Abstract
The epidemic of HIV/AIDS among Chinese men who have sex with men (MSM) is rapidly escalating. We implemented partner notification among HIV-infected MSM, cooperating with MSM-serving community-based organizations (CBOs) in two Chinese cities from June 2014 to May 2015. CBOs participated in identifying new HIV-positive MSM utilizing rapid HIV tests and partner notification among index cases. 253 index cases were recruited and 275 sexual partners were notified and tested with 10.5% screened positive. Compared with previously identified index cases, the proportion of contactable sexual partners of newly identified index cases was higher, but the testing rate was lower (p < 0.001). Overall, 83.7% of sexual partners were casual with a contactable rate of 24.9% and a HIV testing rate of 71.1%. Having no contact information for sexual partners and fear of disclosure of HIV status are the main reasons for declining partner notification. It is feasible and effective to perform partner notification in cooperation with CBOs serving Chinese MSM.
Keywords: Partner notification, HIV/AIDS, screening, community-based organizations, MSM
Background
Although the national HIV prevalence remains at a relatively low level in China, it is clearly on the rise in recent years through sexual transmission. HIV transmission through male–male sex is of particular concern.1 Responding to the rapidly escalating epidemic among men who have sex with men (MSM), expanding HIV testing and scaling up antiretroviral treatment (ART) have been taken as key intervention strategies in China. In addition, the Chinese government emphasized multi-sector coordination and involvement in HIV prevention and control, especially the involvement of community-based organizations (CBOs). This commitment has been clearly described in ‘the 12th Five-Year Plan of Action for Containment and Control of AIDS’. Supported by international and domestic programs, CBOs have played an important role in HIV testing promotion and case finding, especially among MSM.2–4 Although HIV testing coverage is gradually increasing, controlling the HIV epidemic among Chinese MSM still faces challenges.5,6 A large proportion of HIV infections remain undiagnosed or are diagnosed late, posing a vital potential risk for the growing epidemic of HIV/AIDS.7 Measures to effectively identify undiagnosed HIV infections are vital for the control of the HIV/AIDS epidemic in the MSM population.
Previous research suggested that interventions related to sexual partners were valuable and widely accepted in the control of syphilis and gonorrhea.8 Because of the complex sexual networks of MSM, partner notification (PN) and HIV testing might effectively reduce HIV transmission among sero-discordant MSM sexual partners. However, it was deemed that such interventions were underused in the control of HIV infection.9–11 In China, several studies have indicated the value of PN and HIV testing in HIV case finding.12–14 Results of these studies showed a newly identified HIV infection rate of 10%–20%, which was more effective than voluntary counseling and testing (3%), but also showed a high rejection and attrition rate (30%–50%).12,13,15 However, PN and counseling in most studies were focused on the wives of married MSM or stable sexual partners in married and HIV sero-discordant couples. These studies were usually conducted by health workers of local Centers for Disease Control and Prevention (CDCs). Among HIV-infected MSM, interventions targeting their sexual partners were more challenging than among the non-MSM population.16–19 Given that both HIV infection and homosexuality remain highly stigmatized in China,5 health departments and clinics face great challenges in performing sexual partner mobilization among HIV-infected MSM. MSM-serving CBOs may be a strategic ally in the mission to reach the population, as they are well established hubs with access to the demographic.4,20,21 Their participation might be advantageous for improving the implementation of interventions targeting the sexual partners of HIV-infected MSM.
To explore the feasibility and efficiency of sexual PN and HIV testing among HIV-positive MSM in cooperation with MSM-serving CBOs, we performed a pilot study in two Chinese cities. Our study is among the first to conduct a PN and HIV testing program specifically for HIV-infected MSM in cooperation with MSM-serving CBOs.
Methods
Study design
This pilot study was based on a HIV testing promotion program among MSM in two Chinese cities. We cooperated with MSM-serving CBOs to mobilize sexual partners of MSM who were screened to be HIV reactive (hereafter referred as index cases, ICs) for HIV testing. ICs were recruited in two ways. First, the screened reactive MSM identified through our HIV testing promotion program were invited by MSM-serving CBO staff to further join our pilot PN and testing study. Second, to look at differences between the newly and previously identified infections in PN and testing promotion, we also cooperated with local CDCs to recruit ICs among HIV infected MSM who were reported through the national AIDS case reporting system over the previous six months. When those previously reported HIV-infected MSM accessed care services (such as CD4 testing) at local CDCs, local CDC and CBO staff would invite them to participate in our study. Each study city was required to recruit at least 50 participants based on a convenient sampling design.
HIV testing promotion among MSM
The key objective of our current HIV testing promotion program was to explore effective models in promoting HIV case finding among MSM. We cooperated with MSM-serving CBOs to conduct HIV testing intervention among MSM through various approaches including web-based intervention on MSM websites or through MSM apps, outreach intervention by CBOs in MSM gathering areas (e.g. bars, bath houses and clubs) and peer-referrals. MSM who were reached and were willing to have a HIV test were referred to CBO-run HIV testing points (usually the CBO’s office) for HIV rapid testing. HIV rapid testing was also provided by CBO staff in intervention spots such as bathhouses or bars. Each MSM who was tested for HIV was interviewed face-to-face and a questionnaire was completed, collecting information on social democratic characteristics, male–male sexual behaviors, and HIV testing results. If they screened reactive, we interviewed them face-to-face to collect information on their sexual partners, invite them to join our pilot study and refer them to local CDCs for HIV confirmatory tests and subsequent HIV care services. MSM who screened negative for HIV would also receive post-test counseling related to health education.
Two HIV rapid tests were used to screen for HIV infection, following a serial testing algorithm. A first negative rapid test was reported as negative, while a first reactive was followed with a second screening test using a different testing kit. If two screening tests were reactive, this would be reported as screening reactive. The reactive MSM were then referred to local CDCs for a HIV confirmation test (HIV Blot 2.2, Genelabs Diagnostics, Singapore). Only confirmed positive MSM were reported as HIV-infected MSM. The screening testing kits used in this study were finger prick test kits (Alere Determine HIV-1/2Rapid Test®, Abbott Laboratories, USA) and oral test kits (Aware HIV-1/2 OMT, Beijing Marrbio Ltd, Beijing, China).
Study sites
The study was conducted from June 2014 to May 2015 in Hangzhou, the capital of Zhejiang Province and Kunming, the capital of Yunnan Province. The two cities were selected based on previous working experience with CBOs and their willingness to participate. In Hangzhou, the field study was implemented by Zhejiang Provincial CDC and Hangzhou CDC in cooperation with three MSM-serving CBOs: Zhejiang Xinling Huhang Center (ZXHC), Zhejiang Aixin Group (ZAG), and Hong Si Dai Group (HSDG). In Kunming, the Yunnan Provincial CDC and one MSM-serving CBO, Cai Yun Tian Kong Group, were jointly in charge of field study implementation.
PN and testing process
For ICs identified through our HIV testing promotion program, the PN and testing mobilization process started once MSM were screened reactive. With the support of local CDCs, CBO staff provided counseling to those MSM who screened reactive and invited them to participate in our pilot study. They were given basic information about this study, the benefits of early disease detection, assurance of confidentiality and privacy protection for themselves and their sexual partners, and their rights, benefits and potential risks for participation. If somebody refused to participate, MSM-serving CBOs would still continue follow-up, encouraging him to notify his sexual partners and offering assistance. For those previously identified HIV-infected MSM who participated in the study (ICs), the PN and testing promotion process started when they agreed to participate.
Both the newly screened HIV-reactive MSM and previously identified HIV-infected MSM were interviewed face-to-face by the CBO staff. First, their attitude toward PN and HIV testing mobilization and reasons for refusing to notify partners were collected. If they agreed to participate, the CBO staff would obtain informed consent for participation and continue to collect information on social demographic characteristics, frequency of condom use during anal sex in the past six months, number of different types of sexual partners (stable male partners in the past year, casual male and commercial male partners and other female partners in the past six months, including wives of married MSM), and numbers of different types of sexual partners who could be reached. The interview also collected information on their reachable sexual partners: name, age, education level, relationships, contact information (specifically phone number), and sexual behaviors. A unique code was assigned for each participant, linking the questionnaire and HIV testing results.
Next, ICs were offered several options of ways of contacting their different sexual partners. The ICs could choose to mobilize their sexual partners for HIV testing themselves. CBO staff would keep in touch with ICs. If the ICs failed to contact their sexual partners within a month, the CBO staff would contact them directly. The ICs could also ask CBO staff to contact their sexual partners at the outset. In this case, CBO staff would not disclose the IC’s HIV infection status to their sexual partners. They only informed them that one of their partners had been confirmed HIV-positive, and suggested HIV testing for them. The ICs could also ask local CDC staff to contact any of their sexual partners.
Since this was the first time for MSM-serving CBOs in the two cities to be involved in PN and testing mobilization, we invited national experts, experienced CBO staff from other provinces, and HIV-infected MSM as key informants to join a discussion workshop on how to conduct PN and testing promotion. Key topics included how to illicit information on sexual partners, how to initiate a conservation with sexual partners, how to reduce partners’ concerns on confidentiality and privacy protection, etc. MSM-serving CBOs contacted sexual partners of ICs in various ways based on ICs’ individual situation and preference, including telephone calls, chatting using instant message tools and arranging individual meetings at a bar or their offices. For example, several ICs strongly refused to let their wives know that they had sex with men, but agreed to let their wives know their HIV-infection status. The local CDC instead of MSM-serving CBO would notify their wives and provide HIV testing, avoiding exposing ICs’ homosexuality. For those partners who refused for HIV testing, CBO staff would continually contact them at least twice in case they might change their minds.
Once a sexual partner was approached and was willing to participate in this study, CBO staff would provide HIV rapid testing and counseling. If screened reactive, partners would be invited as ICs for the second round of PN and testing mobilization. And so on, screened reactive partners of ICs in the second round would be invited as ICs for the third round. The PN and testing process ended when the third round finished, for there was no screened reactive partners in the third round.
In this study, MSM-serving CBOs were responsible for counselling, performing HIV rapid tests, and referral of screened HIV reactive MSM to local CDC for confirmatory HIV test and subsequent care services. They were also responsible for recruitment of ICs and contacting their sexual partners. CDCs were mainly responsible for supervision and technical support for CBOs and provision of HIV confirmatory tests for screened reactive MSM.
Statistical analysis
Data related to the questionnaire and HIV tests were entered and verified with EpiData software (EpiData 3.1 for windows, The EpiData Association Odense, Denmark), and then analyzed with Statistical Product and Service Solutions (SPSS19.0 for Windows, SPSS Inc., Chicago, IL, USA).
Descriptive analyses were used to show social demographic characteristics, frequency of condom use in the past six months, numbers and types of sexual partners of the ICs, the process of sexual PN and HIV testing promotion, and the attitude of ICs regarding PN. Pearson’s Chi square tests and Fisher’s exact tests were performed to explore the difference for PN and testing process between the newly identified primary ICs and previously identified primary ICs, as well as differences among varying types of sexual partners of the ICs. Although several options were offered for ICs, most PN and testing mobilization were conducted by CBOs excepting local CDCs assisted in reaching several wives of MSM. Therefore, we did not analyze roles of different agency models in PN and testing promotion. Given the limit of a relatively small sample size, we did not analyze the difference of PN and testing process between the two cities too.
Ethics approval
This study was reviewed and approved by the Institutional Review Board of the National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention.
Results
Characteristics of HIV infected ICs
Socio-demographic characteristics
Of the 253 ICs, 148 (58.5%) were newly identified during HIV testing promotion and PN and testing process, 105 (41.5%) were previously identified and registered in the National AIDS Information System (Table 1). In all, 148 (58.5%) were recruited in Hangzhou and the rest recruited in Kunming. In all, 186 (73.5%) aged from 20 to 39 years old, 233 (92.1%) achieved a high school education and above, and 152 (60.1%) were single. Compared with previously identified cases, more newly identified HIV cases were recruited in Hangzhou and aged from 20 to 29 years old (p = 0.007 and p = 0.004, respectively).
Table 1.
Social-demographic and behavioral characteristics of newly and previously identified index cases (ICs).
| Variables | Newly identified HIV positivesa |
Previously identified HIV positivesb |
Total |
|||
|---|---|---|---|---|---|---|
| n = 148 | % | n = 105 | % | n = 253 | % | |
| Field sites (χ2 = 7.29, p = 0.007) | ||||||
| Hangzhou | 97 | 65.5 | 51 | 47.2 | 148 | 58.5 |
| Kunming | 51 | 34.5 | 54 | 52.8 | 105 | 41.5 |
| Age (Fisher’s exact test, p = 0.004) | ||||||
| 20–29 | 69 | 46.6 | 28 | 26.7 | 97 | 38.3 |
| 30–39 | 48 | 32.4 | 41 | 39.1 | 89 | 35.2 |
| 40–49 | 24 | 16.2 | 32 | 30.5 | 56 | 22.1 |
| ≥50 | 7 | 4.7 | 4 | 3.8 | 11 | 4.4 |
| Education | ||||||
| Primary school or less | 13 | 8.8 | 7 | 6.7 | 20 | 7.9 |
| High school | 74 | 50.0 | 64 | 61.0 | 138 | 54.6 |
| College graduate or above | 61 | 41.2 | 34 | 32.4 | 95 | 37.6 |
| Marriage | ||||||
| Single | 90 | 60.8 | 62 | 59.1 | 152 | 60.1 |
| Married | 47 | 31.8 | 29 | 27.6 | 76 | 30.0 |
| Divorce/widowed | 10 | 6.8 | 13 | 12.4 | 23 | 9.1 |
| Unknown | 1 | 0.7 | 1 | 1.0 | 2 | 0.8 |
| Self-reported sexual role | ||||||
| Mainly insertive | 29 | 19.6 | 31 | 29.5 | 60 | 23.7 |
| Mainly receptive | 62 | 41.9 | 31 | 29.5 | 93 | 36.8 |
| Both | 57 | 38.5 | 43 | 41.0 | 100 | 39.5 |
| Self-reported sexual orientation | ||||||
| Homosexual | 96 | 64.9 | 82 | 78.1 | 178 | 70.4 |
| Heterosexual | 1 | 0.7 | 1 | 1.0 | 2 | 0.8 |
| Bisexual | 50 | 33.8 | 22 | 21.0 | 72 | 28.5 |
| Unknown | 1 | 0.7 | 0 | 0.0 | 1 | 0.4 |
| Frequency of condom use in the past 6 months (Fisher’s exact test, P < 0.001) | ||||||
| Never | 14 | 9.5 | 1 | 1.0 | 15 | 5.9 |
| Sometimes | 90 | 60.8 | 28 | 26.7 | 118 | 46.6 |
| Every time | 44 | 29.7 | 56 | 53.3 | 100 | 39.5 |
| Unknown | 0 | 0.0 | 20 | 19.1 | 20 | 7.9 |
| Presence of stable male sexual partner (χ2 = 28.57, p < 0.001) | ||||||
| Yes | 47 | 31.8 | 35 | 33.3 | 82 | 32.4 |
| Yes, but not currently | 10 | 6.7 | 32 | 30.5 | 42 | 16.6 |
| No | 91 | 61.5 | 38 | 36.2 | 129 | 51.0 |
| No. of stable sexual partners in the past year (Fisher’s exact test, p < 0.001) | ||||||
| 0 | 2 | 3.5 | 23 | 34.3 | 25 | 20.2 |
| 1 | 32 | 56.1 | 37 | 55.2 | 69 | 55.7 |
| ≥2 | 23 | 40.4 | 7 | 10.5 | 30 | 24.2 |
| Presence of casual sexual partners (non-commercial) | ||||||
| Yes | 115 | 77.7 | 92 | 87.6 | 207 | 81.8 |
| No | 21 | 14.2 | 13 | 12.4 | 34 | 13.4 |
| Unknown | 12 | 8.1 | 0 | 0.0 | 12 | 4.7 |
| No. of casual partners in the past six months (Fisher’s exact test, p = 0.002) | ||||||
| 0 | 1 | 0.9 | 9 | 9.8 | 10 | 4.8 |
| 1–3 | 80 | 69.6 | 65 | 70.7 | 145 | 70.1 |
| 4–9 | 29 | 25.2 | 11 | 12.0 | 40 | 19.3 |
| ≥10 | 5 | 4.4 | 7 | 7.6 | 12 | 5.8 |
| Presence of commercial sexual partners | ||||||
| Yes | 1 | 0.7 | 2 | 1.9 | 3 | 1.2 |
| No | 50 | 33.8 | 82 | 78.1 | 132 | 52.2 |
| Unknown | 97 | 65.5 | 21 | 20.0 | 118 | 46.6 |
| Presence of other heterosexual partners (non-spouse) | ||||||
| Yes | 2 | 1.4 | 6 | 5.7 | 8 | 3.2 |
| No | 113 | 76.4 | 97 | 92.4 | 210 | 83.0 |
| Unknown | 33 | 22.3 | 2 | 1.9 | 35 | 13.8 |
Newly identified HIV-positive ICs included newly HIV infected MSM identified and invited through HIV testing promotion program and PN and testing process.
Previously identified HIV-positive ICs were previously identified HIV infected MSM recruited in the first round of PN and testing process.
Sexual behavioral characteristics
Of the 253 ICs (Table 1), 93 (36.8%) self-reported mainly taking a receptive role during anal sex, 178 (70.4%) self-identified as homosexual, 133 (52.5%) reported inconsistent condom use during anal sex in the past six months, 82 (32.4%) reported currently having a stable homosexual partner, and 207 (81.8%) reported ever having casual sexual partners (non-commercial), while less than 5% reported ever having commercial sexual partners and non-spouse heterosexual partners. Compared with previously identified cases, newly identified cases reported a lower proportion of consistent condom use in the past six months (p < 0.001).
Sexual PN and HIV testing mobilization
Key outcomes of sexual PN and testing process
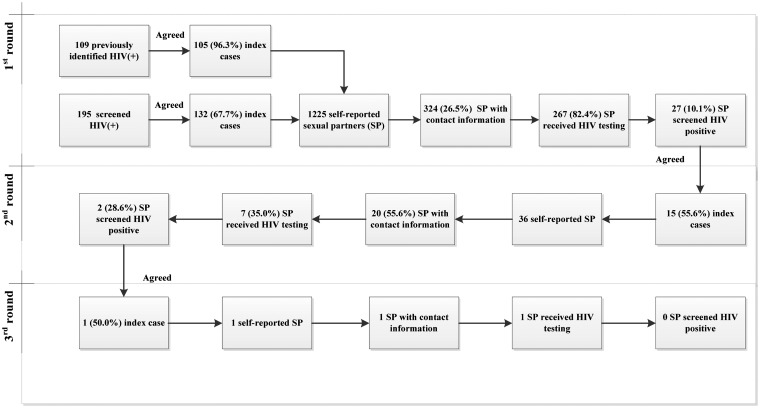
Figure 1 and Table 2 show the key outcomes of sexual PN and HIV testing process. In the first round, 105 of the 109 (96.3%) previously identified HIV infections and 132 of the 195 (67.7%) screened HIV reactive agreed to participate as primary ICs. In total, 1225 sexual partners were reported by primary ICs and 324 (26.5%) of them were reported with contact information in the first round. Among the 324 contactable sexual partners, 267 (82.4%) received HIV testing and 27 (10.1%) screened reactive. In the second round, 15 of the 27 (55.6%) who screened reactive in the first round participated as ICs and reported 36 sexual partners, of whom 20 (55.6%) were reported with contact information. Among the 20 contactable sexual partners, 7 (35.0%) received HIV testing and 2 (28.6%) screened reactive. In the third round, one of the two HIV reactive cases in the second round participated as IC and reported one sexual partner with contact information. This sexual partner received HIV testing and the result was negative. In total, the HIV screened reactive percentage of all reached sexual partners was 10.5% (29/275). Of the 29 screened reactive, 24 (82.8%) were confirmed to be HIV-positive. Of the 24 HIV-positive, 23 were newly diagnosed (one has been confirmed and reported previously).
Figure 1.
Flow chart of sexual PN and testing promotion among HIV positive ICs in Hangzhou and Kunming, China, June 2014 to May 2015.
Table 2.
Sexual PN and testing process among HIV-positive IC in Hangzhou and Kunming, China, June 2014 to May 2015.
| Partner notification and HIV testing process | First round |
Second round |
Third round |
Total |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ICs-newly identified | ICs-previously identified | Total | Primary ICs-newly identified | Primary ICs-previously identified | Total | Primary ICs-newly identified | Primary ICs-previously identified | Total | Primary ICs-newly identified | Primary ICs-previously identified | Total | |
| HIV positives as ICs (n (%)) | 132 (–) | 105 (–) | 237 (–) | 12 (60.0) | 3 (42.7) | 15 (55.6) | 1 (50.0) | – | 1 (50.0) | 145 (–) | 108 (–) | 253 (–) |
| Reported sexual partners (n) | 504 | 721 | 1225 | 26 | 10 | 36 | 1 | – | 1 | 531 | 731 | 1262 |
| Contactable sexual partners (n (%)) | 217 (43.1) a | 107 (14.8) a | 324 (26.5) | 17 (65.4) | 3 (30.0) | 20 (55.6) | 1 (100.0) | – | 1 (100.0) | 235 (44.3) c | 110 (15.1) c | 345 (27.3) |
| Tested sexual partners (n (%)) | 161 (74.2) b | 106 (99.1) b | 267 (82.4) | 7 (41.2) | 0 (0.0) | 7 (35.0) | 1 (100.0) | – | 1 (100.0) | 169 (71.9) d | 106 (96.4) d | 275 (79.7) |
| HIV screened positives among tested sexual partners (n (%)) | 20 (12.4) e | 7 (6.6) e | 27 (10.1) | 2 (28.6) | – | 2 (28.6) | 0 (0.0) | – | 0 (0.0) | 22 (13.0) f | 7 (6.6) f | 29 (10.5) |
χ2 = 121.39, p < 0.001.
χ2 = 30.58, p < 0.001.
χ2 = 132.10, p < 0.001.
χ2 = 27.69, p < 0.001.
χ2 = 1.966, p = 0.161.
χ2 = 2.332, p = 0.127. The significance level: a = 0.05.
Discrepancy between processes initiated by newly and previously identified primary ICs
The whole PN and testing process was divided into two part according to the primary ICs recruited in the first round (newly and previously identified ICs) and key outcomes between them were compared in Table 2. Compared with the process initiated by previously identified primary ICs, the process initiated by newly identified primary ICs found a lower number of sexual partners (1:3.8 vs. 1:6.9 in the first round; 1:3.7 vs. 1:6.8 in the whole process) and a higher proportion of contactable sexual partners (43.1% vs. 14.8% in the first round; 44.3% vs. 15.1% in the whole process; both p < 0.001), but a lower percentage of receiving HIV test among contacted sexual partners (74.2% vs. 99.1% in the first round; 71.9% vs. 96.4% in the whole process; both p < 0.001). In addition, the screened HIV reactive percentage among tested sexual partners in the process initiated by newly identified primary ICs was nearly twice that in the process initiated by previously identified primary ICs, although no statistical significance was detected between them (12.4% vs. 6.6%, p = 0.12 in the first round; 13.0% vs. 6.6%, p = 0.09 in the whole process).
Discrepancy between sexual partner types
Among the total 1262 reported sexual partners (Table 3), 1056 (83.7%) were casual partners (non-commercial) in the past six months, only 401 (31.8%) had contact information. Significant differences were observed in the proportion of sexual partners with contact information between different types of sexual partners (χ2 = 174.00, p < 0.001 for all sexual partners by types; χ2 = 30.49, p < 0.001 for newly identified ICs; χ2 = 173.09, p < 0.001 for previously identified ICs). The HIV testing rate of contacted sexual partners were also significantly different among stable partners, casual partners, and wives of married MSM for both newly identified ICs (Fisher’s exact test, p = 0.001) and previously identified ICs (χ2 = 8.30, p = 0.016). The percentage of screening reactive for sexual partners were different among stable partners (14.8%), casual partners (7.0%), and wives of ICs (7.4%), although not statistically significant (p = 0.188). For casual partners, the contactable rate and testing rate were both higher among newly identified ICs than that among previously identified IC (χ2 = 65.75 and χ2 = 12.84, respectively, both p < 0.001). For wives of ICs, the testing rate among previously identified IC is higher than that of newly identified IC (90.9% vs. 50.0%, p = 0.014).
Table 3.
Comparison of PN and testing by types of sexual partners and HIV-positive (ICs).
| Sexual partner types | ICs-newly identifieda | ICs-previously identifiedb | Total | χ2 | P value | |||
|---|---|---|---|---|---|---|---|---|
| Self-reported sexual partners | ||||||||
| Stable partners in the past year | 88 | 52 | 140 | – | <0.001 c | |||
| Casual partners in the past 6 months | 426 | 630 | 1056 | |||||
| Commercial partners in the past 6 months | 4 | 5 | 9 | |||||
| Wives of married MSM | 22 | 25 | 47 | |||||
| Other heterosexual partners in the past 6 months | 1 | 9 | 10 | |||||
| Total | 541 | 721 | 1262 | |||||
| Sexual partners with contact information (n, % of reported sexual partners) | ||||||||
| Stable partners in the past year | 60 | 68.2 | 42 | 80.8 | 102 | 72.9 | 2.62 | 0.106 |
| Casual partners in the past 6 months | 162 | 38.0 | 101 | 16.0 | 263 | 24.9 | 65.75 | <0.001 |
| Wives of married MSM | 14 | 63.6 | 22 | 88.0 | 36 | 76.6 | 3.87 | 0.049 |
| Total | 236 | 43.6 | 165 | 22.9 | 401 | 31.8 | 113.59 | <0.001 |
| Chi square test | 30.49 | 173.09 | 174.00 | |||||
| P value | <0.001 | <0.001 | <0.001 | |||||
| Sexual partners receiving HIV test (n, % of sexual partners with contact information) | ||||||||
| Stable partners in the past year | 34 | 56.7 | 27 | 64.3 | 61 | 59.8 | 0.60 | 0.44 |
| Casual partners in the past 6 months | 128 | 79.0 | 59 | 58.4 | 187 | 71.1 | 12.84 | <0.001 |
| Wives of married MSM | 7 | 50.0 | 20 | 90.9 | 27 | 75.0 | – | 0.014 c |
| Total | 169 | 71.6 | 106 | 64.2 | 275 | 68.6 | 2.45 | 0.118 |
| Chi square test | – | 8.30 | 5.11 | |||||
| P value | 0.001 c | 0.016 | 0.078 | |||||
Newly identified ICs included newly HIV infected MSM identified and invited through HIV testing promotion program and PN and testing process.
Previously identified ICs were previously identified HIV infected MSM recruited in the first round of PN and testing program.
Fisher’s exact test. The significance level: a = 0.05.
Attitudes toward PN and HIV testing (Table 4)
Table 4.
Attitude toward PN for different sexual partners of HIV-positive MSM.
| Types of sexual partners might be notified |
|||||
|---|---|---|---|---|---|
| Stable partners (n = 124)a | Casual partners (n = 207)a | Commercial sexual partners (n = 3)a | Wives (n = 76)a | Other heterosexual partners (n = 8)a | |
| Would you like to mobilize your sexual partners to take HIV test? (n (%)) | |||||
| Yes | 89 (71.8) | 141 (68.1) | 0 (0.0) | 27 (35.5) | 2 (25.0) |
| No | 15 (12.1) | 41 (19.8) | 3 (100.0) | 8 (10.5) | 5 (62.5) |
| Unknown | 20 (16.1) | 25 (12.1) | – | 41 (53.9) | 1 (12.5) |
| If yes, who would you prefer to mobilize your sexual partners? (single choice, n (%)) | |||||
| Oneself | 71 (79.8) | 107 (75.9) | – | 27 (100.0) | 2 (100.0) |
| CBO workers | 5 (5.6) | 29 (20.6) | – | 0 (0.0) | 0 (0.0) |
| Workers of local CDC | 10 (11.2) | 1 (0.7) | – | 0 (0.0) | 0 (0.0) |
| Unknown | 3 (3.4) | 4 (2.8) | – | – | – |
| If no, reasons for answering no? (multiple choice, n (%)) | |||||
| Fear of disclosing HIV status to partners | 7 (46.7) | 6 (14.6) | – | 7 (87.5) | – |
| Partner is already HIV-positive | 4 (26.7) | 4 (9.8) | – | – | – |
| Fear of discrimination | 3 (20.0) | – | – | – | – |
| Relationship changes due to HIV status | – | 1 (2.4) | – | 4 (50.0) | – |
| Fear of disclosing infidelity to stable partner | – | 1 (2.4) | – | – | – |
| Inability to communicate | 5 (33.3) | 2 (4.9) | – | 3 (37.5) | – |
| No contact information | 10 (66.7) | 31 (75.6) | 3 (100.0) | – | 5 (100.0) |
| Other reasons | 3 (20.0) | 1 (2.4) | – | 7 (87.5)b | – |
n = the number of HIV-positive MSM who expressed their attitude toward a certain type of sexual partners.
HIV infected MSM reported another main reason of refusing to mobilize their wives, which is fear of disclosing homosexual orientation.
Including 253 ICs in the PN and testing process, 309 HIV-positive MSM reported their attitudes toward PN and HIV testing mobilization according to their sexual partner types. The majority of HIV-positive MSM expressed willingness to notify and mobilize their stable or casual partners to undergo HIV testing (71.8% and 68.1%, respectively). Nearly three quarters of HIV-positive MSM reported a desire to mobilize their sexual partners by themselves. Having no contact information was a main reason for study participants to refuse mobilizing sexual partner testing. As for stable partners and wives, another important reason that HIV-positive MSM declined mobilization for HIV testing was fear of disclosing their HIV status to partners.
Discussion
This study endeavored to promote notification and HIV testing for sexual partners of HIV-positive MSM in cooperation with MSM-serving CBOs. Results of this study further provided solid evidence that PN and testing mobilization were helpful to reach more diverse sexual partners to promote early diagnosis of HIV infections. This is consistent with China’s current key strategy of expanding HIV testing and scaling up antiretroviral treatment to prevent and control HIV/AIDS in China. Especially, the study shows us that it is feasible and efficient to conduct PN and testing mobilization for HIV-infected MSM in China, instead of just focusing on HIV sero-discordant couples. Because of perceived challenges to, discrimination against and stigmatization of homosexuality in China, PN and testing for HIV sero-discordant couples usually do not involve the MSM population in China. The HIV-detected positive rate was 10.5% (29/275) for reached sexual partners in our study, which is higher than the HIV prevalence of national surveillance data (7.3%). Although only 21.8% (275/1262) of the reported sexual partners received HIV testing, this also indicates a high potential for HIV case finding. With increased experience and improved PN approaches, we believe PN and testing mobilization will play a more important role in case finding and reducing HIV transmission.
Our study also shows that MSM-serving CBOs can play important roles in PN and testing promotion. Almost all PN and testing mobilization work in this study was conducted by MSM-serving CBOs except that local CDCs provided support for several wives of married MSM notification and HIV testing. Although this is the first time for MSM-serving CBOs in the two cities to be involved in such a study, the proportion of contactable sexual partners is 31.8% and the HIV testing percentage of contactable sexual partners was 68.6% in this study. Although a similar proportion of contactable sexual partners was reported in another study conducted by health professionals in eastern China, but the HIV testing percentage of contactable partners was only 42.7% in that study.18 Other contact tracing studies performed in China also showed lower testing rates of contactable partners.12–14 In addition, different from those studies in which PN were mainly conducted by health professionals targeting sero-discordant married couples,13,14 our study tested a higher proportion of casual sexual partners. This may reflect MSM-serving CBOs’ unique advantage of understanding the MSM community.2–4,22 With further training in PN techniques, MSM-serving CBOs may play an even more important role in HIV testing mobilization among MSM in China.
Studies have shown that knowing HIV infection status is likely to lead to reduced sexual risk behaviors.23 Our study also showed a higher percentage of self-reported consistent condom use for previously identified ICs as compared with the newly identified ICs. However, this cannot change the fact that the HIV transmission risk behavior for previously identified HIV infections remains at a high level. Nearly, 50% of the previously identified ICs reported non-consistent condom use during anal sex. A study conducted in Shanghai and Chengdu, China, also showed a high proportion of HIV-infected MSM engaging in unprotected sexual behavior.24 In addition, our results showed that previously identified ICs reported more casual partners than newly identified ICs. PN among the previously identified ICs also showed a lower observed contact rate and testing rate for reported casual sexual partners, compared with that among newly diagnosed ICs. Several reasons might contribute to this difference. HIV case management services provided by CDCs for previously identified ICs might lead to changes in their risk behaviors. This also might make them less likely to report sexual behaviors or contact partners due to social expectation of reduced risk behaviors. In addition, they might be more likely to lose contact with their partners due to earlier diagnosis. On the other hand, newly tested HIV-positive ICs were identified by CBOs and PN was initiated immediately after post-test counselling. Therefore, collection of sexual partner information and PN immediately after a reactive screening result is helpful to reduce risks of HIV transmission.
This study also investigated the discrepancies of PN among different types of sexual partners and attitudes of PN and HIV testing toward different types of sexual partners. For stable and casual partners, ICs reported more stable partners with contact information than casual partners, but more contacted casual partners received HIV testing than stable partners. It is reasonable to assume that ICs are more likely to remember contact information of stable partners and might care more about them than casual partners. It may also suggested that the potential advantage of CBOs in notifying and mobilizing illicit casual partners for HIV testing. However, further studies are needed to understand concerns and preferences of different sexual partners in PN and HIV testing.
As for attitude, most ICs expressed willingness to mobilize their stable and casual partners for HIV testing but not commercial and other heterosexual partners (non-spouse). Main reasons for not wanting to join partner testing mobilization were fear of disclosure of HIV infection status and lack of contact information. A previous study also showed that the disclosure of HIV status among MSM sexual networks was more difficult for commercial partners compared with stable and casual partners,25 which resulted in more difficulties of commercial PN and HIV testing. Wives’ notification was a challenge for MSM-serving CBOs, for MSM ICs was fear of disclosing homosexual orientation through MSM-serving CBO. In this case, it would be better if health departments worked together with CBOs to do so. Confidentiality and privacy protection are imperative to obtain accurate contact information.
This study as a pilot study only lasted for one year and had some limitations. As the study period was relatively short, training and capacity of PN for CBOs might have been limited and the sample of ICs and associated sexual partners relatively small. However, this study presented a good prospect for PN and HIV testing interventions among MSM through synergistic cooperation with CBOs.
Conclusion
PN and testing mobilization were useful in reaching more diverse sexual partners of HIV-positive MSM, as well as in promoting early diagnosis of HIV infections. It was feasible and efficient to implement the promotion of PN and HIV testing among HIV-infected MSM in cooperation with CBOs. Combining the advantages of CBOs and health departments for different aspects of PN and HIV testing would further improve this.
Acknowledgments
We acknowledge and appreciate the significant contribution of Zhejiang Provincial Center for Disease Control and Prevention and Yunnan Provincial Center for Disease Control and Prevention for data collection and reporting.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the M.A.C AIDS fund.
References
- 1.China Ministry of Health, UNAIDS and WHO. 2011 Estimate of China's ADIS Epidemic. Chin J AIDS STD 2012; 18: 1–5. [Google Scholar]
- 2.Zhang D, Qi J, Fu X, Meng S, et al. Case finding advantage of rapid tests in community settings: men who have sex with men in 12 program areas in China, 2011. Int J STD AIDS 2015; 26: 402–413. [DOI] [PubMed] [Google Scholar]
- 3.Yan H, Zhang M, Zhao J, et al. The increased effectiveness of HIV preventive intervention among men who have sex with men and of follow-up care for people living with HIV after ‘task-shifting' to community-based organizations: a ‘cash on service delivery' model in China. PLoS One 2014; 9: e103146–e103146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yan H, Zhang R, Wei C, et al. A peer-led, community-based rapid HIV testing intervention among untested men who have sex with men in China: an operational model for expansion of HIV testing and linkage to care. Sex Transm Infect 2014; 90: 388–393. [DOI] [PubMed] [Google Scholar]
- 5.Xu J, Han X, Reilly KH, et al. New features of the HIV epidemic among men who have sex with men in China. Emerg Microbes Infect 2013; 2: e45–e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhong F, Lin P, Xu H, et al. Possible increase in HIV and syphilis prevalence among men who have sex with men in Guangzhou, China: results from a respondent-driven sampling survey. AIDS Behav 2011; 15: 1058–1066. [DOI] [PubMed] [Google Scholar]
- 7.Tang HL, Mao YR, Zhang TJ, et al. [Analysis on late diagnosis reasons of newly diagnosed HIV/AIDS patients]. Zhonghua Yu Fang Yi Xue Za Zhi 2012; 46: 1004–1008. [PubMed] [Google Scholar]
- 8.Workowski KA, Berman SM. Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep 2006; 55: 1–94. [PubMed] [Google Scholar]
- 9.(CDC) CfDCaP. Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. MMWR Recomm Rep 2008; 57: 1–83; quiz CE1-4. [PubMed] [Google Scholar]
- 10.van Aar F, Schreuder I, van Weert Y, et al. Current practices of partner notification among MSM with HIV, gonorrhoea and syphilis in the Netherlands: an urgent need for improvement. BMC Infect Dis 2012; 12: 114–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hochberg CH, Berringer K, Schneider JA. Next-generation methods for HIV partner services: A systematic review. Sex Transm Dis 2015; 42: 533–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Y, Chen Q, Liang Y, et al. [A source tracing survey of newly reported HIV/AIDS cases in 2008-2009 in Guangzhou]. Chin J AIDS STD 2011; 2: 131–134. [Google Scholar]
- 13.Ye RH, Xiang LF, Yang YC, et al. [Tracing the sources of newly reported HIV infections in Dehong prefecture of Yunnan province]. Zhonghua Liu Xing Bing Xue Za Zhi 2010; 31: 39–42. [PubMed] [Google Scholar]
- 14.Lin H, He N, Ding Y, et al. Tracing sexual contacts of HIV-infected individuals in a rural prefecture, Eastern China. BMC Public Health 2012; 12: 533–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pu Y, Duan Q, Han W, et al. [Tracing high risk contacts of newly reported HIV-infected cases in Longchuan of Yunnan province]. Chin J AIDS STD 2010; 5: 476–478. [Google Scholar]
- 16.Golden MR, Hogben M, Potterat JJ, et al. HIV partner notification in the United States: a national survey of program coverage and outcomes. Sex Transm Dis 2004; 31: 709–712. [DOI] [PubMed] [Google Scholar]
- 17.Edelman EJ, Gordon KS, Hogben M, et al. Sexual partner notification of HIV infection among a National United States-based sample of HIV-infected men. AIDS Behav 2014; 18: 1898–1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin H, He N, Zhou S, et al. Behavioral and molecular tracing of risky sexual contacts in a sample of Chinese HIV-infected men who have sex with men. Am J Epidemiol 2013; 177: 343–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tomnay JE, Hatch BA, Pitts MK, et al. HIV partner notification: a 2002 Victorian audit. Int J STD AIDS 2004; 15: 629–631. [DOI] [PubMed] [Google Scholar]
- 20.Xu H, Zeng Y, Anderson AF. Chinese NGOs in action against HIV/AIDS. Cell Res 2005; 15: 914–918. [DOI] [PubMed] [Google Scholar]
- 21.Holland CE, Papworth E, Billong SC, et al. Access to HIV services at non-governmental and community-based organizations among men who have sex with men (MSM) in Cameroon: An integrated biological and behavioral surveillance analysis. PLoS One 2015; 10: e0122881–e0122881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tucker JD, Muessig KE, Cui R, et al. Organizational characteristics of HIV/syphilis testing services for men who have sex with men in South China: a social entrepreneurship analysis and implications for creating sustainable service models. BMC Infect Dis 2014; 14: 601–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lai Z, Liu Y, Zhang Y, et al. [Study on the change of unsafe sexual behaviors and its determinants in HIV-positive persons after being notified as HIV seropositive]. Zhonghua Liu Xing Bing Xue Za Zhi 2015; 36: 337–339. [PubMed] [Google Scholar]
- 24.He H, Zhang H, Ding F, et al. [Risky sexual transmission behavior and its influencing factors among HIV-positive MSM population in Shanghai and Chengdu in China]. Zhonghua Liu Xing Bing Xue Za Zhi 2015; 36: 254–258. [PubMed] [Google Scholar]
- 25.Tobin KE, Yang C, Sun C, et al. Discrepancies between HIV prevention communication attitudes and actual conversations about HIV testing within social and sexual networks of African American men who have sex with men. Sex Transm Dis 2014; 41: 221–226. [DOI] [PMC free article] [PubMed] [Google Scholar]