7. [Part 2]. Analysis for Outcome (Univariate and Multivariate Analysis).
| Parameters | Outcome | P Value | Odds Ratio (95% CI) | Adjusted Odds Ratio(95% CI) | |
|---|---|---|---|---|---|
| Alive | Dead | ||||
| Potassium, mEq/L | 0.02 | 1.0 | |||
| Normal (3.5 - 5) | 190 (75.4) | 31 (70.4) | 1.0 | 5.7 (0.8 - 37.5) | |
| Abnormal-high (> 5) | 15 (05.9) | 7 (15.9) | 0.03 | 2.8 (1.0 - 7.5) | 0.3 (0.06-2.1) |
| Abnormal-low (< 3.5) | 47 (18.6) | 6 (13.6) | 0.60 | 0.7 (0.3 - 1.9) | 4.0 (1.1 - 14.0) |
| Bilirubin, mg % | - | ||||
| Normal (up to 1) | 204 (80.9) | 28 (63.6) | 1.0 | 1.0 | |
| Abnormal (> 1) | 48 (19.0) | 16 (36.3) | 0.01 | 2.4 (1.2 - 4.8) | 0.4 (0.1 - 2.1) |
| Pulmonary failure | 0.25 | 1.0 | - | ||
| No | 55 (21.8) | 16 (36.3) | < 0.001 | 1.0 | 1.0 |
| Yes | 197 (78.1) | 28 (63.6) | 0.4 (0.2 - 0.9) | 0.0004 (.00001 - 0.01) | |
| Hepatic failure | 0.003 | - | |||
| No | 184 (73.0) | 22 (50.0) | 1.0 | 1.0 | |
| Yes | 68 (26.9) | 22 (50.0) | 2.7 (1.4 - 5.1) | 0.048 (.007 - 0.20) | |
| Renal failure | 0.31 | - | |||
| No | 251 (99.6) | 38 (86.3) | 1.0 | 1.0 | |
| Yes | 1 (0.40) | 6 (13.6) | 0.82 | 39.6 (4.6 - 338.2) | 5.5 (.08 - 346.4) |
| Hemoglobin, gms/dL a | < 0.001 | - | |||
| Normal (≥ 9) | 225 (89.2) | 28 (63.6) | 1.0 | 1.0 | |
| Abnormal (< 9) | 27 (10.7) | 16 (36.3) | 4.7 (2.2 - 9.9) | 1.5 (0.3 - 6.70) | |
| Platelet, /cu mm | 0.05 | ||||
| Normal (1 - 4 lakh) | 238 (86.2) | 38 (13.7) | 1.0 | 1.0 | |
| Abnormal (< 1 lakh) | 14 (70.0) | 6 (30.0) | 2.6 (0.9 - 7.4) | 1.0 (0.1 - 8.8) | |
| Amylase, U/L* | 0.90 | ||||
| Normal (30 - 130) | 194 (76.9) | 31 (70.4) | 1.0 | - | |
| Abnormal-high (> 130) | 58 (23.0) | 13 (29.5) | 1.0 (0.5 - 1.9) | - | |
| Lipase, U/L a | 0.040 | ||||
| Normal (up to 60) | 205 (81.6) | 30 (68.1) | 1.0 | 1.0 | |
| Abnormal-high (> 60) | 46 (18.3) | 14 (31.8) | 2.1 (1.0 - 4.2) | 1.3(0.3-60) | |
| Infection* | 0.02 | ||||
| No | 206 (81.7) | 25 (56.8) | 1.0 | 1.0 | |
| Yes | 46 (18.2) | 19 (43.1) | 3.4 (1.7-6.6) | 3.0 (0.7 - 11.8) | |
| Organ failure a | |||||
| No organ failure | 45 (17.8) | 2 (4.50) | 1.0 | 1.0 | |
| Single organ failure | 146 (57.9) | 7 (15.9) | 0.001 | 87.6 (6.6 - 1158.3) | 149.8 (9.4 - 2374.7) |
| Multiple organ failure | 61 (24.2) | 35 (79.5) | < 0.001 | 12.9 (2.9 - 56.4) | 183050.0 (1792 - 1.9) |
aValues expressed as f (%).
5. Discussion
Serum amylase and lipase levels are markers of pancreatic inflammation and are standard tests to diagnose acute pancreatitis; however, neither amylase nor lipase is specific for acute pancreatitis (13). Rise of the enzyme is detected in patients with trauma, tumors or intracranial hemorrhage, patients with abdominal trauma and those submitted to cardiac surgery (20). Malinoski et al. (19) reported that elevation in pancreatic enzymes in trauma patients in the absence of a pancreatic injury have an increased risk of morbidity and mortality. The results of our study suggest that elevated serum levels of pancreatic enzymes are independent predictors of organ failure and post trauma mortality. It is often difficult to predict whether enzyme elevations are due to ischemic pancreatitis or the translocation of intraluminal enteric pancreatic enzymes. It is unlikely that circulating pancreatic enzymes are direct cause of organ failure because of abundant protease inhibitors in the blood that bind and limit their activity but they may serve as tools to detect progression to organ failure in trauma patient (17, 21).
Elevation of the serum lipase and amylase is a common problem in clinical practice of an ICU and is not exclusive of pancreatic inflammation (22, 23). Liu et al. (12) reported that 15% of a group of patients admitted because of trauma, infection, tumor or other intracranial injuries showed elevated amylase and lipase levels without any evidence of pancreatitis, and recommend a routine monitoring of these enzymes. Lee et al. (14) reported an association of elevated pancreatic enzymes with various neurosurgery events and diagnoses and a higher mortality rate in patients admitted to the neurosurgery ICU.
The gut has been considered as one of the major sources of the inflammatory response following trauma and has the potential to lead to MOF (14, 24, 25), after traumatic injury intraluminal pancreatic enzymes have been postulated to enter the gut submucosa, activating local inflammatory mediators which then enter the systemic circulation through the mesenteric lymph and might play an important role in the pathogenesis of MOF (9). Several studies have demonstrated that inhibition of intraluminal pancreatic enzymes during the resuscitation minimizes the acute inflammatory response as well as histological organ injury (9, 26, 27). In addition, on ligating the pancreatic duct several weeks before hemorrhage, delayed mucosal injury and prolonged survival has been observed (11, 13).
Low levels of pancreatic enzymes are present in the healthy individual’s circulation in addition to residing in the lumen of intestinal tract (28). Serum pancreatic enzyme levels have been found to be elevated in 36% to 67% of critically ill patients (29, 30). Although some studies suggest that the hyperamylasemia of critical illness is from nonpancreatic sources (16), others depict an increase in either pancreatic lipase or amylase, both of which are specific indicators of pancreatic origin (29, 30). Regardless of which pancreatic enzyme is being measured, all the studies indicate that greater severity of organ failure and illness are correlated with elevated serum enzyme levels. Kumar et al. (16) reported a significant association of the elevation in serum amylase with spleen injury, and GIT injury.
Several clinical studies have demonstrated both histological and clinical evidence of ischemic pancreatic inflammation in a variety of shock states (31). Therefore, direct secretion of pancreatic enzymes into the circulation seems to have a reasonable correlation with progression of organ failure in trauma patient. More than a few studies have reported a mortality rate of 5.1% in patients with MOF (2). A mortality rate of 36.4% was reported in our study.
Malinoski et al. (19) observed that patients with an elevated amylase level were more at a risk of developing organ failure, present in shock and had a greater risk of death and patient with an elevated lipase level were likely to develop organ failure. In our study, patients with an elevated amylase level had a greater risk for renal failure and patients with an elevated lipase level were more prone to develop coagulopathy, MOF and had a greater risk of death. These patients were at higher risk of infection and had an abnormal level of platelet count.
The independent predictors of organ failure in their study (19) were age; ISS, massive transfusion, elevated amylase and lipase and the independent predictors for mortality were age, ISS, massive transfusion, shock and elevated amylase. In the present study, the predictors of organ failure were coagulopathy and infection. Predictors of mortality were organ failure, coagulopathy, infection, GCS, bilirubin, elevated lipase, hemoglobin and platelet count.
Our study corroborates the findings of previous studies in critically ill patients; the increase in serum pancreatic enzymes is associated with greater degrees of shock, injury severity, organ dysfunction, and death. The elevated lipase level was significantly correlated with the incidence of MOF in acutely injured trauma patients. Association between the elevated amylase and organ failure was not significant. Measuring levels of these enzymes after admission, coupled with other laboratory investigations (Hb, bilirubin, and creatinine) may be helpful in the identification of patients who are at a risk of infection and progression towards organ failure and ensuring optimum management of patients following trauma.
Footnotes
Authors’ Contributions:All authors contributed in concepts, design, definition of intellectual content, literature search, clinical studies, experimental studies, data acquisition, data analysis, statistical analysis and manuscript preparation/ editing/ review.
References
- 1.Ciesla DJ, Moore EE, Johnson JL, Burch JM, Cothren CC, Sauaia A. A 12-year prospective study of postinjury multiple organ failure: has anything changed? Arch Surg. 2005;140(5):432–8. doi: 10.1001/archsurg.140.5.432. discussion 438-40. [DOI] [PubMed] [Google Scholar]
- 2.Durham RM, Moran JJ, Mazuski JE, Shapiro MJ, Baue AE, Flint LM. Multiple organ failure in trauma patients. J Trauma. 2003;55(4):608–16. doi: 10.1097/01.TA.0000092378.10660.D1. [DOI] [PubMed] [Google Scholar]
- 3.Le Gall JR, Klar J, Lemeshow S, Saulnier F, Alberti C, Artigas A, et al. The Logistic Organ Dysfunction system. A new way to assess organ dysfunction in the intensive care unit. ICU Scoring Group. JAMA. 1996;276(10):802–10. doi: 10.1001/jama.276.10.802. [DOI] [PubMed] [Google Scholar]
- 4.Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23(10):1638–52. doi: 10.1097/00003246-199510000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 6.Lausevic Z, Lausevic M, Trbojevic-Stankovic J, Krstic S, Stojimirovic B. Predicting multiple organ failure in patients with severe trauma. Can J Surg. 2008;51(2):97–102. [PMC free article] [PubMed] [Google Scholar]
- 7.Moore FA, Moore EE. Evolving concepts in the pathogenesis of postinjury multiple organ failure. Surg Clin North Am. 1995;75(2):257–77. doi: 10.1016/s0039-6109(16)46587-4. [DOI] [PubMed] [Google Scholar]
- 8.Waldo SW, Rosario HS, Penn AH, Schmid-Schonbein GW. Pancreatic digestive enzymes are potent generators of mediators for leukocyte activation and mortality. Shock. 2003;20(2):138–43. doi: 10.1097/01.shk.0000073866.47824.ae. [DOI] [PubMed] [Google Scholar]
- 9.Kistler EB, Hugli TE, Schmid-Schonbein GW. The pancreas as a source of cardiovascular cell activating factors. Microcirculation. 2000;7(3):183–92. [PubMed] [Google Scholar]
- 10.Byrne MF, Mitchell RM, Stiffler H, Jowell PS, Branch MS, Pappas TN, et al. Extensive investigation of patients with mild elevations of serum amylase and/or lipase is 'low yield'. Can J Gastroenterol. 2002;16(12):849–54. doi: 10.1155/2002/836012. [DOI] [PubMed] [Google Scholar]
- 11.Manjuck J, Zein J, Carpati C, Astiz M. Clinical significance of increased lipase levels on admission to the ICU. Chest. 2005;127(1):246–50. doi: 10.1378/chest.127.1.246. [DOI] [PubMed] [Google Scholar]
- 12.Liu KJ, Atten MJ, Lichtor T, Cho MJ, Hawkins D, Panizales E, et al. Serum amylase and lipase elevation is associated with intracranial events. Am Surg. 2001;67(3):215–9. discussion 219-20. [PubMed] [Google Scholar]
- 13.Chen CC. Clinical implication of increased pancreatic enzymes in ICU patients. J Chin Med Assoc. 2010;73(3):129–30. doi: 10.1016/S1726-4901(10)70026-5. [DOI] [PubMed] [Google Scholar]
- 14.Lee CC, Chung WY, Shih YH. Elevated amylase and lipase levels in the neurosurgery intensive care unit. J Chin Med Assoc. 2010;73(1):8–14. doi: 10.1016/S1726-4901(10)70015-0. [DOI] [PubMed] [Google Scholar]
- 15.Malinoski DJ, Barrios C, Kim HD. Role of pancreatic enzymes in the development of multiple organ failure after shock. J Organ Dysfunct. 2008;4:161–7. doi: 10.1080/17471060801925288. [DOI] [Google Scholar]
- 16.Kumar S, Sagar S, Subramanian A, Albert V, Pandey RM, Kapoor N. Evaluation of amylase and lipase levels in blunt trauma abdomen patients. J Emerg Trauma Shock. 2012;5(2):135–42. doi: 10.4103/0974-2700.96482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rothman S, Liebow C, Isenman L. Conservation of digestive enzymes. Physiol Rev. 2002;82(1):1–18. doi: 10.1152/physrev.00022.2001. [DOI] [PubMed] [Google Scholar]
- 18.Antonelli M, Moreno R, Vincent JL, Sprung CL, Mendoca A, Passariello M, et al. Application of SOFA score to trauma patients. Sequential Organ Failure Assessment. Intensive Care Med. 1999;25(4):389–94. doi: 10.1007/s001340050863. [DOI] [PubMed] [Google Scholar]
- 19.Malinoski DJ, Hadjizacharia P, Salim A, Kim H, Dolich MO, Cinat M, et al. Elevated serum pancreatic enzyme levels after hemorrhagic shock predict organ failure and death. J Trauma. 2009;67(3):445–9. doi: 10.1097/TA.0b013e3181b5dc11. [DOI] [PubMed] [Google Scholar]
- 20.Ulvik A, Wentzel-Larsen T, Flaatten H. Trauma patients in the intensive care unit: short- and long-term survival and predictors of 30-day mortality. Acta Anaesthesiol Scand. 2007;51(2):171–7. doi: 10.1111/j.1399-6576.2006.01207.x. [DOI] [PubMed] [Google Scholar]
- 21.Frank B, Gottlieb K. Amylase normal, lipase elevated: is it pancreatitis? A case series and review of the literature. Am J Gastroenterol. 1999;94(2):463–9. doi: 10.1111/j.1572-0241.1999.878_g.x. [DOI] [PubMed] [Google Scholar]
- 22.Yi SY, Tae JH. Pancreatic abscess following scrub typhus associated with multiorgan failure. World J Gastroenterol. 2007;13(25):3523–5. doi: 10.3748/wjg.v13.i25.3523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beauregard JM, Lyon JA, Slovis C. Using the literature to evaluate diagnostic tests: amylase or lipase for diagnosing acute pancreatitis? J Med Libr Assoc. 2007;95(2):121–6. doi: 10.3163/1536-5050.95.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grotz MR, Deitch EA, Ding J, Xu D, Huang Q, Regel G. Intestinal cytokine response after gut ischemia: role of gut barrier failure. Ann Surg. 1999;229(4):478–86. doi: 10.1097/00000658-199904000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flint RS, Windsor JA. The role of the intestine in the pathophysiology and management of severe acute pancreatitis. HPB (Oxford). 2003;5(2):69–85. doi: 10.1080/13651820310001108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Doucet JJ, Hoyt DB, Coimbra R, Schmid-Schonbein GW, Junger WG, Paul LW, et al. Inhibition of enteral enzymes by enteroclysis with nafamostat mesilate reduces neutrophil activation and transfusion requirements after hemorrhagic shock. J Trauma. 2004;56(3):501–10. doi: 10.1097/01.ta.0000114536.98447.f7. discussion 510-1. [DOI] [PubMed] [Google Scholar]
- 27.Acosta JA, Hoyt DB, Schmid-Schonbein GW, Hugli TE, Anjaria DJ, Frankel DA, et al. Intraluminal pancreatic serine protease activity, mucosal permeability, and shock: a review. Shock. 2006;26(1):3–9. doi: 10.1097/01.shk.0000209557.31457.ae. [DOI] [PubMed] [Google Scholar]
- 28.Broderick JW, Geokas MC, Largman C, Fassett M, Johnson JH. Am J Physiol. Molecular Forms of immunoreactive pancreatic cationic trypsin in pancreatitis patient sera. 1979;237(474 -480) doi: 10.1152/ajpendo.1979.237.5.E474. [DOI] [PubMed] [Google Scholar]
- 29.Pezzilli R, Morselli-Labate AM, Romboli E, Dibenedetti F, Massa M, Migliori M, et al. Pancreatic involvement during the early phase of shock. JOP. 2002;3(5):139–43. [PubMed] [Google Scholar]
- 30.Grulke S, Deby-Dupont G, Cassart D, Gangl M, Caudron I, Lamy M, et al. Pancreatic injury in equine acute abdomen evaluated by plasma trypsin activity and histopathology of pancreatic tissue. Vet Pathol. 2003;40(1):8–13. doi: 10.1354/vp.40-1-8. [DOI] [PubMed] [Google Scholar]
- 31.Sakorafas GH, Tsiotos GG, Sarr MG. Ischemia/Reperfusion-Induced pancreatitis. Dig Surg. 2000;17(1):3–14. doi: 10.1159/000018793. [DOI] [PubMed] [Google Scholar]