To the Editor
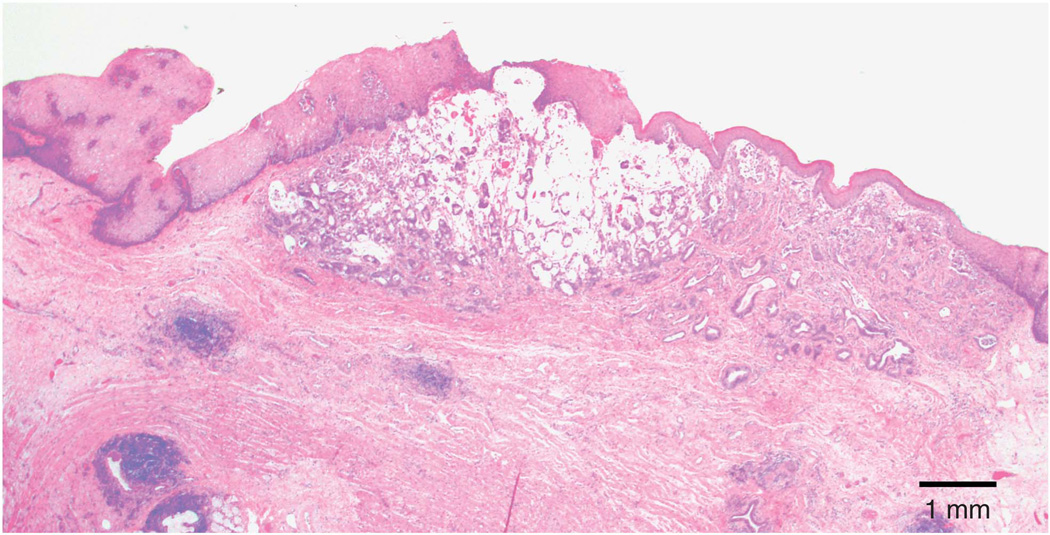
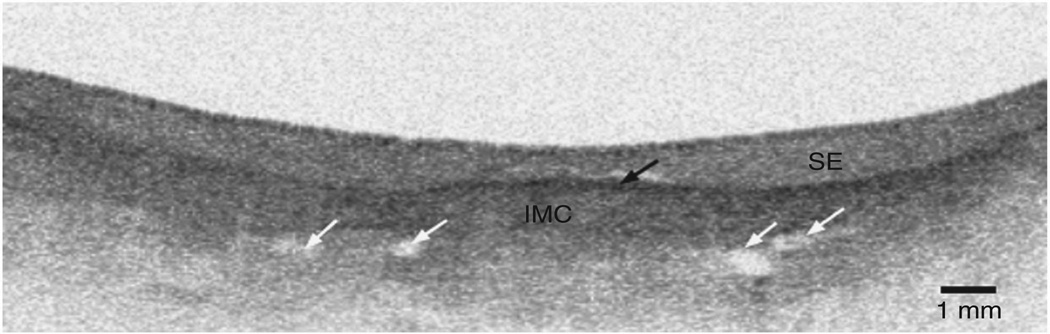
A 74-year-old patient with Barrett’s esophagus (BE) (C5M5) enrolled in a surveillance program was found to have intramucosal adenocarcinoma (IMC) arising in the background of high-grade dysplasia at the gastroesophageal junction. He was treated with a combination of endoscopic mucosal resection (EMR) and radiofrequency ablation (RFA) and achieved complete eradication of intestinal metaplasia. Surveillance biopsies obtained a year following his last RFA treatment showed moderately differentiated IMC identified under squamous epithelium (SE) at a site close in location to his previous cancer. This was not seen on a high-resolution white light endoscopy and was only detected on mapping biopsies. A subsequent EMR was performed over an area of normal-appearing mucosa corresponding to the prior biopsy site. Histopathology demonstrated moderate to poorly differentiated IMC invading into the lamina propria and muscularis mucosa with negative mucosal and submucosal margins for cancer (Figure 1). Endoscopic ultrasound did not show evidence of esophageal wall thickening or regional lymphadeno pathy. Imaging with confocal laser endomicroscopy (CLE) and volumetric laser endomicroscopy (VLE) was performed on the EMR specimen immediately following resection to ensure visualization of identical areas. Surface imaging with CLE using the fluorescent glucose analog 2-NBDG showed a homogenous layer of SE (1). Cross-sectional imaging with VLE demonstrated BE with features suggestive of IMC, including increased signal intensity (black arrow) with numerous atypical-appearing glands and dilated ducts (white arrows) underneath a layer of SE (Figure 2).
Figure 1.
Endoscopic mucosal resection showing subsquamous moderate to poorly differentiated adenocarcinoma invading into the lamina propria and muscularis mucosa.
Figure 2.
Volumetric laser endomicroscopy of endoscopic mucosal resection with features suggestive of intramucosal adenocarcinoma (IMC), including increased signal intensity (black arrow) with atypical appearing glands and dilated ducts (white arrows) underneath a layer of squamous epithelium (SE).
Subsquamous BE is found in ~0.9% of surveillance biopsies following RFA (2). Most of the time, subsquamous BE is non-dysplastic but cancer has clearly been found in multiple series and presents a challenging diagnosis (3). VLE is a second-generation optical coherence tomography device that can generate in-vivo three-dimensional views of the human esophagus (4). Advantages of VLE over CLE are the capacity to perform wide-field imaging and the ability to visualize deeper into the mucosa (Supplementary Figures S1–S3 online). After ablative therapy for BE, it is essential to perform careful mapping biopsies of the mucosa to detect these small areas of residual cancer. This is the first case reported where VLE could clearly detect subsquamous Barrett ’ s adenocarcinoma, which was not seen by routine white light endoscopy or CLE. The use of in-vivo VLE has the potential to enhance the diagnosis of subsquamous BE and associated neoplasia.
Supplementary Material
Footnotes
SUPPLEMENTARY MATERIAL is linked to the online version of the paper at http://www.nature.com/ajg
CONFLICT OF INTEREST
The authors declare no conflict of interest.
REFERENCES
- 1.Gorospe EC, Leggett CL, Sun G, et al. Diagnostic performance of two confocal endomicroscopy systems in detecting Barrett’s dysplasia: a pilot study using a novel bioprobe in ex vivo tissue. Gastrointest Endosc. 2012;76:933–938. doi: 10.1016/j.gie.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Gray NA, Odze RD, Spechler SJ. Buried metaplasia after endoscopic ablation of Barrett’s esophagus: a systematic review. Am J Gastroenterol. 2011;106:1899–1908. doi: 10.1038/ajg.2011.255. quiz 1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Titi M, Overhiser A, Ulusarac O, et al. Development of subsquamous high-grade dysplasia and adenocarcinoma after successful radiofrequency ablation of Barrett’s esophagus. Gastroenterology. 2012;143:564–566 e1. doi: 10.1053/j.gastro.2012.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vakoc BJ, Shishko M, Yun SH, et al. Comprehensive esophageal microscopy by using optical frequency-domain imaging (with video) Gastrointest Endosc. 2007;65:898–905. doi: 10.1016/j.gie.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.