Stiff-person syndrome (SPS) is a neuroimmunologic disorder characterized by painful spasms and muscle rigidity attributed to impaired inhibitory γ-aminobutyric acid (GABA) descending pathways.1 The immunopathogenesis remains unknown and the pathogenic significance of antibodies against glutamic acid decarboxylase (GAD) is controversial. Herein, we report 4 cases of anti-GAD65-positive patients with SPS (table e-1 at Neurology.org/nn) who had significant worsening of symptoms and disability with the serotonin-norepinephrine reuptake inhibitor (SNRI) duloxetine (table e-2). While causation cannot be proven, these observations suggest the importance of investigating the relationship between SNRI use and SPS clinical exacerbations (figure, A).
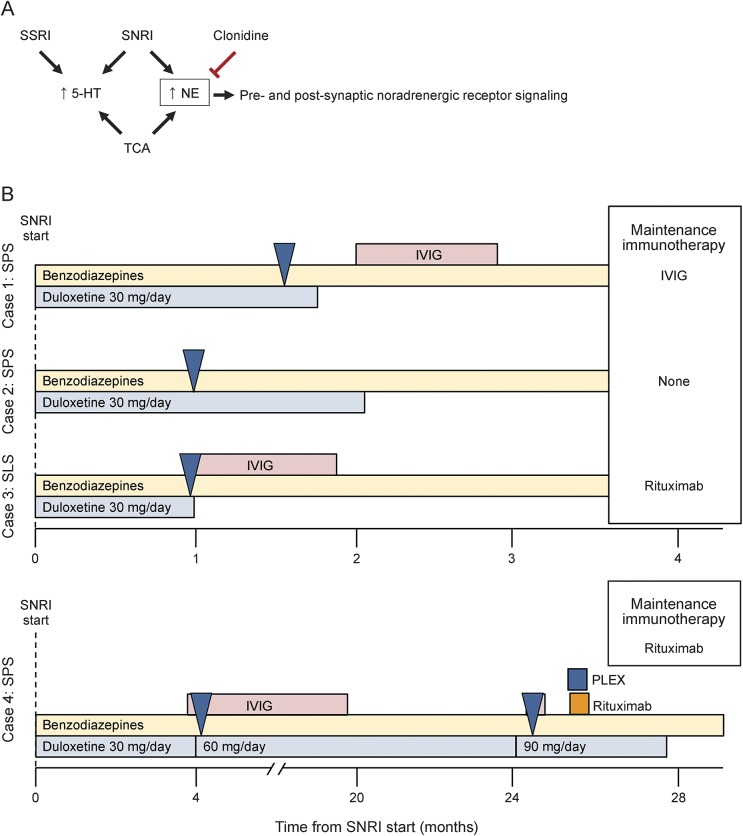
Figure. Model supporting noradrenergic signaling in stiff-person syndrome (SPS) pathophysiology and clinical exacerbations.
(A) Proposed model of serotonin and norepinephrine in SPS. (B) Clinical course of serotonin-norepinephrine reuptake inhibitor (SNRI) use in patients. Clinical exacerbations noted with blue arrow. 5-HT = 5-hydroxytryptamine; IVIg = IV immunoglobulin; NE = norepinephrine; PLEX = plasmapheresis; SLS = stiff-limb syndrome; SSRI = selective serotonin reuptake inhibitor; TCA = tricyclic antidepressant.
Case reports.
Case 1.
A 51-year-old woman with remote stroke developed gradual onset ataxia and frequent falls and required a cane to ambulate within 4 months of symptom onset (figure, B). Her symptoms failed to improve despite therapy with benzodiazepines, gabapentin, and tizanidine. She was prescribed duloxetine 30 mg daily for pain. Over the next 4 weeks, she developed worsening spasms and gait dysfunction, and required a walker to ambulate. Five months after symptom onset, elevated anti-GAD65 antibodies were detected in serum (11,350 U/mL). EMG was consistent with the diagnosis of SPS. Duloxetine was discontinued and she was treated with IV immunoglobulin (IVIg), benzodiazepines, and tizanidine, with marked improvement in symptoms. She remains stable on IVIg at 14 months.
Case 2.
A 38-year-old woman with anti-GAD65-positive SPS, stable for 35 months with remote IVIg use, developed worsening hip pain and was prescribed duloxetine 30 mg daily (figure, B). Within 2 weeks, she had significant worsening in musculoskeletal symptoms and complained of mental fogging. She was treated with benzodiazepines and duloxetine was discontinued. She gradually improved to her baseline over the course of 4 weeks and remains stable at 9 months.
Case 3.
A 49-year-old woman with anxiety disorder and anti-GAD65-positive stiff-limb syndrome required intrathecal baclofen pump for symptom management (figure, B). After IVIg therapy and a period of relative clinical stability, she developed worsening anxiety and was prescribed duloxetine 30 mg daily. Within 1 week of starting duloxetine, she developed painful spasms in her torso and legs, dysphagia, and respiratory distress. She was hospitalized and intubated for airway protection. Her examination was most notable for downbeating nystagmus and severe torso and leg rigidity. Duloxetine was discontinued, and she was treated with IVIg and clinically improved; however, she developed several medical complications and has had a fluctuating clinical course.
Case 4.
A 30-year-old man with diabetes, hypothyroidism, depression, and anti-GAD65-positive SPS developed worsening mood and pain (figure, B). Within 8 months of symptoms onset, he was treated with steroids and prescribed duloxetine 30 mg daily. He experienced severe painful spasms that were refractory to IVIg treatment over 18 months. Duloxetine was gradually titrated to 90 mg daily and within 1 month of this increase, he developed continuous severe painful torso spasms requiring hospitalization. He underwent plasmapheresis for acute SPS exacerbation with modest improvement. After discharge from the hospital, he discontinued duloxetine and noted a remarkable improvement of musculoskeletal symptoms. His pain reliever and benzodiazepine use also decreased. He was treated with rituximab for maintenance immunotherapy and remains neurologically stable.
Discussion.
These 4 cases support a role for noradrenergic circuits in the clinical exacerbation of SPS (figure, A). Previous studies found that rapidly injected clomipramine severely aggravated clinical symptoms in a patient with SPS.2 Clonidine, which is an α2 adrenergic receptor agonist, was shown to improve SPS symptoms.2,3 Taken together, these results may point to a critical function of noradrenergic signaling in the pathophysiology of SPS.3 These findings may also account for the observation that stress and anxiety often precipitate SPS attacks.
Many patients with SPS have comorbid neuropsychiatric disorders, including anxiety and depression.1 The clinical observations presented here suggest caution should be taken when considering use of SNRIs in the management of comorbid neuropsychiatric disorders or musculoskeletal discomfort in patients with SPS. As we cannot exclude chance association, further study is required to identify the causal relationship between SNRI use and SPS clinical exacerbations. These cases suggest the importance of investigating the relationship between SNRIs and SPS in a prospective case-control study. Early recognition and a careful review of medication use may help prevent disease exacerbations in SPS.
Notably, serum autoantibody testing was otherwise negative in all patients. Anti-GAD antibodies are associated with reduced GABA levels4,5 and appear to be associated with clinical symptoms of SPS when passively transferred into animal models.6 However, the pathogenicity of anti-GAD antibodies remains controversial. Autoantibodies to multiple antigens have been described in patients with SPS spectrum disorders.7 Further investigation is required into the role of antibodies to various other antigens in SPS spectrum disorders.
Supplementary Material
Footnotes
Supplemental data at Neurology.org/nn
Author contributions: Study concept and design: Drs. Benavides and Newsome. Acquisition of data: Drs. Benavides and Newsome. Analysis and interpretation of data: Drs. Benavides and Newsome. Drafting of the manuscript: Drs. Benavides and Newsome. Critical revision of the manuscript for important intellectual content: Drs. Benavides and Newsome. Study supervision: Dr. Newsome.
Study funding: No targeted funding.
Disclosure: D.R. Benavides received research support from Mallinckrodt Pharmaceuticals and NIH/NINDS. S.D. Newsome served on the scientific advisory board for Biogen Idec, Genzyme, and Novartis; and received research support from Biogen Idec and Novartis (paid directly to his institution) and National Multiple Sclerosis Society. Go to Neurology.org/nn for full disclosure forms. The Article Processing Charge was paid by the authors.
References
- 1.Murinson BB. Stiff-person syndrome. Neurologist 2004;10:131–137. [DOI] [PubMed] [Google Scholar]
- 2.Meinck HM, Ricker K, Conrad B. The stiff-man syndrome: new pathophysiological aspects from abnormal exteroceptive reflexes and the response to clomipramine, clonidine, and tizanidine. J Neurol Neurosurg Psychiatry 1984;47:280–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meinck HM, Conrad B. Neuropharmacological investigations in the stiff-man syndrome. J Neurol 1986;233:340–347. [DOI] [PubMed] [Google Scholar]
- 4.Dinkel K, Meinck HM, Jury KM, Karges W, Richter W. Inhibition of gamma-aminobutyric acid synthesis by glutamic acid decarboxylase autoantibodies in stiff-man syndrome. Ann Neurol 1998;44:194–201. [DOI] [PubMed] [Google Scholar]
- 5.Dalakas MC, Li M, Fujii M, Jacobowitz DM. Stiff person syndrome: quantification, specificity, and intrathecal synthesis of GAD65 antibodies. Neurology 2001;57:780–784. [DOI] [PubMed] [Google Scholar]
- 6.Hansen N, Grünewald B, Weishaupt A, et al. . Human stiff person syndrome IgG-containing high-titer anti-GAD65 autoantibodies induce motor dysfunction in rats. Exp Neurol 2013;239:202–209. [DOI] [PubMed] [Google Scholar]
- 7.Martinez-Hernandez E, Ariño H, McKeon A, et al. . Clinical and immunologic investigations in patients with stiff-person spectrum disorder. JAMA Neurol 2016;73:714–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.