Abstract
Periodontal disease is infectious, complex, multifactorial, chronic inflammatory disease of supporting periodontal tissues that not only alters the bone morphology but also leads to the reduction in bone height. Different types of bony deformities such as horizontal, vertical, craters, and furcation result from periodontal disease, but vertical and Grade II furcation defects are more amenable to regenerative periodontal therapy. The present case report describes the current concept of periodontal diagnosis and the clinical radiographical efficiency of platelet-rich fibrin and hydroxyapatite bioactive glass composite granules graft combination in the management of localized advance osseous defects with respect to tooth number 36 in chronic periodontitis patient at 1 year postoperatively.
Key words: Furcation defect, hydroxyapatite bioactive glass composite granules, intrabony defect, platelet-rich fibrin, regeneration
Introduction
Regeneration of lost periodontal structures, especially the lost alveolar bone, is a matter of prime concern in the clinical management of periodontal disease as bone destruction is primarily responsible for tooth loss. Different therapeutic modalities such as autogenous bone graft and allograft etc. have been recommended for restoring periodontal osseous defects with their own set of advantages and inherent disadvantages such as sense of procurement of the same, patients discomfort; antigenic reactivity, danger of transmission of diseases such as HIV etc.[1] Recently, Choukroun's platelet-rich fibrin (PRF)[2] and a unique alloplastic graft material hydroxyapatite (HAP)-bioactive glass (BG) composite granules (BioGraft® HABG active) because of promising regenerative potential[1,2] attracted lot of attention of various researchers. The purpose of this case report is to describe the current concept of periodontal diagnosis and to evaluate clinically as well as radiographically the efficacy of Choukroun's PRF and BioGraft® HABG active combination in the treatment of localized advance intrabony and Grade II furcation defect in #36.
Case Report
A 25-year-old female patient reported to the Department of Periodontics with chief complaint of teeth discoloration, mild and intermittent pain in left lower back tooth region, and bleeding gums while brushing since childhood, 12 and 2 months, respectively. On examination, dental fluorosis, local factors, and gingival inflammation were observed [Figure 1]; bleeding on probing, vertical probing depth (VPD) of 4–5 mm with clinical attachment loss (CAL) of 1–2 mm was present in more than 30% teeth, but distobuccal, distolingual, and mid-lingual aspect of vital tooth #36 Showed VPD 11, 4 and 10 mm [Figure 2] with advance CAL of 9, 2, and 8 mm, respectively, along with horizontal probing depth (HPD) of 6 mm with lingual Grade II furcation involvement. The patient was otherwise systemically healthy. The orthopantomogram [Figure 3] and intraoral periapical radiograph [Figure 4] revealed generalized mild bone loss with advance bone loss in furcation and on the distal surface of #36. Generalized mild chronic periodontitis with localized advance loss of periodontal support in #36 was diagnosed.
Figure 1.

Clinical frontal aspect depicts dental fluorosis and local factors associated gingival inflammation
Figure 2.
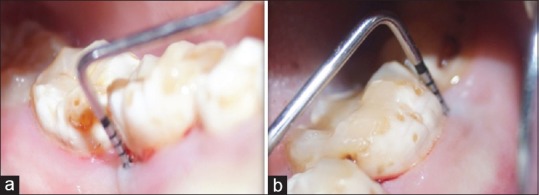
(a) Vertical probing depth of 10 mm at mid-lingual and (b) distobuccal aspect of #36, respectively
Figure 3.

Orthopantomogram reveals generalized mild bone loss with advance bone loss in furcation and on the distal surface of #36
Figure 4.
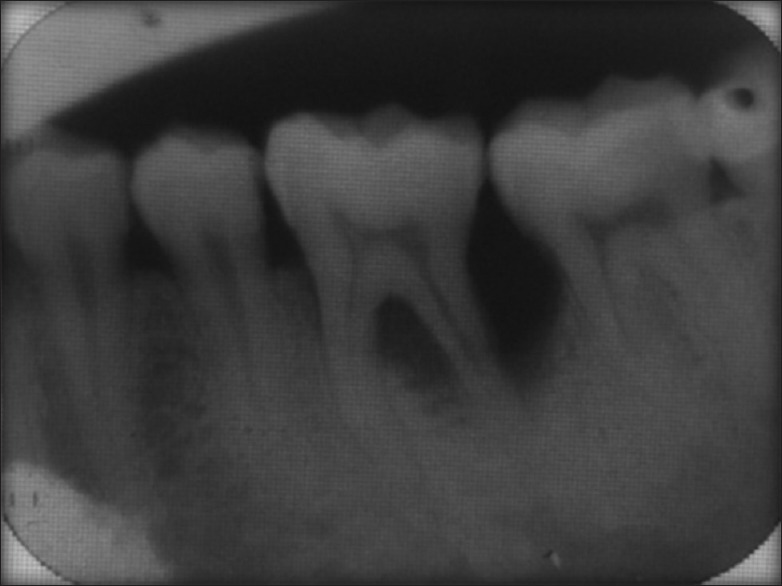
Intraoral periapical radiograph showing interradicular bone loss and severe osseous defect at distal aspect of #36
After Phase I therapy, plaque control was re-evaluated every 2nd week and maintenance therapy was reinforced as per need. By the end of 8 weeks, gingiva was found healthy with normal sulcus depth, but no change was observed in #36. The management of existing isolated intrabony and Grade II furcation defect in #36 utilizing different periodontal regenerative treatment modalities such as bone grafts and guided tissue regeneration was discussed in detail with the patient. Choukroun's PRF and BioGraft® HABG active was selected, and duly signed consent from the patient was taken. The patient was advised routine blood, urine investigations which were within the normal limits and HIV, hepatitis C virus, and hepatitis viral markers were reported to be negative.
PRF prepared just before the surgery as per protocol developed by Choukroun's et al.[3] Ten milliliters of blood sample was taken from antecubital vein of the patient in sterile glass tube without an anticoagulant and centrifuged at 2400–2800 rpm for 12 min. A fibrin clot was formed in the middle part of the tube whereas the upper and bottom part contained acellular plasma and red corpuscles, respectively.
Under aseptic condition, after local anesthesia administration both the buccal and lingual full-thickness flaps were reflected after crevicular incision with respect to #35–#37 followed by thorough subgingival scaling and root planing of both furcation and intrabony defects associated with #36. A fibrin clot formed in the middle part of the tube was obtained and amalgamated with BioGraft® HABG active and filled in both furcation and intrabony defects of #36 followed by direct loop sutures and periodontal dressing application. The patient was instructed oral rinse twice daily with 0.2% chlorhexidine for 2 weeks and amoxicillin 500 mg and ibuprofen 400 mg was advised thrice a day for 5 days.
Surgical wound healed uneventfully, and sutures were removed 2 weeks postoperatively. Reduction in VPD [Figure 5], HPD [Figure 6], and CAL was observed at 3, 9, 12 months as shown in. Postoperative radiographic evaluation of #36 at 3 months showed mild changes [Figure 7a] whereas complete healing of Grade II furcation and intrabony defect up to the adjacent mesial alveolar bone margin of #37 observed at 9 and 12 months [Figure 7b and c].
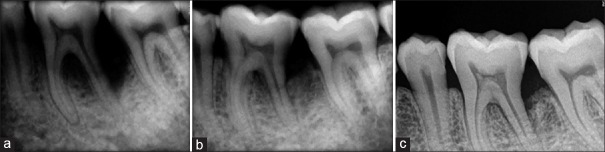
Figure 5.
(a) Vertical probing depth distobuccal aspect reduced to 6 mm (b) reduced to 4 mm (c) reduced to 3 mm at 3, 9 and 12 months postoperative respectively
Figure 6.
(a) Horizontal probing depth 4 mm (b) 3 mm (c) 0 mm at 3, 9 and 12 months postoperatively
Figure 7.
Postoperative healing of hard structures at (a) at 3 months (b) 9 months (c) 12 months respectively
Discussion
Chronic periodontitis is characterized by loss of attachment due to destruction of periodontal ligament, loss of adjacent supporting bone; usually slow to moderate rate of progression but may have the period of rapid destruction localized, involving one area of the tooth's attachment or more generalized. The area of rapid destruction characterized by probing depth >6 mm with attachment loss >4 mm, furcation involvement if present will exceed Class I (incipient) with radiographic evidence of same.[4] The severity and distribution/extent of chronic periodontitis was diagnosed on the basis of 1999 international workshop for classification of periodontal diseases and condition; and American Academy of Periodontology task force report 2014, respectively (the task force preferred to use the percentage of affected teeth rather than the percentage of affected sites as an extent descriptor for chronic periodontitis that is generalized chronic periodontitis may be defined as periodontitis without a clear pattern of disease distribution of affected teeth or >30% of affected teeth).[5] Similarly, in the present case, the generalized chronic mild periodontitis was observed in >30% of the teeth along with localized severe loss of periodontal support with respect to #36, therefore, diagnosed as generalized chronic mild periodontitis associated with localized advance loss of periodontal support in #36.
As regeneration in furcation and deep intrabony defect is difficult to attain because anatomy that impedes the accessibility for individual oral hygiene in molars, professional root debridement and due to slow and difficult integration of the grafted material into the physiological architecture as cited in reports of Sharma and Pradeep[6] and Rastogi et al.,[7] respectively. In spite of different periodontal regenerative approaches, as currently, not a single regenerative material is considered gold standard in the treatment of osseous defects; therefore, amalgamation of BioGraft® HABG active and Choukroun's PRF was utilized because of their promising properties[8,9,10] in the present report to obtain maximum outcome.
Dohan et al.[8] reported that the interleukin (IL) 1β, IL 6, tumor necrosis factor-α, IL 4, vascular endothelial growth factor (VEGF) in the PRF clot play a crucial role in balancing the tissue homeostasis, whereas the healing cytokines IL 4 and VEGF inhibit inflammatory signal pathways thereby support and coordinate the neovascularization which may be the reason for uneventful healing in present case.
The present case report showed reduction in PDs, CAL clinically and complete healing of furcation as well as intrabony defect radiographically; may be due to the property of BioGraft® HABG that bonds with host bone faster than HAP ceramics and resorbs slowly but completely than BG, which is replaced and remodeled by the new bone. PRF when used as a membrane or as a grafting material creates an improved space making effect, which facilitates cell events that are favorable for periodontal regeneration leading to mineralized tissue formation,[9] and it also induces the cell proliferation of osteoblasts, periodontal ligament cells, growth factors, but suppress the oral epithelial cell growth.[10] The combined effect PRF and BioGraft® HABG because of their distinct properties along with thorough debridement may result in excellent outcome in the present case report, which is in accordance with the reports of Rastogi et al.[7] utilized HAP particles with PRF membrane in the intrabony defect, whereas Salaria et al.[11] PRF with BioGraft® HABG active in Grade II furcation defect in molar, respectively.
Conclusion
Amalgamation of PRF and BioGraft® HABG active was effective for the management of adjoin localized advance intrabony and Grade II furcation defect in the same tooth, but long-term randomized clinical trials should be undertaken before reaching final conclusion.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Debnath T, Chakraborty A, Pal TK. A clinical study on the efficacy of hydroxyapatite – Bioactive glass composite granules in the management of periodontal bony defects. J Indian Soc Periodontol. 2014;18:593–600. doi: 10.4103/0972-124X.142451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corso MD, Toffler M, Dohan Ehrenfest DM. Use of an autologous leukocyte and plate let-rich fibrin (L-PRF) membrane in post – Avulsion sites: An overview of Choukroun's PRF. J Implants Adv Clin Dent. 2010;9:27–35. [Google Scholar]
- 3.Choukroun J, Adda F, Schoeffler C, Vervelle A. A opportunite in paroimplantology in PRF. Implatodontie. 2001;42:55–62. [Google Scholar]
- 4.American Academy of Periodontology. Parameter on chronic periodontitis with slight to moderate loss of periodontal support. J Periodontol. 2000;71(5 Suppl):853–5. doi: 10.1902/jop.2000.71.5-S.853. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Periodontology task force report on the update to the classification of periodontal diseases and conditions. J Periodontol. 2015;86:835–8. doi: 10.1902/jop.2015.157001. [DOI] [PubMed] [Google Scholar]
- 6.Sharma A, Pradeep AR. Autologous platelet-rich fibrin in the treatment of mandibular degree II furcation defects: A randomized clinical trial. J Periodontol. 2011;82:1396–403. doi: 10.1902/jop.2011.100731. [DOI] [PubMed] [Google Scholar]
- 7.Rastogi P, Saini H, Singhal R, Dixit J. Periodontal regeneration in deep intrabony periodontal defect using hydroxyapatite particles with platelet rich fibrin membrane-a case report. J Oral Biol Craniofac Res. 2011;1:41–3. doi: 10.1016/S2212-4268(11)60010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part III: Leucocyte activation: A new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e51–5. doi: 10.1016/j.tripleo.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 9.Diss A, Dohan DM, Mouhyi J, Mahler P. Osteotome sinus floor elevation using Choukroun's platelet-rich fibrin as grafting material: A 1-year prospective pilot study with microthreaded implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:572–9. doi: 10.1016/j.tripleo.2007.08.021. [DOI] [PubMed] [Google Scholar]
- 10.Tsai CH, Shen SY, Zhao JH, Chang YC. Platelet rich fibrin modulates cell proliferation of human periodontal related cells in vitro reports. J Dent Sci. 2009;4:130e5. [Google Scholar]
- 11.Salaria SK, Chahal NK, Chahal SS, Singh P. Single flap approach with lingual access in conjugation with PRF and Biograft HABG for the management of residual grade II furcation defect occurring from primary endodontic with secondary periodontal lesion: An interdisciplinary case report. J Pharma Biomed Sci. 2016;6:18–22. [Google Scholar]