Abstract
Aims:
To investigate clinically and radiographically, the bone fill in extraction sockets using demineralized freeze-dried bone allograft alone and along with platelet-rich fibrin (PRF).
Materials and Methods:
A randomized controlled clinical trial was carried out on 36 nonrestorable single-rooted teeth sites. Sites were randomized into demineralized freeze-dried bone allograft (DFDBA) combined with PRF - test and DFDBA - control groups using a coin toss method. After the placement of graft material, collagen membrane was used to cover it. The clinical parameters recorded were ridge width and ridge height. All the parameters were recorded at baseline and at 90 and 180 days.
Statistical Analysis Used:
Independent t-test and paired t-test.
Results:
In both groups, there is significant reduction in loss of ridge width and ridge height from baseline to 90 days (P < 0.001), baseline to 180 days (P < 0.001), and 90–180 days (P < 0.001). However, when both the groups were compared the test group favored in the reduction of ridge width while there was no statistical difference in reduction of ridge height among at different intervals.
Conclusions:
Although DFDBA is considered as an ideal graft material, PRF can be used as an adjunctive with DFDBA for socket preservation.
Key words: Atraumatic extraction, collagen, demineralized freeze-dried bone allograft, platelet-rich fibrin, socket preservation
Introduction
Socket preservation is a procedure to preserve hard and soft tissue of the alveolar ridge after extraction. The alveolar process is a tooth-dependent structure, so after the extraction bone loss occurs very rapidly in the initial 6 months, results into the reduction of 40% of alveolar height, and 60% of alveolar width. Various evidence has proved that the bone loss occurs after extraction and more at the labial side of the alveolar process compared to the lingual or the palatal side.[1]
A clinical study on 46 patients evaluated bone healing and soft tissue contour changes after tooth removal. They found an approximate 50% reduction in the buccolingual width of edentulous sites after 12 months. Therefore, it was concluded that it is a mandatory to preserve the dimensions of the tooth socket after extraction, especially if an osseointegrated implant is planned. There are many studies that showed beneficial effects of using different grafts, membrane, and various growth factors to preserve the sockets compared to sockets which are left untreated.[2] Therefore, the aim was to investigate the bone fill in extraction sockets using demineralized freeze-dried bone allograft alone and along with platelet-rich fibrin (PRF), clinically and radiographically.
Materials and Methods
A randomized controlled, clinical, radiographic study was planned after due Ethical Approval from Institutional Ethics Committee of Sumandeep Vidyapeeth was obtained. Patients who came to the Department of Periodontology from January 2014 to January 2015, for the treatment of a single-rooted, nonrestorable, or hopeless tooth having adjacent teeth were included in this study. Written informed consent was obtained from the participants.
Patients between the age group of 20 and 55 years, requiring extraction of at least one maxillary or mandibular nonrestorable single-rooted tooth were included in the study. Patients with <50% bone loss, uncontrolled systemic disease, severe parafunctional habits, poor maintenance of oral hygiene, pregnancy, smokers, or taking any medications that could compromise healing were excluded from the study. A total of 36 single-rooted teeth in maxillary and mandibular arches, indicated for extraction were included in the study. Scaling and root planning were performed before the procedure, and oral hygiene instruction was given. Any periodontal treatment necessary to provide an oral environment more favorable to wound healing was done. Surgical acrylic resin stents were fabricated using dental casts of all the patients.
Pearson Chi-square test was done to evaluate demographic data. In control group, females were 38.9% and 61.1% male participants and in test group, females were 44.4% and 55.6% male participants. No significant statistical difference was found among the groups that justified, both groups were similar (P = 0.73).
Surgical procedure
Before surgery, alveolar ridge width was calculated with the help of Vernier caliper and calibrated radiographs were made with the help of grid. After anesthetizing the surgical area, it was ensured that minimum trauma was caused while extracting the teeth as shown in Figure 1a and b (test site) and Figure 2a and b (control site). Periotomes and forceps were used with great care taken to maintain the buccal bone and the surrounding soft and hard tissues. Following atraumatic extraction, the height of the buccal and lingual bone plate was clinically examined at the mid buccal and mid lingual region with help of a periodontal probe as well as the height of the socket was measured till the base which helped to measure the amount of vertical bone loss on buccal plate as compared to the lingual plate.
Figure 1.
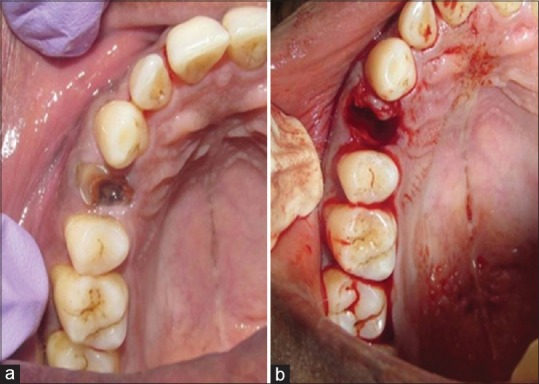
(a) Preoperative test site. (b) Extraction socket test group
Figure 2.
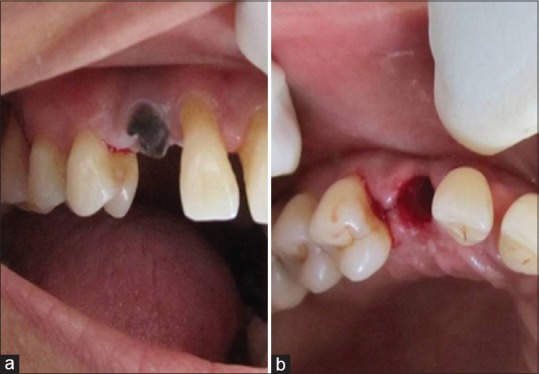
(a) Preoperative control site. (b) Immediate extraction socket control site
Following extraction, granulation tissues were removed with the help of curettes, and the socket was irrigated with sterile normal saline. Computer-generated randomization was used to randomly divide the sockets into two groups.
In test group - demineralized freeze-dried bone allograft (DFDBA) mixed with PRF was condensed into the extraction sockets until the crestal level, and a collagen membrane was used to cover the graft material and in control group - DFDBA was condensed into the extraction socket until the crestal level and similarly, collagen membrane was used to cover the wound.
PRF was prepared by collecting patient's blood from the median cubital vein using a 10 ml syringe and centrifuged at 3000 rpm for 10 min. Blood centrifugation leads to the formation of a fibrin clot that immediately transferred into the socket.
In both groups, the flaps were sutured with criss-cross horizontal mattress technique, to cover as much as possible of the biomaterials. The postoperative instruction was given, and participants were recalled at an interval of 90 and 180 days and calibrated radiographs as shown in Figure 3a–c (In test group) and Figure 4a–c (In control group) with the help of grid, and clinical measurements were recorded.
Figure 3.

(a) Immediate X-ray test site. (b) Test site X-ray -90 days. (c) Test site X-ray -180 days
Figure 4.
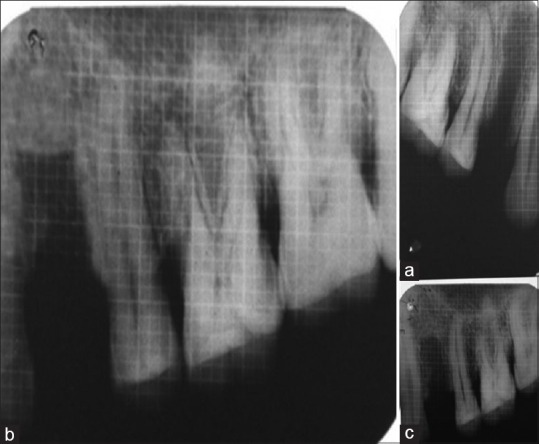
(a) Immediate X-ray control site. (b) Control site X-ray -90 days. (c) Control site X-ray -180 days
Results
A total of 36 sites were treated, and independent t-test was performed to compare the parameters between the two groups and paired t-test was performed to compare the parameter within the same group. The independent t-test was performed to compare ridge width and ridge height at baseline, 90, and 180 days.
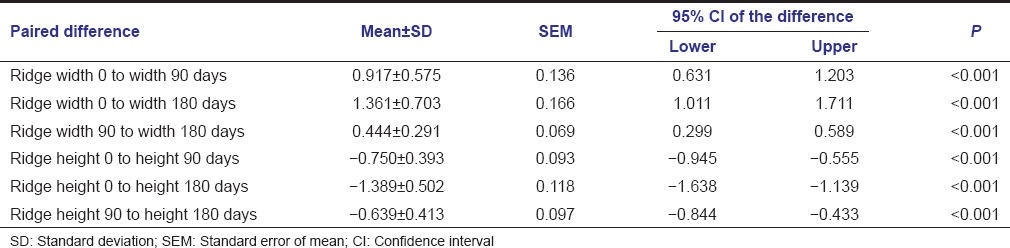
Analysis and comparison of the difference between ridge width and ridge height at different intervals that is baseline, 90, and 180 days were done, and this was facilitated in three pairs each for ridge width and height that is from baseline to 90 days, baseline to 180 days, and 90 to 180 days for the control group. All the results were obtained with P < 0.001 and 95% of confidence interval (CI) and were found to be statistically significant within all pairs thus justifying that there is a significant reduction in loss of ridge width and height at regular intervals for control group [Tables 1 and 2].
Table 1.
Clinical parameters of demineralized freeze-dried bone allograft group at baseline, at 90 days, and at 180 days
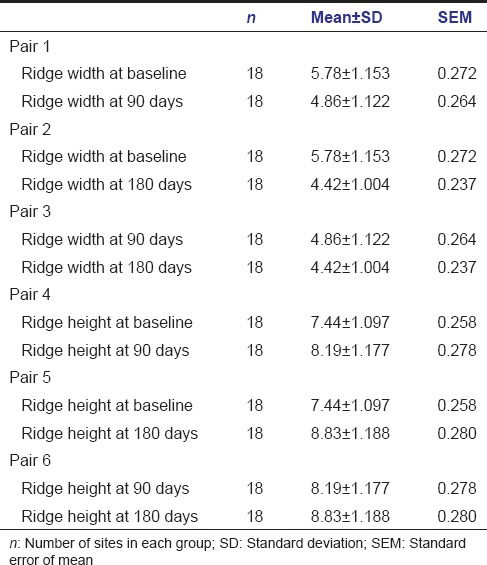
Table 2.
Difference of clinical parameters of demineralized freeze-dried bone allograft group at baseline, at 90 days, and at 180 days
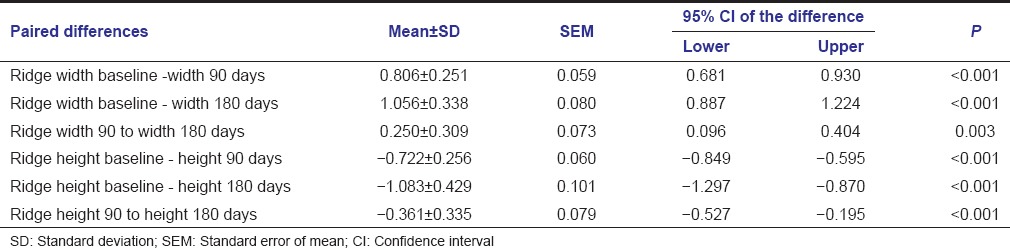
Analysis and comparison of the difference between ridge width and ridge height at different intervals that is baseline, 90, and 180 days was done, and this was facilitated in three pairs each for ridge width and height that is, from baseline to 90 days, baseline to 180 days, and 90 to 180 days for the test group. All the results were obtained with P < 0.001 and 95% of CI and were found to be statistically significant within all pairs thus justifying that there is a significant reduction in loss of ridge width and height at regular intervals. Thus, DFDBA combined with PRF can be used as a graft material to prevent the loss of ridge width and ridge height [Tables 3 and 4].
Table 3.
Clinical parameters of demineralized freeze-dried bone allograft+platelet rich fibrin group at baseline, at 90 days, and at 180 days (mean±standard deviation)

Table 4.
Difference of clinical parameters of demineralized freeze-dried bone allograft+platelet rich fibrin group at baseline, at 90 days, and at 180 days
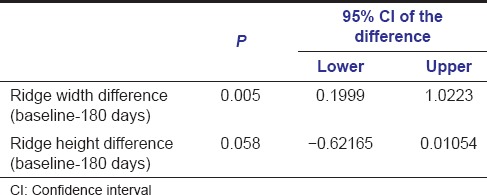
The difference of ridge width and ridge height between the test and the control group are calculated, and the results interpret that in the test group there is loss of 0.75 mm of ridge width while there was loss of 1.36 mm in control group. In control group, 1.36 mm of ridge height was lost, and 1.08 mm was lost in test group. Thus seeing the results, it was proved that using DFDBA combined with PRF had an additional benefit in preserving ridge width better than using DFDBA alone with P < 0.001. Both groups helped to minimize the loss of ridge height, but on comparing both groups, there was no significant statistical difference between groups for ridge height [Tables 5 and 6].
Table 5.
Ridge width and height difference at baseline and at 180 days between demineralized freeze-dried bone allograft group and demineralized freeze-dried bone allograft+platelet rich fibrin
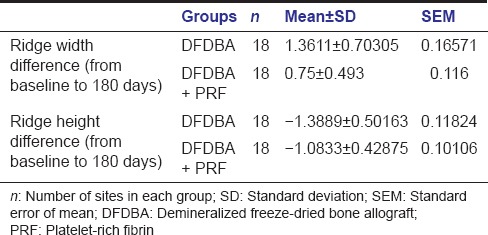
Table 6.
Difference of clinical parameters between test and control groups
Discussion
To achieve a predictable esthetic and functional restoration, it is important to preserve the dimension of alveolar ridge width and height after tooth extraction. Following extraction of tooth various patterns of bone resorption, especially on buccal side, can occur therefore socket preservation plays a very crucial role. Therefore, to preserve the maximum amount of ridge atraumatic extraction was performed which focus on gently severing the periodontal attachment using micro-instrumentation.
Alveolar ridge preservation is a surgical procedure which retains maximum bone and soft tissue after the extraction of tooth is done. The advantage of this procedure is that it maintains the original ridge morphology. Therefore, there will be minimal need for grafting the socket allowing the final restoration to be placed in an esthetic and functional position.[3]
A total of 36 nonrestorable single-rooted teeth were extracted in maxilla or mandible, and sockets preserved with DFDBA combined with PRF were compared with DFDBA alone and dimensional changes were evaluated at 90 and 180 days. In this study at baseline, at 90 days and at 180 days, standardized intraoral periapical radiographs were recorded. The levels of the alveolar bone crest were measured from the most coronal point of the adjacent tooth till the alveolar crest. The type of film, exposure time, processing of film, and radiographic equipment were all standardized.
DFDBA has been widely used in periodontal therapy and is proven to be safe, and it can induce the formation of new bone. DFDBA has both properties osteoconductive and osteoinductive. Use of DFDBA in various animal studies has proved that it could stimulate the formation of new bone by osteoinduction. It stimulates the host undifferentiated mesenchymal cells to differentiate into osteoblasts and lead to bone formation. DFDBA also acts as a scaffold for osteoconduction.[4] As DFDBA fulfills the criteria of an ideal graft material so in this study, it is used in both the groups.
PRF is an autologous source, and it contains various growth factors such as platelet-derived growth factors and insulin-like growth factors. Growth factors are a class of natural biologic mediators that regulate key cellular events in tissue regeneration including cell proliferation, chemotaxis, differentiation, and matrix synthesis via binding to specific cell surface receptors and is also found to enhance healing.[5]
The nature of extraction socket is such that it can cause the loss of the majority of bone graft. Therefore, to avoid the loss of graft material, the use of collagen membrane was used not only to avoid the loss of graft material but also induce stabilize wound and promote blood clot formation. Among all the available membrane collagen membrane was preferred due to its high biocompatibility and hemostatic activity that can facilitate clot formation and would stabilization. Collagen also has a high chemotactic function for fibroblasts. This promotes cell migration, and primary wound coverage maximum efforts were made to achieve complete coverage of membrane, but complete coverage was not obtained in all cases.[6] In a study done by Nam and Park in 2009 showed that if membrane exposure occurs during the healing phase, it does not affect the outcome of ridge preservation. In the present study not a single exposure of membrane occurred. Uneventful healing was noted in all the cases.
While comparing the results of both test and control groups from baseline to 90 days showed statistical significant improvement in all the parameters. Similar improvement was noted for both the groups from baseline to 180 days. However, statistically significant improvement was noted in respect to width from baseline to 180 days in both the groups. This is consistent with the earlier studies done using DFDBA alone for the purpose of socket preservation. The use of PRF along with DFDBA has significant advantages over the use of DFDBA alone. Use of PRF aids in retaining of the bone graft material within the walls of the socket, as it is a fibrin clot, it aids in the arrest of bleeding as well.
All the patients completed the study, and the planned surgical procedures were completed without any complications. The postsurgical phase of healing was uneventful with few patients reporting pain.
However, despite all attempts being made to carry out a study which considers all the required parameters, following some limitations does exist in this study as well. In this study, intraoral radiographic technique was used to measure the bone width and height changes. However, the use of cone beam computed tomography could have been done to achieve more accurate results. Several studies have carried out histomorphometric analysis which was not done in this study. Placement of implants was not done at the follow-up and hence, histological analysis could not be done. In this study, a manual Vernier caliper was used to measure clinical dimensions. However, a digital Vernier caliper could have been used in hindsight. The width of keratinized gingiva could also have been measured in this study.
Conclusion
Irrespective of the reasons for socket preservation, sufficient alveolar ridge width and height are essential to meet the functional and esthetic demand of the patient. The results of this study showed significant reduction in ridge width and height for both groups at 90 and 180 days. when both groups were compared PRF combined with DFDBA preserved ridge width better than DFDBA alone. This procedure would benefit the patient by providing ridge form to meet functional and esthetic needs and spare from future ridge augmentation procedure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Weng D, Stock V, Schliephake H. For which clinical indications in dental implantology is the use of bone substitute materials scientifically subs are socket and ridge preservation techniques at the day of tooth extraction efficient in maintaining the tissues of the alveolar ridge. Eur J Oral Implantol. 2011;4:59–66. [Google Scholar]
- 2.Chan HL, Lin GH, Fu JH, Wang HL. Alterations in bone quality after socket preservation with grafting materials: A systematic review. Int J Oral Maxillofac Implants. 2013;28:710–20. doi: 10.11607/jomi.2913. [DOI] [PubMed] [Google Scholar]
- 3.Avila-Ortiz G, Elangovan S, Kramer KW, Blanchette D, Dawson DV. Effect of alveolar ridge preservation after tooth extraction: A systematic review and meta-analysis. J Dent Res. 2014;93:950–8. doi: 10.1177/0022034514541127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kukreja BJ, Dodwad V, Kukreja P, Ahuja S, Mehra P. A comparative evaluation of platelet-rich plasma in combination with demineralized freeze-dried bone allograft and DFDBA alone in the treatment of periodontal intrabony defects: A clinicoradiographic study. J Indian Soc Periodontol. 2014;18:618–23. doi: 10.4103/0972-124X.142457. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5.Naik B, Karunakar P, Jayadev M, Marshal VR. Role of Platelet rich fibrin in wound healing: A critical review. J Conserv Dent. 2013;16:284–93. doi: 10.4103/0972-0707.114344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zubillaga G, Hagen S, Simon B, Deasy M. Changes in alveolar bone height and width following post-extraction ridge augmentation using a fixed bioabsorbable membrane and demineralized freeze-dried bone osteoinductive graft. J Periodontol. 2003;74:965–75. doi: 10.1902/jop.2003.74.7.965. [DOI] [PubMed] [Google Scholar]


