Abstract
Background
Tibial plateau fractures can be successfully fixed utilizing 3.5 mm locking plates. However, there are some disadvantages to using these plates.
Objectives
In the current prospective study, we investigated the outcome of treating different types of tibial plateau fractures with 3.5 mm simple plates which, to our knowledge, has not been evaluated in previous studies.
Materials and Methods
Between 2011 and 2013, 32 patients aged 40 ± 0.2 years underwent open reduction and internal fixation for tibial plateau fractures with 3.5 mm simple plates. The patients were followed for 16.14 ± 2.1 months. At each patient’s final visit, the articular surface depression, medial proximal tibial angle, and slope angle were measured and compared with measurements taken early after the operation. The functional outcomes were measured with the WOMAC and Lysholm knee scores.
Results
The mean union time was 13 ± 1.2 weeks. The mean knee range of motion was 116.8° ± 3.3°. The mean WOMAC and Lysholm scores were 83.5 ± 1.8 and 76.8 ± 1.6, respectively. On the early postoperative and final X-rays, 87.5% and 84% of patients, respectively, had acceptable reduction. Medial proximal tibial and slope angles did not change significantly by the last visit. No patient was found to have complications related to the type of plate.
Conclusions
In this case series study, the fixation of different types of tibial plateau fractures with 3.5 mm simple non-locking and non-precontoured plates was associated with acceptable clinical, functional, and radiographic outcomes. Based on the advantages and costs of these plates, the authors recommend using 3.5 mm simple plates for different types of tibial plateau fractures.
Keywords: Fracture, Osteosynthesis, Tibial Plateau, Internal Fixation
1. Background
The principles for the treatment of tibial plateau fractures have progressed substantially over the past 50 years. Nonsurgical treatment was used for most of these fractures before the 1980s, but with the development of internal fixation techniques, surgical treatment became more common (1). The advantages of surgical treatment include early mobilization of the knee, rapid bone union, and better quality of reduction (2).
Currently, locking plates are being used increasingly for fixation of tibial plateau fractures. In the past, 4.5 mm plates were used, but some surgeons now tend to use 3.5 mm locking plates (3). These plates are less bulky and easier to adapt on the bone, and good outcomes have been reported with regard to utilizing them in comminuted tibial plateau fractures (4). However, these fixation tools are associated with some disadvantages. They are expensive, and although they are precontoured, they do not all adapt completely to the bone (5). Occasionally, the surgeon is forced to change the shape of the plate to adapt it onto the bone completely, which may damage the locking property of the screw. In some types of locking plates, interfragmentary compression is only achieved when the locking screws are inserted at a 90° angle in relation to the plate (6). Based on these problems, we encourage using 3.5 mm simple plates, which can be easily adapted to the bone. Furthermore, these plates are inexpensive. To our knowledge, there is no study using 3.5 mm simple plates for the treatment of tibial plateau fractures.
2. Objectives
In the current prospective study, we investigated the clinical, functional, and radiological outcomes of treating different types of tibial plateau fractures with T- or L-shaped 3.5 mm simple non-locking and non-contoured plates.
3. Materials and Methods
Between 2011 and 2013, 45 patients with different types of tibial plateau fractures underwent internal fixation using 3.5 mm simple T- or L-shaped plates at our hospital. The exclusion criteria were open fracture, concomitant injuries that could alter the functional outcome (such as ipsilateral femoral shaft fracture), previous major trauma, previous history of knee surgery, deformity of the affected knee, pathologic fracture, preexisting joint disease (severe osteoarthritis, inflammatory arthritis, or a prior fracture), severe systemic illness (a medical contraindication for surgery), open growth plates, vascular injury requiring repair, severe head injury, or other neurological conditions that would interfere with rehabilitation.
After the primary clinical examination, plain radiography of the knee was performed. If there was a tibial plateau fracture, the patient was referred for CT scanning. The amount of displacement and depression of the articular surface was evaluated by anteroposterior (AP) and lateral x-rays, as well as CT scans. If surgical treatment was required, informed consent was obtained.
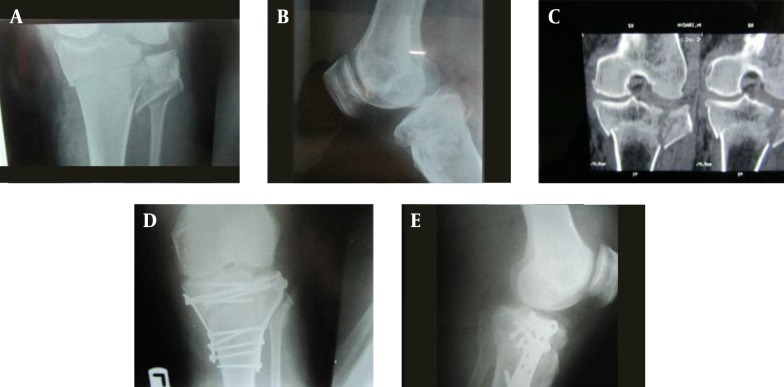
The fractures were classified based on Schatzker’s classification. The condition of the soft tissues was evaluated before the operation, and if this was unsuitable, the operation was delayed until soft-tissue healing. All patients underwent open reduction and internal fixation (ORIF). All of the operations were performed by two expert orthopedic surgeons, and 3.5 mm simple plates were used for all types of fractures, including type V and VI. In patients with type V and VI fractures, posteromedial and anterolateral approaches were used, if necessary (Figure 1).
Figure 1. A 42-year-old patient with type VI tibial plateau fracture, posteromedial and anterolateral approaches were used. A, preoperative anteroposterior X-ray showing the tibial plateau fracture type VI of the left knee; B, preoperative lateral X-ray of the same knee; C, preoperative CT scan of the patient’s knee showing the extent of the fracture in the coronal plane; D and E, postoperative AP and lateral views of the knee fixated using double simple plates.
For reduction of the articular surface, the submeniscal arthrotomy technique was used. In cases with more intra-articular fragments, raft screws (3.5 mm cortical screws or 4 mm cancellous screws) were used. The bone defects were filled by bone grafts; autografts were used for most cases. The coronary ligament and capsule were also repaired. After the operation, the knee was immobilized for 48 hours, followed by early active ROM exercises. The patients wore knee immobilizers for six weeks during walking and sleeping, and they were allowed to do partial weight-bearing after six weeks, depending on union progression. Postoperative X-rays of the knee were taken immediately after the surgery and six weeks later, then every six weeks until bony union occurred. Union was defined as the presence of three bridging cortices on images in two orthogonal planes.
The patients were each recalled to the hospital for a final visit, when WOMAC and Lysholm scores were completed. Anteroposterior and lateral knee X-rays were also obtained, and the amount of articular surface depression, the medial proximal tibial angle (MPTA), and the slope angle were measured and compared with the early postoperative X-rays. Articular surface depression was evaluated as follows:
Excellent: ˂ 2 mm depression
Satisfactory: 2 - 5 mm depression
Poor: > 5 mm depression.
A gap of ≥ 5 mm in the articular surface was considered a poor reduction, and MPTAs of < 80° or > 95° were considered malalignment. The measurements were performed by two orthopedic surgeons, and the final value was defined as the average of the two measurements.
3.1. Statistics
SPSS statistical software (version 15.0; SPSS, Chicago, IL, USA) was used for statistical analysis. Paired t-test was utilized to compare the early postoperative and final MPTAs and slope angles. The quality of reduction was compared using McNemar’s test. A P value of < 0.005 was considered statistically significant.
4. Results
In this case series study, out of 45 patients, 13 were lost during follow-up. One patient was a polytrauma patient, and in four patients, 3.5 mm and 4.5 mm plates were used together. Eight patients did not participate in the follow-up program or were not accessible. The demographics of the 32 patients who completed the study are presented in Table 1.
Table 1. Demographic Characteristics of Patients with Tibial Plateau Fractures a,b.
| Variables | Values |
|---|---|
| Gender | |
| Male | 22 (68) |
| Female | 10 (32) |
| Age (19 - 70), y | 40 ± 0.2 |
| Side of surgery | |
| Right | 18 (56) |
| Left | 14 (4) |
| Type of fracture | |
| I | 3 (9) |
| II | 16 (50) |
| III | 2 (6) |
| IV | 4 (12) |
| V | 3 (9) |
| VI | 4 (12) |
| Follow-up period (6 - 48), mo | 16.14 ± 2.1 |
a Total number of patients is 32.
b Values are expressed as No. (%) or mean ± SD.
The mean union time for at least three cortices was 13 ± 1.2 weeks (range 8 - 24). The interval between the operation time and full weight-bearing averaged 15 ± 1.5 weeks (range 8 - 28). At the final follow-up, the mean ROM was 116.8° ± 3.3° (60° - 140°). The numbers of patients who required bone grafts and raft screws, and the types of plates used, are presented in Table 2.
Table 2. Surgical Details of Patients with Tibial Plateau Fractures.
| Graft and Devices | Frequency (%) |
|---|---|
| Type of graft | |
| Autograft | 14 (43) |
| Allograft | 4 (12 ) |
| Type of plate | |
| T-shaped | 22 (69) |
| L-shaped | 6 (19) |
| Reconstruction plate | 4 (12) |
| Raft screw | 12 (37) |
4.1. Functional Assessment
The means of the WOMAC and Lysholm knee scores were 83.5 ± 1.8 and 76.8 ± 1.6, respectively.
4.2. Radiological Assessment
Immediate postoperative X-rays showed satisfactory to excellent reduction in 28 patients (87.5%). In two cases, an approximately 5 mm gap was found in the articular surface. Two other patients had 5 mm depressions of the articular surface. At the final visit, we found that the articular surface reduction was lost in one patient, while satisfactory to excellent reduction was present in 27 patients (84%). The mean MPTA and slope angle, respectively, were 85.3° ± 4.2° and 8.5° ± 3° on the early postoperative images and 84.5° ± 4° and 8.2° ± 3.5° on the final x-rays.
The degenerative changes did not progress in the patients with preoperative knee osteoarthrosis; however, two patients had developed degenerative changes in the knee at the time of the final follow-up.
4.3. Complications
Limited ROM was found in five patients (15.6%). In four of these, ROM was improved by physical therapy; however, in one patient, knee flexion did not exceed 80° due to lack of patient compliance with exercise therapy. Two patients developed superficial wound infections, and one patient developed a deep infection that was improved with repeated irrigation and debridement. One patient had delayed union, with the fracture healing after nine months.
5. Discussion
The most important finding of the current study was that treatment of tibial plateau fractures using 3.5 mm simple plates was associated with satisfactory clinical, functional, and radiographic outcome.
Tibial plateau fractures can be treated surgically or non-surgically (7). The aim of surgical treatment is to obtain stability, proper alignment, and congruent articular surfaces (8, 9). However, surgical treatment for tibial plateau fractures can lead to many complications, including wound breakdown, deep infection (2.8% - 8%), DVT (3.6% - 7%), compartment syndrome, non-union, peroneal nerve injury, device failure (hardware failure), and arthrofibrosis (10-14). Recently, minimally invasive surgeries have been designed to reduce these complications (15-17). There are several surgical methods, such as external fixation, percutaneous screw fixation, ORIF, less-invasive stabilization systems (LISS), double osteosynthesis, and staged external and internal fixation (18-21), but there is no consensus as to the most appropriate method (22, 23). Blokker et al. suggested surgical treatment when the articular surface depression was > 5 mm (8). Reduction of the articular surface by plate and screws can also reduce the risk of degenerative changes of the knee (24).
In the past, L- or T-shaped 4.5 mm plates were used in lateral or medial tibial plateau fractures, and partial-thread 6.5 mm screws were used for compression of the articular surface (25). In the late 1980s and into the 1990s, with the invention of locking plates, which were thought to enhance mechanical stability, surgeons tended to use the 4.5 mm locking plates for fixation of tibial plateau fractures (26-29). However, although there are satisfactory outcomes from treating plateau fractures with these new plates, some complications have been reported. Krettek et al. reported complications with 4.5 mm plates that included devitalization of the fracture due to extensive stripping of muscle from bone, risk of peroneal nerve injury, and complications from placing the plates in the lateral limited space (17). It seems that using 3.5 mm plates can reduce the risk of these complications, and these plates can be placed on the fracture site easily, with less injury to the soft tissues around the bone. Also, for better stabilization of fragments in comminuted fractures, 3.5 mm screws or K-wire can be used near the articular surface with raft screws or wire (30, 31). Moreover, there is no significant difference in the biomechanical properties between locked 3.5 mm and 4.5 mm plates (32). It has been shown that in cancellous bone, 3.5 mm screws have equivalent pullout strength in comparison to 4.5 mm and 6.5 mm screws (32, 33). Furthermore, the smaller 3.5 mm screws allow more of them to be placed closer to the articular surface, to support the reduced fragments.
Pre-contoured anatomic plates for proximal tibial fractures are made by different manufacturers and have several advantages, such as decreased time spent on intraoperative plate-contouring and the use of minimally invasive surgery. However, in a cadaveric study, Goyal et al. demonstrated that anatomic plates made by popular manufacturers were not matched completely to the bones of the cadaver samples, with the plates not completely touching the bone (5). However, the simple 3.5 mm plates can be formed and placed on the bone easily during the surgery. In addition, non-locking screws can facilitate compression between fracture fragments. Furthermore, locking plates are more expensive than simple plates, which may exert a considerable financial burden on patients.
The complications of 4.5 mm plates (locking or simple), the problems with contouring locking plates to the bone surface, cost-benefit considerations, and a consideration of the efficiency properties led us to use 3.5 mm simple non-locking and non-precontoured plates for the treatment of tibial plateau fractures. In our experience, all of the fractures united, without any complications related to the type or size of the plate. The functional outcomes were acceptable and the reduction achieved with surgery was maintained after 16 months. Even in Schatzker’s type V and VI fractures, under suitable soft-tissue conditions, simple 3.5 mm plates were used with anterolateral and posteromedial approaches if necessary, and there were no cases of failed fixation. In such cases, the 3.5 mm lateral plate must function as a buttress device and the medial plate must function as an anti-glide device. Single lateral plating does not provide sufficient stability (34).
In our study, the functional outcomes were satisfactory, considering the WOMAC and Lysholm scores. All of the fractures healed in an acceptable amount of time. Patients were able to ambulate after 15 days on average, and the average knee range of motion was good (116.8° ± 3.3°). Anatomical reduction was achieved in most of the patients (87.5%); however, in one of them, the reduction was lost after the operation. Unacceptable reductions in four patients were related to severe comminution rather than to the type of plate. The rate of loss of reduction in the current study is similar to other studies that used other types of plates for tibial plateau fractures (29).
The small sample size and the short follow up were limitations.
5.1. Conclusion
Based on the findings of this study, regardless of the type of tibial plateau fracture, ORIF using 3.5 mm simple plates can lead to acceptable clinical, functional, and radiographic outcomes.
Acknowledgments
The authors acknowledge the valuable feedback provided by Davood Jafari during the preparation of this article.
Footnotes
Authors’ Contribution:Study concept and design: Abolfazl Bagherifard; acquisition, analysis, and interpretation of data: Mohammadreza Minator Sajadi and Hossein Karimi Heris; drafting of the manuscript: Mahmoud Jabalameli; critical revision of the manuscript for important intellectual content: Hosseinali Hadi; statistical analysis: Ali Jahansouz; study supervision: Mohammad Rahbar.
References
- 1.Biyani A, Reddy NS, Chaudhury J, Simison AJ, Klenerman L. The results of surgical management of displaced tibial plateau fractures in the elderly. Injury. 1995;26(5):291–7. doi: 10.1016/0020-1383(95)00027-7. [DOI] [PubMed] [Google Scholar]
- 2.Yu Z, Zheng L, Zhang Y, Li J, Ma B. Functional and radiological evaluations of high-energy tibial plateau fractures treated with double-buttress plate fixation. Eur J Med Res. 2009;14(5):200–5. doi: 10.1186/2047-783X-14-5-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaab MJ, Frenk A, Schmeling A, Schaser K, Schutz M, Haas NP. Locked internal fixator: sensitivity of screw/plate stability to the correct insertion angle of the screw. J Orthop Trauma. 2004;18(8):483–7. doi: 10.1097/00005131-200409000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Yoo BJ, Beingessner DM, Barei DP. Stabilization of the posteromedial fragment in bicondylar tibial plateau fractures: a mechanical comparison of locking and nonlocking single and dual plating methods. J Trauma. 2010;69(1):148–55. doi: 10.1097/TA.0b013e3181e17060. [DOI] [PubMed] [Google Scholar]
- 5.Goyal KS, Skalak AS, Marcus RE, Vallier HA, Cooperman DR. Analysis of anatomic periarticular tibial plate fit on normal adults. Clin Orthop Relat Res. 2007;461:245–57. doi: 10.1097/BLO.0b013e31809e6e45. [DOI] [PubMed] [Google Scholar]
- 6.Greiwe RM, Archdeacon MT. Locking plate technology: current concepts. J Knee Surg. 2007;20(1):50–5. doi: 10.1055/s-0030-1248022. [DOI] [PubMed] [Google Scholar]
- 7.DeCoster TA, Nepola JV, el-Khoury GY. Cast brace treatment of proximal tibia fractures. A ten-year follow-up study. Clin Orthop Relat Res. 1988;(231):196–204. [PubMed] [Google Scholar]
- 8.Blokker CP, Rorabeck CH, Bourne RB. Tibial plateau fractures. An analysis of the results of treatment in 60 patients. Clin Orthop Relat Res. 1984;(182):193–9. [PubMed] [Google Scholar]
- 9.Rademakers MV, Kerkhoffs GM, Sierevelt IN, Raaymakers EL, Marti RK. Operative treatment of 109 tibial plateau fractures: five- to 27-year follow-up results. J Orthop Trauma. 2007;21(1):5–10. doi: 10.1097/BOT.0b013e31802c5b51. [DOI] [PubMed] [Google Scholar]
- 10.Andrews JR, Tedder JL, Godbout BP. Bicondylar tibial plateau fracture complicated by compartment syndrome. Orthop Rev. 1992;21(3):317–9. [PubMed] [Google Scholar]
- 11.Chan DB, Jeffcoat DM, Lorich DG, Helfet DL. Nonunions around the knee joint. Int Orthop. 2010;34(2):271–81. doi: 10.1007/s00264-009-0924-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baima J, Krivickas L. Evaluation and treatment of peroneal neuropathy. Curr Rev Musculoskelet Med. 2008;1(2):147–53. doi: 10.1007/s12178-008-9023-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lasanianos NG, Garnavos C, Magnisalis E, Kourkoulis S, Babis GC. A comparative biomechanical study for complex tibial plateau fractures: nailing and compression bolts versus modern and traditional plating. Injury. 2013;44(10):1333–9. doi: 10.1016/j.injury.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 14.Young MJ, Barrack RL. Complications of internal fixation of tibial plateau fractures. Orthop Rev. 1994;23(2):149–54. [PubMed] [Google Scholar]
- 15.Lee JA, Papadakis SA, Moon C, Zalavras CG. Tibial plateau fractures treated with the less invasive stabilisation system. Int Orthop. 2007;31(3):415–8. doi: 10.1007/s00264-006-0176-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.El Barbary H, Abdel Ghani H, Misbah H, Salem K. Complex tibial plateau fractures treated with Ilizarov external fixator with or without minimal internal fixation. Int Orthop. 2005;29(3):182–5. doi: 10.1007/s00264-005-0638-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krettek C, Gerich T, Miclau T. A minimally invasive medial approach for proximal tibial fractures. Injury. 2001;32 Suppl 1:Sa4–13. doi: 10.1016/s0020-1383(01)00056-0. [DOI] [PubMed] [Google Scholar]
- 18.Chin TY, Bardana D, Bailey M, Williamson OD, Miller R, Edwards ER, et al. Functional outcome of tibial plateau fractures treated with the fine-wire fixator. Injury. 2005;36(12):1467–75. doi: 10.1016/j.injury.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Egol KA, Tejwani NC, Capla EL, Wolinsky PL, Koval KJ. Staged management of high-energy proximal tibia fractures (OTA types 41): the results of a prospective, standardized protocol. J Orthop Trauma. 2005;19(7):448–55. doi: 10.1097/01.bot.0000171881.11205.80. [DOI] [PubMed] [Google Scholar]
- 20.Singh S, Patel PR, Joshi AK, Naik RN, Nagaraj C, Kumar S. Biological approach to treatment of intra-articular proximal tibial fractures with double osteosynthesis. Int Orthop. 2009;33(1):271–4. doi: 10.1007/s00264-007-0480-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Su EP, Westrich GH, Rana AJ, Kapoor K, Helfet DL. Operative treatment of tibial plateau fractures in patients older than 55 years. Clin Orthop Relat Res. 2004;(421):240–8. doi: 10.1097/01.blo.0000119247.60317.bc. [DOI] [PubMed] [Google Scholar]
- 22.Ali AM, Saleh M, Bolongaro S, Yang L. Experimental model of tibial plateau fracture for biomechanical testing. J Biomech. 2006;39(7):1355–60. doi: 10.1016/j.jbiomech.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 23.Krupp RJ, Malkani AL, Roberts CS, Seligson D, Crawford CH. 3rd., Smith L. Treatment of bicondylar tibia plateau fractures using locked plating versus external fixation. Orthopedics. 2009;32(8) doi: 10.3928/01477447-20090624-11. [DOI] [PubMed] [Google Scholar]
- 24.Parkkinen M, Madanat R, Mustonen A, Koskinen SK, Paavola M, Lindahl J. Factors predicting the development of early osteoarthritis following lateral tibial plateau fractures: mid-term clinical and radiographic outcomes of 73 operatively treated patients. Scand J Surg. 2014;103(4):256–62. doi: 10.1177/1457496914520854. [DOI] [PubMed] [Google Scholar]
- 25.Sament R, Mayanger JC, Tripathy SK, Sen RK. Closed reduction and percutaneous screw fixation for tibial plateau fractures. J Orthop Surg (Hong Kong). 2012;20(1):37–41. doi: 10.1177/230949901202000108. [DOI] [PubMed] [Google Scholar]
- 26.Smith WR, Ziran BH, Anglen JO, Stahel PF. Locking plates: tips and tricks. J Bone Joint Surg Am. 2007;89(10):2298–307. doi: 10.2106/00004623-200710000-00028. [DOI] [PubMed] [Google Scholar]
- 27.Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma. 2004;18(8):528–35. doi: 10.1097/00005131-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Stannard JP, Wilson TC, Volgas DA, Alonso JE. The less invasive stabilization system in the treatment of complex fractures of the tibial plateau: short-term results. J Orthop Trauma. 2004;18(8):552–8. doi: 10.1097/00005131-200409000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Horesh Z, Rothem DE, Lerner A, Soudry M. Treatment of complex tibial plateau fracture with ilizarov external fixation and minimal open surgical procedure. J Bone Jt Surg, Br Vol. 2008;90(SUPP III):514. [Google Scholar]
- 30.Karunakar MA, Egol KA, Peindl R, Harrow ME, Bosse MJ, Kellam JF. Split depression tibial plateau fractures: a biomechanical study. J Orthop Trauma. 2002;16(3):172–7. doi: 10.1097/00005131-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Yoon YC, Oh JK, Oh CW, Sahu D, Hwang JH, Cho JW. Inside out rafting K-wire technique for tibial plateau fractures. Arch Orthop Trauma Surg. 2012;132(2):233–7. doi: 10.1007/s00402-011-1409-z. [DOI] [PubMed] [Google Scholar]
- 32.Hasan S, Ayalon OB, Yoon RS, Sood A, Militano U, Cavanaugh M, et al. A biomechanical comparison between locked 3.5-mm plates and 4.5-mm plates for the treatment of simple bicondylar tibial plateau fractures: is bigger necessarily better? J Orthop Traumatol. 2014;15(2):123–9. doi: 10.1007/s10195-013-0275-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Westmoreland GL, McLaurin TM, Hutton WC. Screw pullout strength: a biomechanical comparison of large-fragment and small-fragment fixation in the tibial plateau. J Orthop Trauma. 2002;16(3):178–81. doi: 10.1097/00005131-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Wu CC, Tai CL. Plating treatment for tibial plateau fractures: a biomechanical comparison of buttress and tension band positions. Arch Orthop Trauma Surg. 2007;127(1):19–24. doi: 10.1007/s00402-006-0192-8. [DOI] [PubMed] [Google Scholar]