Abstract
Few studies have examined the association between ambient temperature and cognitive function, or used exposure to temperature at a given address instead of a single stationary monitor. The existing literature on the temperature-cognition relationship has mostly consisted of experimental studies that involve a small sample size and a few specific temperature values. In the current study, we examined the association between residential air temperature and Mini-Mental State Examination (MMSE) scores, a quantitative measurement of cognitive function, in a longitudinal cohort of elderly men. Residential air temperature was estimated by a novel spatiotemporal approach that incorporates satellite remote sensing, land use regression, meteorological variables and spatial smoothing in the Northeastern USA. We then applied logistic regression generalized estimating equations to examine the relationship between residential temperature (range: −5.8~25.7 degrees C), and the risk of low MMSE scores (MMSE scores ≤ 25) among 594 elderly men (1,085 visits in total) from the Veterans Affairs Normative Aging Study, 2000–2008. Sensitivity analysis on visits wherein subjects lived within 30 km of the clinic center in Massachusetts or aged ≥ 70 years was also evaluated. A statistically significant, U-shaped association between residential air temperature and low MMSE score (p-value = 0.036) was observed. Sensitivity analysis suggested that the estimated effect remains among individuals aged ≥ 70 years. In conclusion, the data suggest that risk of low MMSE scores is highest when temperature is either high or low, and lowest when ambient temperature is approximately within 10–15 degrees C in a cohort of elderly men. Further research is needed to confirm our findings and assess generalizability to other populations.
Keywords: cognitive function, residential air temperature, mini-mental state examination, elderly, spatiotemporal model
Introduction
In the era of population aging, impairment in cognitive function among elderly people is a global burden (Ferri et al., 2005). Cognitive declines in the elderly are associated with fall risk, nursing home admission, hospitalization, congestive heart failure, and mortality (Almeida and Flicker, 2001; Bassuk et al., 2000; Chodosh et al., 2004; Gaugler et al., 2007; Muir et al., 2012). Studies also reported that elderly people are at an increased risk of morbidity and mortality during heat waves (Bobb et al., 2014; Gronlund et al., 2014; Knowlton et al., 2009). It is possible that short-term temperature-related cognitive declines contribute to this increased risk. For instance, temperature-induced declines in cognition may lead to poor decision-making ability and executive function (Muller et al., 2012; Racinais et al., 2008). Hence the elderly may not be aware of the need of cooling, hydration, or escaping the heat and put themselves at an elevated risk of danger during heat waves.
There is convincing evidence that cognitive function can be affected by environmental factors, such as air pollution, sunlight, and greenness (Kent et al., 2009; Power et al., 2011; Salthouse, 2013; Wells, 2000). Researchers have examined the relationship between cognitive function and temperature, but the findings are mixed: some found worse cognition related to cold or heat, while others did not observe any change (Leavitt et al., 2012; Muller et al., 2012; O’Brien et al., 2007; Pilcher et al., 2002; Racinais et al., 2008; Schlader et al., 2015). In addition, most of the published work consisted of experimental studies in which the sample size was small and/or only a few specific values of temperature were inspected (Makinen et al., 2006; Muller et al., 2012; Racinais et al., 2008). The association of cognitive function with temperature, especially temperature across a wide range, is still unclear.
Elderly people are very likely to spend most of their time at their residence. Therefore, it is crucial to understand how residential temperature plays a role in their health. A recent study demonstrated that temperature at a subject’s residential address had far stronger associations with birth outcomes than temperature from an airport monitor (Kloog et al., 2015). In the current study, we used a novel spatiotemporal approach to estimate short-term exposure to residential air temperature for participants from the Normative Aging Study, and analyzed the relationship between residential air temperature and cognitive function. To the best of our knowledge, this study, for the first time, provides evidence on the association of air temperature with cognitive function in a large sample with repeated measures.
1. Material and methods
1.1 Study sample
The Veterans Affairs Normative Aging Study (NAS) was established in 1963 by the Department of Veterans Affairs, and is an ongoing longitudinal study of aging that enrolled 2,280 community-dwelling, healthy men living in the Greater Boston area (Bell et al., 1972). Participants were free of known chronic medical conditions at enrollment and have undergone examinations every 3 to 5 years. Beginning in 1984, all exams were conducted at 3 year intervals; starting in 1993, these exams included the Mini-Mental State Examination (MMSE) as a cognitive assessment. All participants provided written informed consent. This study was reviewed and approved by the Institutional Review Boards of all participating institutions.
We restricted study subjects to those who completed cognitive testing at least once and whose home address was available for us to estimate residential temperature from the spatiotemporal model between 2000 and 2008. In total, 594 subjects with 1,085 visits were included in this study. 225 (37.9%) of the individuals had one visit, 247 (41.6%) had two visits, and 122 (20.5%) had three during the study period.
1.2 Cognitive function
In the study, cognitive function was measured by the Mini-Mental State Examination (MMSE). The MMSE contains questions on attention, arithmetic, language use, comprehension, etc. It is commonly used in clinical and research settings as a tool to quantitatively assess cognitive impairment and to screen for dementia (Tombaugh and McIntyre, 1992). Subjects had the MMSE test at every visit. That is, there were 1,085 assessments on 594 individuals in this study.
1.3 Spatiotemporal assessment of residential temperature
A novel spatiotemporal approach that incorporates satellite remote sensing, land use regression, meteorological variables and spatial smoothing was used to generate temperature data in the Northeastern USA. Details can be found elsewhere (Kloog et al., 2012; Kloog et al., 2014). Briefly, mixed-effects regression was used to calibrate Moderate Resolution Imaging Spectroradiometer (MODIS) surface temperature with monitored air temperature on a daily basis. Because surface temperature may be unavailable due to cloud cover or retrieval errors, we additionally used a generalized additive mixed model with land use terms, local monitoring data, and spatial smoothing to obtain surface temperature estimates. We then applied out-of-sample 10-fold cross-validation to assess the accuracy of the predictions. Our prediction model performance was excellent for days with surface temperature observations as well as for days without (mean out-of-sample R2 = 0.946 and R2 = 0.941, respectively).
We linked each subject’s home address with the spatiotemporal model within 1 × 1 km to estimate 24-hour mean temperature at residence for the study period 2000–2008. Exposure was defined as the mean temperature on the day of each examination or the preceding few days.
1.4 Statistical analysis
Typically, a score ≤ 24 in the MMSE test is used to suggest a positive screen for dementia. Few subjects in our study had MMSE scores below that level, so we created a binary indicator for low MMSE scores (defined as scores ≤ 25) as previous studies did so (Power et al., 2011). We dichotomized the MMSE score and analyzed the risk of low scores versus high scores in part of because of the ceiling effect of MMSE (Tombaugh and McIntyre, 1992). We conducted logistic regression with generalized estimating equations (GEE) to examine the association between residential temperature and low MMSE scores (Liang and Zeger, 1986), with an exchangeable covariance. In the final model, we adjusted for the following covariates measured at each visit: age (continuous), education (< 12, 12–16, > 16 years), alcohol consumption (≥ 2 drinks/day, < 2 drinks/day), body mass index (BMI, computed as weight [in kilograms] divided by height [in square meters]), smoking status (never, former, current smoker), dark fish consumption (≥ 1 time/week, < 1 time/week), physical activity (< 12, 12 to < 30, ≥ 30 metabolic equivalent hours per week), computer experience (yes, no), English as first language (yes, no), percentage of census tract that is nonwhite (continuous), percentage of census tract ≥ 25 years of age with a Bachelor’s degree or higher (continuous), and season (spring: March–May, summer: June–August, fall: September–November, winter: December–February) (Power et al., 2011; Power et al., 2013).
We hypothesize that temperature may have adverse effects on cognitive function when the weather is cold or hot. Therefore, we included a quadratic term of temperature to allow for this pattern. Because study participants visited the Veterans Affairs clinic center in Boston in the morning after an overnight fast and abstinence from smoking, we took temperature on the previous day before visit, i.e., lag 1 day’s temperature, as the exposure metric. In addition, we performed a sensitivity analysis on people who lived within 30 km of the clinic center (accounted for 62% of all visits) in Massachusetts, as it is likely that those who lived far away were not at home but rather on the way to the clinic center on lag 1 day. A sensitivity analysis among men aged ≥ 70 years old (accounted for 75% of all visits) was also conducted.
Data management was performed with SAS 9.3 (SAS Institute Inc.), and data analysis was performed with R 3.1.2 (http://www.r-project.org/).
2. Results
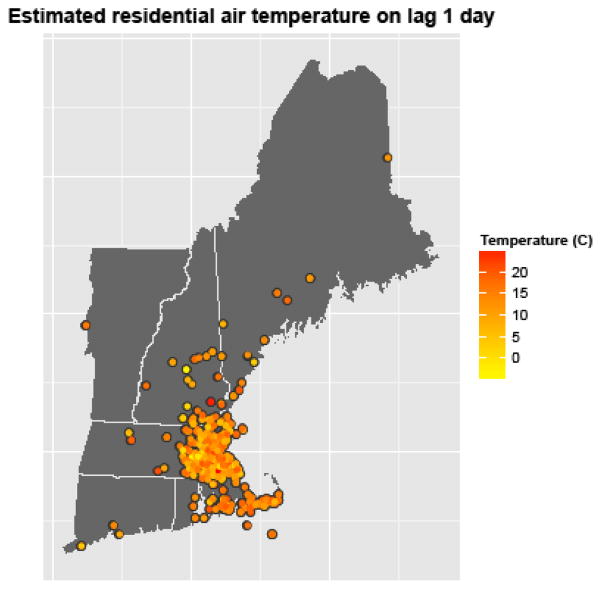
Table 1 summarizes the baseline characteristics of the study sample. At baseline, a total of 89 subjects (15%) had a low MMSE score. The mean age was 73 (SD = 7) years old, and the mean BMI was 28.1 (SD = 4.0) kg/m2. Men in the study (72.6%) had 12 to 16 years of education. The estimated temperature at residence on lag 1 day is shown in Figure 1. Subjects usually had visits during mild weather – estimated temperature ranged from −5.8 to 25.7 degrees C in our study.
Table 1.
Baseline characteristics of the study subjects (n = 594), 2000–2008.
| Continuous | Mean ± SD |
|---|---|
| Age (years) | 73.0 ± 6.7 |
| BMI (kg/m2) | 28.1 ± 4.0 |
| Nonwhite (percentage of census tract) | 11.1 ± 13.0 |
| ≥ 25 years of age with a Bachelor’s degree or higher (percentage of census tract) | 37.8 ± 16.9 |
| Categorical | Number (%) |
| Low MMSE score | |
| Yes | 89 (15.0) |
| No | 505 (85.0) |
| Years of education | |
| < 12 | 22 (3.7) |
| 12–16 | 431 (72.6) |
| > 16 | 141 (23.7) |
| Smoking status | |
| Never | 174 (29.3) |
| Current | 24 (4.0) |
| Former | 396 (66.7) |
| Alcohol consumption (drinks/day) | |
| ≥ 2 | 119 (20.0) |
| < 2 | 475 (80.0) |
| Physician-diagnosed diabetes mellitus | |
| Yes | 77 (13.0) |
| No | 517 (87.0) |
| Physical activity (MET-hour/week) | |
| < 12 | 388 (65.3) |
| 12 to < 30 | 120 (20.2) |
| ≥ 30 | 86 (14.5) |
| Dark fish consumption (times/week) | |
| < 1 | 450 (75.8) |
| ≥ 1 | 144 (24.2) |
| First language | |
| Not English | 55 (9.3) |
| English/bilingual | 539 (90.7) |
| Computer experience | |
| Yes | 321 (54.0) |
| No | 273 (46.0) |
Figure 1.
Estimated 24-hour mean temperature at residence on the previous day of examination. Examination dates can differ from subject to subject. Each dot represents a home address. If one changed his address during the study period, there will be a new dot for each of his new addresses.
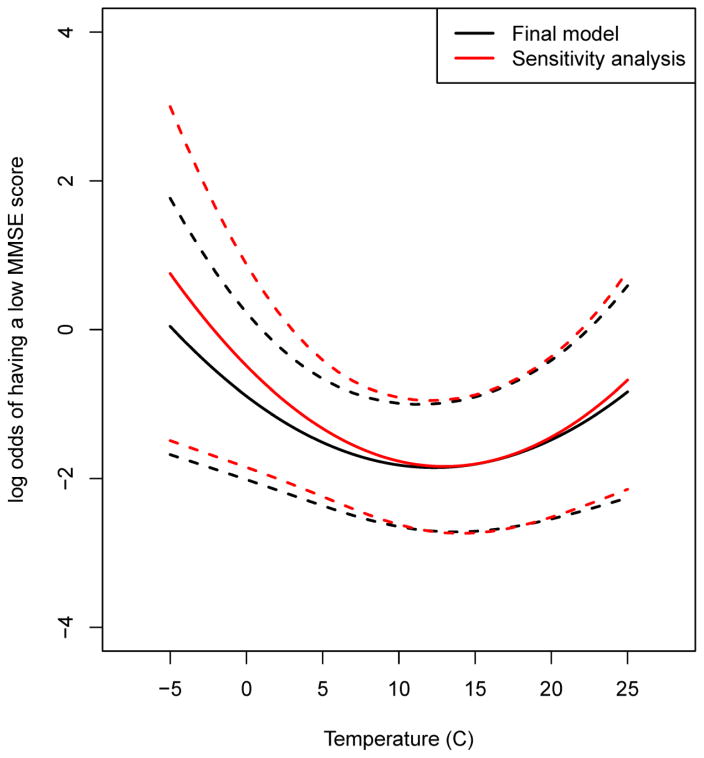
Table 2 shows the estimated coefficients of temperature in main model and in sensitivity analyses. We found that in all the models, temperatures were statistically significant (all p-values < 0.05) based on ANOVA F tests (i.e., temperature terms inclusive versus no temperature). This suggests a significant, U-shaped association between residential air temperature and the risk of having a low MMSE score. In the sensitivity analysis where we restricted to subjects living within 30 km of the clinic center in Massachusetts or those aged ≥ 70 years, the quadratic coefficient, which determines the slope of its derivative, was estimated to be larger than that in the main model (0.010 and 0.008, respectively, in sensitivity analyses versus 0.006 in main model).
Table 2.
Estimated coefficients of linear and quadratic terms of temperature.
| Model | Linear temperature | Quadratic temperature | p-valuec |
|---|---|---|---|
| Main modela | −0.16 | 0.006 | 0.036 |
| Sensitivity analysisb | |||
| Living within 30 km | −0.24 | 0.010 | 0.004 |
| Aged ≥ 70 years | −0.21 | 0.008 | 0.048 |
Adjusted for age, education, alcohol consumption, BMI, smoking, dark fish consumption, physical activity, computer experience, first language, percentage of census tract that is nonwhite, percentage of census tract ≥ 25 years of age with a Bachelor’s degree or higher, and season.
Adjusted for the same covariates as the main model, but restricted to men who lived within 30 km of the clinic center in Massachusetts or those aged ≥ 70 years.
P-values for temperature terms were calculated from ANOVA F tests.
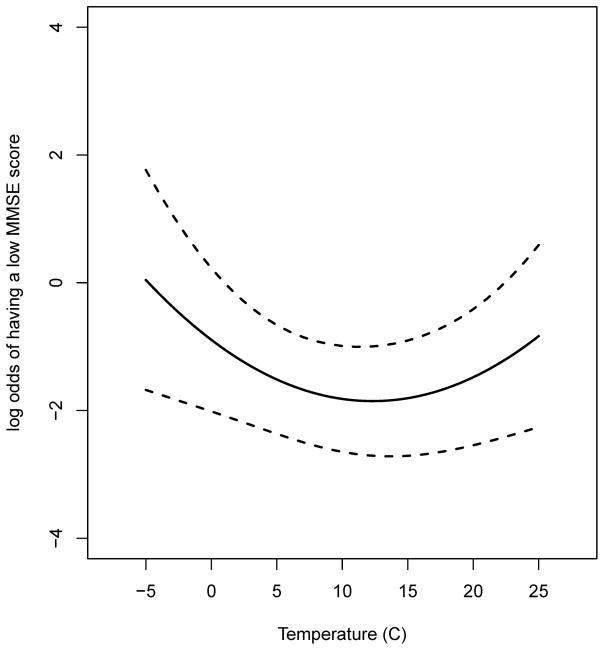
The estimated association and the corresponding 95% confidence interval between residential air temperature and the risk of low MMSE scores are illustrated in Figure 2. We observed that the log odds of low MMSE scores are minimal when temperature is approximately within 10 – 15 degrees C, and are expected to increase when temperature is away from the range.
Figure 2.
Relationship between temperature and log odds of having a low MMSE score in the model.
Figure 3 shows the relationship between air temperature and risk of low MMSE scores among men aged ≥ 70 years. The curve for those men appeared to have steeper slopes at both sides of temperature, especially at low temperatures.
Figure 3.
Association of low MMSE scores with temperature in the sensitivity analysis among subjects aged ≥ 70 years.
3. Discussion and conclusions
In this study, we estimated the effects of residential air temperature and cognitive function in a longitudinal cohort of elderly men. We applied multivariable logistic GEEs and found that residential air temperature was significantly associated with low MMSE scores. Particularly, the risk of low MMSE scores was small when temperature was moderate, and higher when temperature was either high or low.
Most of the existing studies examined a few of temperature points, few ever looked at the relationship between cognitive function and temperature within a wide range. The pattern of the temperature-cognition relationship we have observed is consistent with a previous meta-analysis, which found that hot and cold exposures were negatively associated with performance on cognitive tasks based on 317 experimental participants from 22 studies (Pilcher et al., 2002). Experimental studies usually went for a few hours, and were labelled as short duration (< 2 hours) or long duration (≥ 2 hours) in the meta-analysis. The meta-analysis showed a weaker temperature-cognition association for long duration and the authors argued that people may to some extent adapt to extreme temperatures and improve their performance over time. In the current study, we used a novel exposure metric, 24-hour mean temperature on lag 1 day, and found a significant U-shaped association. Pilcher and co-authors (2002) also reported that exposure to hot temperatures of ≥ 32 degrees C and cold temperatures of ≤ 10 degrees C resulted in the greatest decrement in cognitive performance. Temperature in the current study ranged from −5.8 to 25.7 degrees C. Although we were unable to evaluate the nature of the temperature-cognition relationship beyond this range, the data may suggest a trend that the strength of association would continue to increase at either higher or lower temperatures (see Figure 1).
Aging is associated with declines in cognitive function (Blazer et al., 2015; Drag and Bieliauskas, 2010). For example, Schlader et al. (2015) observed age-related differences in processing speed, memory, and executive function when comparing elderly subjects to middle-aged subjects. In the sensitivity analysis, we restricted to subjects aged ≥ 70 years and found that the temperature-cognition relationship remained significant and showed a similar shape in those subjects. This suggests that there still exists a link between temperature and cognitive function among subjects who might already have aging-associated cognition declines.
Many studies have observed a J- or U-shaped temperature-mortality relationship (Basu and Samet, 2002). Our finding that there is a U-shaped association between residential air temperature and cognition may provide an explanation: temperature-induced declines in cognitive functions can cause poor decision-making ability and executive function, thus people, especially the elderly, may not be aware of the need of adjusting temperature, or avoiding temperature extremes and put themselves at an increased risk of mortality.
Heat exposure
Studies that investigated the association between heat exposure and cognitive function have provided inconsistent findings. In a study by Racinais et al. (2008), 16 middle-aged individuals were randomly assigned to a two hour exposure to a control condition (room temperature set at 20 degrees C), a hot condition (room temperature set at 50 degrees C), or a hot head cool condition (room temperature set at 50 degrees C with cool packs applied to the head and neck), and performed cognitive tests on attention and working memory. Compared to those in the control condition, people in the hot condition had significant declines in performance on working memory tests, but not on attention tests. In a randomized crossover study that included 15 elderly and 14 middle-aged healthy individuals, passive heat stress, induced by perfusing 48 degrees C water through the suit for 40–60 minutes and sufficient to increase subjects’ internal temperature by 1.0–1.6 degrees C, did not affect performance of cognitive tests on attention, memory, and execution function in either group (Schlader et al., 2015). However, Leavitt et al. (2012) reported that warmer outdoor temperature was linked to worse cognitive status (i.e., slowed processing speed and learning/memory problems) in persons with multiple sclerosis in a cross-sectional analysis (No. of patients included = 40) and in a longitudinal analysis (No. of patients included = 45). Research on the underlying mechanisms are rare. A more recent study by those authors has examined the underlying neurophysiological mechanisms for the temperature-cognition relationship (Leavitt et al., 2014), but among people with multiple sclerosis (MS). Briefly, 28 middle-aged MS patients underwent brain scans using functional magnetic resonance imaging (fMRI). The authors collected data on mean outdoor temperature and subjects’ blood-oxygen-level dependent (BOLD) activation, a signal of neural activity, during performance of a simple sustained attention task. Range of outdoor temperature, measured by a local station, was between −5.6 to 26.7 degrees C. They found that warmer outdoor temperature was associated with greater BOLD activation in frontal and parietal regions of cerebral cortex among the subjects.
Cold exposure
There have been a few experimental studies on cold exposure and cognition. The results were also mixed. In a study that examined the association between repeated exposures to cold and cognition, 10 young healthy men performed cognitive tests under control conditions (mean temperature 25 degrees C) for 90 minutes and in cold exposure (mean temperature 10 degrees C) for 120 minutes during a 10-day study period (Makinen et al., 2006). Cognitive function was assessed by various tests including code substitution, logical reasoning, matching-to-sample, recall, simple reaction time, and memory test. The authors observed both improvement and impairment in cognitive performance. In Marrao et al. (2005), 28 healthy male aircrew participated in 9-day military cold weather training, in which mean air temperature ranged from −24.4 to 4.4 degrees C. The authors measured subjects’ cognitive performance with regard to logical reasoning, planning, and vigilance, but they did not observe any significant declines. A recent study exposed 10 healthy male college students to cold air at 10 degrees C for two hours (Muller et al., 2012). Cognitive function was evaluated with four tasks: digit span (an index of working memory), choice reaction time, executive function, and maze navigation. The authors found that performance in the former three cognitive tasks declined during cold exposure. Interestingly, the authors argued that timed tasks such as a working memory task might be affected more by cold temperature than non-timed tasks such as maze navigation. In another experimental study, 10 male enlisted soldiers underwent cooling in cold water until their core temperature fell to 35.5 degrees C or after a maximum of four hours, and then proceeded to the cold air exposure at 10 degrees C (O’Brien et al., 2007). The researchers found that cognitive performance, measured by a series of tests on spatial memory and pattern recognition, complex reaction time, logical reasoning, visual vigilance, simple calculations, and repeated acquisition, can be maintained despite moderate core cooling.
To sum it up, most of the existing studies on the temperature-cognition relationship were experimental studies that typically exposed a small number of subjects to a few specific temperatures for several hours and evaluated subjects’ performance on cognitive tasks during the exposure. The very few epidemiological studies, like Leavitt et al. 2012, measured outdoor temperature from a local weather station. Furthermore, results were mixed.
The differences in findings aforementioned may be attributed to several reasons. First, characteristics of the study population, such as age and occupation, differed. For example, aircrew and soldiers enrolled in the studies of Marrao et al. and O’Brien et al. could be stronger and healthier than the college students in the study by Muller et al., and thus may be more resistant to severe temperatures. Second, the way in which the subjects were exposed and how long they were exposed mattered. Last but not least, cognitive tasks of different types and durations could be affected by temperature differentially.
The underlying biological mechanisms for the temperature-cognition relationship are not well understood yet. Leavitt et al. (2014) found that warmer outdoor temperature was linked with greater BOLD activation in frontal and parietal regions of cerebral cortex among subjects with multiple sclerosis. Furthermore, it is established that temperature affects hippocampal neural activities that are crucial for brain functions like learning and memory; for example, a study that examined the effects of body temperature on neural activity in the hippocampus on the molecular level found that TRPV4 (transient receptor potential vanilloid 4), a thermosensitive transient receptor potential channel, is constitutively activated by heat and controls hippocampal neurons’ excitability (Malenka and Nicoll, 1999; Shibasaki et al., 2007). In addition, people are less comfortable in both hot and cold temperatures, and this may flow through to cognitive function via multiple pathways.
Our study has several strengths. First, experimental studies set temperature at such a few specific values that they cannot show how cognitive function would change within a wide range of temperature, while epidemiological studies usually obtain air temperature data from meteorological stations and hence the spatial coverage is a big concern. Instead, we estimated residential temperature spatially and temporally for all the subjects. Second, unlike the experimental studies that typically exposed participants to certain temperature for a few hours and assessed their cognitive performance during exposure, the current study examined cognitive function linked with a novel exposure metric – 24-hour mean temperature a day before the cognitive test. This provides new insight into the temperature-cognition relationship and may demonstrate that the estimated effects of temperature on cognitive function can be lagged. Third, we applied logistic GEEs to analyze the data. A GEE model has several advantages over other methods (e.g., the generalized linear mixed model): using robust variance estimation, it provides consistent estimates even with mis-specified correlation structure and does not require one to make assumptions about the full joint distribution of the longitudinal measurements (Liang and Zeger, 1986; Overall and Tonidandel, 2004). Other strengths included the repeated measures, multivariable adjustment, relatively large study sample, and long-time follow-up. To the best of our knowledge, this is the first study that estimates the effects of air temperature on cognitive function in a large longitudinal sample.
On the other hand, the limitations of the study cannot be ignored. The MMSE test may fail to detect changes in people with established advanced dementia or poor education (known as floor effects); also, it may be unable to differentiate mild illness and mild/moderate cognitive impairment in well educated people (known as ceiling effects) (Tombaugh and McIntyre, 1992). Since our study sample had a relatively high education level, our study could have MMSE ceiling effects which can lower test sensitivity (Franco-Marina et al., 2010). We have controlled for age and education, but some concerns remain. Using a noisy outcome with lower sensitivity would be expected to reduce the likelihood of finding an association. Although we used a novel spatiotemporal model to estimate air temperature at each subject’s home address, we lacked information on indoor temperature. It is possible that subjects used heating or air conditioning and hence indoor temperature differed from the estimated residential air temperature. Moreover, we did not have information on subjects’ activity on lag 1 day and simply assumed that the elderly spent most of the time at home. As mentioned earlier, we did not have visits at extreme temperatures (range of observed temperature: −5.8 ~ 25.7 degrees C), so we are unable to reveal the temperature-cognition relationship under such conditions. It is possible that under extreme temperatures, people who were cognitively impaired were less likely to make a visit. Further work on extreme temperature and cognition is needed. Still, our study could be informative as it covers temperatures that people could be exposed to during daily life. Furthermore, the spatial resolution of temperature used in the current study was 1 × 1 km. There could be non-differential measurement errors that would bias the results towards the null. Last, all of the study participants were elderly men living in the Northeastern US, and most of them were Caucasian. One should be cautious when generalizing our findings to other populations or areas.
In conclusion, we used a novel spatiotemporal approach to estimate short-term exposure to ambient temperature at residence and conducted multivariable logistic GEEs to examine the relationship between residential temperature and the risk of low MMSE scores in a large longitudinal cohort of elderly men. Our results suggest a U-shaped relationship between cognitive function and residential temperature: either low or high temperature is associated with an increased risk of impairment in cognitive function. The association among individuals aged ≥ 70 years may be stronger. Additional research is needed to confirm our findings and assess generalizability to other populations, such as females, younger people, and other ethnic groups.
Highlights.
A novel spatiotemporal approach was used to estimate short-term exposure to air temperature at each subject’s residence.
We found a significant, U-shaped association between residential air temperature and low Mini-Mental State Examination (MMSE) score, a quantitative measurement of cognitive function.
The temperature-cognition relationship remains in subjects aged ≥ 70 years.
Acknowledgments
Funding Information
This study was supported by the National Institute of Environmental Health Sciences grants ES00002 and ES015172-01, and the U.S. Environmental Protection Agency grant RD-834798-01. Dr. David Sparrow was supported by a VA Research Career Scientist Award.
Dr. Avron Spiro was supported by a VA CSR&D Senior Research Career Scientist Award. The VA Normative Aging Study is supported by the Cooperative Studies Program/Epidemiology Research and Information Centers of the U.S. Department of Veterans Affairs and is a component of the Massachusetts Veterans Epidemiology Research and Information Center, Boston, Massachusetts. Disclaimers: The contents are solely the responsibility of the grantee and do not necessarily represent the official views of the funders. Further, the funders do not endorse the purchase of any commercial products or services mentioned in the publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Almeida OP, Flicker L. The mind of a failing heart: a systematic review of the association between congestive heart failure and cognitive functioning. Intern Med J. 2001;31:290–5. doi: 10.1046/j.1445-5994.2001.00067.x. [DOI] [PubMed] [Google Scholar]
- Bassuk SS, et al. Cognitive impairment and mortality in the community-dwelling elderly. Am J Epidemiol. 2000;151:676–88. doi: 10.1093/oxfordjournals.aje.a010262. [DOI] [PubMed] [Google Scholar]
- Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev. 2002;24:190–202. doi: 10.1093/epirev/mxf007. [DOI] [PubMed] [Google Scholar]
- Bell B, et al. The Normative Aging Study: an interdisciplinary and longitudinal study of health and aging. Aging Hum Dev. 1972;3:4–17. [Google Scholar]
- Blazer DG, et al. Cognitive aging: a report from the Institute of Medicine. Jama. 2015;313:2121–2. doi: 10.1001/jama.2015.4380. [DOI] [PubMed] [Google Scholar]
- Bobb JF, et al. Cause-specific risk of hospital admission related to extreme heat in older adults. Jama. 2014;312:2659–67. doi: 10.1001/jama.2014.15715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chodosh J, et al. Cognitive decline in high-functioning older persons is associated with an increased risk of hospitalization. J Am Geriatr Soc. 2004;52:1456–62. doi: 10.1111/j.1532-5415.2004.52407.x. [DOI] [PubMed] [Google Scholar]
- Drag LL, Bieliauskas LA. Contemporary review 2009: cognitive aging. J Geriatr Psychiatry Neurol. 2010;23:75–93. doi: 10.1177/0891988709358590. [DOI] [PubMed] [Google Scholar]
- Ferri CP, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366:2112–7. doi: 10.1016/S0140-6736(05)67889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franco-Marina F, et al. The Mini-mental State Examination revisited: ceiling and floor effects after score adjustment for educational level in an aging Mexican population. Int Psychogeriatr. 2010;22:72–81. doi: 10.1017/S1041610209990822. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, et al. Predicting nursing home admission in the U.S: a meta-analysis. BMC Geriatr. 2007;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronlund CJ, et al. Heat, heat waves, and hospital admissions among the elderly in the United States, 1992–2006. Environ Health Perspect. 2014;122:1187–92. doi: 10.1289/ehp.1206132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kent ST, et al. Effect of sunlight exposure on cognitive function among depressed and non-depressed participants: a REGARDS cross-sectional study. Environ Health. 2009;8:34. doi: 10.1186/1476-069X-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kloog I, et al. Temporal and spatial assessments of minimum air temperature using satellite surface temperature measurements in Massachusetts, USA. Sci Total Environ. 2012;432:85–92. doi: 10.1016/j.scitotenv.2012.05.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kloog I, et al. Using Satellite-Based Spatiotemporal Resolved Air Temperature Exposure to Study the Association between Ambient Air Temperature and Birth Outcomes in Massachusetts. Environ Health Perspect. 2015 doi: 10.1289/ehp.1308075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kloog I, et al. Predicting spatiotemporal mean air temperature using MODIS satellite surface temperature measurements across the Northeastern USA. Remote Sensing of Environment. 2014;150:132–139. [Google Scholar]
- Knowlton K, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009;117:61–7. doi: 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leavitt VM, et al. Warmer outdoor temperature is associated with worse cognitive status in multiple sclerosis. Neurology. 2012;78:964–8. doi: 10.1212/WNL.0b013e31824d5834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leavitt VM, et al. Warmer outdoor temperature is associated with task-related increased BOLD activation in patients with multiple sclerosis. Brain Imaging Behav. 2014;8:128–32. doi: 10.1007/s11682-013-9267-7. [DOI] [PubMed] [Google Scholar]
- Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Makinen TM, et al. Effect of repeated exposures to cold on cognitive performance in humans. Physiol Behav. 2006;87:166–76. doi: 10.1016/j.physbeh.2005.09.015. [DOI] [PubMed] [Google Scholar]
- Malenka RC, Nicoll RA. Long-term potentiation--a decade of progress? Science. 1999;285:1870–4. doi: 10.1126/science.285.5435.1870. [DOI] [PubMed] [Google Scholar]
- Marrao C, et al. Physical and cognitive performance during long-term cold weather operations. Aviat Space Environ Med. 2005;76:744–52. [PubMed] [Google Scholar]
- Muir SW, et al. The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age Ageing. 2012;41:299–308. doi: 10.1093/ageing/afs012. [DOI] [PubMed] [Google Scholar]
- Muller MD, et al. Acute cold exposure and cognitive function: evidence for sustained impairment. Ergonomics. 2012;55:792–8. doi: 10.1080/00140139.2012.665497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien C, et al. Cognitive, psychomotor, and physical performance in cold air after cooling by exercise in cold water. Aviat Space Environ Med. 2007;78:568–73. [PubMed] [Google Scholar]
- Overall JE, Tonidandel S. Robustness of Generalized Estimating Equation (GEE) Tests of Significance against Misspecification of the Error Structure Model. Biometrical Journal. 2004;46:203–213. [Google Scholar]
- Pilcher JJ, et al. Effects of hot and cold temperature exposure on performance: a meta-analytic review. Ergonomics. 2002;45:682–98. doi: 10.1080/00140130210158419. [DOI] [PubMed] [Google Scholar]
- Power MC, et al. Traffic-related air pollution and cognitive function in a cohort of older men. Environ Health Perspect. 2011;119:682–7. doi: 10.1289/ehp.1002767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power MC, et al. Modification by hemochromatosis gene polymorphisms of the association between traffic-related air pollution and cognition in older men: a cohort study. Environ Health. 2013;12:16. doi: 10.1186/1476-069X-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racinais S, et al. Hyperthermia impairs short-term memory and peripheral motor drive transmission. J Physiol. 2008;586:4751–62. doi: 10.1113/jphysiol.2008.157420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salthouse TA. Within-cohort age-related differences in cognitive functioning. Psychol Sci. 2013;24:123–30. doi: 10.1177/0956797612450893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlader ZJ, et al. Cognitive and perceptual responses during passive heat stress in younger and older adults. Am J Physiol Regul Integr Comp Physiol. 2015;308:R847–54. doi: 10.1152/ajpregu.00010.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibasaki K, et al. Effects of body temperature on neural activity in the hippocampus: regulation of resting membrane potentials by transient receptor potential vanilloid 4. J Neurosci. 2007;27:1566–75. doi: 10.1523/JNEUROSCI.4284-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tombaugh TN, McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc. 1992;40:922–35. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- Wells NM. At Home with Nature: Effects of “Greenness” on Children’s Cognitive Functioning. Environment and Behavior. 2000;32:775–795. [Google Scholar]