Abstract
Background
The association between lipid levels and stroke rates is less than lipid levels and coronary heart disease (CHD)
Objective
To assess if there are geographic, racial, and ethnic differences in total cholesterol (TC), low density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol(HDL-C) and triglyceride levels with incident stroke.
Methods
From The REasons for Geographic AndRacial Differences in Stroke (REGARDS) study we evaluated baseline levels of LDL-C, HCL-C, TC, Non-HDL-C (Total - HDL-C) and triglycerides in participants free of prevalent stroke at baseline. Cox Proportional-Hazard models were the main analytical tool used to examine the association between incident stroke and lipids. For each adjusted lipid measure (LDL-C, HDL-C, triglycerides, TC, and non-HDL-C) we calculated a series of incremental models.
Results
The analysis cohort was 23,867 participants with a mean follow-up time of 7.5 +/− 2.9 years, and 1031 centrally adjudicated strokes (874 ischemic and 77 hemorrhagic strokes). HDL-C baseline level was associated with an overall unadjusted 13% risk reduction (HR 0.87, 95% confidence interval [CI]: 0.81–0.93; p<0.05; 14% for ischemic and 16% for hemorrhagic strokes), and TC with an 8% (HR 0.92, 95%CI: 0.87–0.99; p<0.05) risk reduction of all strokes. When the results were fully adjusted a significant association was observed only for LDL-C and non-HDL-C and ischemic stroke. There were no significant differences in these associations when adjusted for age, race, age*race, gender, education, region, or income.
Conclusion
In a disease free population, LDL-C and non-HDL-C baseline levels are significantly associated with the risk of ischemic stroke.
Keywords: ischemic, hemorrhagic, stroke, lipids, cholesterol
Current stroke prevention recommendations focus on optimizing dyslipidemia although the epidemiologic association between serum cholesterol levels and adjusted stroke rates is not as strong as that between serum cholesterol levels and coronary heart disease (CHD).1–4 In the Asia Pacific Cohort Studies Collaboration there was a 25% increase in ischemic stroke for each 1 mmol increase in total cholesterol (TC), while neither the Atherosclerosis Risk In Communities (ARIC) Study, Cardiovascular Health Study (CHS), the Eurostroke Project, nor Framingham study found an association between cholesterol and stroke risk.5–9 Sex, ethnicity, and race (but not region) have also been studied in The REasons for Geographic And Racial Differences in Stroke (REGARDS) and suggest that stroke is more prevalent in men, African Americans and some Latino Americans, but that the higher prevalence of risk factors in these latter groups only explains some of the excess risk.10 However, most of these studies have relatively few African Americans, and many were confounded by race and region (e.g. all African Americans being from one site). Recently, the Copenhagen City Heart Study reported that in women and to some extent men, stepwise increased levels of non-fasting triglycerides were associated with increasing risk of ischemic stroke, while increasing levels of cholesterol were not.11 Thus, we assessed if there are geographic, racial, and ethnic differences in TC, low density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol (HDL-C) and triglyceride levels measured at baseline from participants in REGARDS study and evaluated their association with incident stroke.
METHODS
Study Population
The REGARDS study is a national, population-based, longitudinal cohort study with oversampling of African Americans (AAs) and persons living in the Stroke Belt region of the United States. Between January 2003 and October 2007, 30,239 individuals were enrolled, including race groups (42% AA, 58% white), and both sexes (45% men). The sample includes 21% of participants from the Stroke Belt Buckle (coastal plain region of North Carolina, South Carolina, and Georgia), 35% from the Stroke Belt states (remainder of North Carolina, South Carolina, and Georgia, plus Alabama, Mississippi, Tennessee, Arkansas, and Louisiana), and the remaining 44% from the other 40 contiguous states (referred to as non-Belt). REGARDS participants were selected from commercially available lists (Genesys). A letter and brochure informed participants of the study and a follow-up phone call introduced the study and solicited participation. During that call, verbal consent was obtained and a 45-minute questionnaire was administered. The verbal consent included agreement to participate in a subsequent in-person examination. The telephone response rate was 33% and the cooperation rate was 49% (similar to other reported epidemiologic studies).12 Demographic information and medical history, including a history of cardiovascular disease (CVD) and risk factors, was obtained by trained interviewers using a computer assisted telephone interview (CATI). Participants were considered to be enrolled in the study if they completed a 45-minute telephone questionnaire and an in-person physical examination. The exam included anthropometric and blood pressure (BP) measurements, blood samples, and an electrocardiogram conducted 3–4 weeks after the telephone interview. Written consent was obtained during the in-person visit. Participants or their proxies were contacted by telephone at 6-month intervals for identification of medical events.
Medical records were obtained for suspected strokes, and were reviewed by at least 2 physician members of a committee of stroke experts. Stroke events were defined following World Health Organization (WHO) definition, and further classified as ischemic or hemorrhagic. Incident stroke was defined as the first occurrence of physician-adjudicated stroke. The study methods were reviewed and approved by all involved Institutional Review Boards (IRB). Additional methodological details are provided elsewhere.13An in-home examination was conducted on REGARDS cohort members by qualified medical personnel. During this examination, fasting blood samples were taken in addition to other measurements.
Main Exposure
Baseline levels of LDL-C, HCL-C, TC, Non-HDL-C (Total - HDL-C) and triglycerides.
Endpoints
For the primary analysis in order to reduce confounding by indication (statins) we included all REGARDS participants free of prevalent stroke at baseline. The primary dependent variable was all strokes, but these were then subdivided into ischemic and hemorrhagic stroke.
Additional covariates
Demographic factors included age (defined in 10-year strata starting with age 45), race, region (Belt, Buckle, or non-Belt) and gender. Measures of socio-economic status included annual household income and education (defined in strata, see Table 1). Stroke risk factors included diabetes (fasting glucose ≥126 mg/dL (≥ 7 mmol/L) or non-fasting glucose >200 mg/dL (≥ 11.1 mmol/L) or self-reported use of diabetes medications), self-reported hypertensive medication use, self-reported use of lipid lowering medication, baseline systolic blood pressure (SBP), baseline smoking status (current, past, or never), history of atrial fibrillation (AF), left ventricular hypertrophy (LVH), and history of heart disease (self-reported event or evidence in ECG). SBP was the average of two measurements using a standard technique. LVH was defined as meeting Sokolow-Lyon LVH limb lead criteria. History of AF was by self-report or ECG evidence from record review.
Table 1.
Demographic and Clinical Characteristics of Subjects at Baseline Examination According to Quartiles of Total Cholesterol (mg/dl).
| Overall | Q1 (TC<164) |
Q2 (164<TC<189) |
Q3 (189<TC<215) |
Q4 (TC>215) |
|
|---|---|---|---|---|---|
| Participants/events | 23867/1031 | 5977/296 | 6098/250 | 5883/250 | 5909/235 |
| TC mg/dl, mean (SD) |
191.5 (39.0) | ||||
| LDL-C mg/dl, mean (SD)** |
114.1 (34.5) | 77.4 (16.6) | 102.1 (14.8) | 121.7 (16.0) | 155.8 (27.3) |
| HDL-C mg/dl, mean (SD)** |
52.2 (16.2) | 45.3 (12.9) | 51.1 (14.6) | 54.8 (16.4) | 58.0 (17.7) |
| Triglycerides mg/dl, mean (SD)** |
126.0 (63.8) | 111.9 (56.4) | 120.5 (60.0) | 127.3 (64.1) | 144.6 (69.7) |
| Non-HDL-C mg/dl, mean (SD)** |
139.2 (37.4) | 99.8 (17.3) | 126.2 (15.8) | 147.1 (17.6) | 184.8 (29.9) |
| Age in years, n (%)** |
64.7 (9.4) | 66.0 (9.6) | 64.9 (9.5) | 64.3 (9.3) | 63.6 (8.9) |
| Follow-up time (years), n (%)** |
7.5 (2.9) | 7.3 (3.0) | 7.6 (2.9) | 7.0 (2.6) | 7.5 (2.9) |
| Black, n (%)* | 9541 (40.0) | 2290 (38.3) | 2388 (39.2) | 2405 (40.9) | 2458 (41.6) |
| Male, n (%)* | 10726 (44.9) |
3621 (60.6) | 2894 (47.5) | 2359 (40.1) | 1852 (31.3) |
| Region, n (%) | |||||
| Belt | 8258 (34.6) | 2094 (35.0) | 2139 (35.1) | 2026 (34.4) | 1999 (33.8) |
| Buckle | 5060 (21.2) | 1329 (22.2) | 1264 (20.7) | 1237 (21.0) | 1230 (20.8) |
| Non-Belt | 10549 (44.2) |
2554 (42.8) | 2695 (44.2) | 2620 (44.5) | 2680(45.4) |
| Income, n (%)* | |||||
| <$20k | 3964 (16.6) | 959 (16.0) | 976 (16.0) | 990 (16.8) | 1039 (17.6) |
| $20k–$35k | 5721 (24.0) | 1468 (24.6) | 1436 (23.6) | 1344 (22.9) | 1473 (24.9) |
| $35k–$74k | 7413 (31.1) | 1901 (31.8) | 1948 (31.9) | 1853 (31.5) | 1711 (29.0) |
| $75k + | 4001 (16.8) | 996 (16.7) | 1043 (17.1) | 1004 (17.1) | 958 (16.2) |
| Refused | 2768 (11.6) | 653 (10.9) | 695 (11.4) | 692 (11.8) | 728 (12.3) |
| Education, n (%)* | |||||
| Less than HS | 2714 (11.4) | 770 (12.9) | 635 (10.4) | 656 (11.2) | 653 (11.1) |
| HS | 6131 (25.7) | 1537 (25.7) | 1511 (24.8) | 1460 (24.8) | 1623 (27.5) |
| Some College | 6397 (26.8) | 1515 (25.4) | 1644 (27.0) | 1609 (27.4) | 1629 (27.6) |
| College Grad and above |
8625 (36.1) | 2155 (36.1) | 2308 (37.9) | 2158 (36.7) | 2004 (33.9) |
| SBP** mmHg, mean (SD) |
127.1 (16.4) | 126.8 (16.1) | 127.0 (16.2) | 126.8 (16.6) | 127.6 (16.9) |
| Smoking, n (%)* | |||||
| Current | 3310 (13.9) | 842 (14.1) | 762 (12.5) | 794 (13.5) | 912 (15.4) |
| Never | 10981 (46.0) |
2496 (41.8) | 2846 (46.7) | 2811 (47.8) | 2828 (47.9) |
| Past | 9576 (40.1) | 2639 (44.2) | 2490 (40.8) | 2278 (38.7) | 2169 (36.7) |
| Hypertensive Meds, n (%)* |
12300 (51.5) |
3606 (60.3) | 3225 (52.9) | 2841 (48.3) | 2628 (44.5) |
| Lipid Lowering Meds, n (%)* |
7796 (32.7) | 2957 (49.5) | 2150 (35.3) | 1532 (26.0) | 1157 (19.6) |
| Atrial Fibrillation, n (%)* |
1936 (8.1) | 662 (11.1) | 476 (7.8) | 417 (7.1) | 381 (6.5) |
| Diabetes, n (%)* | 4727 (19.8) | 1813 (30.3) | 1233 (20.2) | 920 (15.6) | 761 (12.9) |
| LVH, n (%) | 2301 (9.6) | 564 (9.4) | 590 (9.7) | 546 (9.3) | 601 (10.2) |
| Heart Disease, n (%)* |
3899 (16.3) | 1665 (27.9) | 976 (16.0) | 692 (11.8) | 566 (9.6) |
Significant at the .05 level, Chi-Square test
Significant at the .05 level, ANOVA F-test
SD = standard deviation; LDL-C = low density lipoprotein cholesterol; HDL-C=high density lipoprotein cholesterol; HS=high school; SBP=systolic blood pressure; LVH=left ventricular hypertrophy
Statistical Analysis
Baseline characteristics were calculated for the population based on quartiles of total cholesterol. ANOVA F-tests and χ2 tests were used to test differences between quartiles as appropriate. Alternate LDL-C, HDL-C, TC, non-HDL-C, and triglyceride variables were created by dividing by the standard deviation.
Cox Proportional-Hazard models were the main analytical tool used to examine the association between incident stroke and lipids. Follow-up time was calculated as the difference between last follow-up date (or confirmed stroke date) and in home date. For each adjusted lipid measure (LDL-C, HDL-C, triglycerides, TC, and non-HDL-C) we calculated a series of incremental models. The initial model is unadjusted, while model 2 adjusts for age, race, age*race interaction, gender, education, geographic region, and income; and model 3 adds adjustments for SBP, hypertensive medication use, lipid lowering medication use, smoking, AF, LVH, diabetes, and a self-reported history of heart disease. The proportional hazards assumption was tested by including the interaction of the corresponding lipid measure and log-transformed follow-up time in the final multivariable Cox models. SAS 9.3 (The SAS Institute, Cary, NC) was used for all models and calculations.
Multiple imputation for suspected stroke events that could not be adjudicated because of inability to retrieve records and for records currently in the adjudication process (approximately 10% of suspected stroke events for each) was used to reduce potential bias, with details of this approach described elsewhere.14
RESULTS
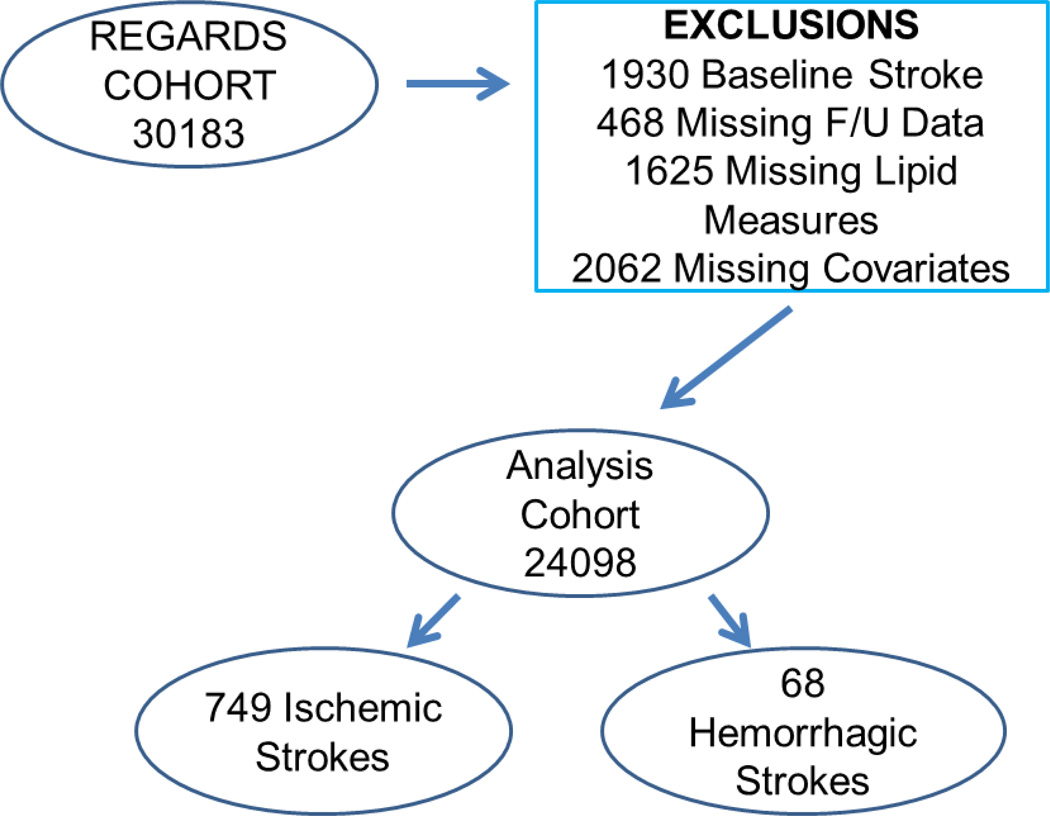
The total REGARDS sample consisted of 30,239 subjects, 30,183 after 56 with data anomalies were excluded. For the primary analysis 1,930 subjects with history of stroke at baseline, 464 with missing follow-up data, 1,625 missing lipid measures and 2,297 with missing covariate data were excluded. As seen in Figure 1, this left an analysis cohort of 23,867 with a mean follow-up time of 6.9 +/− 2.6 years. There were 1031 centrally adjudicated strokes (874 ischemic and 77 hemorrhagic strokes). Table 1 lists the baseline demographic and clinical features of the sample population by quartiles of total cholesterol. Table 2 presents the hazard ratios (HRs) (unadjusted and with modeling) for all strokes, ischemic strokes and hemorrhagic strokes, for the different lipid measurements (LDL-C, HDL-C, triglycerides, TC, and non-HDL-C). In the unadjusted model, HDL-C baseline level was associated with 13% reduction (HR 0.87, 95% confidence interval [CI]: 0.81–0.93; p<0.05; 14% risk reduction for ischemic strokes and 16% for hemorrhagic strokes, respectively), and TC with 8% (HR 0.92, 95%CI: 0.87–0.99; p<0.05) risk reduction of all strokes. When the results were adjusted (model 3) the significant association was observed only for LDL-C and non-HDL-C with increase the risk of ischemic strokes by 8% and 10% respectively (HR 1.07, 95%Cl: 1.01–1.16, and HR 1.10, 95%CI: 1.03–1.18, respectively; p<0.05 for both).
Figure 1.
Exclusionary Cascade
Table 2.
Unadjusted and Adjusted HRs (95 CI) per Standard Deviation of Lipid Measurements
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| All Stroke (1031 events) | |||
| LDL-C | 0.95 (0.89–1.02) | 1.01 (0.95–1.08) | 1.06 (0.99–1.13) |
| HDL-C | 0.87 (0.81–0.93)Ɨ | 0.91 (0.84–0.98)Ɨ | 0.97 (0.90–1.04) |
| Triglycerides | 1.07 (1.01–1.13) | 1.09 (1.02–1.16)Ɨ | 1.02 (0.96–1.09) |
| Total Cholesterol | 0.92 (0.87–0.99)Ɨ | 1.00 (0.94–1.07) | 1.06 (0.99–1.13) |
| NonHDL-C* | 0.98 (0.92–1.04) | 1.04 (0.97–1.11) | 1.07 (1.01–1.15) |
| Ischemic Stroke (874 events) | |||
| LDL-C | 0.96 (0.90–1.03) | 1.02 (0.95–1.10) | 1.08 (1.01–1.16)Ɨ |
| HDL-C | 0.86 (0.79–0.92)Ɨ | 0.89 (0.82–0.96)Ɨ | 0.95 (0.87–1.03) |
| Triglycerides | 1.10 (1.03–1.18)Ɨ | 1.12 (1.04–1.20)Ɨ | 1.05 (0.98–1.14) |
| Total Cholesterol | 0.94 (0.87–1.01) | 1.01 (0.94–1.09) | 1.08 (1.00–1.17) |
| NonHDL-C* | 1.00 (0.93–1.07) | 1.06 (0.99–1.14) | 1.10 (1.03–1.18)Ɨ |
| Hemorrhagic Stroke (77 events) | |||
| LDL-C | 0.91 (0.69–1.18) | 1.01 (0.77–1.32) | 1.02 (0.75–1.39) |
| HDL-C | 0.84 (0.65–1.09) | 1.05 (0.80–1.37) | 1.09 (0.83–1.43) |
| Trigylcerides | 0.84 (0.64–1.10) | 0.80 (0.60–1.07) | 0.76 (0.57–1.01) |
| Total Cholesterol | 0.81 (0.62–1.06) | 0.97 (0.73–1.27) | 0.99 (0.72–1.34) |
| NonHDL-C* | 0.86 (0.66–1.13) | 0.95 (0.72–1.24) | 0.95 (0.71–1.28) |
Non HDL-C = total cholesterol – HDL
Significant at the .05 level
Model 1: Unadjusted
Model 2: Adjusted for age, race, age*race, gender, education, region, and income
Model 3: Model 2 and addition adjustment for SBP, hypertensive medication use, lipid lowering medication use, smoking, atrial fibrillation, left ventricular hypertrophy, history of heart disease, and diabetes
Abbreviations same as Table 1
Discussion
In this analysis of the REGARDS Study we found that LDL-C/non-HDL-C baseline values might be associated with an increased risk increase of ischemic strokes, 8% and 10% respectively, while triglycerides were associated with a nonsignificant 24% risk reduction of hemorrhagic strokes. Both of these associations were not significant in the model adjusting for demographic and socioeconomic factors (model 2), but became apparent only after adjustment for other major cerebrovascular risk factors. This “negative confounding” unmasked an association of LDL-C and non-HDL-C with ischemic stroke risk. This result is the product of (negative) associations of these lipid measures with some of the cerebrovascular risk factors.
The association between cholesterol levels and stroke occurrence is debated in the literature. In the Framingham cohort no association was found between the levels of cholesterol and the incidence of stroke.9 Nonetheless, in young women, a positive correlation between TC levels and stroke-related mortality was observed, while in subjects in 6th and 7th decade of life, an inverse correlation between these parameters was found.15 A combined analysis of cohort trials showed no significant association between the increased level of serum cholesterol and stroke rate, except for patients younger than 45 years.16 The reasons for not finding the clear-cut relationship between cholesterol level and stroke occurrence may be multiple. Firstly, longitudinal cohort studies were predestined to evaluate the role of cholesterol in coronary atherosclerosis, but not in stroke.16 Therefore, by selecting middle-aged subjects for cardiac studies, the older subjects, who were more susceptible to cerebral infarction, were undoubtedly lost. Moreover, analysis of the occurrence of stroke subtypes and differentiation between cholesterol components was not done. Additionally, the prophylactic treatment used might also influence the incidence of stroke.
Hypercholesterolemia might promote atherosclerosis, because elevated concentrations of oxidized or modified LDL cholesterol contribute to endothelial dysfunction.17 The association between hypercholesterolemia and stroke has become more apparent because of data from prospective cohort studies that show higher risks of ischemic stroke with increasing levels of total cholesterol in both men and women.17,18 Increased HDL cholesterol levels have a protective effect against the occurrence of ischemic stroke, but the association between LDL cholesterol and stroke is less clear.19,20 Elevated triglyceride levels have also been reported as a risk factor for stroke.21–24 Moreover, the high prevalence of this condition in the population translates into a larger proportion of strokes potentially attributable to dyslipidemia and, therefore, a greater relative importance in public health.12 Most, but not all, epidemiological studies find an association between higher cholesterol levels and an increased risk of ischemic stroke. In the MRFIT trial, which included almost 320.000 men, the relative risk of death from non-hemorrhagic stroke increased progressively for each level of cholesterol.25 In the Alpha-Tocopherol, Beta-Carotene Cancer Prevention (ATBC) study, which included 28.000 men who smoked, the risk of cerebral infarction was increased among those with TC levels over7 mmol/L (271 mg/dL).26 In the Asia Pacific Cohort Studies Collaboration (APCSC), which included 352.033 persons, there was a 25% increase (95%CI, 13 to 40%) in ischemic stroke rates for every 1 mmol/L (38.7 mg/dL) increase in total cholesterol.5 In the Women’s Pooling Project, which included 24.343 US women 55 years of age with no previous CVD, and in the Women’s Health Study (WHS), a prospective cohort study of 27.937 US women over 45 years of age, higher cholesterol levels were also associated with increased risk of ischemic stroke.27 In other studies the association between cholesterol and stroke risk was not as clear. In the ARIC study, which included 14.175 middle-aged men and women free of clinical CVD, the relationships between lipid values and incident ischemic stroke were weak,6 and in the Eurostroke Project of 22.183 men and women, there was no relationship between cholesterol and cerebral infarction.84 Interpretation of studies evaluating the relationship between cholesterol levels and risk of ischemic stroke may be confounded by the types of ischemic stroke included in the analysis.
Most, but not all, epidemiological studies show an inverse relationship between HDL cholesterol and stroke. HDL-C was inversely related to ischemic strokes in the Copenhagen City Heart Study,11 the Oyabe Study of Japanese men and women,28 middle-aged British men,29 and middle-aged and elderly men in the Israeli Ischemic Heart Disease Study.19 In the Northern Manhattan Stroke Study (NOMASS) that involved a multiethnic community, higher HDL-C levels were also associated with reduced risk of ischemic stroke.20 In the CHS study, high HDL-C was associated with a decreased risk of ischemic stroke in men but not women,7 and the ARIC Study did not find a significant relationship between HDL cholesterol and ischemic stroke6. Five prospective cohort studies included in a systematic review found a decreased risk of stroke ranging from 11% to 15% for each 10 mg/dL increase in HDL cholesterol.03 The results of epidemiological studies that have evaluated the relationship between triglycerides and ischemic stroke are inconsistent, in part because some have used fasting levels and others non-fasting levels. Fasting triglyceride levels were not associated with ischemic stroke in the ARIC study6. Triglycerides did not predict the risk of ischemic stroke among healthy men enrolled in the Physicians’ Health Study.314 Similarly, in the Oslo study of healthy men, triglycerides were not related to the risk of stroke17 In contrast, a meta-analysis of prospective studies conducted in the Asia-Pacific region found a 50% increased risk of ischemic stroke among those in the highest quintile of fasting triglycerides compared with those in the lowest quintile.22 The Copenhagen City Heart Study, a prospective, population based cohort study composed of approximately 14.000 persons, found that elevated non-fasting triglyceride levels increased the risk of ischemic stroke in both men and women. After multivariate adjustment, there was a 15% increased risk (95% CI, 9 to 22%) of ischemic stroke for each 89 mg/dL increase in non-fasting triglycerides. The hazard ratios for ischemic stroke among men and women with the highest compared with the lowest non-fasting triglycerides were 2.5 (95%CI, 1.3 to 4.8) and 3.8 (95%CI, 1.3 to 11), respectively.11 The 10-year risks of ischemic stroke were 16.7% and 12.2%, respectively, in men and women aged 55 years with triglyceride levels >443 mg/dL11. Similarly, the WHS found that in models adjusted for TC and HDL-C and measures of insulin resistance, non-fasting triglycerides, but not fasting triglycerides, were associated were associated with CV events, including ischemic stroke.24
Nutraceuticals and functional food ingredients that are beneficial to vascular health may represent useful compounds that are able to reduce the overall cardiovascular risk induced by dyslipidaemia by acting parallel to statins or as adjuvants in case of failure or in situations where statins cannot be used. The mechanisms underlying such actions are not fully understood but may be related to reducing 7α-hydroxylase, increasing faecal excretion of cholesterol, decreasing 3-hydroxy-3-methylglutaryl-CoA reductase mRNA levels or reducing the secretion of very low-density lipoprotein32,33
Our study has some strengths limitations. The main strengths are the proven track record of the REGARDS study and the size and racial, ethnic and regional distribution of the study participants. Also, in home pill bottle assessments were made and however, typical for observational studies, smoking status, education level, income, and a history of heart disease were ascertained by self-report, and currently only baseline measures are available, and therefore changes over time cannot be assessed. Due to participant time constraints not all measures could be fully explored such as limiting the telephone questionnaire to 45 minutes.
In conclusion, in a disease free population, LDL-C and non-HDL-C baseline levels are significantly associated with the risk of ischemic stroke.
Acknowledgments
Study funding: This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health.
Representatives of National Institute of Neurological Disorders and Stroke or the National Institutes of Health have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authors contributions to this manuscript:
Stephen P. Glasser, MD,
Aleena Mosher, MS,
Maciej Banach, MD,
George Howard, DrPH,
Dr. Stephen P. Glasser, Dr. Maciej Banach, Dr. George Howard, and Aleena Mosher report no disclosures.
Contributor Information
Stephen P. Glasser, Department of Preventive Medicine, University of Alabama at Birmingham, Birmingham, AL, USA, sglasser@uabmc.edu.
Aleena Mosher, Department of Biostatistics, University of Alabama at Birmingham, Birmingham, AL, USA, amosher@uab.edu.
Maciej Banach, Department of Hypertension, Medical University of Lodz, Lodz, Poland, maciejbanach@aol.co.uk.
George Howard, Department of Biostatistics, University of Alabama at Birmingham, Birmingham, AL, USA, ghoward@uab.edu.
BIBLIOGRAPHY
- 1.Kochanek KD, Murphy SL, Xu J, Arias E. Mortality in the United States, 2013. NCHS data brief. 2014:1–8. [PubMed] [Google Scholar]
- 2.Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: A guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42:517–584. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 3.Zhang X, Patel A, Horibe H, Wu Z, Barzi F, Rodgers A, et al. Cholesterol, coronary heart disease, and stroke in the asia pacific region. Int J Epidemiol. 2003;32:563–572. doi: 10.1093/ije/dyg106. [DOI] [PubMed] [Google Scholar]
- 4.Ohira T, Schreiner PJ, Morrisett JD, Chambless LE, Rosamond WD, Folsom AR. Lipoprotein(a) and incident ischemic stroke: The atherosclerosis risk in communities (aric) study. Stroke. 2006;37:1407–1412. doi: 10.1161/01.STR.0000222666.21482.b6. [DOI] [PubMed] [Google Scholar]
- 5.Grobbee DE, Koudstaal PJ, Bots ML, Amaducci LA, Elwood PC, Ferro J, et al. Incidence and risk factors of ischaemic and haemorrhagic stroke in europe. Eurostroke: A collaborative study among research centres in europe: Rationale and design. Neuroepidemiology. 1996;15:291–300. doi: 10.1159/000109919. [DOI] [PubMed] [Google Scholar]
- 6.Psaty BM, Anderson M, Kronmal RA, Tracy RP, Orchard T, Fried LP, et al. The association between lipid levels and the risks of incident myocardial infarction, stroke, and total mortality: The Cardiovascular Health Study. J Am Geriatr Soc. 2004;52:1639–1647. doi: 10.1111/j.1532-5415.2004.52455.x. [DOI] [PubMed] [Google Scholar]
- 7.Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, et al. Traditional risk factors as the underlying cause of racial disparities in stroke: Lessons from the half-full (empty?) glass. Stroke. 2011;42:3369–3375. doi: 10.1161/STROKEAHA.111.625277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lindenstrom E, Boysen G, Nyboe J. Influence of total cholesterol, high density lipoprotein cholesterol, and triglycerides on risk of cerebrovascular disease: The Copenhagen City Heart Study. BMJ. 1994;309:11–15. doi: 10.1136/bmj.309.6946.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17:643–653. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 10.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 11.Howard G, McClure LA, Moy CS, Safford MM, Cushman M, Judd SE, et al. Imputation of incident events in longitudinal cohort studies. Am J Epidemiol. 2011;174:718–726. doi: 10.1093/aje/kwr155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kissela BM, Khoury JC, Alwell K, Moomaw CJ, Woo D, Adeoye O, et al. Age at stroke: Temporal trends in stroke incidence in a large, biracial population. Neurology. 2012;79:1781–1787. doi: 10.1212/WNL.0b013e318270401d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: A report from the American Heart Association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 14.Haheim LL, Holme I, Hjermann I, Leren P, Tonstad S. Trends in the incidence of acute myocardial infarction and stroke: A 21-year follow-up of the oslo study. Scand Cardiovasc J. 2004;38:216–221. doi: 10.1080/14017430410014910. [DOI] [PubMed] [Google Scholar]
- 15.Bowman TS, Sesso HD, Ma J, Kurth T, Kase CS, Stampfer MJ, et al. Cholesterol and the risk of ischemic stroke. Stroke. 2003;34:2930–2934. doi: 10.1161/01.STR.0000102171.91292.DC. [DOI] [PubMed] [Google Scholar]
- 16.Tanne D, Yaari S, Goldbourt U. High-density lipoprotein cholesterol and risk of ischemic stroke mortality. A 21-year follow-up of 8586 men from the Israeli Ischemic Heart Disease Study. Stroke. 1997;28:83–87. doi: 10.1161/01.str.28.1.83. [DOI] [PubMed] [Google Scholar]
- 17.Sacco RL, Benson RT, Kargman DE, Boden-Albala B, Tuck C, Lin IF, et al. High-density lipoprotein cholesterol and ischemic stroke in the elderly: The Northern Manhattan Stroke Study. JAMA. 2001;285:2729–2735. doi: 10.1001/jama.285.21.2729. [DOI] [PubMed] [Google Scholar]
- 18.Patel A, Barzi F, Jamrozik K, Lam TH, Ueshima H, Whitlock G, et al. Serum triglycerides as a risk factor for cardiovascular diseases in the asia-pacific region. Circulation. 2004;110:2678–2686. doi: 10.1161/01.CIR.0000145615.33955.83. [DOI] [PubMed] [Google Scholar]
- 19.Freiberg JJ, Tybjaerg-Hansen A, Jensen JS, Nordestgaard BG. Nonfasting triglycerides and risk of ischemic stroke in the general population. JAMA. 2008;300:2142–2152. doi: 10.1001/jama.2008.621. [DOI] [PubMed] [Google Scholar]
- 20.Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA. 2007;298:299–308. doi: 10.1001/jama.298.3.299. [DOI] [PubMed] [Google Scholar]
- 21.Bansal S, Buring JE, Rifai N, Mora S, Sacks FM, Ridker PM. Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA. 2007;298:309–316. doi: 10.1001/jama.298.3.309. [DOI] [PubMed] [Google Scholar]
- 22.Stamler J, Neaton JD, Cohen JD, Cutler J, Eberly L, Grandits G, et al. Multiple risk factor intervention trial revisited: A new perspective based on nonfatal and fatal composite endpoints, coronary and cardiovascular, during the trial. J Am Heart Assoc. 2012;1:e003640. doi: 10.1161/JAHA.112.003640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Albanes D, Heinonen OP, Taylor PR, Virtamo J, Edwards BK, Rautalahti M, et al. Alpha-tocopherol and beta-carotene supplements and lung cancer incidence in the alpha-tocopherol, beta-carotene cancer prevention study: Effects of base-line characteristics and study compliance. J Natl Cancer Inst. 1996;88:1560–1570. doi: 10.1093/jnci/88.21.1560. [DOI] [PubMed] [Google Scholar]
- 24.Kurth T, Everett BM, Buring JE, Kase CS, Ridker PM, Gaziano JM. Lipid levels and the risk of ischemic stroke in women. Neurology. 2007;68:556–562. doi: 10.1212/01.wnl.0000254472.41810.0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soyama Y, Miura K, Morikawa Y, Nishijo M, Nakanishi Y, Naruse Y, et al. High-density lipoprotein cholesterol and risk of stroke in Japanese men and women: The Oyabe Study. Stroke. 2003;34:863–868. doi: 10.1161/01.STR.0000060869.34009.38. [DOI] [PubMed] [Google Scholar]
- 26.Shaper AG, Phillips AN, Pocock SP, Walker M, Macfarlane PW. Risk factors for stroke in middle aged British men. BMJ. 1991;302:1111–1115. doi: 10.1136/bmj.302.6785.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laird EA, Coates V, Chaney D. Systematic review of descriptive cohort studies on the dynamics of glycaemia among adults admitted to hospital with acute stroke. J Adv Nurs. 2013;69:500–513. doi: 10.1111/j.1365-2648.2012.06094.x. [DOI] [PubMed] [Google Scholar]
- 28.Scicchitano P, Cameli M, Maiello M, Amedeo Modesti P, Muiesan ML, Novo S, Palmiero, Pier Sergio Saba P, Pedrinelli R, Ciccone MM. Nutraceuticals and dyslipidaemia: Beyond the common therapeutics. Journal of Functional Foods. 2014;6:11–13. [Google Scholar]
- 29.Serban MC, Sahebkar A, Dragan S, Stoichescu-Hogea G, Ursoniu S, Andrica F, Banach M. A systematic review and meta-analysis of the impact of Spirulina supplementation on plasma lipid concentrations. Clin Nutr. 2015 Sep 25; doi: 10.1016/j.clnu.2015.09.007. pii: S0261-5614(15)00240-X. [DOI] [PubMed] [Google Scholar]