Abstract
Hamstring injuries are very common in athletes. Acute hamstring strains can occur with high-speed running or with excessive hamstring lengthening. Athletes with proximal hamstring tendinopathy often do not report a specific inciting event; instead they develop the pathology from chronic overuse. A thorough history and examination is important to determine the appropriate diagnosis and rule out other causes of posterior thigh pain. Conservative management of hamstring strains involves a rehabilitation protocol that gradually increases intensity, range of motion and progresses to sport-specific and neuromuscular control exercises. Eccentric strengthening exercises are used for management of proximal hamstring tendinopathy. Studies investigating corticosteroid and platelet-rich plasma injections have mixed results. MRI and ultrasound are effective for identification of hamstring strains and tendinopathy, but have not demonstrated correlation with return to play. The article focuses on diagnosis, treatment and return to play considerations for acute hamstring strains and proximal hamstring tendinopathy in the athlete.
Keywords: Hamstring injuries, hamstring strain, proximal hamstring tendinopathy, rehabilitation
INTRODUCTION
Hamstring injuries are one of the most common injuries in athletes.(4, 34, 42) Injuries can range from acute hamstring muscle strains and ruptures to chronic proximal hamstring tendinopathy. Acute hamstring strains are the most common muscle strain, have high rates of recurrence and can lead to prolonged absence from sports.(4, 42) In professional athletes, acute hamstring strains make up 15% of all injuries in Australian Rules football(43) and 12% of all injuries in British soccer.(25) In the American National Football League (NFL) from 1998 to 2007, there were 2.2 hamstring strain injuries per 1000 athlete exposures in training camp, second only to knee sprains.(21) Some studies have reported that almost 1 in 3 hamstring strains will recur, and many happen within the first 2 weeks of return to sport.(26, 42, 55) The recurrence rate of hamstring strains has been reported to be 30% in professional Australian football and 12% in professional soccer players.(42)
Two different types of acute hamstring strains have been described with different mechanisms of injury.(3–5) Type I acute hamstring strains occur during high-speed running. Injury to the hamstring muscle has been shown to occur during the terminal swing phase of running, when the hamstring muscles eccentrically contract to decelerate the swinging limb and prepare for foot strike.(13) The long head of the biceps femoris is most commonly involved in type I hamstring strains, typically at the proximal muscle-tendon junction.(4, 26, 55) Type II hamstring strains occur in the setting of excessive lengthening of the hamstrings.(5) These types of hamstring strains are more common in activities such as dancing, slide tackling and high kicking that combine hip flexion with knee extension.(26, 55) Type II hamstring strains commonly involve the proximal free tendon of the semimembranosus, close to the ischial tuberosity.(5) Recovery from type II hamstring strains has been shown to be prolonged compared to type I hamstring strains.(2)
Acute hamstring strain injuries can also be classified by severity of pain, weakness and loss of range of motion. Grade I injuries are mild with no loss of strength or function, minimal loss of musculotendinous unit structural integrity, and low-grade inflammation. Grade II injuries include partial or incomplete tears and present with moderate loss of strength. There may be muscular edema and hematoma locally. Grade III injuries are severe, involve complete tears or rupture and result in significant loss of function.(1, 35, 44)
Proximal hamstring tendinopathy is a relatively uncommon cause of posterior thigh pain that can affect a variety of athletes, but are seen more often in sprinters, mid- and long-distance runners and in endurance athletes.(12, 36, 40) It is a chronic, degenerative condition that is caused by mechanical overload and repetitive stretch. Potential factors that can lead to hamstring tendinopathy include overuse, poor lumbopelvic stability and relatively weak hamstring musculature.(22) The semimembranosus is most commonly affected in proximal hamstring tendinopathy.(36) Sciatic nerve irritation has also been reported in the setting of proximal hamstring tendinopathy. It has been thought to be due to repetitive stretch and overload of the proximal hamstring tendons, scarring and adhesions may form around the sciatic nerve, potentially causing additional posterior thigh pain.(36)
The purpose of this article is to review the current literature regarding the diagnosis, treatment and return to play considerations for hamstring injuries in the athlete, specifically focusing on acute hamstring muscle strains and chronic proximal hamstring tendinopathy.
DIAGNOSIS
The history and physical examination are essential when treating an athlete with a suspected hamstring injury. There are many overlapping pain referral patterns that localize to the posterior thigh, including issues from the lumbar spine, hip joint, and sacroiliac joints. Imaging can play a role in diagnosis of acute hamstring strains and chronic proximal hamstring tendinopathy. It is important to maintain an appropriate differential diagnosis when evaluating this athlete.
History
Acute Hamstring Strain
Athletes with hamstring strain injuries will typically describe sudden onset of sharp, stabbing or twinge-like posterior thigh pain.(1, 26, 55) They may describe an audible “pop”, which has been reported primarily in type II (overstretch) hamstring strains.(6) Patients with acute hamstring strains may report difficulty continuing the activity or sport.(26, 55) They may also present with a stiff-legged gait because of avoidance of hip and knee flexion.(15)
Proximal Hamstring Tendinopathy
Patients with proximal hamstring tendinopathy do not usually recall a specific inciting event, and report gradual increase of pain in the posterior thigh.(12, 36) The pain is often described as tightness or cramping in the posterior thigh or deep buttock, located close to or at the ischial tuberosity.(12, 40, 55) Pain can extend down the posterior thigh distally to the popliteal fossa.(12, 22, 35) Symptoms can be exacerbated with repetitive eccentric hamstring contraction, forward flexion of the trunk and with running.(12, 22, 40) Patients will also report increased pain with sitting.(8, 12, 22, 40)
Examination
Physical examination of a patient with a suspected hamstring injury should include inspection and palpation of the affected region, passive stretch of the hamstring muscles and resistance testing of the hamstring muscle. On the palpatory examination, special attention should be placed on hamstring origin at the ischial tuberosity, the muscle belly of the hamstrings to determine if there is focal pain or a palpable focal defect, and the insertion of the hamstring tendons at the pes anserine medially and the fibular head laterally. An examination of the hip and lumbar spine and a complete neurological examination of the lower extremities should also be performed to identify any other potential causes of posterior thigh pain. Neural tension tests such as the seated slump test can be used to determine if symptoms are due to lumbar spine or sciatic nerve involvement.(26)
Acute Hamstring Strain
On inspection, moderate to severe hamstring muscle strains (grades II or III) can result in visible ecchymosis distal to injury site along the posterior thigh and knee.(1) Ecchymosis can be delayed and does not always appear immediately after injury. Direct palpation of the hamstring is important to help identify the specific region that is injured. A palpable defect in the muscle or musculotendinous unit may be appreciated in athletes with complete ruptures.(1, 26) Oftentimes, an athlete with a complete rupture of one of the hamstring muscles will still be able to flex the knee since the other hamstring muscles are intact; however, this may be painful. Passive knee extension can often be more painful for patients with partial tears of the hamstring muscles. Passive straight leg raise and hip flexion with knee extension are used to assess hamstring flexibility and to assess for pain.(26, 53) Knee flexion strength should be examined with the patient in prone position, with resistance applied in both 15 and 90 degrees of knee flexion.(26) Hip extension strength should also be tested in the prone position, with the knee in both 90 and 0 degrees of flexion.(26) The assessment should be performed bilaterally, looking for pain provocation and weakness.(26) The hamstring muscle is tested in multiple positions because of its biarticular nature and subsequently changes length with flexion of the hip and knee.(26)
Proximal Hamstring Tendinopathy
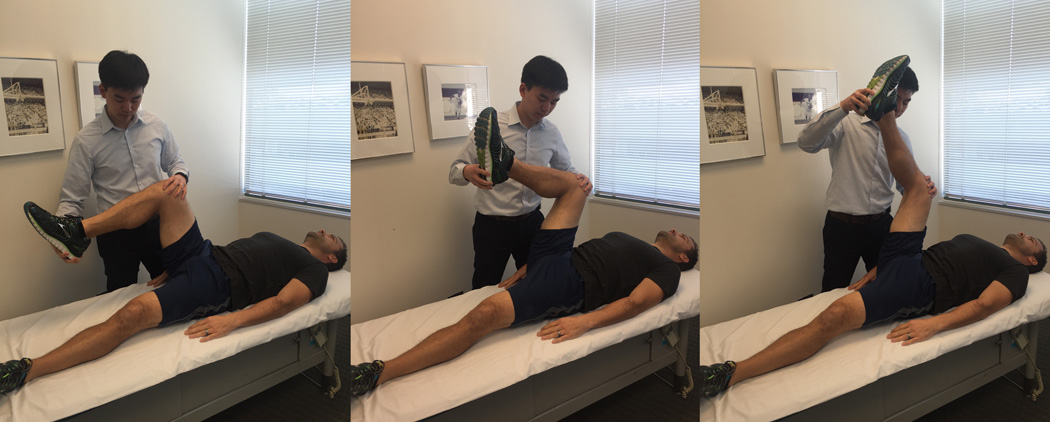
Three physical examination maneuvers have been described for diagnosis of proximal hamstring tendinopathy. The Puranen-Orava test is a standing test that actively stretches the hamstring when the hip is flexed to 90 degrees and the knee is extended fully and the foot is on a support 90 degrees to the standing body (FIGURE 1).(11, 46) The bent-knee stretch test is performed with the patient in supine. The hip and knee are flexed to end range and then the knee is passively extended. To perform the modified bent-knee stretch test, the patient is supine with the legs fully extended. The examiner maximally flexes the hip and knee, and rapidly straightens the knee (FIGURE 2). Each test is considered positive if there is exacerbation of symptoms with the maneuver.(11) All 3 tests demonstrated moderate to high validity, high inter and intra-rater reliability.(11) Other examination findings include tenderness at the hamstring origin at the ischial tuberosity, and pain with active hamstring stretches. There is typically no loss of strength with knee flexion or hip extension.(40) There may also be pain with minimal or no limitation in flexibility.(55)
FIGURE 1.

The Puranen-Orava Test
FIGURE 2.
The Modified Bent-Knee Stretch Test
Imaging
Acute Hamstring Strain
Imaging is usually not needed to make the diagnosis of an acute hamstring strain. There is no significant use for x-ray imaging in the evaluation of acute hamstring strain unless an ischial avulsion injury is suspected.(14) Both ultrasound and MRI have been shown to effectively identify and assess the extent of acute hamstring strain injuries.(16, 32) High signal intensity can be seen on T2-weighted MRI images reflecting edema within or around the muscle in acute hamstring injuries.(14) On ultrasound, edema in the setting of hamstring strains can be visualized as an area of hypoechogenicity, most commonly at the musculotendinous junction.(32) MRI has been shown to be more accurate than ultrasound for evaluation of deeper muscle injuries, when there is scarring from previous hamstring injuries, and for identification of hamstring tendon avulsion.(16, 26, 30) In the athlete population, the availability of ultrasound in the training room can be extraordinarily beneficial if there is a skilled ultrasonographer who can assess for hematoma and muscle tears.(28)
Proximal Hamstring Tendinopathy
For hamstring tendinopathy, MRI and ultrasound can be used for diagnostic purposes. MRI has been shown to have higher sensitivity than ultrasound for diagnosing proximal hamstring tendinopathy.(63) MRI will demonstrate increased tendon girth, T2-weighted signal with distal feathery appearance and increased signal heterogeneity at or around the origin of the hamstring tendons.(18, 31, 36, 40) Other findings on MRI include reactive edema within the ischial tuberosity.(8, 22) Ultrasound findings of hamstring tendinopathy include peritendinous fluid, tendon thickening, hypoechoic regions in the tendon and echogenic foci in the tendon representing calcifications.(31, 63) Ultrasound cannot visualize reactive bone marrow edema. Benefits of ultrasound include decreased costs, ability to perform imaging in real time and provide guidance for injections.(53) Ultrasound also provides the added benefit of serial evaluations for athletes to assess progress for return to play, particularly in settings where the team physician is skilled in ultrasonography to make the assessment in the training room.
Differential Diagnosis
The differential diagnosis of posterior thigh pain includes hamstring tendon avulsion injury, ischial apophyseal avulsion, stress fractures, adductor muscle strain, referred posterior thigh pain from the lumbar spine, hip joint, or sacroiliac joint and ischiogluteal bursitis.(22, 31, 55)
TREATMENT
The primary goals of a rehabilitation protocol for hamstring injuries is to return the athlete to sport at the prior level of performance, and to minimize risk of reinjury.(26)
Acute Hamstring Strain
Three phases of rehabilitation for acute hamstring strains has been described and should be followed in a progressive nature.(26, 55) Phase 1 focuses on decreasing pain and edema, prevention of scar formation, development of neuromuscular control at slow speed and prevention of excessive lengthening.(26, 55) Initial management of hamstring strains in the acute phase includes the RICE protocol of rest, ice, compression and elevation.(1, 10, 14, 34) Conservative medical management can include the use of nonsteroidal anti-inflammatory drugs (NSAIDs).(55) However, the early use of NSAIDs for acute hamstring strains is controversial, as prior studies have not demonstrated benefit.(51) During Phase 1 of rehabilitation, athletes may shorten their strides during ambulation and may use crutches for more moderate or severe injuries.(26, 55) Progressive agility and trunk stabilization exercises can be performed at low to moderate intensity.(55) Isolated resistance training of the affected hamstring muscle should be avoided.(26) Exercises should be done within a limited, protected range of motion, and excessive stretching of the affected hamstring should be avoided.(26) Progression to the next phase can occur when the athlete is able to walk normally without pain, jog at very low speeds without pain and able to perform pain-free isometric hamstring contraction with prone knee flexion at 90 degrees against submaximal resistance (50–70%).(26, 55)
Phase II of rehabilitation involves increase in the intensity and range of motion of the exercises, initiation of eccentric resistance exercises, and neuromuscular training at faster speeds.(26, 55) Compared to Phase I, the exercises will involve a gradual increase in range of motion and lengthening of the hamstring. However, hamstring lengthening to end range should be avoided if there is still weakness during this phase.(26, 55) Ice can be used as needed for pain associated with exercise and rehabilitation. The intensity and speed of neuromuscular control, agility and trunk stabilization exercises are progressively increased.(26) Eccentric strengthening exercises for the hamstrings are also initiated during this phase.(26, 55) Progression to Phase III occurs when there is full strength of the hamstring without pain when performing 1 repetition of maximum isometric contraction with prone knee flexion at 90 degrees, and the athlete can jog forward and backward at 50% maximum speed without pain.(26, 55)
Phase III of rehabilitation involves more advanced neuromuscular control and eccentric strengthening exercises as well as sport-specific exercises with the goal of returning the athlete to play. The athlete generally has no restriction of range of motion during this phase. Progressive ability and trunk stabilization exercises should incorporate more sport-specific drills and dynamic agility exercises.(26, 55) Eccentric hamstring strengthening exercises can be progressed toward end range of motion.(26, 55) Return to sport criteria include no pain with palpation over the injury site, full concentric and eccentric strength of the hamstrings without pain, no kinesiophobia,(55) full functional abilities that include sport-specific movements at near maximum speed and intensity without pain.(26)
Sherry et al performed a randomized controlled trial comparing 2 different hamstring rehabilitation programs. This study randomized 24 athletes with acute hamstring strains into 1 of 2 rehabilitation programs consisting of either progressive agility and trunk stabilization exercises or isolated hamstring stretching and strengthening exercises.(54) The athletes in the progressive agility and trunk stabilization group demonstrated a faster return to play compared to the stretching and strengthening group (22.2 +/ 8.3 days versus 37.4 +/− 27.6 days), as well as a lower re-injury rate (7.7% versus 70%).(54) The authors concluded that a rehabilitation program of progressive agility and trunk stabilization for acute hamstring injuries is more effective than a program emphasizing isolated hamstring stretching and strengthening for return to play and prevention of recurrence in acute hamstring strains.(54) Another study by Silder et al randomized 29 athletes into 1 of 2 rehabilitation groups: a progressive agility and trunk stabilization program or a progressive running and eccentric strengthening program.(56) There was no significant difference in time to return to sport, with a mean of 25.2 +/− 6.3 days in the progressive agility and trunk stabilization group and 28.8 +/− 11.4 days in the progressive running and eccentric strengthening group.(56) Both groups demonstrated similar rates of hamstring recovery as demonstrated on MRI.(56)
The use of corticosteroid injections for acute hamstring strains has not been widely studied. Levine et al performed a retrospective review of 58 professional NFL players who were treated with corticosteroid injections after acute hamstring strains.(37) All players had grade II or III hamstring strains and were given a palpation-guided intramuscular corticosteroid and anesthetic injection. The majority of players (56 of 58) received the injection within 72 hours of the injury. The average time to return to full practice was 7.6 days, ranging from 0 to 24 days, and 49 players missed no games. No complications were reported from the injections.(37) The role of corticosteroid injections in the treatment of acute hamstring strains as well as the potential complications and side effects need to be further studied.
There have been mixed results in the literature regarding the effectiveness of platelet-rich plasma (PRP) for acute hamstring strains. Hamid et al performed a randomized controlled trial where 28 patients with acute, grade II hamstring strains received either PRP with a rehabilitation program or a rehabilitation program alone.(23) The rehabilitation program used in the study was a progressive agility and trunk stabilization protocol. The patients in the PRP group had a statistically significantly faster return time to return to play (26.7 +/− 7.0 days versus 42.5 +/− 20.6 days) as well as significantly lower pain severity scores than the rehabilitation group.(23) However, it should be noted that there was no sham injection included in this study.
Hamilton et al performed a study on 90 professional athletes with grade I or grade II hamstring strains confirmed on MRI, randomizing them to either receive PRP, platelet-poor plasma or no injection.(24) All of the subjects also received a standard rehabilitation program. There was no significant difference for return to sport between the PRP group and the rehabilitation only group, and the authors concluded that there is no benefit of a single PRP injection in athletes with acute hamstring injuries.(24) Reurink et al performed a study in which 80 competitive and recreational athletes with acute hamstring strains confirmed on MRI were randomized to receive intramuscular PRP or a placebo, isotonic saline.(49) They reported no significant difference in time to return to sport (median 42 days in both groups) or re-injury rate (16% in PRP group versus 14% in placebo group).(49) The authors reported also that 1 year post-injection, there was no significant difference in the re-injury rate between the groups.(50) Rettig et al reported that out of 10 NFL players with grade I or II acute hamstring strains, there was no significant difference in time to return to play between the 5 players receiving PRP injection with a rehabilitation program and the 5 players receiving only a rehabilitation program (20 days in PRP group, 17 days in non-PRP group).(47) Overall, the majority of studies demonstrate no significant benefit for PRP injections in acute hamstring strains for return to play and re-injury rates.
Proximal Hamstring Tendinopathy
Conservative management for athletes with proximal hamstring tendinopathy that have been described in the literature include eccentric exercises,(17, 22, 27) soft-tissue mobilization,(22) shockwave therapy,(12) corticosteroid injections,(40, 63) and platelet-rich plasma injections.(60)
One study of 40 professional athletes with chronic proximal hamstring tendinopathy demonstrated that shockwave therapy had a greater improvement in pain scores, Nirschl phase rating scale and higher rate of return to sports than traditional conservative treatment of physical therapy and NSAIDs.(12) Two studies investigated the effect of peritendinous corticosteroid injections in patients with proximal hamstring tendinopathy. Nicholson et al reported that for fluoroscopically-guided corticosteroid injections, there was a significant improvement in pain score and level of athletic participation at 21 months.(40) Zissen et al reported found that 50% of patients who underwent ultrasound-guided corticosteroid injections reported moderate to complete resolution of symptoms for at least 1 month.(63) However, the use of corticosteroid injections in the treatment of chronic tendinopathy is controversial given the potential risks, including local irritation, skin depigmentation, suppression of tenocyte activity and collagen synthesis, and tendon avulsion.(40, 52, 61, 62)
One study investigating PRP injection as a treatment for proximal hamstring tendinopathy showed significant improvement in pain and Nirschl phase rating scale compared to treatment with physical therapy and NSAIDs.(60) The PRP injections in this study were performed using direct palpation without image-guidance. All patients who received PRP returned to play in 4.5 months.(60) Fader et al reported that out of 18 patients with chronic proximal hamstring tendinopathy treated with ultrasound-guided PRP injection, 10 patients reported 80% or greater improvement in pain at 6 months. The overall average improvement was 63%.(20) Larger, controlled studies investigating the effectiveness of PRP for treatment proximal hamstring tendinopathy are required. Image-guided injections should be considered to improve accuracy and safety.
Eccentric exercise has been demonstrated to be an effective treatment for tendinopathy.(29, 39, 41) Hamstring eccentric exercises can be performed using hamstring curl machines, reverse cable curls, weight bearing hamstring curls on exercise ball, reverse plank, kneeling Nordic leg curl, standing single or double leg dead lifts.(17) Cushman et al recently proposed an alternate method of hamstring eccentric strengthening using a treadmill, with the athlete standing backwards and eccentrically resisting movement of the belt.(17) There have been case reports in the literature demonstrating improvement of proximal hamstring tendinopathy with eccentric exercises in athletes.(17, 27) Jayaseelan et al described 2 cases of runners with proximal hamstring tendinopathy who were treated with eccentric hamstring loading, lumbopelvic stabilization exercises and trigger point needling.(27) The athletes in both cases had significant improvements in pain and function over 8–10 weeks and returned to sport without pain.(27)
RETURN TO PLAY
Acute Hamstring Strain
There has been a wide range of reported time to return to play after acute hamstring injuries.(38) A number of factors have been reported to be associated with longer recovery period and time to return to play after acute hamstring injury, including type of hamstring injury,(2, 4, 5, 57) proximity to the ischial tuberosity,(4, 7, 56) injury involving proximal free tendon, (2, 4, 5) and increased length and cross sectional area of injury.(16, 57) Type I hamstring strains have been reported to have a more acute decline in function and a faster recovery than type II hamstring injuries.(2, 4, 5) The type I, or high-speed running injuries have been reported to take a mean of 16 weeks to return to pre-injury level of performance in a study of elite sprinters.(4) The type II, overstretch injuries can take up to a mean of 50 weeks for return to prior level of competition in a study of professional dancers.(5) Shorter times to return to play after acute hamstring strain have been reported in studies on NFL and professional rugby players, ranging from a mean of 8 to 25 days lost from full training and competition.(9, 21) While considerably shorter than the aforementioned studies on type I and II injuries, these studies involved different sports and also did not take into account return to pre-injury level of performance.
Clinical predictors of return to play after hamstring injuries have been studied. Moen et al reported that self-reported time to return to play and passive straight leg raise deficit were significantly associated with time to return to play after hamstring injury.(38) Warren et al studied 59 Australian football players and found that the athletes that required more than 1 day to walk without pain were more likely to take longer than 3 weeks to return to play.(59)
In terms of imaging findings and return to play, a systematic review by Reurink et al(48) reported conflicting evidence, stating that 3 studies showed a significant association between proximity to the ischial tuberosity and longer time to return to play,(4, 7, 56) while 1 study showed no association.(5) The systematic review showed no strong evidence from MRI findings, including length, cross-sectional area, signal volume, that can predict prognosis for time to return to play after acute hamstring injury.(48) Moen et al also report no correlation of MRI findings in grade I and grade II hamstring injuries and time to return to play.(38) Some studies have shown that cross sectional area and length are directly related to time away from sport.(16, 57) However, other studies have shown that the severity of hamstring injuries based on MRI and baseline MRI findings of initial injuries do not predict reinjury.(19, 33, 58) With regard to ultrasound, Petersen et al found no correlation of imaging findings in athletes with acute hamstring injuries with time to return to play.(45)
Proximal Hamstring Tendinopathy
Return to play for athletes with proximal hamstring tendinopathy depends on the severity and duration of the condition.(22) However, there have been limited studies describing specific guidelines for returning to play. Fredericson et al describes one protocol that involves a graduated return to activity, progressing through a walk/run program with limited pace, mileage and incline.(22) They states that prior to return to running after proximal hamstring tendinopathy, the athlete must have full range of motion and no pain with strength testing.(22)
CONCLUSION
Hamstring injuries are very common in athletes and can lead to prolonged time away from sport. Acute hamstring strains can occur with high-speed running or with excessive lengthening of the hamstrings. Athletes with chronic proximal hamstring tendinopathy often do not report a specific inciting event and typically report a gradual increase in posterior thigh pain. A thorough history and physical examination is important to determine the appropriate diagnosis and rule out other potential causes of posterior thigh pain. Imaging modalities such as MRI and ultrasound are effective in detecting acute hamstring strains and proximal hamstring tendinopathy. However, imaging findings generally have not been shown to correlate with prognosis of return to play. Conservative management of hamstring injuries in athletes involves a progressive rehabilitation protocol. For acute hamstring strains, this involves a gradual increase in intensity, range of motion and eccentric resistance leading to more sport-specific and neuromuscular control exercises. Eccentric strengthening exercises are used for management of chronic proximal hamstring tendinopathy. Smaller studies looking at corticosteroid and PRP injections have had mixed results. The type of acute hamstring strain and clinical factors such as time to walk without pain have been shown to correlate with time to return to play.
TABLE 1.
Characteristics of Acute Hamstring Strain and Proximal Hamstring Tendinopathy
| Acute Hamstring Strain | Proximal Hamstring Tendinopathy | |
|---|---|---|
| Mechanism | Type I – high-speed running Type II – overstretch |
Mechanical overload, repetitive stretch |
| Most common location |
Type I – proximal muscle-tendon junction Type II – proximal free tendon of semimembranosus |
Semimembranosus |
| Presentation | Sudden onset “Pop” (primarily type II) Difficulty continuing sport |
No specific inciting event Gradual increase of pain |
| Physical Examination |
Ecchymosis +/− palpable defect Pain and/or weakness with hip extension, knee flexion testing |
Puranen-Orava test Bent-knee stretch test (modified) Tenderness at ischial tuberosity No loss of strength |
| Imaging | Not necessary for diagnosis X-ray if suspect ischial avulsion injury |
MRI or ultrasound. MRI with higher sensitivity. |
| Conservative Treatment |
Phase I – decrease pain and edema, RICE protocol Phase II – increase exercise, neuromuscular training, initiate eccentric exercises Phase III – sport-specific exercises |
Eccentric exercises Graduated return to activity protocol Shockwave therapy Soft-tissue mobilization |
| Injections | Corticosteroids – minimal evidence Platelet-rich-plasma – mixed evidence |
Corticosteroids – minimal evidence, controversial Platelet-rich plasma – minimal evidence |
| Return to play | Faster recovery for Type I strains, shorter time to walk without pain |
Full range of motion and no pain with strength testing required |
Summary Statement.
The article focuses on diagnosis, treatment and return to play for hamstring strains and proximal hamstring tendinopathy in the athlete.
Acknowledgments
DISCLOSURES: Dr. Rho’s time is paid for in part by a grant from the National Institute of Health (K12HD001097-16).
REFERENCES
- 1.Ali K, Leland JM. Hamstring strains and tears in the athlete. Clinics in sports medicine. 2012;31(2):263–272. doi: 10.1016/j.csm.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Askling C, Saartok T, Thorstensson A. Type of acute hamstring strain affects flexibility, strength, and time to return to pre-injury level. British journal of sports medicine. 2006;40(1):40–44. doi: 10.1136/bjsm.2005.018879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Askling CM, Malliaropoulos N, Karlsson J. High-speed running type or stretching-type of hamstring injuries makes a difference to treatment and prognosis. British journal of sports medicine. 2012;46(2):86–87. doi: 10.1136/bjsports-2011-090534. [DOI] [PubMed] [Google Scholar]
- 4.Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. The American journal of sports medicine. 2007;35(2):197–206. doi: 10.1177/0363546506294679. [DOI] [PubMed] [Google Scholar]
- 5.Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during slow-speed stretching: clinical, magnetic resonance imaging, and recovery characteristics. The American journal of sports medicine. 2007;35(10):1716–1724. doi: 10.1177/0363546507303563. [DOI] [PubMed] [Google Scholar]
- 6.Askling CM, Tengvar M, Saartok T, Thorstensson A. Proximal hamstring strains of stretching type in different sports: injury situations, clinical and magnetic resonance imaging characteristics, and return to sport. The American journal of sports medicine. 2008;36(9):1799–1804. doi: 10.1177/0363546508315892. [DOI] [PubMed] [Google Scholar]
- 7.Askling CM, Tengvar M, Thorstensson A. Acute hamstring injuries in Swedish elite football: a prospective randomised controlled clinical trial comparing two rehabilitation protocols. British journal of sports medicine. 2013;47(15):953–959. doi: 10.1136/bjsports-2013-092165. [DOI] [PubMed] [Google Scholar]
- 8.Bencardino JT, Mellado JM. Hamstring injuries of the hip. Magnetic resonance imaging clinics of North America. 2005;13(4):677–690. doi: 10.1016/j.mric.2005.08.002. vi. [DOI] [PubMed] [Google Scholar]
- 9.Brooks JH, Fuller CW, Kemp SP, Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. The American journal of sports medicine. 2006;34(8):1297–1306. doi: 10.1177/0363546505286022. [DOI] [PubMed] [Google Scholar]
- 10.Brukner P, Khan K, Brukner P. 4th. Sydney ; New York: McGraw-Hill; 2012. Brukner & Khan's clinical sports medicine; p. xlvii.p. 1296. [Google Scholar]
- 11.Cacchio A, Borra F, Severini G, Foglia A, Musarra F, Taddio N, et al. Reliability and validity of three pain provocation tests used for the diagnosis of chronic proximal hamstring tendinopathy. British journal of sports medicine. 2012;46(12):883–887. doi: 10.1136/bjsports-2011-090325. [DOI] [PubMed] [Google Scholar]
- 12.Cacchio A, Rompe JD, Furia JP, Susi P, Santilli V, De Paulis F. Shockwave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletes. The American journal of sports medicine. 2011;39(1):146–153. doi: 10.1177/0363546510379324. [DOI] [PubMed] [Google Scholar]
- 13.Chumanov ES, Heiderscheit BC, Thelen DG. Hamstring musculotendon dynamics during stance and swing phases of high-speed running. Medicine and science in sports and exercise. 2011;43(3):525–532. doi: 10.1249/MSS.0b013e3181f23fe8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. The Journal of the American Academy of Orthopaedic Surgeons. 1998;6(4):237–248. doi: 10.5435/00124635-199807000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Cohen S, Bradley J. Acute proximal hamstring rupture. The Journal of the American Academy of Orthopaedic Surgeons. 2007;15(6):350–355. doi: 10.5435/00124635-200706000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR American journal of roentgenology. 2004;183(4):975–984. doi: 10.2214/ajr.183.4.1830975. [DOI] [PubMed] [Google Scholar]
- 17.Cushman D, Rho ME. Conservative Treatment of Subacute Proximal Hamstring Tendinopathy Using Eccentric Exercises Performed With a Treadmill: A Case Report. The Journal of orthopaedic and sports physical therapy. 2015;45(7):557–562. doi: 10.2519/jospt.2015.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Smet AA, Blankenbaker DG, Alsheik NH, Lindstrom MJ. MRI appearance of the proximal hamstring tendons in patients with and without symptomatic proximal hamstring tendinopathy. AJR American journal of roentgenology. 2012;198(2):418–422. doi: 10.2214/AJR.11.6590. [DOI] [PubMed] [Google Scholar]
- 19.De Vos RJ, Reurink G, Goudswaard GJ, Moen MH, Weir A, Tol JL. Clinical findings just after return to play predict hamstring re-injury, but baseline MRI findings do not. British journal of sports medicine. 2014;48(18):1377–1384. doi: 10.1136/bjsports-2014-093737. [DOI] [PubMed] [Google Scholar]
- 20.Fader RR, Mitchell JJ, Traub S, Nichols R, Roper M, Dan OM, et al. Platelet-rich plasma treatment improves outcomes for chronic proximal hamstring injuries in an athletic population. Muscles, ligaments and tendons journal. 2014;4(4):461–466. [PMC free article] [PubMed] [Google Scholar]
- 21.Feeley BT, Kennelly S, Barnes RP, Muller MS, Kelly BT, Rodeo SA, et al. Epidemiology of National Football League training camp injuries from 1998 to 2007. The American journal of sports medicine. 2008;36(8):1597–1603. doi: 10.1177/0363546508316021. [DOI] [PubMed] [Google Scholar]
- 22.Fredericson M, Moore W, Guillet M, Beaulieu C. High hamstring tendinopathy in runners: meeting the challenges of diagnosis, treatment, and rehabilitation. The Physician and sportsmedicine. 2005;33(5):32–43. doi: 10.3810/psm.2005.05.89. [DOI] [PubMed] [Google Scholar]
- 23.Hamid MS, Yusof A, Mohamed Ali MR. Platelet-rich plasma (PRP) for acute muscle injury: a systematic review. PloS one. 2014;9(2):e90538. doi: 10.1371/journal.pone.0090538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamilton B, Tol JL, Almusa E, Boukarroum S, Eirale C, Farooq A, et al. Platelet-rich plasma does not enhance return to play in hamstring injuries: a randomised controlled trial. British journal of sports medicine. 2015;49(14):943–950. doi: 10.1136/bjsports-2015-094603. [DOI] [PubMed] [Google Scholar]
- 25.Hawkins RD, Hulse MA, Wilkinson C, Hodson A, Gibson M. The association football medical research programme: an audit of injuries in professional football. British journal of sports medicine. 2001;35(1):43–47. doi: 10.1136/bjsm.35.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. The Journal of orthopaedic and sports physical therapy. 2010;40(2):67–81. doi: 10.2519/jospt.2010.3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jayaseelan DJ, Moats N, Ricardo CR. Rehabilitation of proximal hamstring tendinopathy utilizing eccentric training, lumbopelvic stabilization, and trigger point dry needling: 2 case reports. The Journal of orthopaedic and sports physical therapy. 2014;44(3):198–205. doi: 10.2519/jospt.2014.4905. [DOI] [PubMed] [Google Scholar]
- 28.Kary JM. Ultrasound. In: Micheli LJ, editor. Encyclopedia of Sports Medicine. Vol. 4. Thousand Oaks, CA: SAGE Reference; 2011. pp. 1522–1525. [Google Scholar]
- 29.Kingma JJ, de Knikker R, Wittink HM, Takken T. Eccentric overload training in patients with chronic Achilles tendinopathy: a systematic review. British journal of sports medicine. 2007;41(6):e3. doi: 10.1136/bjsm.2006.030916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skeletal radiology. 2003;32(10):582–589. doi: 10.1007/s00256-003-0674-5. [DOI] [PubMed] [Google Scholar]
- 31.Koulouris G, Connell D. Hamstring muscle complex: an imaging review. Radiographics : a review publication of the Radiological Society of North America, Inc. 2005;25(3):571–586. doi: 10.1148/rg.253045711. [DOI] [PubMed] [Google Scholar]
- 32.Koulouris G, Connell D. Imaging of hamstring injuries: therapeutic implications. European radiology. 2006;16(7):1478–1487. doi: 10.1007/s00330-005-0075-3. [DOI] [PubMed] [Google Scholar]
- 33.Koulouris G, Connell DA, Brukner P, Schneider-Kolsky M. Magnetic resonance imaging parameters for assessing risk of recurrent hamstring injuries in elite athletes. The American journal of sports medicine. 2007;35(9):1500–1506. doi: 10.1177/0363546507301258. [DOI] [PubMed] [Google Scholar]
- 34.Kujala UM, Orava S, Jarvinen M. Hamstring injuries. Current trends in treatment and prevention. Sports medicine. 1997;23(6):397–404. doi: 10.2165/00007256-199723060-00005. [DOI] [PubMed] [Google Scholar]
- 35.Lempainen L, Banke IJ, Johansson K, Brucker PU, Sarimo J, Orava S, et al. Clinical principles in the management of hamstring injuries. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2015;23(8):2449–2456. doi: 10.1007/s00167-014-2912-x. [DOI] [PubMed] [Google Scholar]
- 36.Lempainen L, Sarimo J, Mattila K, Vaittinen S, Orava S. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. The American journal of sports medicine. 2009;37(4):727–734. doi: 10.1177/0363546508330129. [DOI] [PubMed] [Google Scholar]
- 37.Levine WN, Bergfeld JA, Tessendorf W, Moorman CT., 3rd Intramuscular corticosteroid injection for hamstring injuries. A 13-year experience in the National Football League. The American journal of sports medicine. 2000;28(3):297–300. doi: 10.1177/03635465000280030301. [DOI] [PubMed] [Google Scholar]
- 38.Moen MH, Reurink G, Weir A, Tol JL, Maas M, Goudswaard GJ. Predicting return to play after hamstring injuries. British journal of sports medicine. 2014;48(18):1358–1363. doi: 10.1136/bjsports-2014-093860. [DOI] [PubMed] [Google Scholar]
- 39.Murtaugh B, Ihm JM. Eccentric training for the treatment of tendinopathies. Current sports medicine reports. 2013;12(3):175–182. doi: 10.1249/JSR.0b013e3182933761. [DOI] [PubMed] [Google Scholar]
- 40.Nicholson LT, DiSegna S, Newman JS, Miller SL. Fluoroscopically Guided Peritendinous Corticosteroid Injection for Proximal Hamstring Tendinopathy: A Retrospective Review. Orthopaedic journal of sports medicine. 2014;2(3) doi: 10.1177/2325967114526135. 2325967114526135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ohberg L, Lorentzon R, Alfredson H. Eccentric training in patients with chronic Achilles tendinosis: normalised tendon structure and decreased thickness at follow up. British journal of sports medicine. 2004;38(1):8–11. doi: 10.1136/bjsm.2001.000284. discussion. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Orchard J, Best TM, Verrall GM. Return to play following muscle strains. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2005;15(6):436–441. doi: 10.1097/01.jsm.0000188206.54984.65. [DOI] [PubMed] [Google Scholar]
- 43.Orchard J, Seward H. Epidemiology of injuries in the Australian Football League, seasons 1997–2000. British journal of sports medicine. 2002;36(1):39–44. doi: 10.1136/bjsm.36.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Palmer WE, Kuong SJ, Elmadbouh HM. MR imaging of myotendinous strain. AJR American journal of roentgenology. 1999;173(3):703–709. doi: 10.2214/ajr.173.3.10470908. [DOI] [PubMed] [Google Scholar]
- 45.Petersen J, Thorborg K, Nielsen MB, Skjodt T, Bolvig L, Bang N, et al. The diagnostic and prognostic value of ultrasonography in soccer players with acute hamstring injuries. The American journal of sports medicine. 2014;42(2):399–404. doi: 10.1177/0363546513512779. [DOI] [PubMed] [Google Scholar]
- 46.Puranen J, Orava S. The hamstring syndrome. A new diagnosis of gluteal sciatic pain. The American journal of sports medicine. 1988;16(5):517–521. doi: 10.1177/036354658801600515. [DOI] [PubMed] [Google Scholar]
- 47.Rettig AC, Meyer S, Bhadra AK. Platelet-Rich Plasma in Addition to Rehabilitation for Acute Hamstring Injuries in NFL Players: Clinical Effects and Time to Return to Play. Orthopaedic journal of sports medicine. 2013;1(1) doi: 10.1177/2325967113494354. 2325967113494354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reurink G, Brilman EG, de Vos RJ, Maas M, Moen MH, Weir A, et al. Magnetic resonance imaging in acute hamstring injury: can we provide a return to play prognosis? Sports medicine. 2015;45(1):133–146. doi: 10.1007/s40279-014-0243-1. [DOI] [PubMed] [Google Scholar]
- 49.Reurink G, Goudswaard GJ, Moen MH, Weir A, Verhaar JA, Bierma-Zeinstra SM, et al. Platelet-rich plasma injections in acute muscle injury. The New England journal of medicine. 2014;370(26):2546–2547. doi: 10.1056/NEJMc1402340. [DOI] [PubMed] [Google Scholar]
- 50.Reurink G, Goudswaard GJ, Moen MH, Weir A, Verhaar JA, Bierma-Zeinstra SM, et al. Rationale, secondary outcome scores and 1-year follow-up of a randomised trial of platelet-rich plasma injections in acute hamstring muscle injury: the Dutch Hamstring Injection Therapy study. British journal of sports medicine. 2015;49(18):1206–1212. doi: 10.1136/bjsports-2014-094250. [DOI] [PubMed] [Google Scholar]
- 51.Reynolds JF, Noakes TD, Schwellnus MP, Windt A, Bowerbank P. Non-steroidal anti-inflammatory drugs fail to enhance healing of acute hamstring injuries treated with physiotherapy. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 1995;85(6):517–522. [PubMed] [Google Scholar]
- 52.Scutt N, Rolf CG, Scutt A. Glucocorticoids inhibit tenocyte proliferation and Tendon progenitor cell recruitment. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2006;24(2):173–182. doi: 10.1002/jor.20030. [DOI] [PubMed] [Google Scholar]
- 53.Sherry M. Examination and treatment of hamstring related injuries. Sports health. 2012;4(2):107–114. doi: 10.1177/1941738111430197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. The Journal of orthopaedic and sports physical therapy. 2004;34(3):116–125. doi: 10.2519/jospt.2004.34.3.116. [DOI] [PubMed] [Google Scholar]
- 55.Sherry MA, Johnston TS, Heiderscheit BC. Rehabilitation of acute hamstring strain injuries. Clinics in sports medicine. 2015;34(2):263–284. doi: 10.1016/j.csm.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 56.Silder A, Sherry MA, Sanfilippo J, Tuite MJ, Hetzel SJ, Heiderscheit BC. Clinical and morphological changes following 2 rehabilitation programs for acute hamstring strain injuries: a randomized clinical trial. The Journal of orthopaedic and sports physical therapy. 2013;43(5):284–299. doi: 10.2519/jospt.2013.4452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Slavotinek JP, Verrall GM, Fon GT. Hamstring injury in athletes: using MR imaging measurements to compare extent of muscle injury with amount of time lost from competition. AJR American journal of roentgenology. 2002;179(6):1621–1628. doi: 10.2214/ajr.179.6.1791621. [DOI] [PubMed] [Google Scholar]
- 58.Verrall GM, Slavotinek JP, Barnes PG, Fon GT, Esterman A. Assessment of physical examination and magnetic resonance imaging findings of hamstring injury as predictors for recurrent injury. The Journal of orthopaedic and sports physical therapy. 2006;36(4):215–224. doi: 10.2519/jospt.2006.36.4.215. [DOI] [PubMed] [Google Scholar]
- 59.Warren P, Gabbe BJ, Schneider-Kolsky M, Bennell KL. Clinical predictors of time to return to competition and of recurrence following hamstring strain in elite Australian footballers. British journal of sports medicine. 2010;44(6):415–419. doi: 10.1136/bjsm.2008.048181. [DOI] [PubMed] [Google Scholar]
- 60.Wetzel RJ, Patel RM, Terry MA. Platelet-rich plasma as an effective treatment for proximal hamstring injuries. Orthopedics. 2013;36(1):e64–e70. doi: 10.3928/01477447-20121217-20. [DOI] [PubMed] [Google Scholar]
- 61.Wong MW, Tang YN, Fu SC, Lee KM, Chan KM. Triamcinolone suppresses human tenocyte cellular activity and collagen synthesis. Clinical orthopaedics and related research. 2004;(421):277–281. doi: 10.1097/01.blo.0000118184.83983.65. [DOI] [PubMed] [Google Scholar]
- 62.Wong MW, Tang YY, Lee SK, Fu BS. Glucocorticoids suppress proteoglycan production by human tenocytes. Acta orthopaedica. 2005;76(6):927–931. doi: 10.1080/17453670610046118. [DOI] [PubMed] [Google Scholar]
- 63.Zissen MH, Wallace G, Stevens KJ, Fredericson M, Beaulieu CF. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR American journal of roentgenology. 2010;195(4):993–998. doi: 10.2214/AJR.09.3674. [DOI] [PubMed] [Google Scholar]