Abstract
Objective
Data from a toddler screening study were used to examine: 1) categories of concerns regarding the development of their child reported by parents prior to diagnostic evaluation, 2) congruence of parent concerns with their child’s later diagnosis, 3) the extent to which parent concern(s) were associated with the therapies their child received and types of specialists consulted, and 4) the association between the number of parental concern categories and clinical measures.
Methods
Toddlers who screened positive for autism spectrum disorder (ASD) during well-child check-ups received a diagnostic evaluation and parents completed a history questionnaire (n=532; 274 ASD, 258 non-ASD). Parents’ concerns about their child’s development, therapy received, and specialists consulted were coded into discrete categories.
Results
Most parents (>90%) reported concerns about their child’s development. The most common concern in both the ASD and non-ASD groups was speech/communication (78.6%). Significant differences were found between diagnostic groups in the speech/communication, restricted/repetitive behaviors, social, behavioral, and medical concern categories. Parent concerns were associated with therapies received and specialists consulted. The number of concern categories was positively associated with several ASD scores.
Conclusions
The developmental concerns expressed by parents of undiagnosed toddlers were highly consistent with the diagnosis the child later received. Based in part on their areas of concern, parents made contact with the appropriate professionals and their children received some therapy prior to diagnosis. Finally, parents who reported concerns across different areas endorsed more symptoms during screening. Results emphasize the need for providers to elicit and take seriously parent concerns during the referral and diagnostic processes.
Keywords: autism spectrum disorder (ASD), screening, parent concerns
BACKGROUND
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by significant social, communication, and behavioral deficits.1 According to the most recent prevalence estimate, 1 in 68 children is affected by ASD.2 There is now considerable evidence that ASD can be diagnosed before the third birthday,3,4 although the median age of diagnosis is still after the fourth birthday.2 Furthermore, it has been shown that children with early and intensive behavioral intervention (EIBI) have more improved developmental trajectories when compared to children without EIBI.5 This has led the American Academy of Pediatrics (AAP) to recommend a three-pronged approach consisting of routine, ongoing developmental surveillance, broad developmental screening at 9, 18, and 24/30 months, and universal ASD-specific screening at 18 and 24 months.6 It has been reported that 82% of pediatricians conduct routine developmental screenings,7 whereas compliance rates for autism specific screenings are only 55%;8 compliance with all three prongs of the AAP recommendations is less than 20%.9
Eliciting parents’ concerns about their child’s development is a key component of developmental surveillance.7 Most studies examining parents’ concerns look at how these concerns relate to a diagnosis of ASD,10-13 but few compare these concerns to children with other diagnoses. Severity of ASD has been shown to relate to earlier parent concern;3 similarly, increased ASD risk as measured by a screening questionnaire has predicted more autism-specific concerns.12 A previous study also examined the nature of the initial concern, as well as the age at which the concern was identified,14 but not what the concerned parents did to seek out help for their child.
Parents’ concerns about their child’s development usually emerge during the first two years of the child’s life.12,15,16 Among a sample of toddlers referred for an ASD evaluation based on screening at-risk, ASD-specific parental concerns were reported in 72% of toddlers with an older sibling with ASD, 81% of toddlers with a typical older sibling, and 57% of first-born children,16 indicating that ASD-specific concerns were found in all groups of children in the study. In many studies, language and communication problems are among the most common first concerns reported by parents,11,16 although another study reported social concerns as the first to occur.14 Type of first concerns reported differs according to the age at which the parent recognized the concern.17 Specifically, earlier concerns are more focused on communication and joint attention, whereas later concerns focus more on behavioral and motor differences.17,18
The current study examines the relationship between concerns parents reported and the diagnosis toddlers received in a sample of children who screened positive on an ASD screening questionnaire. Prior to learning about their child’s diagnosis, parents completed a history questionnaire. Open-ended responses eliciting their concerns regarding their child’s health and development were coded. Study hypotheses were: (1) parents of children subsequently diagnosed with ASD versus parents of children with a non-ASD diagnosis are more likely to report autism specific concerns regarding their child’s development, and more likely to have concerns across more concern categories, (2) concerned parents of both ASD and non-ASD diagnosed children are likely to seek intervention and specialist consultation for their child congruent with their concerns, and (3) the number of concern categories coded from parents’ questionnaires will relate to their child’s scores on screening and diagnostic measures.
METHODS
Participants
Archival data from two studies19,20 validating the Modified Checklist for Autism in Toddlers (M-CHAT)21 and its current revision (M-CHAT-R)22 were used for the current study. Low-risk toddlers were screened during 18- and 24-month well-child visits at participating pediatricians’ offices in metropolitan Atlanta and Connecticut. Children who screened positive on the M-CHAT(-R) were offered a free diagnostic evaluation. Parents were told by research staff that their child’s M-CHAT(-R) responses indicated signs of developmental delays and that a diagnostic evaluation would be beneficial. Risk of autism was not explicitly mentioned during these calls. The majority (62.2%) of children who screened positive completed the diagnostic evaluation (n= 471). Other reasons for evaluation include if the physician had ASD concerns regarding the child (n=33), the child screened positive on another screening tool (n=20), the parent expressed ASD concern (n=2). The reason for evaluation was missing from the record for six children. If the child attended the evaluation, the parents completed a history questionnaire prior to evaluation.
Inclusion criteria for the M-CHAT(-R) parent studies required toddlers to be screened during well-child check-ups. Children were excluded from the larger parent studies if: (1) they had an ASD diagnosis prior to screening, or (2) sensory or motor disabilities prevented them from completing the standardized assessment measures. For the current study participants were excluded if the child’s caregiver was not fluent in English. The history questionnaire did not contain information on whether or not a child received a diagnosis in between screening and diagnostic evaluation, therefore they could not be excluded from the study.
Of the 532 children who completed the diagnostic evaluation (70.1% male), the mean age at time of evaluation was 25.65 months (SD=4.73, range 16-43 months). Just over half of the toddlers (n=274; 51.5%) were subsequently diagnosed with ASD; the remaining participants were classified as non-ASD (n=258; 48.5%). Among the non-ASD group, 132 (51.16%) children were diagnosed with global development delay (GDD), 67 (26%) were diagnosed with language delay (LD), and 27 (10.5%) received another diagnosis; 32 children received no diagnosis (6% of the total sample). Please see Table 1 for additional child and parent demographics.
Table 1.
Parent and Child Characteristics from M-CHAT(-R) Validation Studies
| a: Child Characteristics
| ||
|---|---|---|
| Child Information | ASD (n=274) | Non-ASD (n=258) |
| Site [n(%)] | ||
| GSU | 170 (62.0%) | 125 (48.4%) |
| UConn | 104 (38%) | 133 (51.6%) |
| Sex [n(%)] | ||
| Male | 205 (74.8%) | 168 (65.1%) |
| Female | 69 (25.2%) | 90 (34.9%) |
| Mean Age at Evaluation in months (SD) | 25.9 (4.67) | 25.36 (4.78) |
| Mean Age of First Concern in months (SD) | 13.77 (6.5) | 11.43 (6.69) |
| Received Any Type of Therapy [n(%)] | 182 (66.4%) | 153 (59.3%) |
| Saw Any Type of Specialist [n(%)] | 144 (52.6%) | 114 (44.2%) |
| Mean M-CHAT Score (0-23) | 7.72 (4.17) | 5.52 (3.35) |
| Mean M-CHAT-R Score (0-20) | 6.50 (3.77) | 5.33 (2.88) |
| Mean ADOS Severity Score (0-10) | 6.18 (1.89) | 2.33 (1.53) |
| Mean CARS Score (15-60) | 32.38 (5.02) | 21.68 (3.19) |
|
| ||
| b: Parent demographics | ||
|
| ||
| Parent Information | Mother (n=445) | Father (n=413) |
|
| ||
| Mean Age (SD) | 32.35 (7.45) | 35.52 (7.96) |
| Race [n(%)] | ||
| Caucasian, Non-Hispanic | 200 (44.9%) | 184 (44.6%) |
| Other | 189 (42.5%) | 171(41.4%) |
| African American | 88 (19.8%) | 83 (20.1%) |
| Hispanic/Latino | 62 (13.9%) | 52 (12.6%) |
| Other | 39 (8.8%) | 36 (8.7%) |
| Education Level [n(%)] | ||
| 4-Year College Degree | 189 (42.4%) | 62 (15.0%) |
| Bachelor’s Degree | 115 (25.8%) | 36 (8.7%) |
| Graduate Degree | 74 (16.6%) | 26 (6.3%) |
| Less than 4-year Degree | 247 (55.5%) | 147 (35.6%)) |
| No degree or diploma | 65 (14.6%) | 31 (7.5%) |
| High school diploma/GED | 115 (25.8%) | 73 (17.7%) |
| Associates Degree or Technical Degree | 67 (15.1%) | 43 (10.4%) |
| Employment Status [n(%)] | ||
| Employed | 228 (51.2%) | 294 (71.2%) |
| Full Time | 105 (23.6%) | 128(30.1%) |
| Part-Time | 24 (5.4%) | 19 (4.6%) |
| Self Employed | 6 (1.3%) | 8 (1.9%) |
| Other | 93 (20.9%) | 139 (33.7%) |
| Unemployed | 130 (29.2%) | 50 (12.1%) |
Note. GSU- Georgia State University; UConn- University of Connecticut
Measures
All children were screened with the M-CHAT(-R), a 20-23-item yes/no questionnaire completed by parents. See validation studies for more information on M-CHAT(-R).19,20 Prior to receiving a diagnosis, parents completed a detailed history form, which included open-ended and forced choice questions used to gather information about socio-demographics, parent concerns, family history, pre- and perinatal history, developmental milestones, and medical history.
To assess parents’ concerns, three items were coded from the history questionnaire: “Please briefly list any concerns/worries you have about how the child has been developing (walking, speaking, playing) or behaving,” “Concerns about your child’s development,” and “What were the first things that made you concerned about your child’s development? How old was your child at that time?”
To assess whether or not children received therapy or saw a specialist, the following items were coded: “Has your child ever received any of the following: (list reasons on the back if not previously described): speech and/or language therapy, other therapies,” “Has your child been seen by any specialist? If yes identify which: Audiologist, Developmental Pediatrician, Geneticist, Neurologist, Occupational Therapist, Ophthalmologist, Physical Therapist, Psychiatrist, Psychologist, Speech/Language Pathologist, Other (please describe).”
Diagnosis
Evaluations were conducted by a team including a senior clinician (licensed psychologist or developmental pediatrician) and doctoral students in clinical psychology or a related field; all trainees were supervised by the senior clinician. The child’s diagnosis was ascertained by the best clinical estimate using DSM-IV criteria, which incorporated all available information from the evaluation. Diagnostic measures included the Autism Diagnostic Observation Schedule23 (ADOS), the Childhood Autism Rating Scales(-2)24 (CARS(-2)), and the Toddler Autism Symptom Interview (TASI).25 CARS(-2) was completed by the clinicians based on all available data from the evaluation, including behavioral observation, standardized testing, and parent report. If ASD was ruled out, diagnoses of language delay or global developmental delay were considered; if a child did not meet criteria for any developmental delay, they were classified as “No Diagnosis.” Cognitive, language, motor, and adaptive skills were measured with the Mullen Scales of Early Learning26 and the Vineland Adaptive Behavior Scales-II.27
Procedures
IRB approval was obtained at each university site; all parents gave written consent. Procedures for the parent study are reported in Chlebowski et al. (2013) and Robins et al. (2014). Open-ended responses from the history form were transcribed and the content was coded into concern categories, type of therapies the child received, and specialists consulted. Coding was completed by two independent coders; kappa values > 0.7 were achieved for all codes. Coding discrepancies were resolved by consensus from a team of experts.
In order to accurately assess differences in parents’ concerns, free text responses of concerns were coded into nine different concern categories, adapted from the work of Ozonoff and colleagues.12 The current study’s concern categories differed from those used by Ozonoff et al. in three ways: (a) separating out feeding/eating concerns from other medical/regulatory concerns; (b) including sensory concerns with stereotyped behavior concerns; and (c) combining general concerns with development concerns. ASD concerns included: (1) language/communication concerns, (2) restricted or repetitive behaviors (RRB), including sensory concerns, (3) social concerns, (4) parents who named “autism” in their concern. Non-ASD concerns included: (5) motor concerns other than repetitive motor behaviors, (6) behavior/temperament concerns, (7) medical/regulatory concerns, (8) feeding/eating concerns, and (9) developmental/unspecified concerns. Two summary concern categories were created for any ASD concern and any non-ASD concern. Specific examples and descriptions of each category can be seen in Appendix 1. If a parent indicated more than one type of concern, all categories in which they showed concerns were recorded yielding a total concern number between 0 and 9.
Categories for therapies and specialists were based on the most common responses from the history form. Categories of therapies used for analysis included speech therapy, physical therapy, and occupational therapy. Specialist categories used in analysis included audiologists, ophthalmologists/optometrists, and other professionals, including psychiatrists, psychologists, and geneticists. If a parent indicated that a child had seen a speech therapist, the child was coded as having had speech therapy.
Analyses
Preliminary analyses involved evaluation of raw and coded frequency distributions to determine the statistical characteristics of the data. To examine differences in the categories of concerns reported by parents of children with an ASD or a non-ASD diagnosis, chi-square analyses were conducted. To adjust for multiple analyses, a threshold of p=.01 was used for this analysis only. For other analyses a p-value threshold of .05 was used. Logistic regression was used to analyze if parental characteristics are associated with having any concern. Due to sample size, maternal race/ethnicity, paternal race/ethnicity, maternal education, and paternal education were collapsed into binary variables. To assess if there was a difference in the total number of distinct concern categories between the two parent groups, a two-sided t-test was conducted. To see if reporting of a concern was associated with receiving therapy or consulting a specialist, logistic regression analyses were conducted. Pearson correlations were calculated to assess the relationship between number of concerns and the number of therapies/specialists seen by the child, as well the correlation between number of concerns and M-CHAT(-R) scores, ADOS severity,28 and CARS total score. SPSS statistical software version 22 was used for all analyses.
RESULTS
Sample Characteristics
The mean age at diagnostic evaluation was 25.90 months (SD=4.67) for children with ASD and 25.36 months (SD=4.78) for children who were non-ASD, F(2,530)=.418, p=.174. Parents of children who were not diagnosed with ASD retrospectively reported that their concerns about their child began on average two months earlier (11.43 months, SD=6.69) than parents of children diagnosed with ASD (13.77 months, SD=6.50), F(2,316)=.001, p=.002. See Table 1.
Hypothesis 1: Differences in Parent Concern
In the total sample, only 7% of parents had no concerns. For parents who expressed one or more concerns, there were more than 80 combinations of concern categories reported. For parents who had one concern, the most common concern was speech (17%) followed by medical/regulatory (2.3%). For parents who had concerns in two categories, there were 20 different combinations of categories with the most common being speech and motor (7.7%). For parents who had concerns in three or more categories, there were 64 different combinations with the most common combination being speech, motor, and behavior (2.6%). See Figure 1.
Figure 1.
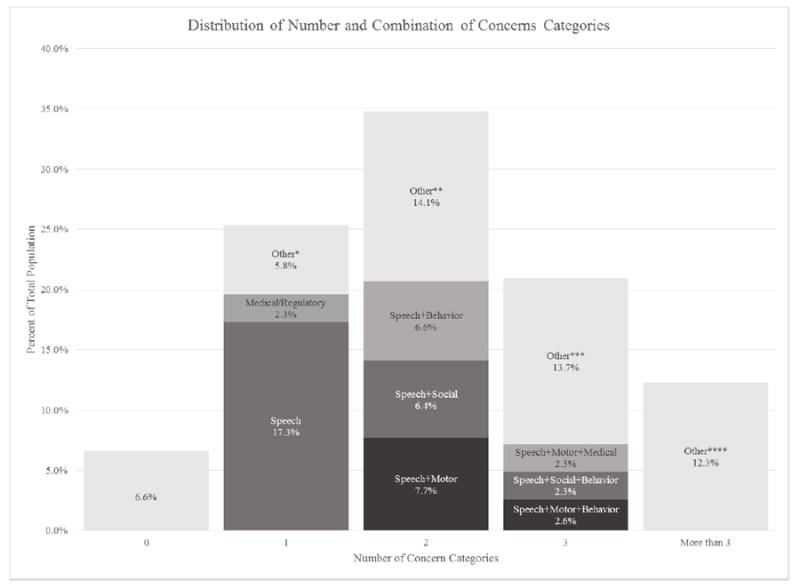
Distribution of Number and Combinations of Concern Categories
* Includes 7 other concern categories
** Includes 17 other concern combinations
*** Includes 23 other concern combinations
**** Includes 40 concern combinations
To test the hypothesis that the number of concerns differs based on child diagnoses as well as that parents with children diagnosed with ASD will have more ASD concerns, the concern categories were examined. The mean number of concern categories endorsed was not significantly different between the ASD group (mean=2.2, SD=.072) and the non-ASD group (mean=2.02, SD=.075), t(530)=1.82, p=.62. However, parents of children with ASD were significantly more likely than the parents of children who were non-ASD to report concerns in speech/communication (p<.001), restricted and repetitive behaviors (p=.001), and social categories (p=.001). Parents of non-ASD children were significantly more likely than parents of children with ASD to have behavior (p=.005) and medical concerns (p=.004). See Table 2. Summary concern scores indicated that the ASD group was significantly more likely than the non-ASD group to have any ASD concern (p<.001) and the non-ASD group was significantly more likely than the ASD group to have any non-ASD concern (p<.015).
Table 2.
Frequency of endorsement of concerns expressed by ASD and non-ASD parent groups
| ASD: n=274 [n(%)] |
Non-ASD: n=258 [n(%)] |
X2 Value | p-value | |
|---|---|---|---|---|
| Any Concern | 261 (95.3) | 236 (91.5) | 3.093 | .079 |
| Speech ** | 234 (85.4) | 184 (71.3) | 15.654 | <.001 |
| RRB or Sensory ** | 45 (16.4) | 18 (7.0) | 11.358 | .001 |
| Social ** | 79 (28.8) | 44 (17.1) | 10.370 | .001 |
| Autism Label | 15 (5.5) | 8 (3.1) | 1.810 | .179 |
| Any Autism Concern** | 245 (89.4) | 196 (76.0) | 16.946 | <.001 |
| Motor | 77 (28.1) | 87 (33.7) | 1.967 | .161 |
| Behavior/Temperament** | 58 (21.2) | 82 (31.8) | 7.722 | .005 |
| Medical/Regulatory** | 33 (12.0) | 55 (21.3) | 8.279 | .004 |
| Feeding/Eating | 30 (10.9) | 14 (5.4) | 5.342 | .021 |
| General Development | 33 (12.0) | 28 (10.9) | 0.186 | .667 |
| Any Non-Autism Concern | 161 (58.8) | 178 (69.0) | 6.019 | .014 |
p-value<.01
Note. RRB- Restricted, repetitive behavior
Within the non-ASD group there were statistically significant differences in speech concerns and behavior concerns based on specific non-ASD diagnosis (ps<.05), but not for RRB/sensory, social, ASD label, motor, medical/regulatory, feeding/eating, and general developmental concerns. Speech concerns were less common in the no diagnosis group and behavior concerns were less common in the GDD group.
Regression analysis examined whether report of concerns related to parents’ race/ethnicity, education level, and employment status; there were no significant findings (ps>.05), regardless of whether maternal, paternal, or both parents’ variables were used.
Hypothesis 2: Parents’ Concerns Relate to Therapeutic Intervention and Specialist Consultation
There was not a statistically significant difference between the number of children who received any type of therapy in the ASD group (n=182) compared to the non-ASD group (n=153; p=.089). There was also not a statistically significant difference between the number of children who saw any type of specialist in the ASD group (n=144) compared to the non-ASD group (n=114; p=.054); effect sizes (Cramer’s V) were 0.074 and 0.084, respectively. The total number of therapies received and specialists seen was significantly correlated with the total number of concerns parents reported, r= 0.308, p <.001.
Logistic regression, using all concern categories as predictors, supported the hypothesis that therapies received and specialists seen differed based on parents’ concerns (see Table 3).
Table 3.
Adjusted Odds ratios with 95% Confidence Intervals from logistics regression analyses conducted to evaluate the association between an expressed parental concern and the therapies received and specialists seen while controlling for other concern categories
| Speech Therapy | Physical Therapy | Occupational Therapy | |
|---|---|---|---|
| Concern | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Speech | 1.648 (1.049-2.588)* | 0.631 (0.365-1.125) | 1.138 (0.644-2.012) |
| RRB/Sensory | 1.733 (0.922-3.025) | 1.279 (0.626-2.613) | 2.424 (1.332-4.411)** |
| Social | 1.022 (0.688-1.563) | 0.960 (0.532-1.731) | 1.471 (0.888-2.436) |
| ASD Label | 2.025 (0.839-4.888) | 2.184 (0.752-6.339) | 2.345 (0.908-6.056) |
| Motor | 1.147 (0.781-1.685) | 3.908 (2.430-6.283)*** | 1.995 (1.274-3.124)** |
| Behavior | 0.637 (0.422-0.936)* | 0.863 (0.493-1.511) | 0.958 (0.578-1.588) |
| Medical/Regulatory | 1.990 (1.227-3.225)** | 3.450 (2.004-5.940)*** | 1.759 (1.107-3.043)* |
| Feeding | 1.582 (0.816-3.066) | 1.311 (0.601-2.861) | 2.170 (1.089-4.321)* |
| Other/Developmental | 1.530 (0.877-2.668) | 2.621 (1.373-5.007)** | 2.348 (1.258-4.384)** |
|
| |||
| Audiologist | Ophthalmologist | Other Professional | |
|
| |||
| Concern | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Speech | 3.244 (1.529-6.82)** | 0.464 (0.232-0.928)* | 1.425 (0.880-2.308) |
| RRB/Sensory | 1.159 (0.585-2.294) | 3.391 (1.527-7.533)** | 1.194 (0.670-2.126) |
| Social | 1.143 (0.671-1.944) | 0.954 (0.432-2.103) | 0.962 (0.612-1.511) |
| ASD Label | 4.045 (1.623-10.082)** | 0.426 (0.050-3.607) | 1.758 (0.726-4.259) |
| Motor | 0.975 (0.592-1.606) | 2.444 (1.314-4.544)** | 1.939 (1.308-2.875)*** |
| Behavior | 1.414 (0.485-2.366) | 0.771 (0.362-1.645) | 0.778 (0.502-1.206) |
| Medical/Regulatory | 1.123 (0.594-2.124) | 2.225 (1.113-4.447)* | 1.954 (1.197-3.190)** |
| Feeding | 1.823 (0.870-2.819) | 1.450 (0.550-3.826) | 2.267 (1.166-4.409)* |
| Other/Developmental | 3.314 (1.751-6.272)*** | 4.165 (2.007-8.643)*** | 2.434 (1.380-4.291)** |
p-value<.05
p-value<.01
p-value<.001
Note. RRB- Restricted, repetitive behavior; ASD- Autism spectrum disorder
Hypothesis 3: Correlation Between the Number of Concern Categories and Diagnostic Measures
To test the hypothesis that number of concerns is associated with M-CHAT(-R), ADOS, and CARS scores, Pearson correlations were conducted. The number of concerns was significantly related to screening scores for all children in the study: M-CHAT total score (r=.279, p<.001; n=176), M-CHAT-R total score (r=.146, p=.006; n=356). Similarly, the number of concern categories was significantly related to ASD severity as measured by the CARS(-2) (r=.130, p=.003) but not the ADOS severity score, r=.023, p=.705.
DISCUSSION
This study supported our hypothesis that the categories of concern parents’ expressed differed based on their child’s diagnosis, but were independent of parent’s education, race/ethnicity, and employment status. Also supported were the hypotheses that before their child received a diagnosis, children received therapies and saw professionals, in part based on their parents’ concerns, and parents who had concerns in more categories also endorsed more ASD risk signs on the M-CHAT(-R).
The results from this study provide important validation of parents’ concerns. This is important because at times professionals may be dismissive of parents’ concerns, or, perhaps, they may not trust parents’ judgment.29 This study has shown that 93.4% of parents of children who screen positive on the M-CHAT(-R) have concerns about their child’s development; of those parents, 94.4% of their children were diagnosed with autism or a developmental delay. Therefore, it is important for physicians and other providers to take time to elicit a comprehensive list of all of the parent’s concerns. This is consistent with the AAP’s recommendation for eliciting parent concerns as an essential component of ongoing developmental surveillance at well-child check-ups.29
Speech was the most common concern category expressed by parents in both groups, which is similar to results reported in other studies.11,16 An important finding from this study is seen in comparisons between the ASD parents and the non-ASD parents. A higher percent of ASD parents reported ASD-related concerns compared to the non-ASD parents, whereas a higher percent of non-ASD parents reported non-ASD concerns when compared to the ASD parents. Parents whose child was later diagnosed with ASD had more concerns that directly related to autism (speech, RRB/sensory, social, autism specific), with 13.4% more of these parents having any broad autism concern compared to the non-ASD parents. This is interesting in light of the fact that (a) both groups of children screened positive on a questionnaire specifically examining ASD risk, and (b) the two parent groups had a similar number of concerns, showing that the significant findings are not due to disproportionate numbers of concerns between groups. Instead, it appears that parents’ concerns different based on their child’s later diagnosis.
Within the ASD group, however, only 5% of the parents named “autism” specifically as a concern. This suggests that, although parents were identifying concerns that were related to autism, they were unaware or unwilling to recognize the congruence of the symptoms with an ASD diagnosis. It is also important to note that the parents’ concerns predated receiving a formal diagnosis, so the diagnostic process did not influence parents.
Even with the statistical significance of these results it is important to note that 76% of parents who had a child not diagnosed with ASD still had an autism concern. This is most likely due to the fact that speech concerns were the most common in both groups. Although speech delays are a core aspect of the DSM-IV criteria for an autism diagnosis, speech delays themselves are not specific to autism. A speech delay can be indicative of ASD as well as a global developmental delay or language delay. In the non-ASD group, 87.6% of children were diagnosed with a developmental delay and 74.8% of those parents indicated a speech concern, compared with only 46.9% of parents of children with no diagnosis. Among the non-ASD parents who had any autism concern, 68.4% of parents only expressed a speech concern; this can be compared to 53.9% of parents in the ASD group. This demonstrated that speech concerns were common among children who received any diagnosis. The difference in autism specific concerns reiterates the importance that physicians should elicit and take seriously all of a parent’s concerns, and then use their best clinical judgment to make the appropriate recommendations and referrals.
In our sample, 94% of the children who had screened positive on the M-CHAT(-R) demonstrated a significant delay or concern and, therefore, benefitted from screening. However, it is possible that observed high prevalence of any autism concern might be even greater in a sample of children who demonstrated high risk on broad developmental screening tools or developmental surveillance, rather than risk on an ASD-specific screening tool. This is because not all children with a non-ASD diagnosis will screen positive on the M-CHAT(-R), whereas it is expected that a broad developmental screening tool may identify more non-ASD cases. This suggests that the non-ASD parents in this study may not be representative of all children with a non-ASD diagnosis, and that in this study they are more similar to the ASD cases than they would be to the general population.
Our hypothesis that the therapies and specialists a child saw are associated with parents’ specific concerns, before they had a diagnosis was supported by the findings. Although the results cannot confirm a causal or temporal association between the concern categories identified by parents and the therapies received and/or specialists seen, an association is evident. One reason that more children in both diagnostic groups were receiving therapy than had seen a specialist may be that it is generally faster to initiate services in the state-provided Early Intervention (EI) system than it is to get an appointment with a private specialist who may have a long waiting list for an appointment.28
It was of interest to identify which concerns were associated with seeking out a particular therapy and/or specialist; this may help identify the concerns that were most important to parents. Prior knowledge led to the hypotheses that: (1) parents with speech concerns would be more likely to have children who received speech therapy, (2) parents with motor concerns would be more likely to have children who received physical therapy, and (3) parents who had medical/regulatory concerns would be more likely to have a child that received occupational therapy. All three of these hypotheses were supported by the data.
Some of the unexpected results included the negative association between behavior concerns and receiving speech therapy, and between speech concerns and seeing ophthalmologists. This demonstrates that not all statistically significant concern category and therapy or specialist combinations had an expected relationship. It is unclear why these associations existed, but this could be a place for further exploration. One possible explanation is that certain concerns take precedence over others. For example, in the total sample at least 7% of parents reported both a speech concern and a behavior concern. When a parent has more than one concern they may need to prioritize their concerns. For example, parents may focus more on correcting their child’s behavior that is disruptive than seeking speech therapy.
The associations between concerns and therapies and specialists were not stratified by diagnosis. This is of importance because it shows that independent of diagnosis, 63% of children had received therapy and 48.5% of children had seen a specialist. As mentioned before, this could be due to the fact that this is a sample of children who screened at-risk on the M-CHAT(-R) and is not a representative sample of all children.
M-CHAT(-R) items indicate risk factors for ASD, but parents do not always demonstrate explicit awareness that their specific responses are atypical or indicative of ASD risk. However, the positive relationship between M-CHAT(-R) scores and number of concerns suggests that parents who endorse more at-risk items, which mark a possibly atypical developmental course, are more likely to have multiple concerns about their child. A higher score on the M-CHAT(-R) does not necessarily mean that there would be more concern categories, because the M-CHAT(-R) contains multiple questions for each developmental domain. Therefore, it is an important finding that for both the M-CHAT and the M-CHAT-R there were positive associations between endorsements of at-risk responses on the parent-report screening tool and the number of concerns articulated prior to evaluation. This correlation, even though it was small, shows that when parents are having multiple concerns, they are more likely to endorse more at-risk items on the initial screening questionnaire.
There was a similar positive correlation between the number of parent concerns and the child’s score on the CARS(-2), however there was no correlation between number of parent concerns and ADOS severity scores. The CARS(-2) broadly surveys 15 symptoms related to ASD, and higher scores indicate more severe ASD. Similarly, the ADOS severity score is a 10-point range indicating severity,29 although speech/language is factored out of the severity score in order to compare children across different modules (determined by language level) of the ADOS. It is still somewhat surprising that ADOS severity score did not relate to the number of concerns; given that the severity score is a relatively new metric, this should be further explored in future studies.
Results from this study show that although parents may not recognize the collective signs and symptoms of ASD, they are recognizing the individual signs and reporting them as concerns. It is up to professionals to take the time to listen to parents and realize their concerns reflect specific signs of ASD. Parents are recognizing the warning signs of autism, even if they are not expressing their concerns specifically as an autism concern. Because parents are recognizing developmental delays in their children, it is important that pediatricians elicit parents’ concerns as part of developmental surveillance.6, 29
One limitation to the study is that the history questionnaire was completed at the time of evaluation, which could lead to recall bias. Since the first parent concerns occurred on average about 13 months before evaluation, it is possible for parents to have forgotten earlier concerns and focus more on recent concerns. The screening process also may have influenced parents’ concerns, given that concerns were not elicited prior to screening. The screening process itself may have made parents more aware of potential developmental delays in their children, but care was taken not to describe specific domains of possible delay, and autism was not mentioned specifically. There is also the possibility of bias due to the fact that the parents were attending the diagnostic evaluation, which may have increased focus on their child, leading them to identify more concerns than if they had not been invited for a diagnostic evaluation.
In our study speech concerns were coded as an ASD concern; although speech delays are part of the DSM-IV criteria for ASD, they are not specific to ASD. Therefore, future research into parents’ concerns that rely on diagnosis is based on DSM-5 criteria may benefit from removing speech concerns from the ASD category.
Only looking at concerns in a low-risk group of toddlers is another limitation. Parents of higher risk groups may have different concerns, earlier concerns, or more specific concerns if they already know their child is at risk for ASD. This could reflect greater knowledge about the symptoms of ASD and the developmental milestones that their child should be reaching.
A final limitation to the current study is that the history questionnaire had limited detail about therapies and specialists seen. For example, the history questionnaire provided no information about the quality and frequency of therapies or specialists. It also did not ask about specific therapies other than speech, which could have led parents to under report therapies received. Such information might increase understanding about why certain children were receiving therapies and others were not when their parents had the same concerns. Furthermore, future research would benefit from assessing the factors that led a child to be in early intervention, to better understand the roles of the primary care provider, parent, and any other specialists in referring children to therapies.
A major strength of this study was the large sample size of 532 toddlers. The format of the history questionnaire allowed parents to write down all of their concerns and did not limit parents to pre-determined concern categories. The free-text response format allowed parents to express their concerns even when they did not know exactly what their concern was related to. For example, if a mother was concerned because her child had difficulty paying attention, she may not necessarily know that it is a behavior concern. By being able to describe her concern, it could be properly coded. It was also beneficial that concerns were divided into autism concerns and non-autism concerns. This was because most parents did not express a specific ASD concern; however, by looking at the aggregate any ASD concern category, the number of parents who had concerns about symptoms of ASD could be determined.
CONCLUSION
This study found that parents expressed concerns about their children before receiving a diagnosis. These concerns were congruent with the specific diagnosis their child subsequently received and parents of children with ASD expressed more concerns related to autism symptoms. Before a child received a diagnosis, children received certain therapists and specialists based on their parents’ concerns. Finally, there was a positive correlation between the number of concerns a parent had and their child’s M-CHAT(-R) score. These results help validate parents’ concerns. They show that despite parents not naming autism as a specific concern, they are recognizing the developmental delays and signs of ASD in their children, and are seeking help relating to these concerns.
Acknowledgments
We would like to give special thanks Diana Thao for help coding history questionnaire responses, and Kiauhna Haynes for extraction of the dataset. We also thank all of the children, parents, and physicians that participated in the study. Finally, we are thankful to the Early Detection and Intervention team at the A.J. Drexel Autism Institute for their support during this project. We thank our funding sources, the Eunice Kennedy Shriver National Institute of Child Health and Human Development R01HD039961, Maternal and Child Health Bureau, R40MC00270, U.S. Department of Education Student-Initiated Research Grant, University of Connecticut’s Research Foundation Faculty Grant, National Alliance of Autism Research, and a National Institute of Mental Health Predoctoral Fellowship, F31MH12550.
Funding: This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, R01HD039961, Maternal and Child Health Bureau, R40MC00270, U.S. Department of Education Student-Initiated Research Grant, University of Connecticut’s Research Foundation Faculty Grant, National Alliance of Autism Research, and a National Institute of Mental Health Predoctoral Fellowship, F31MH12550
Appendix 1
Categories for Parents Concerns
| Concern | Description | Example |
|---|---|---|
| Autism Specific | ||
| Speech/Communication | Speech production and gestures; language comprehension; reciprocity of language | “He doesn’t talk” |
| “He doesn’t say ‘Mama’” | ||
| RRB/Sensory | Restricted, repetitive, or stereotyped behaviors in sensory, motor, or object use | “He likes to spin in circles” |
| “Doesn’t like things on her hands” | ||
| Social | Social engagement, social attention, play | “He doesn’t like playing with other kids” |
| “She doesn’t look at us” | ||
| Autism Label | Specific mention of autism | “I think he might have autism” |
| Non-Autism Specific | ||
| Motor | Delays in motor development, general clumsiness, or muscle development | “She isn’t walking yet” |
| Behavior/Temperament | Attention, activity level, self-injurious behavior, etc. | “I am afraid he will hurt himself” |
| “She seems to be introverted” | ||
| Medical/Regulatory | Medical issue/condition or related to a regulatory behavior (sleeping, toileting) | “He wasn’t gaining weight” |
| “She still isn’t potty-trained” | ||
| Feeding/ Eating | Feeding and eating | “Does not like many foods, tastes, and textures” |
| Developmental/Other | General development concerns and any concern not contained in another area | “He hasn’t reached his milestones yet” |
| “Nothing specific, just general development” | ||
Note. RRB- Restricted, repetitive behavior
Footnotes
Conflict of Interest: Diana Robins is a co-owner of M-CHAT, LLC, which receives royalties from companies that incorporate the M-CHAT(-R) into commercial products. Data in the current study is from the freely available version of the M-CHAT(-R).
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. 2013. [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Developmental Disabilities Monitoring Network. Prevalence and characteristics of autism spectrum disorder among children aged 8 years - Autism and Developmental Disabilities Monitoring network, 11 sites, United States, 2012. MMWR. 2016;65;3:1–23. doi: 10.15585/mmwr.ss6503a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andersson GW, Miniscalco C, Gillberg C. Preschoolers assessed for autism: Parent and teacher experiences of the diagnostic process. Res Dev Disabil. 2014;35:3392–3402. doi: 10.1016/j.ridd.2014.08.027. [DOI] [PubMed] [Google Scholar]
- 4.Ozonoff S, Young GS, Landa RJ, et al. Diagnostic stability in young children at risk for autism spectrum disorder: a baby siblings research consortium study. J Dev Behav Pediatr. 2015;56:988–998. doi: 10.1111/jcpp.12421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klintwall L, Eldevik S, Eikeseth S. Narrowing the gap: effects of intervention on developmental trajectories in autism. Autism. 2015;19(1):53–63. doi: 10.1177/1362361313510067. [DOI] [PubMed] [Google Scholar]
- 6.Johnson CP, Myers SM. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120:1183–1215. doi: 10.1542/peds.2007-2361. [DOI] [PubMed] [Google Scholar]
- 7.Dosreis S, Weiner CL, Johnson L, et al. Autism spectrum disorder screening and management practices among general pediatric providers. J Dev Behav Pediatr. 2006;27:S88–94. doi: 10.1097/00004703-200604002-00006. [DOI] [PubMed] [Google Scholar]
- 8.Daniels AM, Mandell DS. Children’s compliance with American Academy of Pediatrics’ well-child care visit guidelines and the early detection of autism. J Autism Dev Disord. 2013;43:2844–2854. doi: 10.1007/s10803-013-1831-x. [DOI] [PubMed] [Google Scholar]
- 9.Arunyanart W, Fenick A, Ukritchon S, et al. Developmental and Autism Screening A Survey Across Six States. Infants Young Child. 2012;25:175–187. [Google Scholar]
- 10.Chawarska K, Paul R, Klin A, et al. Parental recognition of developmental problems in toddlers with autism spectrum disorders. J Autism Dev Disord. 2007;37:62–72. doi: 10.1007/s10803-006-0330-8. [DOI] [PubMed] [Google Scholar]
- 11.De Giacomo A, Fombonne E. Parental recognition of developmental abnormalities in autism. Eur Child Adolesc Psychiatry. 1998;7:131–136. doi: 10.1007/s007870050058. [DOI] [PubMed] [Google Scholar]
- 12.Ozonoff S, Young GS, Steinfeld MB, et al. How Early Do Parent Concerns Predict Later Autism Diagnosis? J Dev Behav Pediatr. 2009;30:367–375. doi: 10.1097/dbp.0b013e3181ba0fcf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun X, Allison C, Auyeung B, et al. Parental concerns, socioeconomic status, and the risk of autism spectrum conditions in a population-based study. Res Dev Disabil. 2014;35:3678–3688. doi: 10.1016/j.ridd.2014.07.037. [DOI] [PubMed] [Google Scholar]
- 14.Guinchat V, Chamak B, Bonniau B, et al. Very early signs of autism reported by parents include many concerns not specific to autism criteria. Res Autism Spectr Disord. 2012;6:589–601. [Google Scholar]
- 15.Glascoe FP. Parents’ evaluation of developmental status: how well do parents’ concerns identify children with behavioral and emotional problems? Clin Pediatr (Phila) 2003;42:133–138. doi: 10.1177/000992280304200206. [DOI] [PubMed] [Google Scholar]
- 16.Herlihy L, Knoch K, Vibert B, et al. Parents’ first concerns about toddlers with autism spectrum disorder: Effect of sibling status. Autism. 2013;19:20–8. doi: 10.1177/1362361313509731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bolton PF, Golding J, Emond A, et al. Autism spectrum disorder and autistic traits in the Avon Longitudinal Study of Parents and Children: precursors and early signs. J Am Acad Child Adolesc Psychiatry. 2012;51:249–260.e225. doi: 10.1016/j.jaac.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 18.Sivberg B. Parents’ detection of early signs in their children having an autistic spectrum disorder. J Pediatr Nurs. 2003;18:433–439. doi: 10.1016/s0882-5963(03)00139-8. [DOI] [PubMed] [Google Scholar]
- 19.Chlebowski C, Robins DL, Barton ML, et al. Large-scale use of the modified checklist for autism in low-risk toddlers. Pediatrics. 2013;131:e1121–1127. doi: 10.1542/peds.2012-1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robins DL, Casagrande K, Barton M, et al. Validation of the modified checklist for Autism in toddlers, revised with follow-up (M-CHAT-R/F) Pediatrics. 2014;133:37–45. doi: 10.1542/peds.2013-1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robins DL, Fein D, Barton M. The Modified Checklist for Autism in Toddlers (M-CHAT) Self-published. Available at www.mchatscreen.com.
- 22.Robins DL, Fein D, Barton M. The Modified Checklist for Autism in Toddlers, Revised with Follow-Up (M-CHAT-R/F) doi: 10.1542/peds.2013-1813. Self-published. Available at www.mchatscreen.com. [DOI] [PMC free article] [PubMed]
- 23.Lord C, Risi S, Lambrecht L, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30:205–223. [PubMed] [Google Scholar]
- 24.Schopler E, Reichler RJ, Renner BR. Childhood Autism Rating Scale-2. Los Angeles, CA: Western Psychological Services; 2010. [Google Scholar]
- 25.Barton M, Boorstein H, Herlihy L, Dumont-Mathieu T, Fein D. Toddler ASD symptom interview. 2012 Self-published. [Google Scholar]
- 26.Mullen EM. Mullen Scales of Early Learning. American Guidance Service, Inc. 1995 [Google Scholar]
- 27.Sparrow SS, Cicchetti DV, Balla DA. Vineland Adaptive Behavior Scales. 2. Livonia, MN: Pearson Assessments; 2005. [Google Scholar]
- 28.Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. J Autism Dev Disord. 2009;39:693–705. doi: 10.1007/s10803-008-0674-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Academy of Pediatrics. Council on Children With Disabilities; Section on Developmental and Behavioral Pediatrics. Bright Futures Steering Committee. Medical Home Initiatives for Children With Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. 2006;118:405–420. doi: 10.1542/peds.2006-1231. Published correction appears in Pediatrics. 2006;119: 1808–1809. [DOI] [PubMed] [Google Scholar]


