Abstract
Background: Around one out of two mothers give births by cesarean section (CS) surgery in Iran and about half of this number is due to previous CS. Recently Health Sector Evolution (HSEP) program (started in April 2014) targets the high rate of CS in Iran. To assess the impact of the interventions, we emphasized that the First Birth Cesarean (FBC) proportion is one of the main indicators to assess the controlling programs.
Methods: Data on the mode of delivery were collected in Kerman province between 21 March and 20 March 2015 classified by hospital ownership. FBC proportion is defined as the number of CS in the first pregnancies divided by the total number of first births. Chi-square test for trend was used to assess the trends.
Results: Total number of births was around 34000. There were 8.9 and 13.1 percent reduction in CS and FBC proportion respectively. CS proportion was 54.5 at the end of the first quarter of the studied period and reached to 49.6 at the end of the period (p<0.0001). Also, FBC proportion was 54.1 percent at first and reached to 47 percent at the end of the study period. The main reason for CS was due to previous CS. At the hospital level, the highest reduction in CS and FBC proportion were in public hospitals.
Conclusion: Results suggested more reduction in FBC proportion than the CS proportion, so this is a very good sign since more potential CS cases will be prevented. As repeated CS is one of the main indications for the operation, in the short term, even effective policies may change the overall proportion slightly, while the FBC proportion is more sensitive to reflect the impacts. Therefore, it is necessary to target the main fuel to reduce CS proportion effectively.
Keywords: Cesarean, Delivery, Health Policy
Introduction
Today world encounters a steadily increasing trend of Cesarean section (CS) proportion (1). CS has been a common surgical method to improve reproductive health around the world, while considerable numbers are unnecessary (1,2). However, it reflects high availability and access to health care it should be noted that most of the time it is not necessary and could endanger the health of mother and child.
Based on the latest report of WHO Iran is among the countries with high rates of CS. Forty-eight percent of births are by CS In Iran (3). Meaning one out of two mothers give births by CS surgery, which is much higher than the recommended range by WHO and also three times higher than middle east (4). This high rate and increasing trend need more attention (2,3,5-7). Recently researchers and Policymakers become interested in this health challenge.
CS is recommended in occasions such as dystocia, malpresentation, preeclampsia and some cases of infections like HIV, presence of active genital lesions of Herpes simplex, etc; but in low-risk women may cause serious complications (8). However, subsequent morbidities are more frequent in low risk and unnecessary CS cases compared to vaginal delivery (9-13). Based on recent evidences in countries with the rate of CS less than 15% as a life-saving surgery, there was a negative association between neonatal, infant and maternal mortality and cesarean section, in the case of exceeding more than 15% there was no additional gain (14). To improve maternal health and also reduce the economic burden on the health systems, planning and implementing the effective intervention to reduce CS proportion is necessary (6,15).
Health Sector Evolution Plan (HSEP) program which is recently implemented by Ministry of Health and Medical Organization (MOHME) of Iran, primarily intended to reduce the financial burden of treatment procedures on people. The first phase of HSEP initiated in May 2014. One out of seven parts of this guideline is about increasing natural vaginal delivery (NVD) by decreasing unnecessary CS cases. The other goals of this program are presented by others (16). The final goal of this part is to improve maternal and neonatal heath. The ideal range of CS proportion is 25-30%. In each university 2.5% reduction to the baseline is recommended in a three month time intervals and finally 10 percent reduction by the first year. CS rate (number of CS cases divided by total births) has been determined as the main indicator. This study aimed to make a suggestion to this program.
To plan preventive programs to reduce CS rate effectively, precise data on the causes of CS is needed. Nowadays the most common indication for CS is due to previous CS, so the primary CS serves as a good resource for continuing the high rate of CS. In other words, the concern is primary CS especially the cesarean section in the first pregnancy. Therefore, if a sustainable reduction is a goal, addressing the CS cases in first pregnancies is needed. Despite the importance of such cases, there is no reliable data on it and its causes. In this study data on first birth, CS were collected alongside the other recommended items by MOHME in HSE program. This paper aimed to emphasize cesarean section in the first pregnancy versus in all pregnancies (FBC proportion) as an important issue in evaluating cesarean reduction policies. Also, evaluate FBC proportion in Kerman University of Medical Sciences (KMU) during a twelve month period (21 March 2014, 20 March 2015). The study period started 45 days earlier than the HSEP initiation.
Methods
Kerman as one of the largest province of Islamic Republic of Iran with a population of more than three million people is located in the southeast. Medical and Health services to this big province are provided by four medical universities. Kerman University of Medical Sciences (KMU) provides services to seven districts out of 26. CS surgery is a common mode of delivery in this region as the other parts of Iran. More than fifty percent (52%) of the births in the year previous this study commence were by CS surgery. Chi-square test for trend was used to assess the trends. Statistical significance was defined by a p-value of <0.05.
CS and FBC proportion were calculated at the end of the three month intervals. CS proportion is calculated as total number of CS cases divided by total number of births. First Birth Cesarean Section proportion (FBC) calculated as total number of cesarean section in the first pregnancy divided by total number of first births. Changes were calculated at the end of each interval compared to the first by hospital ownership.
First Birth Cesarean Proportion
FBS proportion= Number of cesarean section in first pregnancy / Total number of cesarean section
Results
Total number of births and births in first pregnancies were 33888 and 12383, respectively. Overall CS and FBC proportion were 51.2 and 47.7 in the study period, respectively. There were 8.9 and 13.1 percent reduction in CS and FBC proportion, respectively. CS proportion was 54.5 at the end of the first quarter of the studied period and reached to 49.6 at the end of the period (p<0.001). Also, FBC proportion was 54.1 percent at first and reached to 47 percent at the end of the study period (Table 1). The main reason for CS was due to previous CS. There was a declining trend for CS and a steeper one for FBC. At the hospital level, the highest reduction in CS and FBC proportion were in public hospitals.
Table 1. CS and FBC proportion at hospital level in each interval .
| Hospital Ownership | Indicator |
First Quarter |
Second Quarter |
Third Quarter |
Fourth Quarter |
p-value for trend |
| Public Sector | Births | 6129 | 6594 | 6914 | 6548 | - |
| First Births | 2361 | 2251 | 2142 | 2260 | - | |
| CS (%) | 3127(51) | 3101(47) | 3322(48) | 3065(46.8) | <0.001 | |
| FBC (%) | 1160(49.1) | 962(42.7) | 809(37.8) | 1002(44.3) | <0.001 | |
| Private Sector | Births | 1865 | 2166 | 1844 | 1828 | - |
| First Births | 906 | 957 | 789 | 717 | - | |
| CS (%) | 1230(66) | 1321(61) | 1082(58.7) | 1092(59.7) | <0.001 | |
| FBC (%) | 607(67) | 553(57.8) | 440(55.8) | 398(55.5) | <0.001 | |
| Total | Births | 7994 | 8760 | 8758 | 8376 | - |
| First Births | 3267 | 3208 | 2931 | 2977 | - | |
| CS (%) | 4357(54.5) | 4422(50.5) | 4404(50.3) | 4157(49.6) | <0.001 | |
| FBC (%) | 1767(54.1) | 1515(46.4) | 1249(42.6) | 1400(47) | <0.001 |
Around 23 percent of the births and 27.2 of the cesarean case occurred in hospitals owned by private sector. On the other hand, 27.2 percent of nulliparous women deliver in this sector, but the portion of the cesarean section in the first pregnancies is higher. In other words, 33.7 percent of cesarean section in the first pregnancies occurred in the private sector.
Previous CS was the main reason for CS in near half of the CS cases (Fig. 1). Around 13 percent of CS surgery cases were due to fetal distress and also seven percent because of prolonged labor.
Fig. 1 .
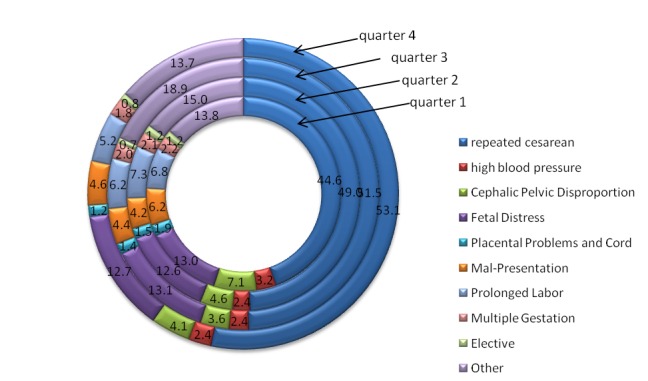
Causes of CS at the end of each quarter
Fifty-six out of ninety obstetricians gave services all the study period. On physician level, for the CS proportion indicator around fifty percent of them reduced CS proportion more than 10 percent and 5.4 percent experienced no change (Fig. 2).
Fig. 2 .
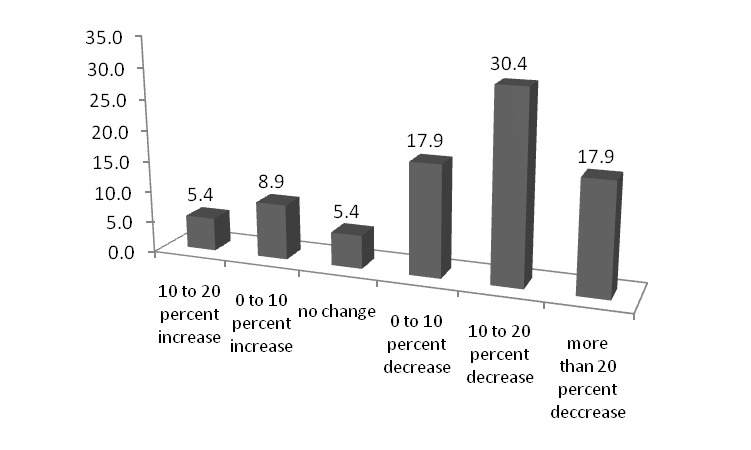
distribution of the physicians based on change in CS proportion at the end of the study period compared with the first quarter
Discussion
At the end of the study period, there was 8.9 percent reduction in CS proportion and more reduction was in FBC proportion. Since about half of the CS cases were due to previous CS, more reduction in FBC proportion than CS proportion is very good for future because more of the prospective CS cases will be prevented. Although, our study started in March 2014 (45 days before the HSEP initiation) so we can attribute some of this reduction to the implementation of this program. As this program installed just in the public sector further reduction in the public sector can be considered evidence for this claim.
Mode of delivery in Iran has changed substantially recently (3,7). CS proportion increased 30 percent in 2010 compared to 2000 in Iranian women with a higher increase in rural population (7). CS had been a common mode of birth, and this is not true just about Iran (1,2,17). Zizza, A. et al., declared that near half of the countries around the world exceeded the recommended range by WHO (2). In the United States during an eight-year period a 40 percent increase in CS has reported which mainly was due to increase in primary cases. In Ethiopia a ten-fold increase during a 15 years period is reported (18). In China around 55 percent of birth are by cesarean (19). Thailand experienced twofold increase between 1992 and 2011 (20). Although CS is a lifesaving surgery, postpartum maternal morbidity and mortality, neonatal complications are more frequent among the cases, and it will impose an additional burden on the health system due to cost and complications if it is not necessary nor medically indicated (1,9,11,12,14,21-24).
If we want to reduce caesarean sections substantially, we should work on its causes. Most of the time, as in this study, previous CS is the most common reason for CS surgery (6,20,22,25,26).Therefore, it is a good source for future cases of CS. In the case of previous CS physician and health workers have two options for the mother, again CS surgery or Vaginal Birth after Cesarean (VBAC). Since VABC may fail and result in additional harm and costs the safer option is prevention of the primary CS (27). In other countries also a reduction in CS proportion along with a reduction in primary and first births is reported. In the United States, one of the Healthy People 2010 objectives was reducing CS in women giving birth for the first time to 15 percent. In this country, similar to the result of the present study, CS decreased more steeper in nulliparous, term, singleton in a vertex presentation in comparison to the CS in all women (28). Also, Roberts and his colleagues reported the increase in CS in multiparous following the increase in CS in nulliparous cases (29).
Conclusion
Unfortunately, there is no reliable data on birth order but as the findings show a considerable proportion of the CS cases were in first pregnancy cases. So based on a clear view of causes of primary CS and especially CS in first pregnancy substantial decline in CS cases is expected. Having a good picture about the causes of CS cases especially about the CS in first pregnancies is necessary to prevent prospective cases and plan effective strategies. Therefore, targeting the CS in first pregnancies and their causes is recommended to this HSEP program which is also emphasized by American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine and others (28,30-32). This study aimed to emphasis on addressing FBC proportion to achieve a considerable reduction in cesarean cases.
Limitations
One of the limitations of this study was lack of access to the data on CS in detail before the initiative of the HSEP. So we couldn’t assess the effect of this program. The other one was lack of data on the physician level to calculate FBC proportion. So calculation of the indicator at physician level was aborted. Data collection on these items to calculate FBC proportion and systematic monitoring is recommended. Alongside, development of educational programs to aware women about complications of CS and arrange a committee in each case for decision about mode of delivery specially for the primary cases and first births is recommended. The authors recommend providing and monitoring comprehensive data on the primary CS cases and cesarean section in the first pregnancies including causes at national, provincial, hospital and physician level in order to prevent prospective CS cases more effectively.
Cite this article as: Safari-Faramani R, Haghdoost AA, Nakhaei N, Foroudnia Sh, Mahmoodabadi Z, Safizadeh M. First birth cesarean proportion: A missed indicator in controlling policies. Med J Islam Repub Iran 2016 (10 July). Vol. 30:394.
References
- 1.Niino Y. The increasing cesarean rate globally and what we can do about it. Biosci Trends. 2011;5(4):139–50. doi: 10.5582/bst.2011.v5.4.139. [DOI] [PubMed] [Google Scholar]
- 2.Zizza A, Tinelli A, Malvasi A, Barbone E, Stark M, De Donno A. et al. Caesarean section in the world: a new ecological approach. J prev med hyg. 2011;52(4):161–73. [PubMed] [Google Scholar]
- 3.Azami-Aghdash S, Ghojazadeh M, Dehdilani N, Mohammadi M, Asl Amin Abad R. Prevalence and Causes of Cesarean Section in Iran: Systematic Review and Meta-Analysis. Iranian Journal of Public Health. 2014;43(5):545–55. [PMC free article] [PubMed] [Google Scholar]
- 4.Moore B. Appropriate technology for birth. The Lancet. 1985;326(8458):787. [Google Scholar]
- 5.Ahmad-Nia S, Delavar B, Eini-Zinab H, Kazemipour S, Mehryar A, Naghavi M. Caesarean section in the Islamic Republic of Iran: prevalence and some sociodemographic correlates. East Mediterr Health J. 2009;15(6):1389–98. [PubMed] [Google Scholar]
- 6.Badakhsh MH, Seifoddin M, Khodakarami N, Gholami R, Moghimi S. Rise in cesarean section rate over a 30-year period in a public hospital in Tehran, Iran. Arch Iran Med. 2012;15(1):4–7. [PubMed] [Google Scholar]
- 7. Rashidian A, Khosravi A, Kabiri R, Khodayari-Moez E, Elahi E, Arab M, et al. Islamic Republic of Iran's Multiple Indicator Demographic and Health Survey (IrMIDHS) 2010. Tehran: Ministry of Health and Medical Education 2012.
- 8.Tita ATN. When Is Primary Cesarean Appropriate: Maternal and Obstetrical Indications. Seminars in Perinatology. 2012;36(5):324–7. doi: 10.1053/j.semperi.2012.04.014. [DOI] [PubMed] [Google Scholar]
- 9.Deneux-Tharaux C, Carmona E, Bouvier-Colle M-H, Bréart G. Postpartum maternal mortality and cesarean delivery. Obstetrics & Gynecology. 2006;108(3, Part 1):541–8. doi: 10.1097/01.AOG.0000233154.62729.24. [DOI] [PubMed] [Google Scholar]
- 10.Liu S, Liston RM, Joseph K, Heaman M, Sauve R, Kramer MS. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. Canadian medical association journal. 2007;176(4):455–60. doi: 10.1503/cmaj.060870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Souza JP, Gülmezoglu A, Lumbiganon P, Laopaiboon M, Carroli G, Fawole B. et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004-2008 WHO Global Survey on Maternal and Perinatal Health. BMC medicine. 2010;8(1):71. doi: 10.1186/1741-7015-8-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Werner EF, Han CS, Savitz DA, Goldshore M, Lipkind HS. Health outcomes for vaginal compared with cesarean delivery of appropriately grown preterm neonates. Obstetrics & Gynecology. 2013;121(6):1195–200. doi: 10.1097/AOG.0b013e3182918a7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Villar J, Valladares E, Wojdyla D, Zavaleta N, Carroli G, Velazco A. et al. Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. The Lancet. 2006;367(9525):1819–29. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- 14.Volpe FM. Correlation of Cesarean rates to maternal and infant mortality rates: an ecologic study of official international data. Revista Panamericana de Salud Pública. 2011;29:303–8. doi: 10.1590/s1020-49892011000500001. [DOI] [PubMed] [Google Scholar]
- 15.Barber EL, Lundsberg L, Belanger K, Pettker Cm, Funai EF, Illuzzi JL. Contributing Indications to the Rising Cesarean Delivery Rate. Obstetrics and gynecology. 2011;118(1):29. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moradi-Lakeh M, Vosoogh-Moghaddam A. Health Sector Evolution Plan in Iran; Equity and Sustainability Concerns. International journal of health policy and management. 2015;4(10):637. doi: 10.15171/ijhpm.2015.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klemetti R, Che X, Gao Y, Raven J, Wu Z, Tang S. et al. Cesarean section delivery among primiparous women in rural China: an emerging epidemic. American journal of obstetrics and gynecology. 2010;202(1):65 e1–e6. doi: 10.1016/j.ajog.2009.08.032. [DOI] [PubMed] [Google Scholar]
- 18.Gebremedhin S. Trend and socio-demographic differentials of Caesarean section rate in Addis Ababa, Ethiopia: analysis based on Ethiopia demographic and health surveys data. Reproductive health. 2014;11(1):14. doi: 10.1186/1742-4755-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu Y, Li G, Chen Y, Wang X, Ruan Y, Zou L. et al. A descriptive analysis of the indications for caesarean section in mainland China. BMC pregnancy and childbirth. 2014;14(1):410. doi: 10.1186/s12884-014-0410-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Charoenboon C, Srisupundit K, Tongsong T. Rise in cesarean section rate over a 20-year period in a public sector hospital in northern Thailand. Archives of gynecology and obstetrics. 2013;287(1):47–52. doi: 10.1007/s00404-012-2531-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iyoke C, Ugwu G, Ezugwu F, Lawani O, Onah H. Risks associated with subsequent pregnancy after one caesarean section: A prospective cohort study in a Nigerian obstetric population. Nigerian Journal of Clinical Practice. 2014;17(4):442. doi: 10.4103/1119-3077.134035. [DOI] [PubMed] [Google Scholar]
- 22. Menacker F, Declercq E, Macdorman MF, editors. Cesarean delivery: background, trends, and epidemiology. Seminars in Perinatology; Elsevier 2006. [DOI] [PubMed]
- 23.O'Neill SM, Agerbo E, Kenny LC, Henriksen TB, Kearney PM, Greene RA. et al. Cesarean Section and Rate of Subsequent Stillbirth, Miscarriage, and Ectopic Pregnancy: A Danish Register-Based Cohort Study. PLoS medicine. 2014;11(7):e1001670. doi: 10.1371/journal.pmed.1001670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA. et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstetrics & Gynecology. 2006;107(6):1226–32. doi: 10.1097/01.AOG.0000219750.79480.84. [DOI] [PubMed] [Google Scholar]
- 25.Festin MR, Laopaiboon M, Pattanittum P, Ewens MR, Henderson-Smart DJ, Crowther CA. Caesarean section in four South East Asian countries: reasons for, rates, associated care practices and health outcomes. BMC pregnancy and childbirth. 2009;9(1):17. doi: 10.1186/1471-2393-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sanavi FS, Rakhshani F, Ansari-Moghaddam A, Edalatian M. Reasons for Elective Cesarean Section amongst Pregnant Women; A Qualitative Study. Journal of Reproduction & Infertility. 2012;13(4):237. [PMC free article] [PubMed] [Google Scholar]
- 27.Obstetricians ACo, Gynecologists Gynecologists. Obstetricians ACo, GynecologistsACOG Practice bulletin no115: Vaginal birth after previous cesarean delivery. Obstetrics and gynecology. 2010;116(2 Pt 1):450. doi: 10.1097/AOG.0b013e3181eeb251. [DOI] [PubMed] [Google Scholar]
- 28.Osterman M, Martin JA. Trends in Low-risk Cesarean Delivery in the United States, 1990-2013 National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2014;63(6):1–16. [PubMed] [Google Scholar]
- 29.Roberts CL, Algert CS, Ford JB, Todd AL, Morris JM. Pathways to a rising caesarean section rate: a population-based cohort study. BMJ open. 2012;2(5):e001725. doi: 10.1136/bmjopen-2012-001725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Obstetricians ACo, Gynecologists. Save prevention of the primary cesarean delivery. Obstetric care consensus Washington, DC: ACOG 2014.
- 31.Wanjari SA. Rising caesarean section rate: a matter of concern? International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2014;3(3):728–31. [Google Scholar]
- 32.Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstetrics and gynecology. 2012;120(5):1181. doi: 10.1097/aog.0b013e3182704880. [DOI] [PMC free article] [PubMed] [Google Scholar]


