Abstract
BACKGROUND
Unlike congenital auricular malformations which are identified by underdevelopment of dermal and cartilaginous tissues, deformed ears are less sever congenital anomalies characterized only by a misshaped pinna structure and can be improved with acceptable cosmetic results and minimal cost through ear molding if treated in early neonatal period. In this study, authors present the first report of using splinting techniques for treatment of deformational auricular anomalies in Iranian children.
METHODS
Our case load consisted of a series of 29 patients (Male=16, Female=13) who were referred to Plastic Surgery Unit of Shiraz University of Medical Sciences from September 2011 to December 2014. Children aged more than 6 moths were excluded. Twenty-nine children affected by various deformities including prominent ears (n=11), lop ears (n=8) and constricted ears (n=10) were treated by splintage as a nonsurgical technique. The mean time of treatment was 13.33±2 weeks.
RESULTS
Eight (27.6%) patients did not complete the treatment. Splinting resulted in excellent or satisfactory results in 12 (57.14%) of treated cases. No improvement was observed at the end of the molding treatment in 9 patients. No complication was observed during the treatment in any of the patients.
CONCLUSION
The nonsurgical molding can be used as an effective approach for achieving natural outcomes and correcting cosmetic abnormalities. Rate of satisfaction is dependent on type of deformity, the neonatal age in which treatment started and also parents’ adherence to treatment methods and principals. Concerning the low rate of complications and high satisfactory results the method can be used instead of surgery in appropriate cases.
Key Words: Congenital auricular deformities, Non-surgical, Management
INTRODUCTION
Anomalies of the auricles can lead to substantial social and communicating difficulties in the growing children. Congenital ear anomalies are categorized into either malformations (microtia, cryptotia), which are mostly caused due to embryologic maldevelopment in fetal auricular cartilage framework between the fifth and the ninth gestational week, or deformations that only show an abnormal shape without any irregularities in chondro-cutaneous components. Partial absence of skin or cartilage in malformations results in a constricted or underdeveloped pinna requiring surgical intervention during childhood or adolescence for best treatment.1,2
On the other hand, deformities including lop, constricted and Stahl’s ear are less severe forms arising after the ninth week of gestation with a misshaped but fully developed pinna and structural cartilage. Although several distinct types exist, prominent or protruding ears are the most common variant.3 Lop ears are characterized by drooping upper pole, whereas Stahl’s ears have abnormal kinks of the helix combined with an anti-helical crus perpendicular to the helical rim.4
Congenital ear deformities are not usually caused by disturbance in the process of morphogenesis but rather result as a consequence of external positioning forces determined by the pressure or malinsertion of the seven intrinsic and four extrinsic muscles in the prenatal period.5 To improve the appearance of children with such deformities, otoplasty as a common cosmetic surgical procedure to the plastic surgeons, is usually performed under general anesthesia especially in younger children.6
However, despite the introduction of many different surgical techniques in the past decades for correction and rehabilitation of this irritating aesthetic handicap, considerable collateral complications and the uneventful course of postoperative care have caused great interest in avoiding surgery.7 Further, surgical correction of deformities is usually performed between 5 and 6 years of age when the auricle has reached about 90% of the adult size.8 The concept of applying mechanical forces by using mold casting to achieve a normal shape in congenital deformities has been previously established in treatment of hip dislocation and club foot. In the late 1980s, Japanese plastic surgeons published the first reports of non-surgical correction of congenital auricular deformities and demonstrated that permanent correction may occur by forcing and maintaining the ear into the proper position for several weeks.9-11
Currently, ear deformities are usually amenable to early ear splinting and can be appropriately manipulated to a normal shape in the neonatal period. As neonatal auricle is immediately soft and becomes harder in the first weeks after birth while loosing its innate elasticity, it is believed that the earlier the molding starts, better results are obtained.12 In this study, authors present the first experience of ear molding in a case load of 29 Iranian children with deformational auricular anomalies who were treated over a 4-year period.
MATERIALS AND METHODS
Prior to the conduction of study the ear molding as a possible technique that may be performed in early ages instead of otoplasty was described to the staff in different neonatal wards affiliated with Shiraz university of Medical sciences. Furthermore, to raise awareness of parents related posters were installed on community notification boards of hospitals in popular spots. From September 2011 to December 2014 twenty-nine patients suffering from various types of ear deformities, who were found to be suitable cases for ear molding, were referred to our plastic surgery ward by the neonatal staff.
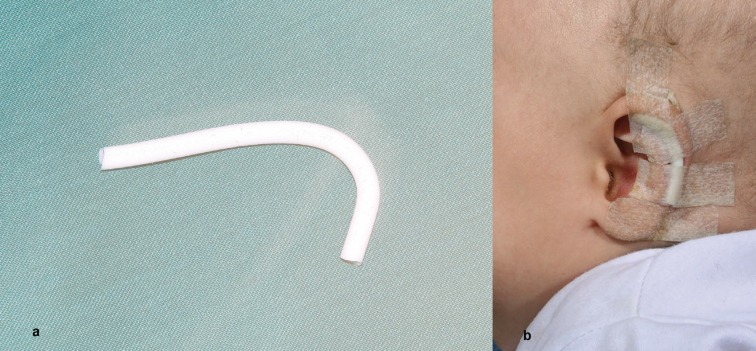
Children more than 6 months were also excluded. Prior to the start of treatment, patients were monitored for a 24 hours period to confirm that splinting was indicated and ears could not reform by spontaneous correction in a short or sudden course. Benefits of the proposed treatment in comparison to other alternatives and also the risks in achieving highly satisfactory results were thoroughly explained to the parents. Besides, an informed written consent was obtained from each participant’s parents in this study. The method we used was principally the same as the one described by Schonauer et al.13 Soft and flexible silicone with 4 mm diameter was used as the covering component of the splint whilst stainless steel wire was deployed within this segment (Figure 1a).
Fig. 1.
Public poster for introducing non-surgical management of congenital auricular deformities
Then, we curved the whole structure according to the desired shape and fixed it by surgical tapes on the anterolateral surface of the auricle in the groove between helix and antihelix as a supporting pillar. Surgical tapes could also help to position the auricle closer to the scalp (Figure 1b). Further, most patients wore elastic bonds as adjunct supporters to facilitate the process and keep the mold in place. Splinting was applied with no demand to any kinds of anesthetics. To prevent any complicated handling of the procedure by parents, we avoided using a second mold on the posteromedial aspect of the auricle as described in some previous studies.
Clinical evaluations were made at follow up visits every 2 weeks after beginning of the treatment. In each session the splintage was removed, remodeled according to the achieved correction and then and reapplied with fresh steri strips. Photographs were taken at each visit. To stabilize the correct form of ear, molding was continued after achieving early satisfactory results for one more month and final inspection was performed at this point after completion of molding. The criteria for assessment of cosmetic results was categorized as excellent (>80% improvement), improved (50-80% improvement), or minimal to not improved (<50% slight improvement or failure of the method).8
Improvement was rated by the surgeon and a trained nurse after comparing the initial and final photographs. All the procedures of the study were approved by the Ethics Committee of Shiraz University of Medical Sciences. Data were collected and presented as mean±SD. Statistical analysis was done by SPSS software (Version 20, Chicago, IL, USA) using Mann–Whitney U test, Kruskal–Wallis test and Spearman test for correlation. Statistical values p<0.05 were considered significant.
RESULTS
This non-surgical method was used to correct deformed auricles in 29 children. Thirteen patients were female and 16 were male. Of these auricular deformities, children represented prominent (n=6, 20.7% upper part - n=5, 17.2% lower part), lop (n=8, 27.6%) and constricted (n=10, 34.5%) ears. Eight patients including 3 cases with prominent ear (2 upper part, 1 lower part), 3 with lop ear and 2 with constricted ear were lost to follow ups as being non compliant. However, no treatment complication such as superficial skin irritation or necrosis was observed. Besides, we recorded no recurrence in any of the patients who completed the molding course. For those who completed the molding course, the average age at the start of study was 7.52±5.60 weeks (Min=2, Max=24). Age at the onset of treatment for each group is shown in Table 1.
Table 1.
Age at the onset of treatment for each group
| Age (weeks) | Mean±SD | Min | Max |
|---|---|---|---|
| Prominent (upper part) ear | 8.25±6.84 | 2 | 16 |
| Prominent (lower part) ear | 10.25±9.25 | 4 | 24 |
| Lop ear | 6.40±3.04 | 3 | 10 |
| Constricted ear | 6.50±4.56 | 2 | 16 |
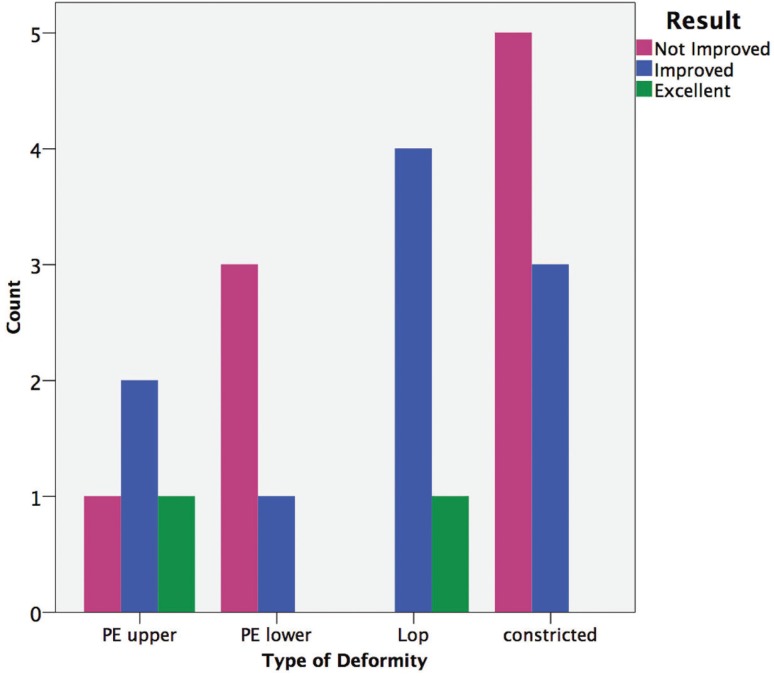
The average duration of treatment for those who completed the treatment was 13.33±2 weeks (Min=11, Max=18). All types of ears required similar period of treatment and there was no significant difference in managing time between the diverse treated forms of deformities (p=0.997). There was no significant correlation between the onset age of splinting and the achieved results. Regardless of those who abandoned treatment, more than 50% of children enrolled in this study obtained improvement. The end results ratings are summarized in Table 2 and Figure 2.
Table 2.
The correlation between the onset age of splinting and the achieved results
| Variable | Excellent | Improved | Not improved | Total |
|---|---|---|---|---|
| Prominent (upper) ear | 1 | 2 | 1 | 4 |
| Prominent (lower) ear | 0 | 1 | 3 | 4 |
| Lop ear | 1 | 4 | 0 | 5 |
| Constricted ear | 0 | 3 | 5 | 8 |
| Total | 2 | 10 | 9 | 21 |
Fig. 2.
a) Ear mold shape, (b) splintage supported in place by surgical tapes
The mean onset age of treatment in patients who had no improvement at the end of splinting was higher than those with improvement or excellent results; however, there was no significant difference in average onset age between the two groups (p=0.193). Table 3 depicts patients mean age categorized according to final outcome. It is noteworthy that most parents were sensitive about taking photographs of their children and only 8 cases actually allowed us to publish the images of which three cases are demonstrated in Figures 3-5. Synchronically with the active efforts in advancing the effectiveness of mold casting, in the next phases of our study, we planned to upgrade the mold by designing new and optimized templates that can cover the entire auricle and form the ear in a more dynamic state (Figure 6).
Table 3.
The patients’ mean age according to final treatment outcome
| Age (weeks) | Mean±SD | Min | Max |
|---|---|---|---|
| Excellent (N=2) | 4.00±2.82 | 2 | 6 |
| Improved (N=10) | 6.40±3.56 | 2 | 12 |
| Not improved (N=9) | 9.55±7.33 | 3 | 24 |
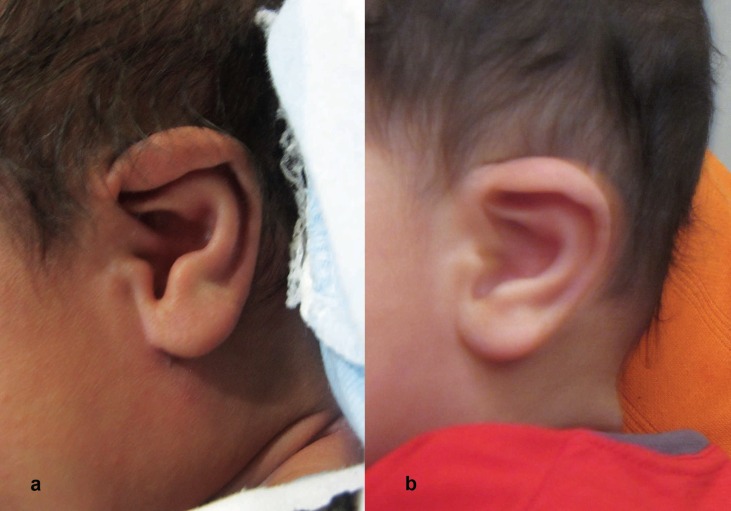
Fig. 3.
(a) left sided lope ear, (b) correction at the end of molding
Fig. 5.
(a) A girl with right sided prominent ear, (b) (c) the same auricle after mold casting
Fig. 6.
a) Design of the new ear mold, (b) application of the new mold covering the entire auricle
Fig. 4.
(a) right sided prominent ear, (b) the same child after completion of auricular splintage
DISCUSSION
Although, there are various reports about the incidence of different types of congenital ear anomalies, a comprehensive data is still lacking. Outer ear malformations is believed to affect neonates with a ratio of 1 in 6000 births.14 There is also no specific data available on the prevalence of auricular anomalies in Iranian newborns. However, deformed auricles seem to account for 3.2% of congenital deformities.15 Causes of these deformities vary from abnormal functioning of the ear muscles during the prenatal life to malpostioning of the head in the neonatal periods. Our report agrees with the study of Merlob et al. as none of the patients demonstrated spontaneous correction.16
In most studies, judgment on the results is empirically made by authors or by asking a lay opinion. Few recurrences are reported in the literature, probably due to short follow-up time or placing the results in poor category. Similar to many other studies we utilized rounded splints, which can be easily bended in the scaphal hollow. However, Yotsuyanagi has reported that in conditions such as cryptotia a rigid splint with the ability to sandwich the ear from both sides is largely preferred.17,18 Also for the treatment of protruding ears, Sorribes presented the interesting concept of a specially designed plastic clamp, named as the Auri method, to maintain bilateral squeeze pressure during the night.19
We planned to upgrade the mold by designing new and optimized templates that can cover the entire auricle and form the ear in a more dynamic state (Figure 6). Despite the lack of clear data in the literature, results are frequently poor in older children; however, fair to excellent outcomes are reported in 70-100% of cases.20 Matsuo, one of the first pioneers on this method, states that satisfactory and irreversible results can be obtained if treatment started at least by the third day after birth.10 Tan et al., as additional advocates for early diagnosis, emphasized that to increase the efficacy, it is pivotal to initiate molding in the first three months of life.21,22
On the contrary, successful treatment of over 50% of children older than 1 year (0-14 years) using thermoplastic moldings with average period of 2.1 months splint application has been reported by Yotsuyanagi et al.17,18 Further, in a 2004 study on 243 patients he showed a varying rate of success from 91% in newborns to 33% in 9-year-olds.23 In Doft study on 158 ears using the Ear Well Infant Ear Correction System before 2 weeks of life 96 percent of the deformities were corrected with an average treatment time of 14 days. Authors concluded that initiating molding during the first weeks of life by using a more rigid device can reduce the molding period from 6-8 weeks to 2 weeks.24
Ear splinting applies external pressure and force on dermal and cartilaginous components of auricular structure. External stresses affect mechanochemical transduction in cartilage, and subsequently cartilage behavior and structure. Mechanical loading induced strains change the expression of genes and the regulation of cellular metalloproteinases levels and induction of collagen and aggrecan biosynthesis as result of both cell–cell and cell–extra cellular matrix interactions.25,26 Skin size can also reform as a response to tensile force.27,28 Besides, the malleable nature of the neonatal ear is directly controlled by blood levels of hyaluronic acid, which is elevated by maternal estrogen and plays crucial role in the elasticity of ear cartilage.29
Normally, circulating estrogen is highest during the first 72 hours after birth and then declines rapidly to those similar in children by 6 weeks of age. Thus, reshaping is easily achieved in a newborn infant when the responsiveness of ear cartilage is immense. Accordingly, breast-feeding extends the presence of milk estrogen in blood and prolongs the required interval for molding.30,31 Compared to the literature the results from our study are not highly satisfactory. A major portion of our patients was from rural areas and of lower social classes and hence, step by step adherence to treatment guidelines by patients’ parents was not satisfactory. Additionally, a large proportion of our patients presented late. Consequently, this indicates the importance of starting splinting soon after birth. It should also be noted that several other authors state that only newborns should be treated and mentioned poor results in older babies.16,32,33
Surprisingly, this elegant non-invasive technique is not widely practiced by plastic surgeons. On the other hand, there are mostly low knowledge in general public and medical associations about such procedure. Moreover, the belief about gradual self-correction of misshapen ears in all infants will definitely lower the chance of early diagnosis and hinder the possibility of a non-surgical prosperous treatment at an appropriate age when splints can be applied. In a Mayo Clinic pilot study of ten infants who were identified by newborn hearing screeners, educated on evaluation of congenital auricular deformities, all patients exhibited improvement from the original deformity after 1-4 weeks of correction with a simple splint initiated immediately in neonatal period. This pilot study shows that early identification of auricular deformities by properly educated newborn hearing screeners is an ideal opportunity that can enhance successful and early initiation of splinting therapy.34
Thus, raising the awareness among the medical community and parents by lectures and through the media not only may help children with such annoying deformities in an early age but also can save them from the consequent complications of future surgical interventions including infection, hemorrhage, scarring and residual deformity.
ACKNOWLEDGMENT
Authors appreciate contribution of Ms. Mitra Zartosht in preparing and completion of this article. This work was part of plastic surgery thesis by Dr. Ali Akbar Mohammadi at the Faculty of Medicine, Shiraz University of Medical Sciences.
Please cite this paper as:
Mohammadi AA, Imani MT, Kardeh S, Karami MM, Kherad M. Non-surgical Management of Congenital Auricular Deformities. World J Plast Surg 2016;5(2):139-147.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
References
- 1.Porter CJ, Tan ST. Congenital auricular anomalies: topographic anatomy, embryology, classification, and treatment strategies. Plast Reconstr Surg. 2005;115:1701–12. doi: 10.1097/01.prs.0000161454.08384.0a. [DOI] [PubMed] [Google Scholar]
- 2.Artunduaga MA, Quintanilla-Dieck MD, Greenway S, Betensky R, Nicolau Y, Hamdan U, Jarrin P, Osorno G, Brent B, Eavey R, Seidman C, Seidman JG. A classic twin study of external ear malformations, including microtia. N Engl J Med. 2009;361:1216–8. doi: 10.1056/NEJMc0902556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith WG, Toye J, Smith R. Nonsurgical treatment of protruding ears: A case report and review of literature. Can J Plast Surg. 2003;11:87. doi: 10.1177/229255030301100202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakajima T, Yoshimura Y, Kami T. Surgical and conservative repair of Stahl’s ear. Aesthet Plast Surg. 1984;8:101–7. doi: 10.1007/BF01575252. [DOI] [PubMed] [Google Scholar]
- 5.Thorne CH, Wilkes G. Ear deformities, otoplasty, and ear reconstruction. Plast Reconstr Surg. 2012;129:701e–16e. doi: 10.1097/PRS.0b013e3182450d9f. [DOI] [PubMed] [Google Scholar]
- 6.Gasques JL, de Godoy JP, Cruz EN. Psychosocial effects of otoplasty in children with prominent ears. Aesthetic Plast Surg. 2008;32:910–4. doi: 10.1007/s00266-008-9179-x. [DOI] [PubMed] [Google Scholar]
- 7.Kelley P, Hollier L, Stal S. Otoplasty: evaluation, technique, and review. J Craniofac Surg. 2003;14:643–53. doi: 10.1097/00001665-200309000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Ullmann Y, Blazer S, Ramon Y, Blumenfeld I, Peled IJ. Early nonsurgical correction of congenital auricular deformities. Plast Reconstr Surg. 2002;109:907–13. doi: 10.1097/00006534-200203000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Kurozumi N, Ono S, Ishida H. Non-surgical correction of a congenital lop ear deformity by splinting with Reston foam. Br J Plast Surg. 1982;35:181–2. doi: 10.1016/0007-1226(82)90160-6. [DOI] [PubMed] [Google Scholar]
- 10.Matsuo K, Hirose T, Tomono T, Iwasawa M, Katohda S, Takahashi N, Koh B. Nonsurgical correction of congenital auricular deformities in the early neonate: a preliminary report. Plast Reconstr Surg. 1984;73:38–50. doi: 10.1097/00006534-198401000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Muraoka M, Nakai Y, Sasaki T, Ohashi Y, Maruoka K, Furukawa M. Tape attachment therapy for correction of congenital malformations of the auricle: clinical and experimental studies. Laryngoscope. 1985;95:167–76. doi: 10.1288/00005537-198502000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Leonardi A, Bianca C, Basile E, Ungari C, Arangio P, Filiaci F, Papoff P, Vellone V, Moretti C, Cascone P. Neonatal molding in deformational auricolar anomalies. Eur Rev Med Pharmacol Sci. 2012;16:1554–8. [PubMed] [Google Scholar]
- 13.Schonauer F, La Rusca I, Molea G. Non-surgical correction of deformational auricular anomalies. J Plast Reconstr Aesthet Surg. 2009;62:876–83. doi: 10.1016/j.bjps.2007.11.072. [DOI] [PubMed] [Google Scholar]
- 14.Bartel-Friedrich S, Wulke C. Classification and diagnosis of ear malformations. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2007;6:Doc05. [PMC free article] [PubMed] [Google Scholar]
- 15.Karbasi SA, Golestan M, Fallah R, Mirnaseri F, Barkhordari K, Bafghee MS. Prevalence of congenital malformations. Acta Medica Iranica. 2009;47:149–53. [Google Scholar]
- 16.Merlob P, Eshel Y, Mor N. Splinting therapy for congenital auricular deformities with the use of soft material. J Perinatol. 1994;15:293–6. [PubMed] [Google Scholar]
- 17.Yotsuyanagi T, Yokoi K, Sawada Y. Nonsurgical treatment of various auricular deformities. Clin Plast Surg. 2002;29:327–32. doi: 10.1016/s0094-1298(01)00011-6. [DOI] [PubMed] [Google Scholar]
- 18.Yotsuyanagi T, Yokoi K, Urushidate S, Sawada Y. Nonsurgical correction of congenital auricular deformities in children older than early neonates. Plast Reconstr Surg. 1998;101:907–14. doi: 10.1097/00006534-199804040-00004. [DOI] [PubMed] [Google Scholar]
- 19.Sorribes MM, Tos M. Nonsurgical treatment of prominent ears with the Auri method. Arch Otolaryngol Head Neck Surg. 2002;128:1369–76. doi: 10.1001/archotol.128.12.1369. [DOI] [PubMed] [Google Scholar]
- 20.Byrd HS, Langevin C-J, Ghidoni LA. Ear molding in newborn infants with auricular deformities. Plast Reconstr Surg. 2010;126:1191–200. doi: 10.1097/PRS.0b013e3181e617bb. [DOI] [PubMed] [Google Scholar]
- 21.Tan S, Wright A, Hemphill A, Ashton K, Evans J. Correction of deformational auricular anomalies by moulding: Results of a fast-track service. NZ Med J. 2003;116:U584. [PubMed] [Google Scholar]
- 22.Tan ST, Abramson DL, MacDonald DM, Mulliken JB. Molding therapy for infants with deformational auricular anomalies. Ann Plast Surg. 1997;38:263–8. doi: 10.1097/00000637-199703000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Yotsuyanagi T. Nonsurgical correction of congenital auricular deformities in children older than early neonates. Plast Reconstr Surg. 2004;114:190–1. doi: 10.1097/01.prs.0000128819.03187.5d. [DOI] [PubMed] [Google Scholar]
- 24.Doft MA, Goodkind AB, Diamond S, DiPace JI, Kacker A, LaBruna AN. The Newborn Butterfly Project: A Shortened Treatment Protocol for Ear Molding. Plast Reconstr Surg. 2015;135:577e–83e. doi: 10.1097/PRS.0000000000000999. [DOI] [PubMed] [Google Scholar]
- 25.Silver FH, Bradica G. Mechanobiology of cartilage: how do internal and external stresses affect mechanochemical transduction and elastic energy storage? Biomech Model Mechanobiol. 2002;1:219–38. doi: 10.1007/s10237-002-0017-9. [DOI] [PubMed] [Google Scholar]
- 26.Huang AH, Farrell MJ, Mauck RL. Mechanics and mechanobiology of mesenchymal stem cell-based engineered cartilage. J Biomech. 2010;43:128–36. doi: 10.1016/j.jbiomech.2009.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ladd MR, Lee SJ, Atala A, Yoo JJ. Bioreactor maintained living skin matrix. Tissue Eng Part A. 2008;15:861–8. doi: 10.1089/ten.tea.2008.0195. [DOI] [PubMed] [Google Scholar]
- 28.Wilson CJ, Pearcy MJ, Epari DR. Mechanical tension as a driver of connective tissue growth in vitro. Med Hypotheses. 2014;83:111–5. doi: 10.1016/j.mehy.2014.03.031. [DOI] [PubMed] [Google Scholar]
- 29.Uzuka M, Nakajima K, Ohta S, Mori Y. The mechanism of estrogen-induced increase in hyaluronic acid biosynthesis, with special reference to estrogen receptor in the mouse skin. Biochim Biophys Acta. 1980;627:199–206. doi: 10.1016/0304-4165(80)90321-9. [DOI] [PubMed] [Google Scholar]
- 30.Patriarca MT, de Moraes ARB, Nader HB, Petri V, Martins JRM, Gomes RCT, Soares JM Jr. Hyaluronic acid concentration in postmenopausal facial skin after topical estradiol and genistein treatment: a double-blind, randomized clinical trial of efficacy. Menopause. 2013;20:336–41. doi: 10.1097/GME.0b013e318269898c. [DOI] [PubMed] [Google Scholar]
- 31.Lindford AJ, Hettiaratchy S, Schonauer F. Postpartum splinting of ear deformities. Br Med J. 2007;334:366. doi: 10.1136/bmj.39063.501377.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oroz J, Pelay M, Colas C, Pérez M, Rabell J. Congenital anomalies of the auricle: correction using external splints. Eur J Plast Surg. 1995;18:288–92. [Google Scholar]
- 33.Smith W, Toye J, Reid A, Smith R. Nonsurgical correction of congenital ear abnormalities in the newborn: case series. Pediatr Child Health. 2005;10:327. doi: 10.1093/pch/10.6.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Petersson RS, Recker CA, Martin JR, Driscoll CL, Friedman O. Identification of congenital auricular deformities during newborn hearing screening allows for non-surgical correction: A Mayo Clinic pilot study. Int J Pediatr Otorhinolaryngol. 2012;76:1406–12. doi: 10.1016/j.ijporl.2012.06.011. [DOI] [PubMed] [Google Scholar]