Abstract
Purpose
The proportion of women in urology has increased from <0.5% in 1981 to 10% today. Furthermore, 33% of students matching in urology are now female. This analysis sought to characterize the female workforce in urology in comparison to men with regard to income, workload, and job satisfaction.
Materials and Methods
We collaborated with the American Urologic Association to survey its domestic membership of practicing urologists regarding socioeconomic, workforce, and quality of life issues. 6,511 survey invitations were sent via e-mail. The survey consisted of 26 questions and took approximately 13 minutes to complete. Linear regression models were used to evaluate bivariable and multivariable associations with job satisfaction and compensation.
Results
A total of 848 responses (n=660 (90%) male, n=73 (10%) female) were collected for a total response rate of 13%. On bivariable analysis, female urologists were younger (p<0.0001), more likely to be fellowship trained (p=0.002), worked in academics (p=0.008), were less likely to be self-employed, and worked fewer hours (p=0.03) compared to males. On multivariable analysis, female gender was a significant predictor of lower compensation (p = 0.001) when controlling for work hours, call frequency, age, practice setting and type, fellowship training, and Advance Practice Provider employment. Adjusted salaries among female urologists were $76,321 less than men. Gender was not a predictor for job satisfaction.
Conclusions
Female urologists are significantly less compensated compared to males, after adjusting for several factors likely contributing to compensation. There is no difference in job satisfaction between male and female urologists.
Keywords: urology, gender, job satisfaction, socioeconomic factors, clinical practice patterns
Introduction
In past decades, the barriers preventing women from entering medicine have been substantially reduced, and approximately 50% of students entering U.S. medical schools are now female.1 Coinciding with a rise in the number of female medical students, the number of women entering the field of urology has increased significantly, although urology remains largely male-dominated. Since 1981, the number of female urologists has risen from 34 to 512, representing a relative increase of more than 1000% but an absolute increase of only 5%.2 Despite an increase in the number of female urologic residents, female urologists still comprise <10% of the urology workforce.3
With the growing number of women entering urology, interest in the impact of gender on job satisfaction, work hours, and compensation has become apparent. Traditionally, female physicians have been reimbursed at lower levels than their male counterparts with lower income among female urologists also reported.4 Furthermore, monetary compensation and the level of reported satisfaction appear to be positively correlated, although specific analyses did not directly associate dissatisfied women with less income.5
Given the rapidly changing landscape for women in urology, we sought to further characterize gender differences in income, workload, and job satisfaction by conducting a survey of urologists currently practicing in the United States. The purpose of this study was to examine the current state of the female urologic workforce and potential explanatory factors affecting income and job satisfaction.
Materials and Methods
We collaborated with the AUA to query its domestic membership of practicing urologists regarding socioeconomic, workforce, and quality of life issues. A quantitative survey was designed by the AUA, and a total of 6,511 survey invitations were sent to all members via e-mail. Although we do not know the exact gender distribution of survey invitations, the AUA is currently comprised of 92.3% male and 7.7% female urologists and survey invitations likely paralleled these proportions. The survey consisted of 26 questions and took approximately 13 minutes to complete. A total of 848 responses were collected for a response rate of 13%. Our sample size allowed confidence intervals around percentages to be calculated with high precision- the maximum width of a 95% exact binomial confidence interval is +/-3.4%.
Survey questions included a number of provider-related demographics, including age, gender, and years in practice. Additional practice-based questions included provider compensation, workload, training, practice focus, and practice characteristics. Payor mix was not assessed. Questions related to career differences included practice type and career satisfaction with possible answers described in parentheses: 1) What is your current employment status? (academic, employed, self-employed); 2) How would you rate your current satisfaction with work? (very satisfied, somewhat satisfied, ambivalent, somewhat unsatisfied, very unsatisfied); 3) Would you choose medicine again as a career? (yes, no, unsure). Factors such as prior year's compensation, average weekly hours worked, and average monthly number of call days allowed free text responses. Survey responses were compared between currently practicing female and male urologists.
Exact 95% binomial confidence intervals were reported for percentages as appropriate. Multivariable linear regression models were used to evaluate associations of compensation and job satisfaction with gender, after controlling for covariates of interest, with p-values<0.05 deemed statistically significant. Of note, years in practice and age were collinear and therefore could not be included in the model together. Therefore, each model was fit separately with age or years in practice; and AICs were compared. Given that age provided the lowest AIC, age was included in the analysis in lieu of years in practice. All analyses were conducted using SAS v9.3 statistical software (Cary, NC).
Results
733 providers completed the job satisfaction question and are included in these analyses, of whom 90% were male and 10% female (Table 1). The median respondent age was 49 years with 7% <37 years, 26% between 37-45, 31% between 45-54, 28% between 55-64, and 8% 65 years and older. The majority of respondents worked in urban (47%) or suburban practices (38%), and half were self-employed followed by employed (30%) and academic (21%). Approximately 40% of survey respondents were fellowship-trained, and the majority used an advanced practice provider (APP), defined as an advanced practice nurse or physician assistant, in their practice (62%). Ancillary income was reported by 42% of respondents. Respondents also reported a median of 7 calls per month, $385,000 annual salary ($128 per hour), and 60 hours worked per week.
Table 1. Comparison of Provider Characteristics among Surveyed Male and Female Urologists.
| Respondent Characteristics | All (N=733) | Female (N = 73) | Male (N = 660) | p-value | |
|---|---|---|---|---|---|
| Age | Overall Median (IQR) | 49 (41.0, 57.0) | 42.0 (37.0, 49.0) | 50.0 (42.0, 57.0) | <0.0001 |
| Under 37 years | 49 (7%) | 11 (15.1%) | 38 (5.8%) | <0.0001 | |
| 37-45 years | 192 (26%) | 36 (49.3%) | 156 (23.6%) | ||
| 45-54 years | 224 (31%) | 14 (19.2%) | 210 (31.8%) | ||
| 55-64 years | 205 (28%) | 11 (15.1%) | 194 (29.4%) | ||
| 65 years and older | 61 (8%) | 0 (0%) | 61 (9.2%) | ||
| Location of Practice | Rural | 108 (15%) | 8 (11.0%) | 100 (15.2%) | 0.25 |
| Urban | 346 (47%) | 41 (56.2%) | 305 (46.2%) | ||
| Suburban | 279 (38%) | 24 (32.9%) | 255 (38.6%) | ||
| Fellowship | No | 442 (60%) | 32 (43.8%) | 410 (62.1%) | 0.002 |
| Yes | 291 (40%) | 41 (56.2%) | 250 (37.9%) | ||
| Employment Type | Employed | 217 (30%) | 27 (37.0%) | 190 (28.8%) | 0.008 |
| Self-Employed | 360 (49%) | 24 (32.9%) | 336 (50.9%) | ||
| Academic | 154 (21%) | 21 (28.8%) | 133 (20.2%) | ||
| Use of APP | No | 281 (38%) | 23 (31.5%) | 258 (39.1%) | 0.21 |
| Yes | 452 (62%) | 50 (68.5%) | 402 (60.9%) | ||
| Job Satisfaction Score (1= very dissatisfied, 5= very satisfied) | Median (IQR) | 4.0 (3.0, 5.0) | 4.0 (3.0, 4.0) | 4.0 (3.0, 5.0) | 0.63 |
| 1 | 37 (5%) | 3 (4.1%) | 34 (5.2%) | 0.84 | |
| 2 | 100 (14%) | 13 (17.8%) | 87 (13.2%) | ||
| 3 | 81 (11%) | 7 (9.6%) | 74 (11.2%) | ||
| 4 | 320 (44%) | 32 (43.8%) | 288 (43.6%) | ||
| 5 | 195 (27%) | 18 (24.7%) | 177 (26.8%) | ||
| Years in practice | Median (IQR) | 17.0 (9.0, 25.0) | 10.0 (5.0, 17.0) | 18.0 (10.0, 2.0) | <0.0001 |
| Calls per month | Median (IQR) | 7 (5.0, 10.0) | 6.0 (4.0, 8.0) | 7.0 (5.0, 10.0) | 0.09 |
| Last year salary (n=693) | Median (IQR) | $385,000 ($300,000, $480,000) | $318,422 ($250,000, $400,000) | $400,000 ($300,000, $500,000) | <0.0001 |
| Salary per hour | Median (IQR) | $128.21 (96.15,173.08) | $106.30 (83.01, 160.26) | $131.12 (100.27, 174.83) | 0.004 |
| Ancillary income | No | 428 (58%) | 51 (70%) | 377 (57%) | 0.04 |
| Yes | 305 (42%) | 22 (30%) | 283 (43%) | ||
| Hours per week | Median (IQR) | 60 (50, 60) | 55.0 (45.0, 60.0) | 60.0 (50.0, 62.0) | 0.03 |
Female respondents were significantly younger than their male counterparts with a median age of 42.0 versus 50.0 years old (p<0.0001) (Table 1). Additionally, women reported less years in practice compared to men (p<0.0001). Approximately two-thirds of female providers practiced in an employed or self-employed practice with the remaining 28.8% in an academic setting. Females were more likely to be employed in a practice or academic setting compared to their male counterparts (p = 0.008). Correspondingly, male respondents were significantly more likely to be self-employed (50.9% vs. 32.9%).
The majority of female respondents reported practicing in an urban location with a larger proportion compared to male respondents (56.2% vs. 46.2%). However, the differences in practice location were not statistically significant (p=0.25). With regard to gender differences between fellowship training, female providers were significantly more likely to have had completed fellowship training (56.2% vs. 37.9%, p=0.002). There were no significant differences in the use of APPs by gender (p=0.21).
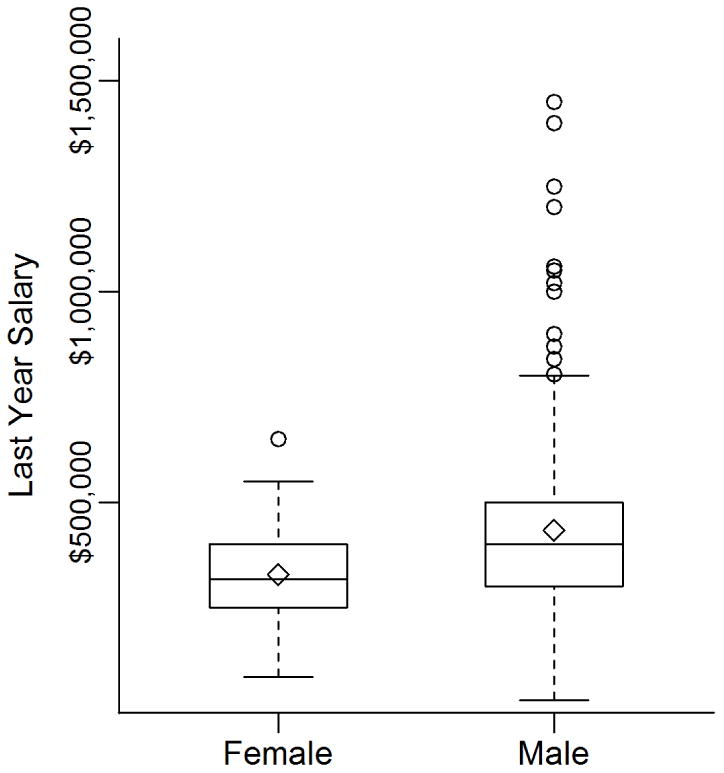
Female providers worked fewer median hours per week compared to men (55.0 vs. 60.0 hours; p = 0.03). Additionally, female urologists reported working 6.0 call days per month compared to 7.0 for males (p=0.09). Only 36% of survey respondents reported work relative value units (WVRUs), but among those who did, women reported a median of 6000 annual WRVUs compared to 8,450 reported by men (p=0.0006), but mean WRVUS were higher among women (11,272 vs. 9,083 WRVUs). Given the large number of missing values, WRVU was not included in the multivariable analysis. The median salary among female urologists was $81,578 less than their male counterparts (p < 0.0001) (Figure 1). This corresponded to a lower median hourly salary of $106.30 for women compared to $131.12 earned by male urologists (p = 0.004). Female urologists were less likely to report ancillary income compared to males (30.1% vs. 42.9%, p = 0.04) (Table 1).
Figure 1. Boxplot of Last Year Salary by Gender.
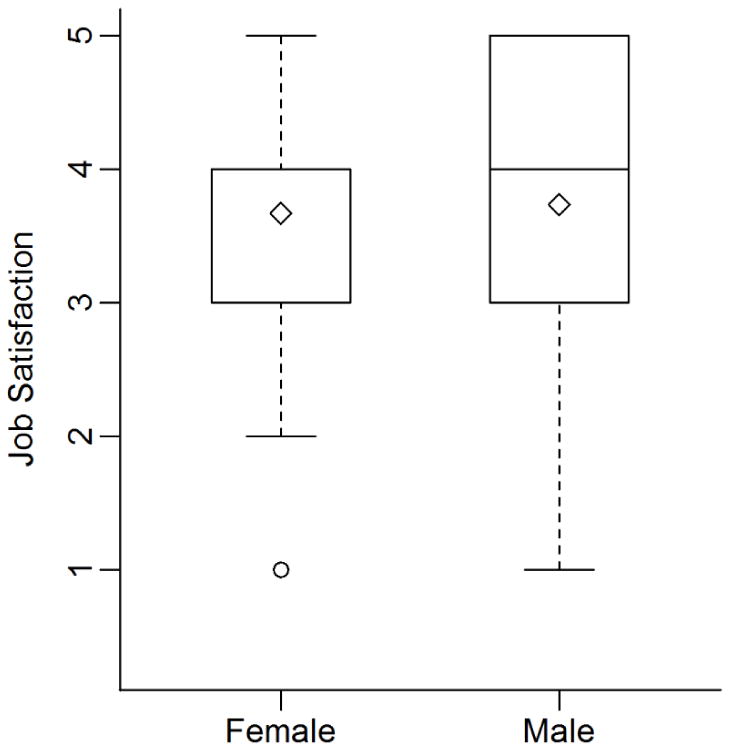
With regard to satisfaction scores, 70% (95%CI: 66.9,73.6%) of providers reported being “satisfied” (defined as either “very satisfied” or “somewhat satisfied”), 63% (95%CI: 59.8, 66.8%) reported that they would choose medicine again, and 83% (95%CI: 80.0, 85.7%) would choose urology again. Although there was no apparent difference in job satisfaction based on gender (Figure 2), female respondents reported a lower rate of choosing medicine again (53% vs. 64%, p=0.07) and choosing urology again (75% vs. 84%, p=0.07).
Figure 2. Boxplot of Job Satisfaction by Gender.
On multivariable analysis, gender remained a significant predictor of lower compensation (p=0.001) after controlling for age, practice setting and type, fellowship training, call frequency, work hours, employment of APPs, and ancillary income (Table 2). Both use of APPs and ancillary income were independent predictors of higher compensation, and on average, annual salary was about $30,000 higher for respondents reporting these characteristics. Those in academic practices reported significantly lower income than their counterparts (-$44,959, p=0.03), as did urologists who were <37 years (-$54,742, p=0.04).
Table 2. Multivariable Analysis assessing Predictors of Annual Compensation and Job Satisfaction.
| Annual Compensation (N=693) | Job Satisfaction (1-5) (n=733) | ||||
|---|---|---|---|---|---|
| Variable | Estimate | p-value | Estimate | p-value | |
| Gender (Ref = Male) | Female | -76,321 | 0.001 | -0.212 | 0.14 |
| Age (Ref = 37-45) | <37 | -54,742 | 0.04 | 0.263 | 0.14 |
| 46-54 | 6,142 | 0.72 | -0.280 | 0.01 | |
| 55-64 | 9,497 | 0.59 | -0.167 | 0.14 | |
| 65 and over | -32,031 | 0.24 | 0.163 | 0.34 | |
| Location of Practice (Ref = Urban) |
Rural | 8,765 | 0.66 | -0.004 | 0.97 |
| Suburban | -13,958 | 0.34 | 0.042 | 0.66 | |
| Fellowship Training (Ref = Not Fellowship Trained) |
Fellowship Trained | 19,269 | 0.21 | 0.149 | 0.13 |
| Type of Practice (Ref = Self-Employed) |
Academic | -44,959 | 0.03 | 0.214 | 0.12 |
| Employed | -8,287 | 0.61 | 0.028 | 0.79 | |
| Work Hours per Week | Hours per Week | 920 | 0.09 | -0.006 | 0.08 |
| Call Days per Month | Call Days per Month | -1,248 | 0.21 | -0.009 | 0.18 |
| Employment of APPs (Ref = No Use of APPs) |
Use of APPs | 31,210 | 0.03 | 0.134 | 0.14 |
| Ancillary (ref=No) |
Yes | 29,717 | 0.04 | -0.036 | 0.70 |
Finally, female compensation was grouped more closely when compared to wider dispersion of male income. Only a single female urologist reported earning enough to place her above the 1.5IQR of the upper quartile of female earners. However, this individual still fell below $750,000 for annual compensation (Figure 1). Comparatively, there were many male outliers, all of whose annual incomes were above $750,000, placing them at two to three times the median male income. The highest male earner's reported salary was $1,500,000 compared to $650,000 for females. Lastly, gender was not a predictor for job satisfaction in multivariable analysis (p = 0.14)(Table 2).
Discussion
Income disparities between men and women within the medical field are well-established and have been reported within the specialty of urology, despite a recent increase in the prevalence of female urologists. However, no previous studies, to our knowledge, have attempted to delineate the causes of gender inequality by concurrently examining important training and practice characteristics known to impact compensation. In our study, we found that women made approximately $76,000 less than men after adjusting for other known predictors of compensation level. Moreover, gender was one of the strongest predictors of compensation in our multivariable model, suggesting that variations in practice setting and training do not explain the documented income inequalities between men and women within urology. In contrast, we did not find any significant gender differences in job satisfaction. Despite these known inequalities in compensation, there are still an increasing number of females entering the field of urology.
In 1995, the female-to-male physician ratio was 1:4 while the ratio in urology was 1:84.6,7 Women comprised only 4.2% of urology residents and 1.2% of board-certified urologists.6,7 This has slowly increased over time to the present where women make up approximately 10% of the practicing urology workforce (consistent with the 10% female respondents of our survey). The percentage of women who successfully matched into urology residency parallels this trend as demonstrated by match rates of 19% in 2004 increasing to 26% as of the 2014-2015 AUA match.8,9 While these numbers portray a relative narrowing of the gender gap, women remain underrepresented and inequalities persist in regard to compensation.
Inequalities in compensation between male and female medical providers have been well-documented.4,6,10 In 1993, the average income claimed by practicing female urologists was 65% that of the national average reported by all urologists.6 This income gender gap was comparable to the national female physician income gap of 62% of that reported by male physicians during the same time period.6,11 In 2002, according to a MGMA income survey, the mean compensation for a full-time female urologist was reported to be 66% that of their male counterparts.4 In the present study we found that female urologists reported median annual income of $318,422 compared to $400,000 for men indicating, that females earn 80% of the income reported by males.
Importantly, the discrepancy between male and female compensation was comparable even after adjusting for other important predictors of income suggesting that, although variations in training and clinical practice are important, women continued to earn 81% that of their male counterparts after accounting for these predictors. Nevertheless, our results may indicate that the gender gap is closing. Lightner and colleagues reported a 33% difference in compensation between men and women, relative to a 19% difference in the present analyses.4 This is supported by similar trends in compensation in all fields of medicine with regard to gender.12,13 It is possible that increased awareness and appreciation of gender-based compensation disparities and the increasing presence of women within the physician workforce may account for the narrowing of this gap.
While gender-related compensation inequity is undeniable, the underlying causes are less clear. It has been proposed that some of the income inequity between genders may be due to female urologists preferentially pursuing part-time work and academically based careers,6 working less hours and taking less call,4,14 or being “pigeonholed” through preferential referral of time-consuming, low-revenue, non-operative cases.4 However, available evidence regarding these potential causes of inequality has been mixed, with several studies reporting that female surgeons actually worked longer hours relative to males4,15 and may have a tendency to underreport their work time, whereas men may tend to over-report hours worked.16-18 Our findings were likely influenced by a greater proportion of women seeking academic appointments in the present sample, which are typically associated with lower compensation, but often allow for more flexibility of schedule, less call requirements, and more emphasis on research.2,19 Academic appointments frequently offer retirement contributions which may not be included in private practice compensation, narrowing the gender compensation gap further.
Beyond work-related differences such as hours and case load, gender differences in compensation could also be impacted by differences in negotiation techniques. A study that evaluated starting salaries of graduate students noted 57% of men and 7% of women tried to negotiate for a higher offer.18 Women who attempt negotiation often violate a “perceived gender norm,” and pay a long-term cost in future advancement and general “likeability.”18 Whether negotiation differences exist in urology warrants further study, but could explain compensation differences that begin in early practice and persist over time.
With regard to income dispersion, female compensation was grouped more closely when compared to male income. The income of very few women fell outside the standard deviation for female compensation. Conversely, there were many male outliers whose annual income placed them at least two to three times the median male salary. We found that 4% of men earned greater than $750,000 annually, whereas no women surveyed earned this much. The highest male earner's reported salary was $1,500,000 compared to $650,000 for women. Similar to many instances within corporate America, a glass ceiling may exist for women urologists.20,21 Another contributor to male outliers in compensation included ancillary income, which was reportedly higher among male urologists compared to females. Further research is needed to delineate these differences. Nevertheless, controlling for ancillary income in multivariable analysis did not impact the association of gender with compensation.
Although income is an important measure of success, it must be viewed in the context of overall job satisfaction. Studies have demonstrated that these concepts are closely related but not interchangeable.5 Female urologists who worked more hours achieved greater financial compensation, and those who are well-compensated report a higher level of career satisfaction.5 However, dissatisfied women did not necessarily earn less.5,22 Women in urology consistently demonstrate high levels of job satisfaction despite two-thirds reporting gender discrimination and half having been discouraged from pursuing urology.6 Female urologic surgeons also have fewer children, higher induction rates and incidence of pregnancy complications.23,24 Despite these findings, a recent survey of female urologists reported that 87% were happy with their choice of urology,5 and 94% would encourage other women to apply.6
The results of the present analyses must be viewed with several limitations in mind. Although we were able to account for many known predictors of compensation, data on work productivity, payor mix, and the types of case loads were unavailable. In addition, we note that any study utilizing self-reported survey data has inherent limitations associated with selection and reporting biases. However, we note that our response rate was higher than many comparable surveys, and the rate of male and female respondents mirrored that of current practitioners. With the advent of the AUA annual census, further investigation into gender-specific differences in the urologic workforce will be important to monitor as we aim to narrow the gender gap in urology.
Conclusions
This study highlights several important aspects of gender inequality in the urology workforce. While the growth of female urologists is both exciting and encouraging, further research efforts are needed to quantify and characterize the factors associated with compensation disparities and understand their root causes. Discussion at regional and national levels will ensure that gender-related disparities are addressed by our governing bodies as we plan for the future of our specialty.
Acknowledgments
Details of all funding sources for work in question: The project described was supported by the University Cancer Research Fund and the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2TR001109.
References
- 1.Association of American Medical Colleges. Applicants and matriculants data: Total U.S. medical school enrollment by race/ethnicity and sex, 2013-2014 and 2014-2015. [Accessed: May 2015];Association of American Medical Colleges. https://www.aamc.org/download/321534/data/factstable28.pdf. Updated: December 2014.
- 2.Pruthi RS, Nielsen ME. Age, gender, and the urology work force: Evolving trends. [Accessed: May 2015];Urology Times. http://urologytimes.modernmedicine.com/urology-times/content/tags/career/age-gender-and-urology-work-force-evolving-trends?page=full. Updated: June 2013.
- 3.Grimsby GM, Wolter CE. The journey of women in urology: The perspective of a female urology resident. J Urol. 2013;81(1):3–6. doi: 10.1016/j.urology.2012.07.050. [DOI] [PubMed] [Google Scholar]
- 4.Lightner DJ, Terris MK, Tsao AK, et al. Status of women in urology: Based on a report to the society of university urologists. J Urol. 2005;173(2):560–563. doi: 10.1097/01.ju.0000149739.51103.d3. [DOI] [PubMed] [Google Scholar]
- 5.Marley CS, Lerner LB, Panagopoulos G, et al. Personal, professional and financial satisfaction among American women urologists. International Braz J Urol. 2011;37(2):187–194. doi: 10.1590/s1677-55382011000200005. [DOI] [PubMed] [Google Scholar]
- 6.Bradbury CL, King DK, Middleton RG. Female urologists: A growing population. J Urol. 1997;157(5):1854–1856. doi: 10.1016/s0022-5347(01)64884-5. [DOI] [PubMed] [Google Scholar]
- 7.Roback G, Randolph L, Seidman B. Physician characteristics and distribution in the US, 1990. Amer Medical Assn. 1990 [Google Scholar]
- 8.Kim SJ, Hyun G. MP15-04 Women in urology: Time to lean in. J Urol April. 2014;191(4):e145. [Google Scholar]
- 9.American Urological Association. Results of 2015 Urology Residency Match. [Accessed: May 2015];2015 Updated: January 2015. [Google Scholar]
- 10.Ash AS, Carr PL, Goldstein R, et al. Compensation and advancement of women in academic medicine: Is there equity? Ann Intern Med. 2004;141(3):205–212. doi: 10.7326/0003-4819-141-3-200408030-00009. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez M. Physician marketplace statistics, 1994. Amer Medical Assn. 1994 [Google Scholar]
- 12.Peckham C. Medscape physician compensation report 2015. [Accessed: May 2015]; Updated: April 21, 2015. [Google Scholar]
- 13.Kane L, Peckham C. Medscape physician compensation report 2014. [Accessed: May 2015]; Updated: April 15, 2014. [Google Scholar]
- 14.Carr PL, Gareis KC, Barnett RC. Characteristics and outcomes for women physicians who work reduced hours. J Womens Health. 2003;12(4):399–405. doi: 10.1089/154099903765448916. [DOI] [PubMed] [Google Scholar]
- 15.Frank E, Brownstein M, Ephgrave K, et al. Characteristics of women surgeons in the united states. Am J Surg. 1998;176(3):244–250. doi: 10.1016/s0002-9610(98)00152-4. [DOI] [PubMed] [Google Scholar]
- 16.Akers MD, Eaton TV. Underreporting of chargeable time: The impact of gender and characteristics of underreporters. J Manage Issues. 2003:82–96. [Google Scholar]
- 17.Krugman S. Women in accounting: Tearing down barriers. Accounting Today. 2000 Sep-Aug;1:56. [Google Scholar]
- 18.Sandberg S. Lean in. Random House; 2014. [Google Scholar]
- 19.Friedberg MW, Chen PG, Van Busum KR, et al. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. [Accessed: January 2015]; http://www.rand.org/content/dam/rand/pubs/research_reports/RR400/RR439/RAND_RR439.pdf. Updated: 2013. [PMC free article] [PubMed]
- 20.Johns ML. Breaking the glass ceiling: Structural, cultural, and organizational barriers preventing women from achieving senior and executive positions. Perspect Health Inf Manag. 2013;10:1e. [PMC free article] [PubMed] [Google Scholar]
- 21.Achkar E. Will women ever break the glass ceiling in medicine? Am J Gastroenterol. 2008;103(7):1587–1588. doi: 10.1111/j.1572-0241.2008.01988.x. [DOI] [PubMed] [Google Scholar]
- 22.Pruthi NR, Deal A, Langston J, et al. Factors related to job satisfaction in urology. Unpublished data. 2015 doi: 10.1016/j.urpr.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 23.Lerner LB, Baltrushes RJ, Stolzmann KL, et al. Satisfaction of women urologists with maternity leave and childbirth timing. J Urol. 2010;183(1):282–286. doi: 10.1016/j.juro.2009.08.113. [DOI] [PubMed] [Google Scholar]
- 24.Lerner LB, Stolzmann KL, Gulla VD. Birth trends and pregnancy complications among women urologists. J Am Coll Surg. 2009;208(2):293–297. doi: 10.1016/j.jamcollsurg.2008.10.012. [DOI] [PubMed] [Google Scholar]


