Abstract
BACKGROUND
The platelet-rich plasma (PRP) and hyaluronic acid (HA) constitute a system of tissue growth that can regenerate damaged tissue. This study was performed to evaluate the effect of PRP and HA in treatment of complications of Achilles tendon reconstruction.
METHODS
We selected ten patients affected by Achilles tendon injuries resulting from post-surgical complications subsequent to tenorrhaphy and have treated them with autologous PRP in combination with HA to evaluate the improvement of lesions with wound closure.
RESULTS
The treatment with PRP and HA for post-surgical complications of Achilles tendon was effective in healing and regeneration of soft and hard tissues. The healing time was shortened, and the treated area preserved a satisfying strength in plantar flexion and extension of the ankle, denoting to a decisive improvement in texture and a more rapid healing and a good cutaneous elasticity, with a significant reduction of the costs of hospitalization and the pain already the immediate postoperatively. The functional rehabilitation in terms of deambulation and joint mobility was complete.
CONCLUSION
The treatment we proposed allowed an easier and more rapid wound closure with excellent aesthetic improvement. Furthermore, the minimally invasive technique is well tolerated by patients.
Key Words: Platelet rich plasma, Hyaluronic acid, Achilles tendon, Reconstruction
INTRODUCTION
The Achilles tendon is the largest and strongest tendon in the human body. It does not have a true synovial sheath but is coated by the paratenon, a not organized loose connective tissue, of variable thickness. The vascular supply of the tendon originates distally from intra-bony vessels and proximally by intramuscular branches of the calcaneus. It presents an area relatively variable from 2 cm to 6 cm from the calcaneus that is more vulnerable both to degeneration and to lesions. This tendon very often suffers from ruptures due to its peculiar anatomy.1
Tendons have been viewed as a composite matrix of collagen fibers surrounded by the gel-like extra fibrillar matrix. Work by several groups revealed variations in collagen type and glycosaminoglycan, proteoglycan, and water content in different tendon regions.1 Other studies defined collagen content about the tendon–bone interface, delineating the transition from pure tendon matrix to bone via fibro-cartilage and mineralized fibro-cartilage zones.2
Furthermore, the components of specific tendons have been studied. Notably, proteoglycan 4 (PRG4),3 lubricin,4 and fibronectin3-5 have been implicated in the gliding characteristics of flexor tendons. This approach allows a better understanding of tendons and ligaments physiology. Moreover it allows us to comprehend the ability of repair and regeneration of the tissues. It is hypothesized that tendon crimp and interactions between the fibers and extracellular matrix are responsible for tendon’s nonlinear properties, which can be seen in the low-stiffness toe region.6 Finally, the viscoelastic response has been shown to be related to the presence of proteoglycans, glycosaminoglycans, and water in the tissue.7 This study was performed to evaluate the effect of platelet rich plasma and hyaluronic acid in treatment of complications of Achilles tendon reconstruction.
MATERIALS AND METHODS
The authors treated at the Department of Plastic and Reconstructive Surgery “University of Rome Tor Vergata” ten patients with exposure of the Achilles tendon for postoperative complication of tenorrhaphy with no absorbable sutures as Vicryl. The authors considered inclusion and exclusion criteria. The inclusion criteria were (i) Age between 20-80 years, (ii) Chronic or traumatic orthopedic surgery subsequent to tenorrhaphy of TdA, (iii) Use of advanced medications for a minimum of two weeks.
The exclusion criteria were divided in two types of local and systemic. The systemic criteria included platelet disorders, thrombocytopenia, anti-aggregating therapy, bone marrow aplasia, uncompensated diabetes, sepsis and cancer. The local criteria were osteomyelitis, loss of substance of more than 50% of the segments. The authors did not consider exclusion criteria of tobacco use, compensated diabetes, vascular disease and genetic disorders.
All patients were enrolled after a series of advanced medications (with different materials such as collagen, hydro cellulose fiber and calcium alginate dressing) which allowed preparation of wound bed. Patient anonymity was respected and written informed consent was obtained before the surgical procedure and the production of images. In order to establish the effects of their treatment, the authors compared their results with control group made up of 10 patients.
The control group comprised 5 females and 5 males aged between 23 and 62 years all affected by exposure of the Achilles tendon and lower extremity ulcers. This sample group was treated with curettage and application of hyaluronic acid in the bed of the ulcers. The medication based on hyaluronic acid where removed from the authors after 15 days. The level of evidence was therapeutic IV.
Platelet rich plasma (PRP) is a mixture of autologous proteins, that contains more than 300000-350000 platelets/ul, whose action consists in stimulating skin fibroblasts favoring tissue growth by new synthesis of collagen. Platelet gel, being a laboratory product, is easy and safe to use; it cannot be contaminated and is lacking of surface antigens, responsible of potential allergic reaction.
In the platelets there are actives substances that are involved in tissue repair mechanism such as chemotaxis, cell proliferation and differentiation, angiogenesis, intracellular matrix deposition, immune-modulation, antimicrobial activity, and remodeling. Some of the numerous GFs (growth factors) released by the platelets after activation have been identified as PDGF (platelet derived growth factor), TGF α&β (transforming growth factor alpha and beta), EGF (epidermal growth factor), FGF (fibroblast growth factor), KGF (keratinocyte growth factor), IGF (insulin growth factor), PDEGF (platelet derived epidermal growth factor), IL8 (interleukin 8), TNFα (tumor necrosis factor alpha), CTGR (connective tissue growth factor) and GM-CSF (granulocyte macrophage colony stimulating factor.
During the wound-healing process (four phases: hemostasis, inflammation, proliferation, remodeling) platelet GFs serve as messengers to regulate a well-orchestrated and complex series of events involving cell-cell and cell-matrix interactions and promoting the proliferation of cell at the wound site. Autologous platelet derived wound healing factor were proposed to regulate wound healing of chronic ulcers by promoting the formation of granulation tissue in the early healing phase.
In addition to their tissue forming and proliferative effects, GFs exhibit chemotactic effect that causes the migration of neutrophils and macrophages, adding an antimicrobial component to the wound site. For each patient obtained 9-10 cc platelet rich plasma after first centrifugation. The PRP activated after CaCl, CaGl or autologous thrombin added is reintroduced in a centrifuge and subjected to second centrifugation for 15 minutes at 1100 rpm. The product obtained present increases of consistency (solid-gel form). Control of infection deep is essential during the treatment of defects in the soft tissues and the PRP in particular has the intrinsic factor antibacterial that allows reducing the rate of infection in defects of the soft tissues. Not to forget also the antalgic action carried out by PRP.
After infiltration of a local anesthetic and/or sedation, was performed a through curettage of the wound. Where present, are removed the stitches the previous tenorrhaphy, recognized like a foreign body. It has been used a disposable kit to elaborate 16 ml of peripheral venous blood. The kit includes two or more vacuum tubes sterile, for the collection of blood, needles, and a device for transferring. Blood was taken up in two collecting platelet tubes (8 mL each). All tubes were centrifuged to 1500 g (corresponding to 3000 rpm) for 10 minutes.
The PRP received by this method is of the highest quality and with a high content of growth factors and platelets undamaged (platelet yield of 93%, lower levels of P-selectin on not activated PRP). The PRP is injected intra tendons, intra-lesional and peri-lesional after activation. The PRP gel was applied to the lesion and cover with three-dimensional polymerized HA - (hyaluronic acid as biological dressing). The HA is left in place for 15-20 days during the peak of the growth factors and to allow the subsequent release of the angiogenesis active oligomers. In order to reduce the interference with veno-lymphatic regeneration process, we making an elastic compressive bandage on the limb. During the intra-operative time antibiotic therapy were administered in accordance to the results of culture with antibiogram, which continued for 7 days.
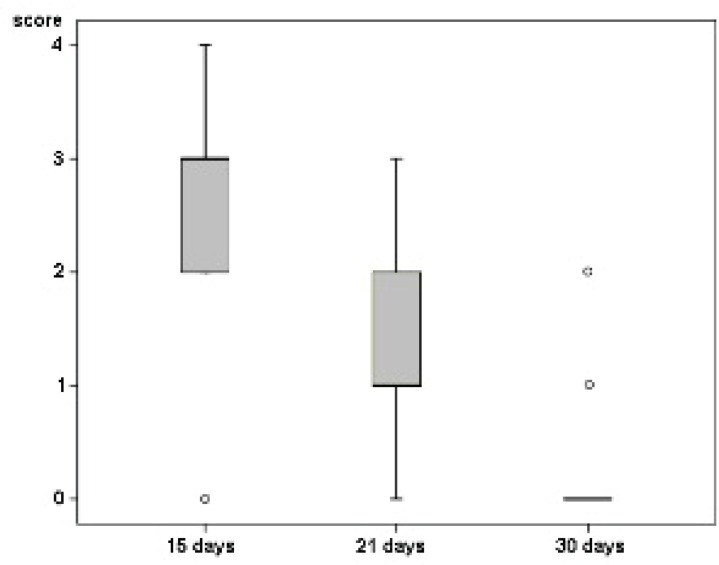
For our study, the follow-up was carried out as follows: At 7 days, the secondary dressing (gauze) was changed, at 15-days, silicone film (part of the hyaluronic acid matrix) was removed, at 21 days, the excess of hyaluronic acid and replacement as necessary was removed, and at 30 days, healing or apposition of new hyaluronic acid was undertaken. At 21 to 31 days after surgery, the condition of wounds in terms of depth of lesion was evaluated using the following rating system: 0=closed wound, 1=superficial cutaneous lesion interesting the epidermis, 2=deep skin lesion interesting epidermis and derma, 3=exposed tendon and 4=tendon exposure combined with infection. Comparisons between the assessments performed 15 and 21 days after the intervention and between the assessments performed at 21st and 30th day were performed using the Mann-Whitney U-test.
RESULTS
Our patients were not evaluated to days 7 and 15 because the primary medication was left in situ and from our protocol. On day 21 we assessed: 4 patients with score 0, 4 with a score 1 and 2 with score 2. At Day 30 we evaluated: 8 patients with score 0, 1 with a score 1 and 1 with score 2. Table 1 demonstrates the detail of patients treated with PRP and HA.
Table 1.
Detail of patients treated with PRP and HA
| Patients |
ULCER DIMENSION
(lenght x wide) |
AGE | CO-MORBIDITY | 7° day | 15° day | 21° day | 30° day |
|---|---|---|---|---|---|---|---|
| 1) P.B | 5 cm × 2 cm | 49 | Ipertension | - | - | 1 | 0 |
| 2) A.F | 3 cm × 3 cm | 25 | No | - | - | 0 | 0 |
| 3) S.L | 4 cm × 3 cm | 36 | No | - | - | 0 | 0 |
| 4) C.M | 7 cm × 3 cm | 74 | Compensated Diabetes | - | - | 2 | 1 |
| 5) S.O | 4 cm × 2 cm | 43 | Ipertension | - | - | 1 | 0 |
| 6) T.P | 9 cm × 2 cm | 80 | Compensated Diabetes | - | - | 2 | 2 |
| 7) F.G | 6 cm × 2 cm | 65 | Vascular Disease | - | - | 1 | 0 |
| 8) G.T | 3 cm × 4 cm | 20 | No | - | - | 0 | 0 |
| 9) P.P | 5 cm × 2,5 cm | 33 | No | - | - | 0 | 0 |
| 10) R.E | 4 cm × 3,5 cm | 51 | Dislipidemy | - | - | 1 | 0 |
In this assessment, during the treatment period no case of infection was recorded. The post-operative pain was absent. The severity of injuries was significantly reduced after treatment with PRP and HA and only one patient had needed a second regenerative intervention.
The results of the assessment of wound status, shown in figure 1 reveals a complete wound healing of 4 patients after 21 days, 8 patients after 30 days, with a progressive significant reduction of the score from 15 to 21 days (p<0.001) and from 21 to 30 days (p<0.001).
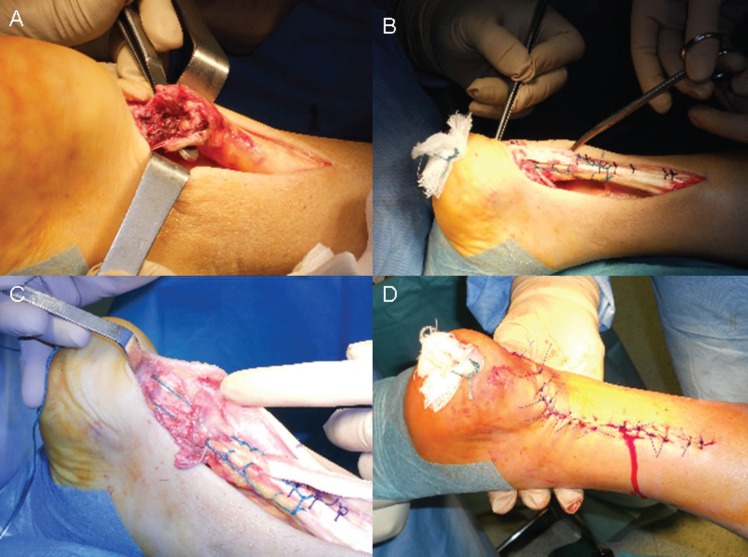
Fig. 1.
A) pre-operative situation with detail of tendon rupture; B) intra-operative situation during tenorraphy; C) intra-operative situation during tenorraphy in detail; D) suture completed
In our experience, treatment with PRP in combination with HA for post-surgical complications of Achilles tendon was effective in healing and regeneration of soft and hard tissues. The treatment allowed an easier and more rapid wound closure with excellent aesthetic improvement. Furthermore, the minimally invasive technique is well tolerated by patients. The healing time was shortened, and was reduced need for additional reconstructive surgical procedures of soft tissues. The treated area preserved a satisfying strength in plantar flexion and extension of the ankle, and there was a decisive improvement in texture and a more rapid healing and a good cutaneous elasticity, with a significant reduction of the costs of hospitalization and the pain already the immediate postoperatively were noted.
The functional rehabilitation in terms of deambulation and joint mobility was complete. The complications using absorbable surgical suture was prevented during the interventions of tenorrhaphy. The collagen based, elastin and biomaterials were available specifically for the reconstruction of tendon. Figure 1 reveals the pre-operative situation with detail of tendon rupture; intra-operative situation during tenorraphy; intra-operative situation during tenorraphy in detail; and suture completed. The pre-operative situation after tendon reconstruction following tenorraphy; pre-operative situation with detail of wound dehiscence, and exposition of sutures; pre-operative situation with diameter of wound dehiscence; and pre-operative situation with diameter of wound dehiscence were shown in Figure 2.
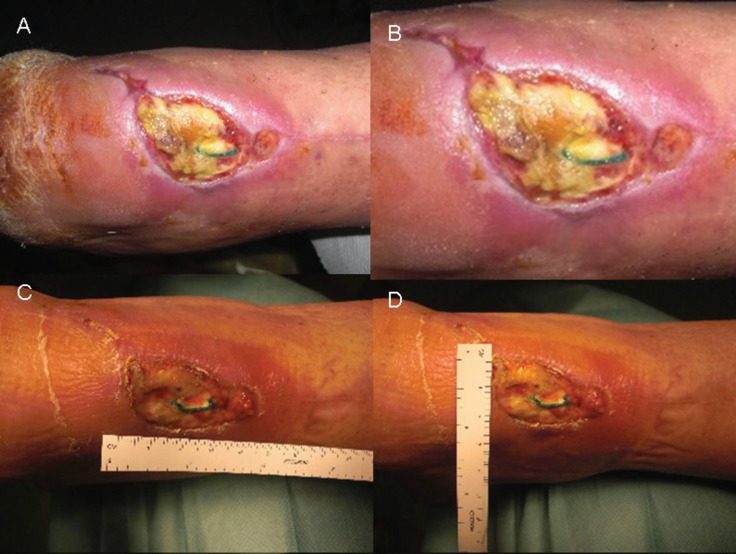
Fig. 2.
A) pre-operative situation after tendon reconstruction following tenorraphy; B) pre-operative situation with detail of wound dehiscence, and exposition of sutures; C) pre-operative situation with diameter of wound dehiscence; D) pre-operative situation with diameter of wound dehiscence
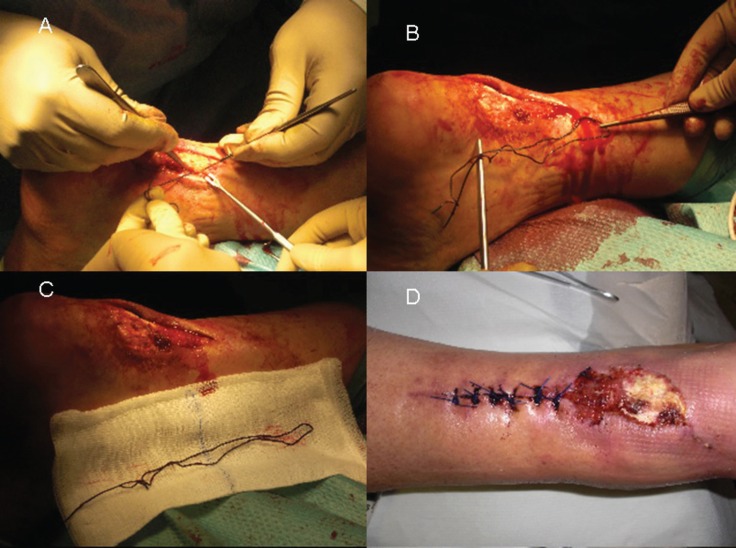
The intra-operative situation during sutures removal; intra-operative situation with detail of sutures removed; intra-operative situation with detail of sutures removed; and post-operative situation after 10 days from the treatment based on sutures removal and reconstruction of damaged soft tissue were demonstrated in Figure 3. Figure 4 denotes to intra-operative situation during PRP infiltration in the bed of the ulcers; post-operative situation after 15 days; post-operative situation after 30 days; and post-operative situation after 45 days from the treatment with completely wound healing. Box plot of the score used to assess the status of wounds as described in the materials and methods section (wide line represents the median, the grey box the scores between 25th and 75th percentile, the vertical bars include all the samples, with the exception of the scores accounted as outliers and plotted as circles) was presented in Figure 5.
Fig. 3.
A) intra-operative situation during sutures removal; B) intra-operative situation with detail of sutures removed; C) intra-operative situation with detail of sutures removed; D) post-operative situation after 10 days from the treatment based on sutures removal and reconstruction of damaged soft tissue
Fig. 4.
A) intra-operative situation during PRP infiltration in the bed of the ulcers; B) post-operative situation after 15 days; C) post-operative situation after 30 days; D) post-operative situation after 45 days from the treatment with completely wound healing
Fig. 5.
Box plot of the score used to assess the status of wounds as described in the materials and methods section (wide line represents the median, the grey box the scores between 25th and 75th percentile, the vertical bars include all the samples, with the exception of the scores accounted as outliers and plotted as circles
DISCUSSION
The complex wounds are chronic injuries that do not heal spontaneously within three months. Usually these wounds are treated with the advanced dressing, for example: biosynthetic or hydro fiber cellulose expanded of foam polyurethane, photolytic enzymes, hydrogels, hydrocolloid, Vac therapy and hyaluronic acid. Wound healing is an evolutionarily conserved complex multi-cellular process that in skin aims at barrier restoration. The process involves the coordinated efforts of several cell types including keratinocytes, fibroblasts, endothelial cells, macrophages and platelets. The migration, infiltration, proliferation and differentiation of these cells will culminate in an inflammatory response, the formation of new tissue and ultimately wound closure.8
This complex process is executed and regulated by an equally complex signaling network involving numerous growth factors, cytokines and chemokines. Particular relevance is the epidermal growth factor (EGF) family, transforming growth factor beta (TGF-beta) family, fibroblast growth factor (FGF) family, vascular endothelial growth factor (VEGF), granulocyte macrophage colony stimulating factor (GM-CSF), platelet-derived growth factor (PDGF), connective tissue growth factor (CTGF), interleukin (IL) family, and tumor necrosis factor-alpha family.9 These proteins could stimulate neo angiogenesis and PRP constitute a three-dimensional matrix that allows the arrangement of cellules into the correct spatial organization.10
PRP is increasingly used in treatment of chronic non-healing tendon injuries including the elbow, patella, and the Achilles among others. Because of mechanical factors, tendons are vulnerable to injury and hardly to heal. Tendons are made of specialized cells including tenocytes, water, and fibrous collagen proteins. Millions of these collagen proteins weave together to form a durable strand of flexible tissue to make up a tendon. They naturally anchor to the bone and form a resilient mineralized connection.11-13
Tendons also bear the responsibility of transferring a great deal of force, and as a result are susceptible to injury when they are overwhelmed. With repetitive overuse, collagen fibers in the tendon may form micro tears, leading to what is called tendonitis, or more appropriately tendinosis or tendinopathy. The injured tendons heal by scarring which adversely affects function and increases risk of re-injury. Furthermore, tendons heal at a slow rate compared with other connective tissues, secondary to poor vascularization.14-16
Histologic samples from chronic cases indicate that there is not an inflammatory response, but rather a limitation of the normal tendon repair system with a fibroblastic and a vascular response called, angio-fibroblastic degeneration.17 Thus, organically based strategies to promote healing while facilitating the release of one’s own natural growth factors is attracting interest. During normal tissue repair in vivo, platelets release high concentrations of biologically active proteins including growth factors18 in doing so, they are able to influence a wide range of processes and promote the recruitment, growth and morphogenesis of cells. The ability of platelets to release growth factors and cytokines at supra-physiological concentrations within a growing clot can be harnessed therapeutically to accelerate natural healing.19
It is necessary for tissue regeneration to increase the number of cells constituting the tissue as well as reconstruct a structure of extracellular matrix (ECM) to support the proliferation and differentiation of cells for regeneration induction. For these reasons, it is easy to understand the important role of hyaluronic acid (HA) in tissue repair processes, facilitating the entry of a large number of cells into the injured area and contributing to the orientation of the fibrous component of the ECM. HA, is a wound dressing that acts as a temporary dermal substitute in the treatment of wounds or deep burns.9 HA is a three-dimensional scaffold is promptly colonized by fibroblasts and ECM components, favoring an ordered reconstruction of the dermal tissue.20
Recently, many studies suggesting regenerative medicine procedures associated with next-generation biomaterials have been proposed to restore an appropriate environment that encourages healing. HA acts as a scaffold for the PRP. An ideal scaffold should promote rapid remodeling, possess increased strength, demonstrate improved healing and permit early rehabilitation and return to function after implantation. In addition, the availability of such a scaffold would reduce the likelihood of donor site morbidity, increased surgical time, increased cost and poor function associated with autologous tendon harvest (currently considered the ‘gold standard’ in clinical practice). In summary, an optimized scaffold would have the potential to vastly improve the treatment of tendon and ligament injuries, especially those associated with tumor, trauma, and congenital deficiencies where auto graft or allograft tissue might not be available in sufficient quantity for reconstruction.21
The aim of our study is to demonstrate that PRP and HA can be used to cover defects of soft tissues, without require frequent dressing changes, and their combined use decreases edema and chronic pain. Finally, the consequent increase in local blood promotes the formation of a healthy granulation tissue also in both acute and chronic injury caused to complications of Achilles tendon tenorrhaphy.
Even though clinical examination, which assesses functional impairment, is often adequate for rupture after injury diagnosis, approximately 10-20% of acute complete ruptures are not promptly diagnosed. There are also spontaneous breakage dates by repetitive micro trauma that weaken over time the tendon rupture. Have been described various techniques for repairing or increase the tendon, which can also be used in combination, such as the use of autologous materials, including the increase of the tendon with autologous by the gracilis or semitendinosus, the transplantation of aponeurosis gastrocnemius, the transfer of the flexor hallucis longus tendon, the peroneus brevis and percutaneous suture.22
They can also be used synthetic materials, such as polyester, or biomaterials, such as collagen of animal origin. In some patients, there is a large gap (more than 6 cm) between the ends of the plantaris tendon, despite maximal flexion of the ankle and traction on the stumps of the Achilles tendon and the premises are not sufficient to bridge the gap: in such cases as an option is suitable for reconstruction with ipsilateral hamstring tendon. Nor should we forget the possibility of homologous transplants due to musculoskeletal tissue bank. The reconstruction of the Achilles tendon is unfortunately not free of postoperative complications including wound dehiscence, skin necrosis; intolerance means of sutures, infection and deep vein thrombosis (DVT) are known in the surgical repair.22
The object of our study considered patients undergoing tenorrhaphy with complications of soft tissue in eight patients treated with conventional techniques that have been subjected to a second operation and the treatment of the lesion with platelet-rich plasma in combination with hyaluronic acid. In our experience, treatment with PRP-HA for post-surgical complications of Achilles tendon was effective in healing and regeneration of soft and hard tissues: PRP and HA, act in synergy allowing tissue regeneration because they show to have logical and similar mechanisms of action and are not immunogenic, control pain and local infection, interact with the MEC and the cells forming a scaffold for cell growth. The treatment we propose has allowed an easier and more rapid wound closure with excellent aesthetic improvement. Furthermore, the minimally invasive technique is well tolerated by patients.
This evaluation has found that it was simplified rapid formation of the granulation tissue; the healing time was shortened, and was reduced need for additional reconstructive surgical procedures of soft tissues. The treated area preserves a satisfying strength in plantar flexion and extension of the ankle, is a decisive improvement in texture and a more rapid healing and a good cutaneous elasticity, with a significant reduction of the costs of hospitalization and the pain already the immediate postoperatively.
The functional rehabilitation in terms of deambulation and joint mobility was complete. In order to prevent complications of this kind we recommend using Absorbable Surgical suture, during the interventions of tenorrhaphy, collagen based and elastin and biomaterials available specifically for the reconstruction of tendon. Finally, the use of PRP and HA together best significantly the formation of granulation and tissue regeneration as it helps to prevent infection. Our results add to increasing evidence that PRP and HA are useful in therapeutic measures for the open wounds.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Please cite this paper as:
Gentile P, De Angelis B, Agovino A, Orlandi F, Migner A, Di Pasquali C, Cervelli V. Use of Platelet Rich Plasma and Hyaluronic Acid in the Treatment of Complications of Achilles Tendon Reconstruction. World J Plast Surg 2016;5(2):124-132.
References
- 1.Fan L, Sarkar K, Franks DJ, Uhthoff HK. Estimation of total collagen and types I and III collagen in canine rotator cuff tendons. Calcif Tissue Int. 1997;61:223–9. doi: 10.1007/s002239900327. [DOI] [PubMed] [Google Scholar]
- 2.Fujioka H, Wang GJ, Mizuno K, Balian G, Hurwitz SR. Changes in the expression of type-X collagen in the fibrocartilage of rat Achilles tendon attachment during development. J Orthop Res. 1997;15:675–81. doi: 10.1002/jor.1100150508. [DOI] [PubMed] [Google Scholar]
- 3.Rees SG, Davies JR, Tudor D, Flannery CR, Hughes CE, Dent CM, Caterson B. Immunolocalisation and expression of proteoglycan 4 (cartilage superficial zone proteoglycan) in tendon. Matrix Biol. 2002;21:593–602. doi: 10.1016/s0945-053x(02)00056-2. [DOI] [PubMed] [Google Scholar]
- 4.Sun Y, Berger EJ, Zhao C, Jay GD, An KN, Amadio PC. Expression and mapping of lubricin in canine flexor tendon. J Orthop Res. 2006;24:1861–8. doi: 10.1002/jor.20239. [DOI] [PubMed] [Google Scholar]
- 5.Banes AJ, Link GW, Bevin AG, Peterson HD, Gillespie Y, Bynum D, Watts S, Dahners L. Tendon synovial cells secrete fibronectin in vivo and in vitro. J Orthop Res. 1988;6:73–82. doi: 10.1002/jor.1100060110. [DOI] [PubMed] [Google Scholar]
- 6.Hansen KA, Weiss JA, Barton JK. Recruitment of tendon crimp with applied tensile strain. J Biomech Eng. 2002;124:72–7. doi: 10.1115/1.1427698. [DOI] [PubMed] [Google Scholar]
- 7.Lujan TJ, Underwood CJ, Henninger HB, Thompson BM, Weiss JA. Effect of dermatan sulfate glycosaminoglycans on the quasi-static material properties of the human medial collateral. J Orthop Res. 2007;25:894–903. doi: 10.1002/jor.20351. [DOI] [PubMed] [Google Scholar]
- 8.Mehrabani D, Manafi N. Role of cultured skin fibroblasts in aesthetic and plastic surgery. World J Plast Surg. 2013;2:2–5. [PMC free article] [PubMed] [Google Scholar]
- 9.Costagliola M, Agrosi M. Second-degree burns: a comparative,,multicenter, randomized trial of hyaluronic acid plus silver sulfadiazine vs silver sulfadiazine alone. Curr Med Res Opin. 2005;21:1235–40. doi: 10.1185/030079905X56510. [DOI] [PubMed] [Google Scholar]
- 10.Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008;16:585–601. doi: 10.1111/j.1524-475X.2008.00410.x. [DOI] [PubMed] [Google Scholar]
- 11.Rajabi H, Sheikhani Shahin H, Norouzian M, Mehrabani D, Dehghani Nazhvani S. The Healing Effects of Aquatic Activities and Allogenic Injection of Platelet-Rich Plasma (PRP) on Injuries of Achilles Tendon in Experimental Rat. World J Plast Surg. 2015;4:66–73. [PMC free article] [PubMed] [Google Scholar]
- 12.Modarressi A. Platlet Rich Plasma (PRP) Improves Fat Grafting Outcomes. World J Plast Surg. 2013;2:6–13. [PMC free article] [PubMed] [Google Scholar]
- 13.Manafi A, Kaviani Far K, Moradi M, Manafi A, Manafi F. Effects of platelet-rich plasma on cartilage grafts in rabbits as an animal model. World J Plast Surg. 2012;1:91–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Fenwick SA, Hazlelman BL, Riley GP. The vasulature and its role in the damaged and healing tendon. Arthritis Res. 2002;4:252–60. doi: 10.1186/ar416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hayem G. Tenology: a new frontier Joint, Bone, Spine. Rev Rhum. 2001;68:19–25. doi: 10.1016/s1297-319x(01)00261-5. [DOI] [PubMed] [Google Scholar]
- 16.Cervelli V, Gentile P, Brinci L, Pasquali CD, Bocchini I, Angelis BD. Use of platelet rich plasma (PRP) and hyaluronic acid in treatment of extremity gunshot injuries: a case report. World J Plast Surg. 2016;5:80–84. [PMC free article] [PubMed] [Google Scholar]
- 17.Edwards SG, Calandruccio JH. Autologous blood injections for refractory lateral epicondylitis. Am J Hand Surg. 2003;28:272–8. doi: 10.1053/jhsu.2003.50041. [DOI] [PubMed] [Google Scholar]
- 18.Reed GL. Platelet secretory mechanisms. Semin Thromb Hemost. 2004;30:441–50. doi: 10.1055/s-2004-833479. [DOI] [PubMed] [Google Scholar]
- 19.Anitua E, Sánchez M, Zalduendo MM, de la Fuente M, Prado R, Orive G, Andía I. Fibroblastic response to treatment with different preparations rich in growth factors. Cell Prolif. 2009;42:162–70. doi: 10.1111/j.1365-2184.2009.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stark HJ, Willhauck MJ, Mirancea N, Boehnke K, Nord I, Breitkreutz D, Pavesio A, Boukamp P, Fusenig NE. Authentic fibroblast matrix in dermal equivalents normalises epidermal histogenesis and dermoepidermal junction in organotypic coculture. Eur J Cell Biol. 2004;83:631–45. doi: 10.1078/0171-9335-00435. [DOI] [PubMed] [Google Scholar]
- 21.Whitlock PW, Smith TL, Poehling GG, Shilt JS, Van Dyke M. A naturally derived, cytocompatible, and architecturally optimized scaffoldfor tendon and ligament regeneration. Biomaterials. 2007;28:4321–9. doi: 10.1016/j.biomaterials.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 22.Maffulli N, Longo UG, Gougoulias N, Denaro V. Ipsilateral free semitendinosus tendon graft transfer for reconstruction of chronic tears of the Achilles tendon. BMC Musculoskelet Disord. 2008;9:100. doi: 10.1186/1471-2474-9-100. [DOI] [PMC free article] [PubMed] [Google Scholar]