Abstract
Hazardous drinking is prevalent among persons living with HIV/AIDS (PLWHA). Anxiety sensitivity is a vulnerability factor that is highly associated with hazardous drinking among seronegatives, but has yet to be tested in PLWHA. Additionally, there is a need to examine potential mechanisms underlying associations of anxiety sensitivity and hazardous drinking. Emotion dysregulation is one potential construct that may explain the association between anxiety sensitivity and hazardous drinking. The current study examined emotion dysregulation as a potential explanatory variable between anxiety sensitivity and four, clinically significant alcohol-related outcomes among PLWHA: hazardous drinking, symptoms of alcohol dependence, number of days consuming alcohol within the past month, and degree of past heavy episodic drinking. The sample included 126 PLWHA (Mage=48.3; SD=7.5; 65.9% male). Results indicated significant indirect effects of anxiety sensitivity via emotion dysregulation in all models. Indirect effects (κ2) were of medium effect size. Alternative models were run reversing the predictor with mediator and, separately, reversing the mediator with the proposed outcome(s); alternative models yielded non-significant indirect effects in all but one case. Together, the current results indicate that anxiety sensitivity is associated emotion dysregulation, which, in turn, is associated with hazardous drinking outcomes. Overall, these findings may provide initial empirical evidence that emotion dysregulation may be a clinical intervention target for hazardous drinking.
Keywords: Alcohol, Hazardous Drinking, Vulnerabilities, Anxiety Sensitivity, Emotion Dysregulation
1. Introduction
Hazardous drinking, defined as a pattern of substance use that increases the risk of harmful consequences (World Health Organization [WHO], 2015), is highly common among persons living with HIV/AIDS (PLWHA; Conigliaro, Justice, Gordon, Bryant, & VACS Alcohol and Behavior Change Research Group, 2006; Schneider, Chersich, Neuman, & Parry, 2012). Hazardous drinkers do not necessarily meet full diagnostic criteria for an alcohol use disorder (AUD), but their drinking volume and patterns increase their risk of health and social problems. Even using conservative standard definitions, hazardous drinking is common among PLWHA (from 37-68%; Conigliaro et al., 2006), which is nearly double the rate found in the general population (Dew, Elifson, & Sterk, 2007; Galvan et al., 2002). For example, hazardous drinking has been associated with severe problems, such as HIV medication non-adherence (Kleeberger et al., 2001; Samet, Horton, Traphagen, Lyon, & Freedberg, 2003), risky sexual behavior (Ehrenstein, Horton, & Samet, 2004; Stein et al., 2005), other types of substance use, (Gonzalez, Barinas, & O’Cleirigh, 2011), smoking (Vidrine, Marks, Arduino, & Gritz, 2012), global psychological and physical health complications (Dew et al., 1997), rapid disease progression (Conigliaro et al., 2003), medication toxicities (Fein, Fletcher, & Di Sclafani, 1998), peripheral neuropathy (Ferrari & Levine, 2010), organ failure, and poor virologic control (Arnsten et al., 2001), and may lead to increased risk of transmission and premature death (Galvan et al., 2002).
Individual differences in psychological factors are an important consideration for better understanding hazardous drinking among PLWHA (for review, see Shuper et al., 2010). Anxiety sensitivity is one individual difference construct that may be particularly relevant to hazardous drinking among PLWHA. Anxiety sensitivity is a cognitive factor that reflects the extent to which an individual experiences physiological arousal as potentially harmful or dangerous (Kushner, Thuras, Abrams, Brekke, & Stritar, 2001; Reiss & McNally, 1985). Anxiety sensitivity is a risk factor for anxiety and depression (Naragon-Gainey, 2010) and it has consistently been related to hazardous drinking among those without HIV (seronegatives; Schmidt, Buckner, & Keough, 2007; Stewart, Peterson, & Pihl, 1995; Stewart, Samoluk, & MacDonald, 1999). Research suggests greater arousal-dampening effects of alcohol for individuals with higher anxiety sensitivity when compared with lower anxiety sensitivity (e.g., Stewart, Zvolensky, & Eifert, 2001; Zack, Poulos, Aramakis, Khamba, & MacLeod, 2007). Individuals with higher anxiety sensitivity also report greater alcohol-related problems, including increased rates of excessive alcohol consumption (Conrod, Stewart, & Pihl, 1997; Stewart et al., 1999), drinking to legal intoxication more frequently (Stewart et al., 1995, 2001), and higher rates of alcohol dependence (Lewis & Vogeltanz-Holm, 2002). Further, longitudinal studies have implicated anxiety sensitivity in the development of alcohol problems. For example, Schmidt and colleagues (2007) reported that individuals with high anxiety sensitivity were more likely to have developed an alcohol use disorder after 24 months than were individuals with low anxiety sensitivity. However, little is known about relationship between anxiety sensitivity and hazardous drinking among PLWHA. Anxiety sensitivity may be particularly important in PLWHA due to the common physiological arousal/distress associated with symptoms of disease progression and medication side effects (Ammassari et al., 2001).
In addition to examining the direct association of anxiety sensitivity and hazardous alcohol use among PLWHA, there is a need to explicate the processes governing such associations. Indeed, examining underlying factors may help to explicate explanatory mechanisms by which anxiety sensitivity may impact alcohol use in this population. One construct that may provide explanatory value among associations of anxiety sensitivity and hazardous drinking is emotion dysregulation (Chandley, Luebbe, Messman-Moore, & Ward, 2014). Emotion dysregulation has been defined as difficulties engaging a set of abilities wherein one can observe, understand, evaluate, and differentiate one’s emotions and subsequently access strategies to regulate emotions and control behavioral responses (Gratz & Roemer, 2004; Tull & Aldao, 2015). Generally, emotion dysregulation is associated with increased alcohol consumption and dependence (Berking et al., 2011), as well as increased alcohol-related problems (Dvorak et al., 2014). Among PLWHA, those meeting criteria for hazardous drinking have greater levels of emotion dysregulation, relative to those not meeting such criteria (Garey et al., 2015).
Theoretically, individuals with greater anxiety sensitivity may respond to physiological sensations (e.g., those associated with anxiety) with less acceptance (i.e., greater emotion dysregulation), resulting in greater subjective distress (Kashdan, Zvolensky, & McLeish, 2008). As a result of such emotion dysregulation, these individuals may use alcohol as a means of regulating negative emotions. Importantly, the theoretical framework derived from other areas of research in substance use (e.g., smoking; Johnson, Farris, Schmidt, & Zvolensky, 2012) indirectly support emotion dysregulation as a factor underlying anxiety sensitivity and hazardous drinking. For example, Johnson and colleagues (2012) demonstrated evidence of an indirect effect from anxiety sensitivity to smoking-relevant outcomes via emotion dysregulation. Currently, no such model has been tested examining anxiety sensitivity, emotion dysregulation, and hazardous alcohol use in general or among PLWHA specifically.
Together, the current study tested the hypothesis that anxiety sensitivity would exert an indirect effect on alcohol-related criterion variables via emotion dysregulation (see Figure 1). Specifically, anxiety sensitivity was expected to positively predict emotion dysregulation, which, in turn, would be associated with the alcohol dependent variables. In the current study, four clinically significant dependent variables identified in past work among PLWHA (e.g., Fiellin, McGinnis, Maisto, Justice, & Bryant, 2013; Surah et al., 2013) were evaluated: 1) hazardous drinking, 2) symptoms of alcohol dependence, 3) number of days consuming alcohol within the past month, and 4) past report of heavy episodic drinking. It was expected that such an effect of anxiety sensitivity via emotion dysregulation would be evident on all criterion measures over and above variance accounted for by the following covariates: gender, sexual orientation, time since HIV diagnosis, and presence of a substance use disorder. These covariates were selected as past work has shown significant associations of each with alcohol consumption (Conen et al., 2009; Marshal et al., 2008; Nolen-Hoeksema, 2004).
Figure 1.
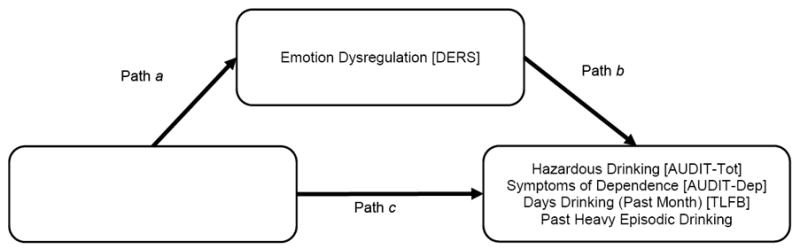
Proposed model examining the indirect effect of Anxiety Sensitivity on Alcohol Use criterion variables (AUDIT-Tot, AUDIT-Dep, TLFB, and Past Heavy Episodic Drinking) via Difficulties with Emotion Regulation.
2. Method
2.1 Participants
Participants included 129 adults living with HIV/AIDS recruited from AIDS service organizations in Houston, Texas. Flyers were placed in local community health clinics, and doctors’ offices as well as in newspaper/magazine advertisements and on webpage announcements (e.g., Craigslist.com). Further advertisement was conducted via public speaking engagements (e.g., Ryan White Foundation Houston, Houston AIDS Foundation) and word-of-mouth. Interested individuals contacted our clinic/research lab to schedule an appointment, completed confidentially (i.e., no identifying information on study materials). Participants were eligible for inclusion if they were at least 18 years old, were previously diagnosed with HIV/AIDS per self-report, and had the cognitive capacity to give written informed consent, as assessed by their ability to read the consent form and explain the study purpose to assessment personnel. Study measures were completed as part of a larger assessment battery. Participants were paid $20 in gift cards for completing a two-hour baseline assessment consisting of diagnostic interview and questionnaires.
Three participants were missing data on one or more measures of interest and were excluded from analyses yielded 126 individuals for the current study. The majority of participants (65.9%) were male and the mean age was 48.3 years (SD = 7.5). In terms of ethnicity, 55.1% of the sample identified as Black, 28.6% as White/Caucasian, 13.4% as Hispanic, and 4.5% identified as “mixed/other” (e.g., Native American). Regarding sexual orientation, 45.2% identified as heterosexual, 38.1% homosexual, 14.3% bisexual, and 2.4% ‘other’. Although 85.7% reported completion of high school or further education, 74.3% of participants reported current unemployment and 55.6% reported earning less than $10,000 annually. The average CD4 t-cell count within the sample was 567.3 (SD = 264.5; range: 28-1300); CD4 counts range from 500-1,200 in seronegative individuals with CD4 ≤200 contributing to a diagnosis of AIDS. Less than half (43.7%) self-reported diagnosis of AIDS. The majority of participants (87.3%) reported current use of anti-retroviral therapy (ART). Of those on ART, 78.2% reported having an undetectable viral load. The sample reported having a diagnosis of HIV for an average of 17.0 years (SD=8.6). The most common psychological diagnoses were generalized anxiety disorder (26.2%), major depressive disorder (24.3%), and (non-alcohol) substance use disorder (SUD; 22.2%).
2.2 Measures
2.2.1 MINI International Neuropsychiatric Interview
(MINI; Lecrubier et al., 1997). The MINI is a brief semi-structured diagnostic interview, which was developed in order to assess for the presence of current Axis I psychological disorders (e.g., anxiety, mood, substance-use, psychosis) based on DSM-IV criteria. The MINI has been utilized in prior studies examining HIV+ samples (e.g. Breuer et al., 2014) and has been deemed psychometrically sound (see Lecrubier et al., 1997). A subset of 12.5% of cases where checked for diagnostic reliability by a research staff member; no cases of disagreement were noted.
2.2.2 Anxiety Sensitivity Index-3
(ASI-3; Taylor et al., 2007). The ASI-3, derived in part from the original ASI, is an 18-item self-report measure of anxiety sensitivity (Reiss & McNally, 1985). Items (e.g., “When my stomach is upset, I worry that I might be seriously ill”) are rated on a scale from 0 (very little) to 4 (very much) and summed to a total score. The ASI-3 maintains strong psychometric properties (Farris et al., 2015; Taylor et al., 2007). ASI-3 scores in the current sample (M=26.06, SD=18.54) are similar to those in past studies among PLWHA (M=27.10, SD=26.21; Garey et al., 2015). In the current sample, internal consistency was excellent (α = .96) per commonly used interpretive range (i.e., ≥ 0.9; George & Mallery, 2003).
2.2.3 Difficulties in Emotion Regulation Scale
(DERS; Gratz & Roemer, 2004M). The DERS is a 36-item multidimensional self-report measure of emotion dysregulation. Participants rate each item (e.g., “I experience my emotions as overwhelming and out of control”) on a 5-point Likert scale ranging from 1 (almost never) to 5 (almost always) and summed to a total score. The DERS has demonstrated excellent psychometric properties including test-retest reliability, construct validity and predictive validity (Gratz & Roemer, 2004) and has been in samples of PLWHA (Brandt, Gonzalez, Grover, & Zvolensky, 2012). DERS scores in the current sample (M=88.22, SD=27.72) are similar to those in past studies among PLWHA (M=91.41, SD=26.21; Garey et al., 2015). Internal consistency was excellent in the current study (α = .95).
2.2.4 The Alcohol Use Disorders Identification Test
(AUDIT; Babor, Higgins-Biddle, Saunders, & Monteiro, 2001). The AUDIT is a 10-item self-report measure that was developed by the World Health Organization to assess problematic alcohol use (Babor et al., 2001). Items (e.g., “How often do you have a drink containing alcohol?”) are rated from 0 to 4 and summed to a total score. The AUDIT has strong psychometric properties, including reliability and validity (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). In addition to a total score (AUDIT-Tot), the three items targeting alcohol dependence (AUDIT-Dep; e.g., “How often during the last year have you needed a first drink in the morning to get yourself going after a heavy drinking session?”) are used to screen for problematic alcohol use. In the current study, AUDIT-Tot and AUDIT-Dep were used as criterion variables and had good internal consistencies among the current sample (α = .86, and .77, respectively), consistent with past work among PLWHA (Surah et al., 2013). Scores on the AUDIT-Tot (M=4.80, SD=6.28) in the current study are similar to those obtained in past work among PLWHA (median AUDIT-Tot score = 5; Surah et al., 2013), although many studies (e.g., Trillo et al., 2013; Woolf-King, Neilands, Dilworth, Carrico, & Johnson, 2014) have reported only AUDIT categories among PLWHA (e.g., abstainer, low-risk) and not average scores, highlighting a need for additional work in this area. In this sample, 20.6% met criteria for hazardous drinking on the AUDIT-Tot (total scores of 8 or greater for men/7 or greater for women; Conigrave, Hall, & Saunders, 1995).
2.2.5 Timeline Follow-back
(TLFB; Sobell & Sobell, 1995). The TLFB is a self-report measure that obtains day-by-day estimates of drinking for a designated period of time. The current study used the past 30-day TLFB, which assessed the number of days during which alcohol was consumed over that period. Individuals were presented with a calendar on which they write events, which then serve as memory prompts for estimating the days during which they consumed alcohol. The TLFB has been deemed a reliable measure of alcohol consumption with excellent temporal stability (Carey, Carey, Maisto, & Henson, 2004; Sobell, Sobell, Leo, & Cancilla, 1988) and has been used as a measure of alcohol consumption among PLWHA (Fiellin et al., 2013). Number of days drinking in the past 30 days in the current sample (M=4.72, SD=8.63, 15.73% of days) is consistent with past work using the 30-day TLFB among PLWHA (16.60% of days; Simpson, Xie, Blum, & Tucker, 2011).
2.2.6 Past Heavy Episodic Drinking
To approximate the degree past heavy episodic drinking, one item (“During the period in your life when you were drinking most heavily, how often did you have 6 [if you are a man] / 4 [if you are a woman] drinks on one occasion?”) was created. Participants provided a rating on a scale from 0 “never” to 4 “daily or almost daily”. While the cutoff of 5 or more drinks is commonly used to mark heavy episodic drinking, others (e.g., Mäkelä et al., 2001) have used the cutoff of 6 or more drinks in one occasion.
2.3 Data Analytic Strategy
Analyses were conducted using the PROCESS macro for SPSS 20 (Hayes, 2012), which calculates the indirect effect of a predictor (X) on an outcome (Y) via some mediating factor (M; West & Aiken, 1997). Effect sizes (κ2) were calculated for the indirect effects, following recommendations of Preacher and Kelly (2011). Bootstrapping with 10,000 re-samples with replacement was performed to obtain 95% confidence intervals. The association of anxiety sensitivity via emotion dysregulation was examined with four dependent variables: hazardous drinking (AUDIT-Tot), symptoms of alcohol dependence (AUDIT-Dep), number of days drinking in the past month (TLFB), and degree of past heavy episodic drinking. Covariates included gender, sexual orientation, time since diagnosis, and presence of an SUD. For each model, two planned comparison models were also evaluated. First, the predictor and mediating factor were reversed such that the effects of emotion dysregulation via anxiety sensitivity were evaluated. Next, the outcome and mediating factor were reversed to evaluate the possibility of anxiety sensitivity predicting emotion dysregulation via the alcohol-related variables. It was hypothesized that each of the comparison models would yield non-significant indirect effects, adding confidence to the focal models (Figure 1) testing effects of anxiety sensitivity via emotion dysregulation.
3. Results
Descriptive statistics and Pearson correlations are presented in Table 2. At the bivariate level, anxiety sensitivity was strongly associated with emotion dysregulation (r = .67; p < .001) and weakly with hazardous drinking (r = .19; p < .001). Emotion dysregulation was moderately associated with hazardous drinking (r = .28; p < .001) and symptoms of alcohol dependence (r = .26; p < .001). Data were normally distributed with skewness within acceptable range (0.2-2.0; George & Mallery, 2003).
Table 2.
Model Fit Statistics
| N = 126 Antecedent | Consequent
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mediator (M) DERS
|
Criterion AUDIT-Tot
|
|||||||||
| path | Coeff. | SE | t | p | path | Coeff. | SE | T | p | |
| ASI-3 | a | 0.98 | 0.10 | 9.70 | < .001 | c′ | 0.01 | 0.04 | 0.04 | .970 |
| DERS | - | - | - | - | - | b | 0.07 | 0.03 | 2.60 | .011 |
| Gender | 4.56 | 4.65 | 0.98 | .329 | 2.34 | 1.37 | 1.71 | .090 | ||
| Time since Dx | -0.01 | 0.02 | -0.77 | .442 | 0.01 | 0.01 | 1.28 | .204 | ||
| SO | 9.77 | 4.50 | 2.17 | .032 | -0.28 | 1.34 | -0.21 | .834 | ||
| SUD | 2.68 | 4.43 | 0.60 | .547 | 1.78 | 1.30 | 1.37 | .174 | ||
| constant | 57.55 | 7.45 | 7.72 | <.001 | -4.56 | 2.67 | -1.71 | .090 | ||
|
|
|
|||||||||
| R2 = .48 | R2 = .14 | |||||||||
| F(5, 120) = 22.21, p < .001 | F(6, 119) = 3.24, p = .006 | |||||||||
|
| ||||||||||
| N = 126 Antecedent | Consequent
|
|||||||||
| Mediator (M) DERS
|
Criterion AUDIT-Dep
|
|||||||||
| path | Coeff. | SE | t | p | path | Coeff. | SE | t | p | |
|
| ||||||||||
| ASI-3 | a | 0.98 | 0.10 | 9.70 | < .001 | c′ | -0.01 | 0.01 | -0.19 | .851 |
| DERS | - | - | - | - | - | b | 0.02 | 0.01 | 2.44 | .016 |
| Gender | 4.56 | 4.65 | 0.98 | .329 | 0.10 | 0.49 | 0.20 | .843 | ||
| Time since Dx | -0.01 | 0.02 | -0.77 | .442 | 0.01 | 0.01 | 1.53 | .130 | ||
| SO | 9.77 | 4.50 | 2.17 | .032 | -0.19 | 0.48 | -0.40 | .689 | ||
| SUD | 2.68 | 4.43 | 0.60 | .547 | 0.64 | 0.46 | 1.39 | .166 | ||
| constant | 57.55 | 7.45 | 7.72 | <.001 | -1.71 | 0.95 | -1.81 | .073 | ||
|
|
|
|||||||||
| R2 = .48 | R2 = .10 | |||||||||
| F(5, 120) = 22.21, p < .001 | F(6, 119) = 2.30, p = .039 | |||||||||
|
| ||||||||||
| N = 126 Antecedent | Consequent
|
|||||||||
| Mediator (M) DERS
|
Criterion TLFB
|
|||||||||
| path | Coeff. | SE | t | p | path | Coeff. | SE | t | p | |
|
| ||||||||||
| ASI-3 | a | 0.98 | 0.10 | 9.70 | < .001 | c′ | -0.05 | 0.05 | -0.96 | .340 |
| DERS | - | - | - | - | - | b | 0.08 | 0.04 | 2.25 | .026 |
| Gender | 4.56 | 4.65 | 0.98 | .329 | 3.38 | 1.84 | 1.84 | .069 | ||
| Time since Dx | -0.01 | 0.02 | -0.77 | .442 | 0.01 | 0.01 | 0.41 | .680 | ||
| SO | 9.77 | 4.50 | 2.17 | .032 | -4.18 | 1.81 | -2.31 | .023 | ||
| SUD | 2.68 | 4.43 | 0.60 | .547 | 2.03 | 1.75 | 1.16 | .248 | ||
| constant | 57.55 | 7.45 | 7.72 | <.001 | -2.50 | 3.60 | -0.70 | .488 | ||
|
|
|
|||||||||
| R2 = .48 | R2 = .17 | |||||||||
| F(5, 120) = 22.21, p < .001 | F(6, 119) = 4.16, p < .001 | |||||||||
|
| ||||||||||
| N = 86 Antecedent | Consequent
|
|||||||||
| Mediator (M) DERS
|
Criterion HED
|
|||||||||
| path | Coeff. | SE | t | p | path | Coeff. | SE | t | p | |
|
| ||||||||||
| ASI-3 | a | 0.89 | 0.12 | 7.64 | <.001 | c′ | -0.01 | .01 | -1.16 | .252 |
| DERS | - | - | - | - | - | b | 0.02 | .01 | 1.80 | .076 |
| Gender | 7.66 | 5.27 | 1.45 | .150 | 0.12 | 0.42 | 0.30 | .769 | ||
| Time since Dx | -0.01 | 0.02 | -0.20 | .843 | 0.01 | 0.01 | 0.40 | .693 | ||
| SO | 10.66 | 5.26 | 2.03 | .046 | -0.36 | 0.43 | -0.84 | .404 | ||
| SUD | 0.46 | 5.40 | 0.08 | .933 | 0.32 | 0.43 | 0.75 | .457 | ||
| constant | 57.03 | 8.60 | 6.63 | <.001 | 0.59 | 0.85 | 0.70 | .487 | ||
|
|
|
|||||||||
| R2 = .45 | R2 = .06 | |||||||||
| F(5, 80) = 13.03, p < .001 | F(6, 79) = 0.86, p = .530 | |||||||||
In the model of hazardous drinking (AUDIT-tot), there was a significant positive indirect effect of anxiety sensitivity via emotion dysregulation (unstandardized point estimate = .07, SE = .03, BC 95% CI: .02 to .14; direct effect of anxiety sensitivity controlling for emotion dysregulation = .01, SE = .04, t = 0.04; p = .970). The size of the indirect effect via emotion dysregulation was medium (completely standardized point estimate = .20, SE = .08, BC 95% CI: .05 to .36; κ2 = .14, SE = .06, BC 95% CI: .02 to .26). The first comparison model yielded non-significant indirect effect (emotion dysregulation as X, anxiety sensitivity as M, hazardous drinking as Y; unstandardized point estimate = .01, SE = .02, BC 95% CI: -.04 to .04); however, the second comparison model yielded a significant indirect effect (anxiety sensitivity as X, hazardous drinking as M, emotion dysregulation as Y; unstandardized point estimate = .05, SE = .04, BC 95% CI: .01 to .15).
In predicting symptoms of dependence (AUDIT-Dep) scores, there was a significant positive indirect effect of anxiety sensitivity via emotion dysregulation (unstandardized point estimate = .02, SE = .01, BC 95% CI: .01 to .05; direct effect of anxiety sensitivity controlling for emotion dysregulation = -.01, SE = .01, t = -0.19; p = .851). The size of the indirect effect via emotion dysregulation was medium (completely standardized point estimate = .19, SE = .07, BC 95% CI: .05 to .34; κ2 = .14, SE = .05, BC 95% CI: .03 to .24). Neither of the comparison models were significant (comparison model 1 [emotion dysregulation as X, anxiety sensitivity as M, symptoms of dependence as Y]: unstandardized point estimate = .01, SE = .01, BC 95% CI: -.02 to .01; comparison model 2 [anxiety sensitivity as X, symptoms of dependence as M, emotion dysregulation as Y]: unstandardized point estimate = .04, SE = .03, BC 95% CI: -.01 to .12).
There was a significant positive indirect effect of anxiety sensitivity via emotion dysregulation in predicting number of days drinking (TLFB; unstandardized point estimate = .08, SE = .04, BC 95% CI: .01 to .16; direct effect of anxiety sensitivity controlling for emotion dysregulation = -.05, SE = .05, t = -0.96, p = .340). The size of the indirect effect via emotion dysregulation was medium (completely standardized point estimate = .18, SE = .08, BC 95% CI: .03 to .34; κ2 = .09, SE = .06, BC 95% CI: .01 to .21). Neither of the comparison models were significant (comparison model 1 [emotion dysregulation as X, anxiety sensitivity as M, number of days drinking as Y]: unstandardized point estimate = -.02, SE = .02, BC 95% CI: -.07 to .03; comparison model 2 [anxiety sensitivity as X, number of days drinking as M, emotion dysregulation as Y]: unstandardized point estimate = .01, SE = .02, BC 95% CI: -.02 to .07).
For past heavy episodic drinking, there was a significant positive indirect effect of anxiety sensitivity via emotion dysregulation (unstandardized point estimate = .01, SE = .01, BC 95% CI: .01 to .03; direct effect of anxiety sensitivity controlling for emotion dysregulation = -.01, SE = .01, t = -1.16, p = .252). The size of the indirect effect via emotion dysregulation was medium (completely standardized point estimate = .17, SE = .09, BC 95% CI: .01 to .35; κ2 = .12, SE = .06, BC 95% CI: .01 to .24). Neither of the comparison models were significant (comparison model 1 [emotion dysregulation as X, anxiety sensitivity as M, heavy episodic drinking as Y]: unstandardized point estimate = -.01, SE = .01, BC 95% CI: -.02 to .01; comparison model 2 [anxiety sensitivity as X, heavy episodic drinking as M, emotion dysregulation as Y]: unstandardized point estimate = .01, SE = .03, BC 95% CI: -.06 to .06).1
4. Discussion
The current study examined the indirect effects of anxiety sensitivity via emotion dysregulation in predicting hazardous drinking, symptoms of alcohol dependence, past-month alcohol consumption, and degree of past heavy episodic drinking among a sample of PLWHA. As hypothesized, there were significant indirect effects of anxiety sensitivity via emotion dysregulation for four all models tested. The size of these effects were medium in each model κ2 = .09-.14), and evident over and above variance accounted for by the covariates (gender, sexual orientation, time since HIV diagnosis, and presence of an SUD). The lack of impact of SUD was surprising. Indeed, there were no bivariate correlations of SUD with any outcome, and SUD was not a significant covariate in any model tested. Thus, hazardous drinking appears to be present, and clinically significant, independent of SUD. Future work should follow up on the interplay of alcohol and other substance use in this population. As data were collected at one time point, competing models were run to examine potential model misspecification. For each hypothesized model (testing the indirect effect of anxiety sensitivity via emotion dysregulation), two competing models were run (i.e., eight total comparison models). The competing models yielded non-significant indirect effects in all but one case (i.e., confidence intervals for the indirect effect contained ‘0’), adding confidence to the hypothesized model testing the indirect association of anxiety sensitivity via emotion dysregulation. Overall, the regulation of emotions may represent an important intermediate variable linking catastrophic interpretation of physiological arousal (anxiety sensitivity) to hazardous alcohol use. Indeed, the present data suggest anxiety sensitivity may be related to emotion dysregulation, which, in turn, may affect hazardous drinking. Future longitudinal work is needed to further evaluate this model given the current cross-sectional findings.
Interestingly, the direct and total effects of anxiety sensitivity in predicting the alcohol-related outcomes were not statistically significant in any of the models, with the exception of a significant total effect for hazardous drinking (see Table 3). Additionally, there was one significant bivariate correlation (i.e., ASI-3 and AUDIT-Total), the association failed to maintain significance once covariates were entered. The lack of a consistent direct/total effect of anxiety sensitivity was unexpected given well-documented associations of elevated anxiety sensitivity and hazardous drinking among non-HIV samples (DeMartini & Carey, 2011). One possible explanation for this set of findings is that anxiety sensitivity may be more strongly associated with drinking motives (e.g., negative affect reduction) than with drinking behavior, although this remains to be empirically tested. These data suggest the association between anxiety sensitivity and hazardous drinking outcomes (particularly symptoms of dependence, past-month drinking, and heavy episodic drinking) may be more complex among PLWHA, with the current results suggesting an indirect association via emotion dysregulation.
Table 3.
Direct, indirect, and total unstandardized effects of anxiety sensitivity on hazardous drinking outcomes via difficulties in emotion regulation.
| Criterion | Effect of IV on M | Effect of M on DV | Direct effect | Indirect effect | Total effect | ||
|---|---|---|---|---|---|---|---|
| (a) | (b) | (c′) | (a × b) | 95% CI | (c) | 95% CI | |
| AUDIT-Tot | .98 | .07 | .01 | .07 | .02 - .14 | .07 | .01-.13 |
| AUDIT-Dep | .98 | .02 | -.01 | .02 | .01 - .05 | .02 | -.01-.04 |
| TLFB | .98 | .08 | -.05 | .08 | .01 - .16 | .03 | -.05-.11 |
| HED | .89 | .02 | -.01 | .01 | .01 - .03 | .01 | -.02-.02 |
The findings of the present study may potentially inform interventions for hazardous drinking among PLWHA. These results suggest that targeting and improving emotion dysregulation may have benefits in terms of addressing hazardous drinking. Such an approach would be consistent with intervention work on emotion dysregulation and alcohol use disorders among non-HIV samples (e.g., Berking et al., 2011). For example, changes in the use of maladaptive emotion regulation strategies over the course of treatment have been shown to predict changes in anxiety- and alcohol-related psychopathology in a sample with comorbid anxiety and alcohol use disorders (Conklin et al., 2015). Given that newer treatments directly targeting emotion regulation are mounting growing evidence in treating a range of emotional outcomes (Gratz, Weiss, & Tull, 2015), such treatments may serve as additional options for the treatment of hazardous drinking among PLWHA.
The current study has several limitations. First, due to the cross-sectional design of the study, temporal ordering cannot be elucidated. Attempts were made to examine alternative models, which were rejected, adding confidence to the findings, but future work utilizing a longitudinal design is required to determine temporal effects and rule out the possibility of alternative explanations (e.g., alcohol use leading to emotion dysregulation, and anxiety sensitivity, in turn). Second, method variance may have influenced the current findings. All measures, while validated, were completed via self-report. Thus, future work should consider multi-method assessment approaches to index the constructs of interest. Third, although the sample was diverse in terms of ethnicity, it was limited to an older adult, primarily male group of individuals living with HIV/AIDS who volunteered to participate in a study for monetary reward. Although men comprise a large percentage of the HIV/AIDS population (Vermund, 2014), future studies would benefit from examining more heterogeneous samples of persons with HIV/AIDS. Moreover, it may be advisable to offer other types of incentives instead of those that are financial in nature to ascertain whether there is any type of sampling bias. The current study was underpowered to test more complex interactions (e.g., gender by sexual orientation by substance user) and future work using large samples should replicate and extend the current findings to probe for such interactions. Relatedly, it is possible that clusters of individuals (e.g., with specific racial, gender, and sexual orientation identities with/without certain diagnoses) may demonstrate unique associations, as is the case in any diverse and heterogeneous sample. Nevertheless, bootstrapping with 10,000 resamples of the data was used to identify significant 95% confidence bands around the indirect effects, adding confidence to the findings. Finally, the study criterion variables were limited to numerous indices of hazardous drinking. Future work could potentially benefit by further extending the present work to other alcohol-related processes, such as motives and outcome expectancies for use. It also may be advisable to explore how anxiety sensitivity and emotion dysregulation relate to a broader array of alcohol-related impairment indices, such as quality of life.
Overall, the present study serves as an initial exploration into the association between anxiety sensitivity, emotion dysregulation, and hazardous drinking among PLWHA. There was consistent empirical evidence of indirect associations of anxiety sensitivity via emotion dysregulation. Accordingly, if replicated and extended using prospective designs, treatments for hazardous drinking may benefit from consideration of emotion regulation therapeutic tactics.
Supplementary Material
Table 1.
Zero-order correlations among study variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender a | - | -.56*** | .10 | -.10 | -.09 | .16 | .02 | .30** | .10 | -.09 | |
| 2. Sexual Orientation a | - | -.23* | .01 | .05 | -.09 | -.03 | -.31*** | -.11 | .18* | ||
| 3. Time since Diagnosis a | - | -.05 | -.18* | .07 | .09 | .07 | .07 | -.21* | |||
| 4. SUD a | - | .13 | .13 | .15 | .09 | .07 | .12 | ||||
| 5. ASI-3 b | - | .19* | .16 | .04 | .01 | .67*** | |||||
| 6. AUDIT-Tot c | - | .82*** | .36*** | .42*** | .28** | ||||||
| 7. AUDIT-Dep c | - | .26** | .34** | .26** | |||||||
| 8. TLFB c | - | .14 | .13 | ||||||||
| 9. HED c | - | .14 | |||||||||
| 10. DERS d | - | ||||||||||
|
| |||||||||||
| Descriptive Statistics | Mean (n) | 83 | 57 | 204.25 | 28 | 26.06 | 4.80 | 0.98 | 4.72 | 1.74 | 88.22 |
| SD (%) | 65.90 | 45.20 | 103.33 | 22.2 | 18.54 | 6.28 | 2.18 | 8.63 | 1.57 | 27.72 | |
Note: Gender = coded as Male = 1 and Female = 0, with descriptive statistics for number and percentage male; Sexual Orientation, coded as Heterosexual = 1 and Gay/Lesbian/Bisexual/Other = 0, with descriptive statistics for number and percentage heterosexual; Time since Diagnosis = time in months since diagnosed with HIV; SUD = Substance Use Disorder diagnosis, coded as yes = 1 and no = 0 with descriptive statistics for number and percentage with a diagnosis; ASI-3 = Anxiety Sensitivity Index-3; AUDIT-Tot= total scale score on the Alcohol Use Disorders Identification Test; AUDIT-Dep= Alcohol Use Disorders Identification Test, Dependence symptoms subscale; TLFB = Timeline Follow-Back, Number of Drinking Days (Past Month); HED = Past Heavy Episodic Drinking; DERS = Difficulties with Emotion Regulation Scale.
Covariates.
Predictor.
Outcome Variable.
Mediator.
p < .05.
p < .01.
p < .001.
Highlights.
Anxiety sensitivity (AS) is associated with hazardous drinking in seronegatives
Little is known about anxiety sensitivity among persons living with HIV/AIDS
Emotion dysregulation may underlie anxiety sensitivity and hazardous drinking
AS was indirectly associated with outcomes via emotion dysregulation
Acknowledgments
Role of Funding Sources
Funding for the study was from a pre-doctoral National Research Service Award from the National Institute of Mental Health (F31-099922) awarded to Charles P. Brandt and endowment awarded to Dr. Zvolensky.
Footnotes
Moderated mediation models were also tested using PROCESS. Separate analyses examined each covariate (gender, sexual orientation, time since HIV diagnosis, and presence of a substance use disorder) as moderators of the indirect association of anxiety sensitivity via emotion dysregulation on each of the four outcomes. There were significant indirect effects in males and females, for heterosexual and lesbian/gay/bisexual/other individuals, for those with high, average, and low time since diagnosis, and for those with and without SUD in all four models, respectively. Full results can be obtained by contacting the corresponding author.
Contributors: Mr. Brandt and Dr. Zvolensky designed the parent study and data collection. Mr. Paulus and Mr. Brandt conducted literature searches and provided summaries of previous research studies for the current paper. Mr. Paulus and Mr. Jardin, conducted the statistical analysis and wrote the first draft of the manuscript. All authors edited the manuscript and provided text used in the final draft. All authors have approved the final manuscript.
Conflict of Interest: This work has not been presented previously in any form. No authors have any conflicts of interests or financial disclosures to report. The study was approved by Institutional Review Board at the University of Houston. Informed written consent was obtained prior to initiating study procedures. No animals have been employed in this research.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ammassari A, Murri R, Pezzotti P, Trotta MP, Ravasio L, De Longis P, et al. AdICONA Study Group. Self-reported symptoms and medication side effects influence adherence to highly active antiretroviral therapy in persons with HIV infection. Journal of Acquired Immune Deficiency Syndromes (1999) 2001;28(5):445–449. doi: 10.1097/00042560-200112150-00006. [DOI] [PubMed] [Google Scholar]
- Arnsten JH, Demas PA, Farzadegan H, Grant RW, Gourevitch MN, Chang C-J, Schoenbaum EE, et al. Antiretroviral Therapy Adherence and Viral Suppression in HIV-Infected Drug Users: Comparison of Self-Report and Electronic Monitoring. Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of America. 2001;33(8):1417–1423. doi: 10.1086/323201. http://doi.org/10.1086/323201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. Geneva: World Health Organization, Department of Mental Health and Substance Dependence; 2001. [Google Scholar]
- Berking M, Margraf M, Ebert D, Wupperman P, Hofmann SG, Junghanns K. Deficits in emotion-regulation skills predict alcohol use during and after cognitive–behavioral therapy for alcohol dependence. Journal of Consulting and Clinical Psychology. 2011;79(3):307–318. doi: 10.1037/a0023421. http://doi.org/10.1037/a0023421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt CP, Gonzalez A, Grover KW, Zvolensky MJ. The Relation Between Emotional Dysregulation and Anxiety and Depressive Symptoms, Pain-Related Anxiety, and HIV-Symptom Distress Among Adults with HIV/AIDS. Journal of Psychopathology and Behavioral Assessment. 2012;35(2):197–204. http://doi.org/10.1007/s10862-012-9329-y. [Google Scholar]
- Breuer E, Stoloff K, Myer L, Seedat S, Stein DJ, Joska JA. The validity of the Substance Abuse and Mental Illness Symptom Screener (SAMISS) in people living with HIV/AIDS in primary HIV care in Cape Town, South Africa. AIDS and Behavior. 2014;18(6):1133–1141. doi: 10.1007/s10461-014-0698-y. http://doi.org/10.1007/s10461-014-0698-y. [DOI] [PubMed] [Google Scholar]
- Carey KB, Carey MP, Maisto SA, Henson JM. Temporal stability of the timeline followback interview for alcohol and drug use with psychiatric outpatients. Journal of Studies on Alcohol. 2004;65(6):774–781. doi: 10.15288/jsa.2004.65.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandley RB, Luebbe AM, Messman-Moore TL, Ward RM. Anxiety sensitivity, coping motives, emotion dysregulation, and alcohol-related outcomes in college women: A moderated-mediation model. Journal of Studies on Alcohol and Drugs. 2014;75(1):83–92. doi: 10.15288/jsad.2014.75.83. http://doi.org/10.15288/jsad.2014.75.83. [DOI] [PubMed] [Google Scholar]
- Conen A, Fehr J, Glass TR, Furrer H, Weber R, Vernazza P, et al. Swiss HIV Cohort Study. Self-reported alcohol consumption and its association with adherence and outcome of antiretroviral therapy in the Swiss HIV Cohort Study. Antiviral Therapy. 2009;14(3):349–357. [PubMed] [Google Scholar]
- Conigliaro J, Gordon AJ, McGinnis KA, Rabeneck L, Justice AC Veterans Aging Cohort 3-Site Study. How harmful is hazardous alcohol use and abuse in HIV infection: do health care providers know who is at risk? Journal of Acquired Immune Deficiency Syndromes (1999) 2003;33(4):521–525. doi: 10.1097/00126334-200308010-00014. [DOI] [PubMed] [Google Scholar]
- Conigliaro J, Justice AC, Gordon AJ, Bryant K VACS Alcohol and Behavior Change Research Group. Role of alcohol in determining human immunodeficiency virus (HIV)-relevant outcomes: A conceptual model to guide the implementation of evidence-based interventions into practice. Medical Care. 2006;44(8 Suppl 2):S1–6. doi: 10.1097/01.mlr.0000223659.36369.cf. http://doi.org/10.1097/01.mlr.0000223659.36369.cf. [DOI] [PubMed] [Google Scholar]
- Conigrave KM, Hall WD, Saunders JB. The AUDIT questionnaire: Choosing a cut-off score. Addiction. 1995;90(10):1349–1356. doi: 10.1046/j.1360-0443.1995.901013496.x. http://doi.org/10.1111/j.1360-0443.1995.tb03552.x. [DOI] [PubMed] [Google Scholar]
- Conklin LR, Cassiello-Robbins C, Brake CA, Sauer-Zavala S, Farchione TJ, Ciraulo DA, Barlow DH. Relationships among adaptive and maladaptive emotion regulation strategies and psychopathology during the treatment of comorbid anxiety and alcohol use disorders. Behaviour Research and Therapy. 2015;73:124–130. doi: 10.1016/j.brat.2015.08.001. http://doi.org/10.1016/j.brat.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrod PJ, Stewart SH, Pihl RO. Validation of a measure of excessive drinking: frequency per year that BAL exceeds 0.08% Substance Use & Misuse. 1997;32(5):587–607. doi: 10.3109/10826089709027314. [DOI] [PubMed] [Google Scholar]
- DeMartini KS, Carey KB. The role of anxiety sensitivity and drinking motives in predicting alcohol use: A critical review. Clinical Psychology Review. 2011;31(1):169–177. doi: 10.1016/j.cpr.2010.10.001. http://doi.org/10.1016/j.cpr.2010.10.001. [DOI] [PubMed] [Google Scholar]
- Dew BJ, Elifson KW, Sterk CE. Differences in HIV Sexual Risk Behaviors between Heterosexual and Nonheterosexual Male Users of Methamphetamine. Journal of Drug Issues. 2007;37(2):281–298. http://doi.org/10.1177/002204260703700203. [Google Scholar]
- Dew MA, Becker JT, Sanchez J, Caldararo R, Lopez OL, Wess J, Banks G, et al. Prevalence and predictors of depressive, anxiety and substance use disorders in HIV-infected and uninfected men: a longitudinal evaluation. Psychological Medicine. 1997;27(2):395–409. doi: 10.1017/s0033291796004552. [DOI] [PubMed] [Google Scholar]
- Dvorak RD, Sargent EM, Kilwein TM, Stevenson BL, Kuvaas NJ, Williams TJ. Alcohol use and alcohol-related consequences: Associations with emotion regulation difficulties. The American Journal of Drug and Alcohol Abuse. 2014;40(2):125–130. doi: 10.3109/00952990.2013.877920. http://doi.org/10.3109/00952990.2013.877920. [DOI] [PubMed] [Google Scholar]
- Ehrenstein V, Horton NJ, Samet JH. Inconsistent condom use among HIV-infected patients with alcohol problems. Drug and Alcohol Dependence. 2004;73(2):159–166. doi: 10.1016/j.drugalcdep.2003.10.011. http://doi.org/10.1016/j.drugalcdep.2003.10.011. [DOI] [PubMed] [Google Scholar]
- Farris SG, DiBello AM, Allan NP, Hogan J, Schmidt NB, Zvolensky MJ. Evaluation of the Anxiety Sensitivity Index-3 among treatment-seeking smokers. Psychological Assessment. 2015;27(3):1123–1128. doi: 10.1037/pas0000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, Fletcher DJ, Di Sclafani V. Effect of chronic alcohol abuse on the CNS morbidity of HIV disease. Alcoholism, Clinical and Experimental Research. 1998;22(5 Suppl):196S–200S. doi: 10.1111/j.1530-0277.1998.tb04000.x. [DOI] [PubMed] [Google Scholar]
- Ferrari LF, Levine JD. Alcohol consumption enhances antiretroviral painful peripheral neuropathy by mitochondrial mechanisms. The European Journal of Neuroscience. 2010;32(5):811–818. doi: 10.1111/j.1460-9568.2010.07355.x. http://doi.org/10.1111/j.1460-9568.2010.07355.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiellin DA, McGinnis KA, Maisto SA, Justice AC, Bryant K. Measuring alcohol consumption using timeline followback in non-treatment-seeking medical clinic patients with and without HIV infection: 7-, 14-, or 30-day recall. Journal of Studies on Alcohol and Drugs. 2013;74(3):500–504. doi: 10.15288/jsad.2013.74.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvan FH, Bing EG, Fleishman JA, London AS, Caetano R, Burnam MA, Shapiro M, et al. The prevalence of alcohol consumption and heavy drinking among people with HIV in the United States: results from the HIV Cost and Services Utilization Study. Journal of Studies on Alcohol. 2002;63(2):179–186. doi: 10.15288/jsa.2002.63.179. [DOI] [PubMed] [Google Scholar]
- Garey L, Bakhshaie J, Sharp C, Neighbors C, Zvolensky MJ, Gonzalez A. Anxiety, depression, and HIV symptoms among persons living with HIV/AIDS: The role of hazardous drinking. AIDS Care. 2015;27(1):80–85. doi: 10.1080/09540121.2014.956042. http://doi.org/10.1080/09540121.2014.956042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George D, Mallery M. SPSS for windows step by step: A simple study guide and reference, 17.0 update, 10/e. Pearson Education India; 2003. [Google Scholar]
- Gonzalez A, Barinas J, O’Cleirigh C. Substance use: impact on adherence and HIV medical treatment. Current HIV/AIDS Reports. 2011;8(4):223–234. doi: 10.1007/s11904-011-0093-5. http://doi.org/10.1007/s11904-011-0093-5. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. http://doi.org/10.1023/B:JOBA.0000007455.08539.94. [Google Scholar]
- Gratz KL, Weiss NH, Tull MT. Examining emotion regulation as an outcome, mechanism, or target of psychological treatments. Current Opinion in Psychology. 2015;3:85–90. doi: 10.1016/j.copsyc.2015.02.010. http://doi.org/10.1016/j.copsyc.2015.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modelling [White paper] 2012 [Google Scholar]
- Johnson KA, Farris SG, Schmidt NB, Zvolensky MJ. Anxiety sensitivity and cognitive-based smoking processes: Testing the mediating role of emotion dysregulation among treatment-seeking daily smokers. Journal of Addictive Diseases. 2012;31(2):143–157. doi: 10.1080/10550887.2012.665695. http://doi.org/10.1080/10550887.2012.665695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB, Zvolensky MJ, McLeish AC. Anxiety sensitivity and affect regulatory strategies: Individual and interactive risk factors for anxiety-related symptoms. Journal of Anxiety Disorders. 2008;22(3):429–440. doi: 10.1016/j.janxdis.2007.03.011. http://doi.org/10.1016/j.janxdis.2007.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleeberger CA, Phair JP, Strathdee SA, Detels R, Kingsley L, Jacobson LP. Determinants of heterogeneous adherence to HIV-antiretroviral therapies in the Multicenter AIDS Cohort Study. Journal of Acquired Immune Deficiency Syndromes (1999) 2001;26(1):82–92. doi: 10.1097/00126334-200101010-00012. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Thuras P, Abrams K, Brekke M, Stritar L. Anxiety mediates the association between anxiety sensitivity and coping-related drinking motives in alcoholism treatment patients. Addictive Behaviors. 2001;26(6):869–885. doi: 10.1016/s0306-4603(01)00240-4. [DOI] [PubMed] [Google Scholar]
- Lecrubier Y, Sheehan Dv, Weiller E, Amorim P, Bonora I, Sheehan KH, Dunbar GC, et al. The Mini International Neuropsychiatric Interview (MINI): A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry. 1997;12(5):224–231. http://doi.org/10.1016/S0924-9338(97)83296-8. [Google Scholar]
- Lewis BA, Vogeltanz-Holm ND. The effects of alcohol and anxiousness on physiological and subjective responses to a social stressor in women. Addictive Behaviors. 2002;27(4):529–545. doi: 10.1016/s0306-4603(01)00190-3. [DOI] [PubMed] [Google Scholar]
- Mäkelä P, Fonager K, Hibell B, Nordlund S, Sabroe S, Simpura J. Episodic heavy drinking in four Nordic countries: a comparative survey. Addiction. 2001;96(11):1575–1588. doi: 10.1080/09652140120080714. http://doi.org/10.1046/j.1360-0443.2001.961115755.x. [DOI] [PubMed] [Google Scholar]
- Marshal MP, Friedman MS, Stall R, King KM, Miles J, Gold MA, Morse JQ, et al. Sexual orientation and adolescent substance use: a meta-analysis and methodological review. Addiction (Abingdon, England) 2008;103(4):546–556. doi: 10.1111/j.1360-0443.2008.02149.x. http://doi.org/10.1111/j.1360-0443.2008.02149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naragon-Gainey K. Meta-analysis of the relations of anxiety sensitivity to the depressive and anxiety disorders. Psychological Bulletin. 2010;136(1):128–150. doi: 10.1037/a0018055. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clinical Psychology Review. 2004;24(8):981–1010. doi: 10.1016/j.cpr.2004.08.003. http://doi.org/10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. In: Reiss S, Bootsin RR, editors. Theoretical issues in behavior therapy. San Diego, CA: Academic Press; 1985. pp. 107–121. [Google Scholar]
- Samet JH, Horton NJ, Traphagen ET, Lyon SM, Freedberg KA. Alcohol Consumption and HIV Disease Progression: Are They Related? Alcoholism: Clinical and Experimental Research. 2003;27(5):862–867. doi: 10.1097/01.ALC.0000065438.80967.56. http://doi.org/10.1097/01.ALC.0000065438.80967.56. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction (Abingdon, England) 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Buckner JD, Keough ME. Anxiety sensitivity as a prospective predictor of alcohol use disorders. Behavior Modification. 2007;31(2):202–219. doi: 10.1177/0145445506297019. http://doi.org/10.1177/0145445506297019. [DOI] [PubMed] [Google Scholar]
- Schneider M, Chersich M, Neuman M, Parry C. Alcohol consumption and HIV/AIDS: the neglected interface. Addiction (Abingdon, England) 2012;107(8):1369–1371. doi: 10.1111/j.1360-0443.2012.03824.x. http://doi.org/10.1111/j.1360-0443.2012.03824.x. [DOI] [PubMed] [Google Scholar]
- Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal Considerations on Alcohol and HIV/AIDS — A Systematic Review. Alcohol and Alcoholism. 2010;45(2):159–166. doi: 10.1093/alcalc/agp091. http://doi.org/10.1093/alcalc/agp091. [DOI] [PubMed] [Google Scholar]
- Simpson CA, Xie L, Blum ER, Tucker JA. Agreement between prospective interactive voice response telephone reporting and structured recall reports of risk behaviors in rural substance users living with HIV/AIDS. Psychology of Addictive Behaviors. 2011;25(1):185–190. doi: 10.1037/a0022725. http://doi.org/10.1037/a0022725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol consumption measures. Assessing Alcohol Problems: A Guide for Clinicians and Researchers. 1995;4:55–76. [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: Assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. British Journal of Addiction. 1988;83(4):393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. http://doi.org/10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Stein M, Herman DS, Trisvan E, Pirraglia P, Engler P, Anderson BJ. Alcohol use and sexual risk behavior among human immunodeficiency virus-positive persons. Alcoholism, Clinical and Experimental Research. 2005;29(5):837–843. doi: 10.1097/01.alc.0000164363.40533.e0. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Peterson JB, Pihl RO. Anxiety sensitivity and self-reported alcohol consumption rates in university women. Journal of Anxiety Disorders. 1995;9(4):283–292. http://doi.org/10.1016/0887-6185(95)00009-D. [Google Scholar]
- Stewart SH, Samoluk SB, MacDonald AB. Anxiety sensitivity and substance use and abuse. In: Taylor S, editor. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers; 1999. pp. 287–319. [Google Scholar]
- Stewart SH, Zvolensky MJ, Eifert GH. Negative-reinforcement drinking motives mediate the relation between anxiety sensitivity and increased drinking behavior. Personality and Individual Differences. 2001;31(2):157–171. http://doi.org/10.1016/S0191-8869(00)00213. [Google Scholar]
- Surah S, Kieran J, O’Dea S, Shiel C, Raffee S, Mulcahy F, Lyons F, et al. Use of the Alcohol Use Disorders Identification Test (AUDIT) to determine the prevalence of alcohol misuse among HIV-infected individuals. International Journal of STD & AIDS. 2013;24(7):517–521. doi: 10.1177/0956462412473885. http://doi.org/10.1177/0956462412473885. [DOI] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Cardenas SJ, et al. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19(2):176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Trillo AD, Merchant RC, Baird JR, Ladd GT, Tao Liu, Nirenberg TD. Interrelationship of alcohol misuse, HIV sexual risk and HIV screening uptake among emergency department patients. BMC Emergency Medicine. 2013;13(1):1–14. doi: 10.1186/1471-227X-13-9. http://doi.org/10.1186/1471-227X-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Aldao A. Editorial overview: New directions in the science of emotion regulation. Current Opinion in Psychology. 2015;3:iv–x. http://doi.org/10.1016/j.copsyc.2015.03.009. [Google Scholar]
- Vermund SH. Global HIV Epidemiology: A Guide for Strategies in Prevention and Care. Current HIV/AIDS Reports. 2014;11(2):93–98. doi: 10.1007/s11904-014-0208-x. http://doi.org/10.1007/s11904-014-0208-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidrine DJ, Marks RM, Arduino RC, Gritz ER. Efficacy of Cell Phone Delivered Smoking Cessation Counseling for Persons Living With HIV/AIDS: 3-Month Outcomes. Nicotine & Tobacco Research. 2012;14(1):106–110. doi: 10.1093/ntr/ntr121. http://doi.org/10.1093/ntr/ntr121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West SG, Aiken LS. Toward understanding individual effects in multicomponent prevention programs: Design and analysis strategies. In: Bryant KJ, Windle M, West SG, editors. The science of prevention: Methodological advances from alcohol and substance abuse research. Washington, DC, US: American Psychological Association; 1997. pp. 167–209. [Google Scholar]
- Woolf-King SE, Neilands TB, Dilworth SE, Carrico AW, Johnson MO. Alcohol use and HIV disease management: The impact of individual and partner-level alcohol use among HIV-positive men who have sex with men. AIDS Care. 2014;26(6):702–708. doi: 10.1080/09540121.2013.855302. http://doi.org/10.1080/09540121.2013.855302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization [WHO] Lexicon of alcohol and drug terms published by the World Health Organization. 2015 Retrieved from http://www.who.int/substance_abuse/terminology/who_lexicon/en/
- Zack M, Poulos CX, Aramakis VB, Khamba BK, MacLeod CM. Effects of drink-stress sequence and gender on alcohol stress response dampening in high and low anxiety sensitive drinkers. Alcoholism, Clinical and Experimental Research. 2007;31(3):411–422. doi: 10.1111/j.1530-0277.2006.00322.x. http://doi.org/10.1111/j.1530-0277.2006.00322.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


