Abstract
Dental trauma to the permanent dentition can lead to clinical complications and its management may considerably challenge a practitioner. The incidence of pulp canal obliteration following dental trauma has been reported to be approximately 4 – 24%. Attempting to locate canals following calcific metamorphosis and negotiating it to full working length may lead to iatrogenic errors such as fractured instrument and perforation. This review article describes the possible etiology of Calcific Metamorphosis, its clinical and radiographic features as well as its management.
Keywords: calcific metamorphosis, pulp canal obliteration, dental trauma, endodontics
Introduction
Dental trauma to the permanent dentition can lead to clinical complications and its management may considerably challenge a practitioner. One such complication is Calcific Metamorphosis (CM) which can complicate entry in to the root canal system in the future due to difficulty in locating the canal and gaining access. This condition is also known as Pulp Canal Obliteration, Dystrophic Calcification, Diffuse Calcification and Calcific Degeneration. (1) Other causes of CM can be dentinal dysplasia and dentinogenesis imperfecta, mainly type 2 (2) and teeth which have been rigidly splinted. (3) Calcific Metamorphosis is defined by the American Association of Endodontists (4) as “A pulpal response to trauma characterized by rapid deposition of hard tissue within the canal space.”
Methodology
A literature review was conducted to identify the possible causes of calcific metamorphosis along with its clinical and radiographic features as well as its management. Search engine used were Google Scholar and Pubmed. Statements used to search for relevant publications were “calcific metamorphosis”, “calcific metamorphosis endodontics”, “pulp canal obliteration”, and “dental trauma”. Review articles, original studies and case reports were included in this review.
Mechanism of calcification
This is more often observed in patients who have suffered concussion or subluxation injuries. (5) Robertson et al. (6) found this obliteration to be either, dentine like, bone like or fibrotic in primary teeth. Holan (7) observed tube-like structures with histological appearance of osteodentine with cellular inclusions in primary teeth. Lundberg and Cvek (8) evaluated permanent maxillary incisors and found that the tissue changes were characterized by increase in collagen content and a marked decrease in the number of cells. They too found osteoid tissue with cellular inclusions adjacent to mineralized areas in pulp. The rate of deposition is uncontrolled (9) and could be as high as 3.5 μm per day. (10) CM is not the same as pulp stones. True pulp stones are made of dentine which is lined by odontoblasts, whereas false pulp stones are formed by mineralization of pulp cells that have degenerated. (11) CM is initiated by stimulation of odontoblastic activity. (12) The mechanism of CM is not known but may be due to injury to the neurovascular supply of the pulp. (13) Another theory suggests that the bleeding in the canal and blood clot could be a focal point for calcification in case the pulp remains vital following trauma. (3) Hence, traumatic injury to the apical blood vessels, which may not be sufficient to cause pulpal necrosis and the pulp remains vital, could lead to CM. (2, 14, 15)
Radiographic features
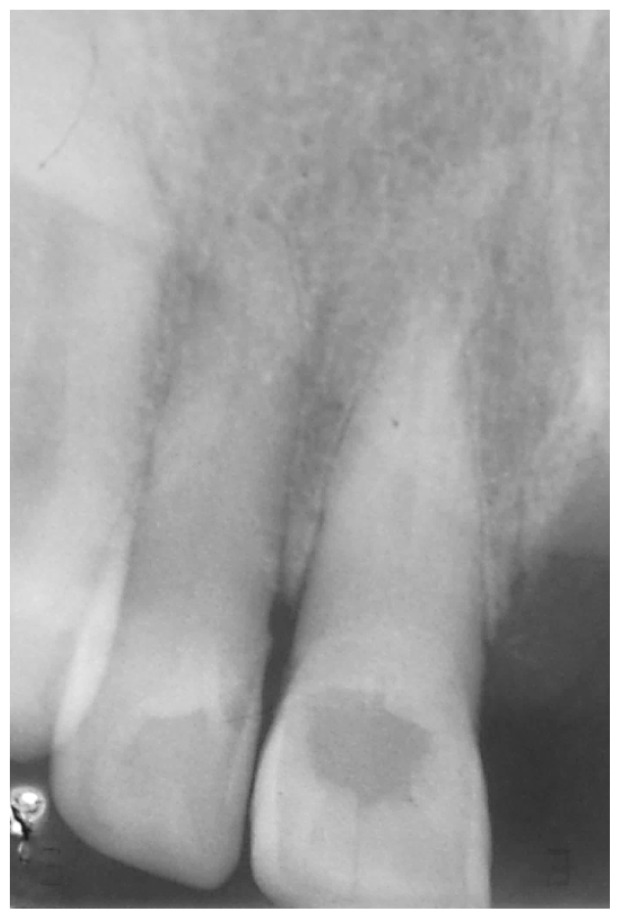
A radiograph usually reveals obliteration of pulp space with absence of the pulp chamber (Figure 1). Unless there is evidence of apical involvement of bone, the lamina dura will be intact with no widening of the periodontal membrane space.
Figure 1.
Periapical radiograph of upper right central incisor revealing absence of a chamber and obliteration of the canal in the coronal 1/3 of the root. However, the canal is visible from mid-root to the apical region. This patient gave a history of trauma to the front of his face.
Radiographically, CM can be classified (1) as either:
Partial Obliteration – the pulp chamber is not visible and the canal is markedly narrowed but visible
Total Obliteration – the pulp chamber and canal is hardly or not visible
Literature suggests that a narrow canal is always present irrespective of its identification on the radiograph. (10, 16, 17)
Clinical presentation
CM is generally asymptomatic and clinically the patients present to the practitioner with yellow discoloration of the affected tooth crown. This discoloration is due to a greater thickness of dentine deposition. (16) It is worth noticing that not all teeth will undergo a color change. (18) CM is more common in the anterior teeth (16) and may be recognized as early as 3 months after injury although it may not be detected up to 1 year. (10, 19) The incidence of pulp canal obliteration following dental trauma has been reported to be approximately 4–24%. (18) Vital pulp testing may be unreliable (false negative) despite the presence of a vital pulp due to the increased thickness of dentine. (20, 21)
Management
Endodontic intervention in a tooth demonstrating pulp canal obliteration without symptoms or periapical pathosis is debatable. Follow up and continuous observation is recommended before deciding to intervene. (18) According to literature, the incidence of a calcified tooth developing pulpal pathology is in the range of 1 – 16%. (22, 23, 24) If the patient’s complaint is only discoloration, then a vital (external) bleaching technique can be an option. (18) However, if the discoloration is due to irregular reparative dentine formation, intentional endodontics may have to be performed to aid in non-vital (internal) bleaching. (16)
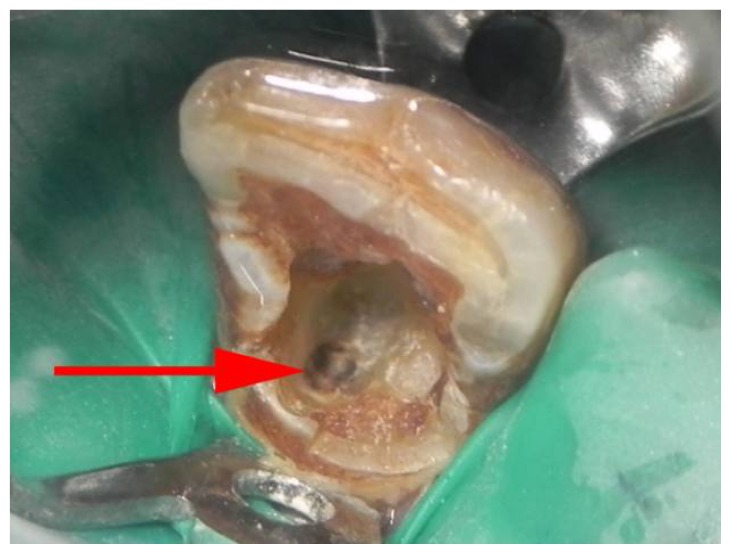
If root canal treatment is decided, a sound knowledge of the normal root canal anatomy and its possible variations is very important. It is quite helpful for the operator to prepare the access cavity before placing the rubber dam. This may help to evaluate the root relationships and work in the long axis of the tooth. (25) Once the canal is located, a rubber dam should be immediately placed and further treatment carried out. The access cavity should be of normal size and shape. (10) A change in color of dentine in the center of the root should indicate the position of the canal (Figure 2). An indicator such as methylene blue or the bubble test using sodium hypochlorite can be used to aid in visualizing the location of the calcified canal.
Figure 2.
Pigmentation evident on the floor (red arrow) after clearing the floor using a round low speed tungsten carbide bur
A DG-16 endodontic explorer (Hu-Friedy, Chicago, IL) is a very helpful tool in location and exploration of the canal. (20) To negotiate these canals, long-necked round drills (LN-drill, Dentsply Maillefer, Oklahoma, USA) may be used with gentle brushing strokes. The Mueller bur (Brasseler, Savannah, GA, USA) and ultrasonic tips are highly effective for this purpose (25) and has an added advantage over the burs that they maintain high cutting efficiency without rotation which enhances safety and control over the instrument whereby reducing the risks of mishaps such as perforation. Micro openers and debriders (Denstply, Maillefer, USA) can also be used to gain access in to calcified canals. They are specially designed to remove the fingers from the field of vision which greatly enhances operator efficiency when locating and accessing such canals under the microscope. Radiographs should be done repeatedly with the bur or ultrasonic tip in place to confirm the straight and centered access. Once the canal is negotiated, the use of a lubricant is advised along with #8 or #10 K-type file with a gentle watch winding motion with slight vertical pressure. (18) The “crown down technique” is highly recommended for canal preparation along with copious irrigation using 2.5 – 5.25% sodium hypochlorite. (19)
Fachin et al. (26) described the “Modified-Tip Instrument” technique for removal of hard pastes from the root canal during retreatment and suggested its use to gain length in extremely calcified canals. The tip of a K-type file (quadrangular section), #30 and #35, is cut by 4 mm using an orthodontic wire cutter producing a sharp edge at the new working end. Used with an apical pressure and reaming motion this file now becomes an efficient and potent cutting instrument. Similar technique has been reported by Siddiqui (27) and Kobayashi (28) also. Possible drawbacks of this technique could be:
Repeated radiographs to assess the progress and direction of the file;
Perforation if misdirected due to the files aggressiveness; and
Difficult to work in curved canals.
Surgical management can be an option if the canal cannot be located with the conventional approach. However, canal identification after root end resection can also be difficult since there is no sign for the clinician to mark the canal opening. (18) It is proposed that once the apex is resected, necrotic pulp pockets trapped during the calcification process may be exposed to the surrounding periapical tissues which could cause failure of treatment due to persistent chronic inflammation. (10) Hence surgery should only be considered once the conventional orthograde treatment has failed or the canal cannot be located.
It is worth noting that complete obliteration of the canal radiographically may not always suggest absence of a canal space. Kyun and Walton (17) measured the canal widths radiographically of 36 teeth and then measured and compared the widths of the same sample histologically. They found a canal space in all their samples in the histologic sections despite some teeth showing complete absence of canal space radiographically. Fischer (29) suggested root canal treatment in such cases due to the decrease in cellular content which in turn would lead to decreased ability of the pulp to heal making it more susceptible to infection. However, Lundberg and Cvek (8) found 1 out of 20 permanent teeth showing inflammatory cells and concluded that such conditions did not indicate endodontic treatment. The incidence of periapical pathology in such teeth has been reported to be between 1–16% only and hence it is advisable to manage such cases through routine follow ups and observation until signs and symptoms of infection is evident clinically and/or radiographically. Numerous case reports and reviews mention a set protocol for the management of CM. Root perforation, instrument fracture and root fracture due to excessive preparation to locate the canal are possible complications. (18) However, mishaps during treatment may be avoided by following the general guidelines:
Pulp chamber is always located in the center of the tooth at the level of the CEJ;(30)
Calcified pulp chamber is darker than the surrounding dentine; (30)
The file should be used parallel to the long axis of the root since the crown (specifically in the upper anteriors) are usually inclined and may misdirect the operator leading to early perforation.
Use of magnification with light; and
Repeated radiographs to assess the direction of the bur during location of canal as well as direction of file during negotiation within the root.
Conclusion
From the literature it seems that the time of endodontic intervention in a progressive calcifying pulp space is debatable. If a root canal procedure is planned, calcific metamorphosis can challenge the skills of practitioners, and early recognition of canal obliteration with the help of radiographs can save much frustrations. Owing to the low incidence of such teeth developing periapical pathosis, early intervention as a prophylactic measure may not be reasonable. (10, 15) Hence, prophylactic intervention, if planned, needs to be justified. Surgical intervention may be a possibility once other treatment modalities have failed. Given the difficulty in its management, it is advised to refer teeth showing signs of obliteration to an Endodontist who in conjunction with specialist training, magnification, proper equipment and detailed knowledge of dental anatomy, can manage such cases with minimal errors, hence providing a better prognosis.
References
- 1.Reis LC, Nascimento VDMA, Lenzi AR. Operative microscopy – indispensable resource for the treatment of pulp canal obliteration: a case report. Braz J Dent Traumatol. 2009;1(1):23–26. [Google Scholar]
- 2.Soames JV, Southam JC. Oral Pathology. 4th Ed. Oxford; 2008. [Google Scholar]
- 3.Cohen S, Hargreaves KM. Pathways of the Pulp. 10th Ed. St. Louis, Mo: Elsevier Mosby; 2011. [Google Scholar]
- 4.Glossary of Endodontic Terms. 8th Ed. American Association of Endodontics; 2012. [Google Scholar]
- 5.Oginni AO, Adekoya-Sofowora CA. Pulpal sequelae after trauma to anterior teeth among adult Nigerian dental patients. BMC Oral Health. 2007;7:11. doi: 10.1186/1472-6831-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robertson A, Lundgren T, Andreasen JO, Dietz W, Hoyer I, Noren JG. Pulp calcifications in traumatized primary incisors. A morphological and inductive analysis study. Eur J Oral Sci. 1997;105:196–206. doi: 10.1111/j.1600-0722.1997.tb00201.x. [DOI] [PubMed] [Google Scholar]
- 7.Holan G. Tube-like mmineralization n the dental pulp of traumatized primary incisors. Endod Dent Traumatol. 1998;14:279–284. doi: 10.1111/j.1600-9657.1998.tb00853.x. [DOI] [PubMed] [Google Scholar]
- 8.Lundberg M, Cvek M. A light microscopy study of pulps from traumatized permanent incisors with reduced pulpal lumen. Acta Odontol Scand. 1980;38:89–94. doi: 10.3109/00016358009003483. [DOI] [PubMed] [Google Scholar]
- 9.de Cunha FM, de Souza IM, Monnerat J. Pulp canal obliteration subsequent to trauma: perforation management with MTA followed by canal localization and obturation. Braz J Dent Traumatol. 2009;1(2):64–68. [Google Scholar]
- 10.Amir FA, Gutman JL, Witherspoon DE. Calcific metamorphosis: a challenge in endodontic diagnosis and treatment. Quintessence Int. 2001;32(6):447–55. [PubMed] [Google Scholar]
- 11.Goga R, Chandler NP, Oginni AO. Pulp stones: a review. Int Endod J. 2008;41:457–468. doi: 10.1111/j.1365-2591.2008.01374.x. [DOI] [PubMed] [Google Scholar]
- 12.Fonseca GM, Fonseca MM. Calcific metamorphosis with pathological root resorption in permanent teeth: morphohistometric evaluation of two cases. 2015;33(2):712–718. [Google Scholar]
- 13.Robertson A. A retrospective evaluation of patients with uncomplicated crown fractures and luxation injuries. Endod and Dent Traumatol. 1998;14:245–56. doi: 10.1111/j.1600-9657.1998.tb00848.x. [DOI] [PubMed] [Google Scholar]
- 14.Ajmera K, Mulay S. Multimodality esthetic management – a case report. Int J Sci Res. 2013;4(1):1176–80. [Google Scholar]
- 15.Moule AJ, Moule CA. The endodontic management of traumatized permanent anterior teeth: a review. Aust Dent J. 2007;52( 1 Suppl):S122–37. doi: 10.1111/j.1834-7819.2007.tb00520.x. [DOI] [PubMed] [Google Scholar]
- 16.Munley PJ, Goodell GG. Calcific metamorphosis. Clinical Update for Naval Postgraduate Dental School. 2005;27(4) [Google Scholar]
- 17.Kuyk JK, Walton RE. Comparison of the radiographic appearance of root canal size to its actual diameter. J Endod. 1990;16( 11):528–33. doi: 10.1016/S0099-2399(07)80215-9. [DOI] [PubMed] [Google Scholar]
- 18.McCabe PS, Dummer PMH. Pulp canal obliteration: an endodontic diagnosis and treatment challenge. Int Endod J. 2011;45:177–197. doi: 10.1111/j.1365-2591.2011.01963.x. [DOI] [PubMed] [Google Scholar]
- 19.Oginni AO, Adekoya-Sofowora, Kolawole KA. Evaluation of radiographs, clinical signs and symptoms associated with pulp canal obliteration: an aid to treatment decision. Dental Traumatol. 2009;25(6):620–5. doi: 10.1111/j.1600-9657.2009.00819.x. [DOI] [PubMed] [Google Scholar]
- 20.Malhotra N, Kundabala M. Calcific metamorphosis. Literature review and clinical strategies. Dent Update. 2013;39:48–60. doi: 10.12968/denu.2013.40.1.48. [DOI] [PubMed] [Google Scholar]
- 21.Schindler WG, Gullickson DC. Rationale for the management of calcific metamorphosis secondary to traumatic injuries. J Endod. 1988;14(8):408–12. doi: 10.1016/S0099-2399(88)80126-2. [DOI] [PubMed] [Google Scholar]
- 22.Stalhane I, Hedegard B. Traumatized permanent teeth in children aged 7–15 years. Part II. Swed Dent J. 1975;68:157–169. [PubMed] [Google Scholar]
- 23.Jacobsen I, Kerekes K. Long-term prognosis of traumatized permanent anterior teeth showing calcifying processes in the pulp cavity. Scand J Dent Res. 1977;85:588–598. doi: 10.1111/j.1600-0722.1977.tb02119.x. [DOI] [PubMed] [Google Scholar]
- 24.Andreasen F, Zhijie Y, Thomsen B, Andersen P. Occurrence of pulp canal obliteration after luxation injuries in the permanent dentition. Endod Dent Traumatol. 1987;3:103–115. doi: 10.1111/j.1600-9657.1987.tb00611.x. [DOI] [PubMed] [Google Scholar]
- 25.Vertucci FJ. Root canal morphology and its relationship to endodontic procedures. Endodontic Topics. 2005;10:3–29. [Google Scholar]
- 26.Fachin EV, Wenckus CS, Aun CE. Retreatment using a modified-tip instrument. J Endod. 1995;21(8):425–8. doi: 10.1016/S0099-2399(06)80830-7. [DOI] [PubMed] [Google Scholar]
- 27.Siddiqui SH. Management of Pulp Canal Obliteration using the Modified-Tip Instrument Technique: A case report. Int J Health Sci. 2014;8(4):427–428. [PMC free article] [PubMed] [Google Scholar]
- 28.Kobayashi C. Penetration of constricted canals with modified K files. J Endod. 1997;23( 6):391–393. doi: 10.1016/S0099-2399(97)80190-2. [DOI] [PubMed] [Google Scholar]
- 29.Fischer C. Hard tissue formation of the pulp in relation to treatment of traumatic injuries. Int Dent J. 1974;24:387–396. [PubMed] [Google Scholar]
- 30.Krasner P, Rankow HJ. Anatomy of the pulp chamber floor. J Endod. 2004;30:5–16. doi: 10.1097/00004770-200401000-00002. [DOI] [PubMed] [Google Scholar]