Abstract
Purpose
Despite the importance of timely evaluation for patients with brachial plexus injuries (BPI), in clinical practice we have noted delays in referral. Because the published BPI experience is largely from individual centers, we used a population-based approach to evaluate the delivery of care for patients with BPI.
Methods
We used statewide administrative databases from Florida (2007–2013), New York (2008–2012) and North Carolina (2009–2010) to create a cohort of patients who underwent surgery for BPI (exploration, repair, neurolysis, grafting, or nerve transfer). Emergency department and inpatient records were used to determine the time interval between the injury and surgical treatment. The distances between the treating hospitals and between the patient’s home ZIP code and the surgical hospital were recorded. A multivariable logistic regression model was used to determine predictors for time from injury to surgery exceeding 365 days.
Results
Within the 222 patients in our cohort, the median time from injury to surgery was 7.6 months and exceeded 365 days in 29% of cases. Treatment at a smaller hospital for the initial injury was significantly associated with surgery beyond 365 days after injury. Patient insurance type, travel distance for surgery, the distance between the two treating hospitals, or changing hospitals between injury and surgery did not significantly influence time to surgery.
Conclusions
Nearly one-third of patients in FL, NY, and NC underwent BPI surgery more than one year after their injury. Patients initially treated at smaller hospitals are at risk for undergoing delayed BPI surgery.
Clinical Relevance
These findings can inform administrative and policy efforts to expedite timely referral of patients with BPI to experienced centers.
INTRODUCTION
Although there is no current consensus on the optimal timing of surgical intervention after brachial plexus injuries (BPI), it is generally agreed that delay beyond 6 to 12 months compromises the feasibility and functional outcome of nerve reconstruction procedures [1–4]. Given the more favorable improvements in strength, function, and pain relief noted with earlier treatment [5], delays in referral and treatment are suboptimal for both the patient and surgeon.
While most patients with BPI receive their definitive surgical treatment at academic tertiary care centers, details of the referral patterns for patients with BPI in the United States have not been extensively studied. As with many subspecialized surgical procedures, it is possible that patients are traveling substantial distances to receive care for BPI. In consideration of previous studies that demonstrated an association between traveling to an academic referral center for subspecialty care and postoperative complications, the expected benefits gained by traveling to receive specialized care must be balanced against the potential risks associated with doing so [6].
To better understand potential reasons for delays in referral and to gain a better appreciation of the distances traveled by patients, we used a population-based approach to evaluate delivery of care for patients undergoing outpatient brachial plexus exploration, repair, decompression, or neurolysis. We asked the following research questions:
What is the time interval between traumatic injury and surgical treatment of BPI?
Does patient travel distance influence timing of surgery for BPI?
MATERIALS AND METHODS
Data Sources and Cohort Assembly
We used Healthcare Cost and Utilization Project (HCUP) statewide administrative databases from, Florida (2005–2013), New York (2006–2012) and North Carolina (2007–2010). These states and specific timeframes were selected based on the availability and completeness of data from the requisite datasets. For each of these states, we accessed the State Inpatient Databases (SID), State Ambulatory Surgery and Services Databases (SASD), and State Emergency Department Databases (SEDD). The SID contain records from hospital admissions (with procedures identified via ICD-9-CM codes only), the SASD contain records from outpatient surgery (with procedures identified via CPT-4 codes only), and the SEDD contain billing records from emergency department encounters that do not result in hospital admission. We queried the SASD and SID using three approaches in order to identify patients undergoing surgery for BPI:
SASD query using CPT-4 procedure codes to identify patients at least 18 years of age who underwent surgical treatment of BPI coded as brachial plexus suture (CPT-4 64861) and brachial plexus neuroplasty (CPT-4 64713: exploration, neurolysis, or nerve decompression) as an ambulatory/outpatient surgery.
SASD query for patients at least 18 years of age who had an associated ICD-9-CM diagnosis code of brachial plexus injury (953.4,) and undergoing a procedure with a CPT-4 code for neuroplasty, nerve repair, nerve grafting, or nerve transfer (Appendix 1: List of diagnosis and procedure codes used for identification of patients to include in the study cohort).
SID query for patients at least 18 years of age who had an associated ICD-9-CM diagnosis code of brachial plexus injury (953.4) and undergoing a procedure with a ICD-9-CM procedure code for neurolysis, peripheral nerve decompression, peripheral nerve graft, nerve transplantation, nerve repair, or neuroplasty (Appendix 1). CPT-4 codes are not available in SID.
In each of these databases, there is a unique identifier for each patient that allows linkage across the individual state’s databases. Patients cannot be tracked across different states.
In order to allow evaluation of 2 years of preceding SID and SEDD data for hospitalizations or emergency department visits, we identified patients who underwent surgery from SASD and SID records. The date of surgery (defined by the procedure date corresponding to the relevant CPT-4 code) was included. Using an unique personal identifier, we searched the SID and SEDD for any hospitalizations or emergency department visits by the patient within 2 years preceding the identified BPI surgery. ICD-9-CM diagnosis codes and “E codes” (for external causes of injury) from a prior hospitalization or emergency department visit were used to identify corresponding injuries (Appendix 2: List of unique diagnosis included as injury codes in the study cohort). These diagnosis codes from the “injury” event were collated and reviewed by a fellowship-trained orthopaedic hand surgeon (XXX) to determine appropriateness for inclusion in the study cohort. The date of injury was recorded from the admission date of the “injury” event, using the E code as the injury date if both types of codes were present. Only those patients in whom we were able to identify both surgery and injury dates and we could identify an attributable injury mechanism were included in this study. This cohort does not include patients who may have had injuries that were not followed by a hospitalization or emergency room visit (for example, an iatrogenic brachial plexus injury following a shoulder arthroplasty).
Additional Data Considerations
Only state residents were included, as out-of-state residents who underwent surgery could have been treated originally or followed-up after surgery at an out-of-state hospital. Free functioning muscle transfers or tendon transfers were also not included in this study. Our data collection and analysis using de-identified administrative data sources received an exemption from review by our institutional review board.
Variables
Based on the event dates, we calculated the number of calendar days between the injury and surgical intervention (“time to surgery”), which was our outcome measure. We analyzed patient age, sex, race (categorized as white or non-white), payer (insurance type: private, Medicare, Medicaid, other/none), hospital identifier, and ZIP code of patient residence from the data entry related to the surgery record. We also analyzed payer (insurance type) and the hospital identifier from the injury encounter prior to the surgery. We determined the location type (urban or non-urban) and number of inpatient beds for both the hospital where BPI surgery was done (“surgery hospital”) and the hospital where the patient’s initial injury was treated (“injury hospital”), if different, by linking the data to the American Hospital Association Annual Survey. Number of inpatient beds was converted to a categorical variable, with hospitals placed into one of the following groups: ≤200 beds, 201–400 beds, 401–600 beds, and ≥600 beds. Hospital identifier information was retained in order to determine if patients followed-up for surgery at the same hospital where they were treated for their injury and to determine the characteristics of the hospitals involved. Comorbidities were identified from the list of diagnosis codes in the Elixhauser index [7], which uses ICD-9 diagnosis codes to summarize the comorbidity burden of each patient. This index was developed specifically for use with administrative data [7], with a recent systematic review demonstrating acceptable-to-excellent predictive ability for in-patient mortality [8]. We calculated the straight-line distance in miles between the center of the patient’s ZIP code and the center of the ZIP code of the hospital where they underwent surgery (“patient travel distance”). We used US Census data to determine characteristics of the patient’s community based on ZIP code: median household income (national quartile) and location of residence (urban or non-urban).
Statistical Analysis
The number of days from injury to surgery was calculated for each patient. Patients who underwent BPI surgery >365 days after their injury date were compared to those who underwent surgery ≤365 days from their injury date using univariate statistics (t-test for continuous variables, chi-square test for categorical variables, or non-parametric equivalents if data were not normally distributed as determined by the Jarque-Bera test [9]. We constructed a multivariable logistic regression model with time to surgery more than 365 days as the dependent variable. Potential independent variables were evaluated in simple logistic regression models to determine suitability for inclusion as covariates in the regression model. Variables with p-values < 0.20 were entered in a forward stepwise manner into the multivariable logistic regression model. Only those variables that retained a p-value <0.05 in the model were included in the final model. All variables included in the final model were tested for two-way interactions. The two-way interactions were added to the model if statistically significant. Potentially multicollinearity among predictor variables was evaluated using univariate statistics (t-tests, correlation, chi-square tests, or their non-parametric equivalents, as described above) to evaluate their independence from one another; any variables that exhibited potential multi-collinearity were removed from the regression model.
RESULTS
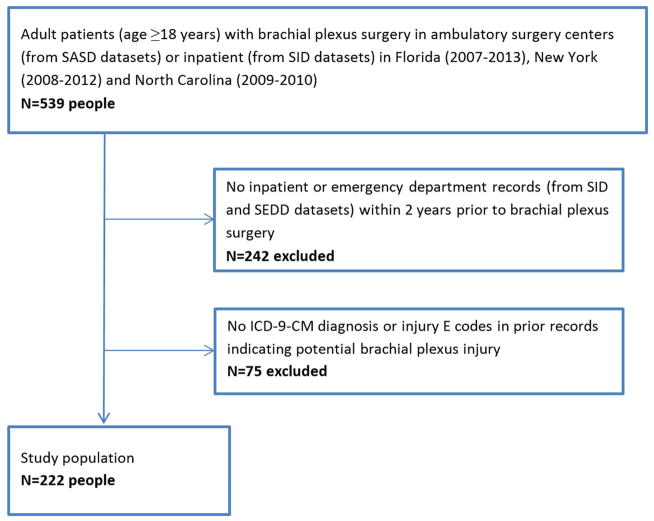
We identified 539 patients from the SID and SASD who had brachial plexus exploration, repair, decompression, or neurolysis. Of these 539 patients, 297 had an SID or SEDD record within the prior 2 years. We were able to identify an injury mechanism in a total of 222 patients – this comprised the cohort of patients included in this study (Figure 1). The median age was 42 years (minimum 18 years, maximum 86 years; interquartile range 28 to 53 years) and 62% were male (Table 1). The median time from injury to surgery was 229 days (7.6 months; min 2 days, max 730 days; interquartile range 130 days to 423 days). Time from injury to surgery exceeded 365 days in 29% of cases. There was no difference in timing of surgery, patient characteristics, or hospital characteristics among the three different states included.
Figure 1.
Flow chart for selection of study population
Table 1.
Demographics of patients included in study (n=222 except where noted)
| Patient demographics and characteristics | |
|
| |
| Age (years) | 42.9 ± 16.6 |
|
| |
| Sex | |
| Male | 137 (62%) |
| Female | 85 (38%) |
| Missing | ** |
|
| |
| Race | |
| White | 142 (69%) |
| Black | 27 (13%) |
| Hispanic | 24 (12%) |
| Other | 12 (5%) |
| Missing | 17 |
|
| |
| Payer | |
| Medicaid | 27 (12%) |
| Medicare | 42 (18%) |
| Private (commercial) | 105 (47%) |
| Other (self-pay, uninsured, no charge, workman’s compensation) | 49 (22%) |
|
| |
| Comorbidities | |
| 0 | 84 (55%) |
| 1 | 30 (19%) |
| 2+ | 40 (26%) |
| Missing | 68 |
|
| |
| Changed insurance type between injury and BPI surgery | 51 (23%) |
|
| |
| Changed hospitals between injury and BPI surgery | 157 (71%) |
|
| |
| Patient travel distance (miles; n=199 patients) | Mean: 42.4± 62.4 |
| Median: 16.5 | |
| Min: 0 | |
| Max: 322 | |
|
| |
| Hospital characteristics (n=222 patients) | |
|
| |
| Injury hospital | |
| Location (urban vs rural; n/% urban) | 194 (88%) |
| Teaching status (n/% % teaching) | 111 (50%) |
| Bed size (n/% % >400 beds) | 115 (52%) |
|
| |
| BPI surgery hospital | |
| Location (urban vs rural; n/% % urban) | 178 (89%) |
| Teaching status (n/% % teaching) | 145 (73%) |
| Bed size (n/% % >400 beds) | 98 (49%) |
|
| |
| Patient community characteristics | |
|
| |
| Median household income of patient’s ZIP code (national quartile) | |
| 1st | 57 (26%) |
| 2nd | 53 (24%) |
| 3rd | 54 (25%) |
| 4th | 54 (25%) |
| Missing | ** |
|
| |
| Residence Location | |
| Urban | 174 (81%) |
| Large rural town | 11 (5%) |
| Small rural town | 17 (8%) |
| Isolated rural | 14 (6%) |
| Missing | ** |
Values less than 11 cannot be reported per HCUP Data Use Agreement.
The results of the simple regression models used to determine suitability for entry into the multivariable model are listed in Table 2; with the exception of patient sex, there was no statistically significant association between patient demographic characteristics (including insurance status) and time from injury to surgery >365 days. Number of inpatient beds at the initial/injury hospital were significantly associated with time from surgery to injury >365 days (Table 2). Variables with p<0.20 were included in the multivariable logistic regression model. In the multivariable logistic regression model, time to surgery >365 days was associated with hospital size for the initial/injury treatment (≤200 beds: odds ratio (95% confidence interval) 5.18 [2.21, 12.13]; 201–400 beds: 4.01 [1.63, 9.91], 401–600 beds: 1.56 [0.56, 4.35]; reference group ≥600 beds). Patient sex and age were included in the multivariable model, but their coefficients did not meet statistical significance.
Table 2.
Results of simple logistic regression models used to evaluate suitability of potential independent variables for multivariable regression modeling; includes full study cohort.
| Patient demographics and characteristics (n=222 patients) | Odds Ratio for probability of > 365 days from injury to surgery (95% confidence interval) |
|---|---|
| Age (years divided by 10) | 1.15 (0.97,1.37) |
|
| |
| Sex (female) | 2.00 (1.11,3.59) |
|
| |
| Race (white) | 1.30 (0.71,2.40) |
|
| |
| Payer (at initial injury) | |
| Medicaid | 1.32 (0.47,3.73) |
| Medicare | 1.35 (0.63,2.93) |
| Private (commercial) | 0.63 (0.35,1.13) |
|
| |
| Payer (at time of brachial plexus surgery) | |
| Medicaid | 0.99 (0.41,2.40) |
| Medicare | 1.91 (0.95,3.85) |
| Private (commercial) | 0.58 (0.32,1.04) |
|
| |
| Hospital characteristics (n=222 patients) | |
|
| |
| Injury hospital | |
| Location (urban) | 0.47 (0.21,1.07) |
| Teaching status (teaching) | 0.32 (0.17,0.59) |
| Bed size* | |
| <= 200 beds | 5.80 (2.52,13.36) |
| 201–400 beds | 4.27 (1.72,10.43) |
| 401–600 beds | 1.55 (0.56,4.30) |
|
| |
| BPI surgery hospital | |
| Location (urban) | 0.25 (0.10,0.64) |
| Teaching status (teaching) | 0.29 (0.15,0.57) |
| Bed size* | |
| <= 200 beds | 1.88 (0.85,4.15) |
| 201–400 beds | 1.10 (0.50,2.43) |
| 401–600 beds | 2.04 (0.70,6.01) |
Comparison group is > 600 beds
The median distance from the patient’s home ZIP code to the surgical hospital was 16.5 miles (interquartile range: 8.0, 44.2; Table 2), with 22% and 14% of patients traveling more than 50 miles and 100 miles for surgery, respectively. There was no difference in time-to-surgery when comparing patients based on a 50 mile threshold (p=0.92; Wilcoxon rank sum test) or a 100 mile threshold (p=0.83; Wilcoxon rank sum test).
DISCUSSION
The subspecialized nature of care for brachial plexus injuries can create challenges in delivering efficient and timely treatment. Our population-based evaluation demonstrated at least a 12 month time interval between injury and surgery in 29% of patients who underwent BPI surgery in Florida, New York, and North Carolina. Median times to surgery in case series at two individual centers in the United States were reported as 9 months and 12 months [10,11]. However, both series included patients who underwent free functional muscle transfers, which can be performed at a later time interval than brachial plexus exploration. In our series, which included only those patients coded for nerve reconstruction procedures (and not free functional muscle transfers), the median time to surgery was 7.6 months. These findings are sobering given that nerve reconstruction surgery more than 6 months after injury is considered as “delayed” and more than 12 months after injury is considered as “late” [1–4]. Due to the fact that our study is based on three states within the United States, it is difficult to know whether delays of this magnitude are experienced in other areas of the United States or in other countries.
Our findings support prior calls to improve accessibility of care for BPI patients [10]. We found that treatment of the original injury in a smaller hospital was associated with a greater likelihood of having surgery more than one year of the injury. Smaller hospitals may be staffed by with physicians who are not as familiar with BPI prognosis and treatment options, and as a result these patients may encounter difficulty in receiving detailed and accurate information [10]. Based on these findings, outreach and education efforts by BPI treatment teams are necessary to improve communication and education of potential referring providers at surrounding smaller and rural hospitals. We are also working to improve the accessibility of information to patients, regarding the importance of timing in evaluation and surgery.
Lack of familiarity with BPI among clinicians at smaller hospitals may be associated with delays in referral to BPI specialists at other hospitals, but this would be largely dependent on the smaller hospital’s referral networks. The increasing consolidation of individual hospitals into health systems within the United States may change the utilization patterns for patients with BPI, as rapid referrals from smaller hospitals to tertiary care centers may become more readily available. Alternatively, other motives to keep patients within a closed health system/referral network (as suggested by the experience with replantation in the United States [12]) may influence patients’ access to subspecialty surgeons who perform BPI surgery. We agree with Franzblau et al in calling for the development of clinical pathways to improve coordination of BPI referral among all hospitals [10], and are currently working with our hospital system’s leadership to develop this type of regional pathway. Because it is likely that BPI surgery in the United States is largely performed at large, academic hospitals, we are hoping to develop a resource that will help direct and/or coordinate referral of patients to centers within their geographic regions that perform BPI. We did not find an increased risk of delayed surgery based on patient travel distance, demonstrating that timely referral of patients to other centers successfully occurred in our sample. However, the states included in our studies may have different densities of health care providers (both in general and for BPI surgeons) than other states, which may explain the relatively short travel distances seen in our study. Lastly, it is important to note that delays to surgery occurred throughout the sample (and not only among patients transferred from smaller hospitals). This suggests that delays in treatment may occur even after referral to the treating hospital, which represents an opportunity for improvement in the delivery of expedient care for patients with BPI.
The current study carries limitations inherent to studies that rely on administrative datasets. More than half of the identified with BPI did not have an injury record (from an emergency room or inpatient hospitalization) that was detectable using our methodology. While these inclusion criteria were used to allow the identification of an injury event that could be linked to the subsequent BPI surgery for analysis of utilization patterns, only 222 patients met these criteria (of the 539 patients who had BPI surgery in these 3 states during the study period). Exclusion of the remaining 59% of patients leaves our results subject to selection bias and limited generalizability to all patients with BPI, as our findings may only be relevant to those patients with BPI who are first seen in an emergency room or hospitalized for their injury. Additionally, the demographics (age and sex) of our study population (62% male, median age 42 years) are substantially different from those typically associated with BPI (young men – 89% male and mean age 29 years in Midha’s single-center series [13]). This may be the result of selection bias associated with assembly of the study cohort. These demographic differences may also limit the generalizability of our findings. Furthermore, we identified injury hospitalizations and ED visits based on review of administrative claims, rather than review of medical records. We carefully reviewed the associated diagnosis codes for all hospitalizations within 2 years prior to the brachial plexus surgery to optimize the chances of accurately matching injury hospitalizations to the brachial plexus injury. Despite these efforts, diagnosis codes for the mechanism of injury (derived from ICD-9-CM codes and “E” codes for external causes of injury) may be inaccurate, unreliable, and/or incomplete, which can lead to a mischaracterization of the timing and nature of the injury hospitalization. Another limitation of using administrative data from individual states is the inability to evaluate patients who receive care across state lines, which may occur in densely populated areas near state borders. We attempted to minimize this influence by only including state residents in our study, but these exclusions also limit the generalizability of our findings especially as it relates to patient travel. Additionally, our study does not include clinical data regarding the manner and timing in which patients sought care for their BPI or the decision-making by the surgeon and patient for the BPI. While we recognize that these factors may greatly influence the overall path to surgery for each patient, we cannot capture these characteristics using administrative data. Lastly, we have incorporated data on delivery of care from multiple centers in three geographically and demographically diverse states. The population density and population demographics of these states are not necessarily reflective of the United States as a whole, thus further potentially limiting the generalizability of our findings. Improved coordination of care and consideration of regionalized referral networks (such as those being considered for total joint arthroplasty [14] and replantation [15]) for patients with BPI are necessary to provide optimal clinical outcomes for these patients.
Acknowledgments
This publication was made possible by Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 (CJD and DAO), Sub award KL2 TR000450 (DAO) from the NIH-National Center for Advancing Translational Sciences (NCATS), components of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. The Center for Administrative Data Research is supported in part by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH), Grant Number R24 HS19455 through the Agency for Healthcare Research and Quality (AHRQ), and Grant Number KM1CA156708 through the National Cancer Institute (NCI) at the National Institutes of Health (NIH). This publication’s contents are solely the responsibility of the authors and do not necessarily represent the official view of NCATS, ARHQ, NCI, or NIH.
Appendix 1: List of diagnosis and procedure codes used for identification of patients to include in the study cohort
| CPT-4 Procedure Codes | 64713 | Neuroplasty, major peripheral nerve, arm or leg; brachial plexus |
| 64861 | Suture of brachial plexus | |
| 64708* | Neuroplasty, major peripheral nerve, arm or leg; other than specified | |
| 64856* | Suture of major peripheral nerve, arm or leg, except sciatic; including transposition | |
| 64857* | Suture of major peripheral nerve, arm or leg, except sciatic; without transposition | |
| 64859* | Suture of each additional major peripheral nerve | |
| 64872* | Suture of nerve; requiring secondary or delayed suture | |
| 64874* | Suture of nerve; requiring extensive mobilization, or transposition of nerve | |
| 64876* | Suture of nerve; requiring shortening of bone of extremity | |
| 64892* | Nerve graft (includes obtaining graft), single strand, arm or leg; up to 4 cm length | |
| 64893* | Nerve graft (includes obtaining graft), single strand, arm or leg; more than 4 cm length | |
| 64897* | Nerve graft (includes obtaining graft), multiple strands (cable), arm or leg; up to 4 cm length | |
| 64898* | Nerve graft (includes obtaining graft), multiple strands (cable), arm or leg; more than 4 cm length | |
| 64901* | Nerve graft, each additional nerve; single strand | |
| 64902* | Nerve graft, each additional nerve; multiple strands | |
| 64905* | Nerve pedicle transfer; first stage | |
| 64907* | Nerve pedicle transfer; second stage | |
| ICD-9-CM Procedure Codes | 03.6* | Lysis of adhesions of spinal cord and nerve roots |
| 04.49* | Other peripheral nerve or ganglion decompression or lysis of adhesions, peripheral nerve neurolysis NOS | |
| 04.5* | cranial or peripheral nerve graft | |
| 04.6* | transposition of cranial and peripheral nerves, nerve transplantation | |
| 04.74* | Other anastomosis of cranial or peripheral nerve | |
| 04.76* | Repair of old traumatic injury of cranial and peripheral nerves | |
| 04.79 * | Other neuroplasty |
Included in study cohort only if ICD-9-CM diagnosis code 953.4 (brachial plexus injury) is included within same record as the procedure code
Appendix 2: Unique ICD-9-CM diagnosis codes and E codes (supplementary classification of external causes of injury) included in the “injury” record for the study cohort
| 337.2 | Reflex sympathetic dystrophy |
| 338.19 | Acute pain |
| 353.0 | Brachial plexus lesions |
| 354.0 | Carpal tunnel syndrome |
| 354.8 | Mononeuritis |
| 355.9 | Mononeuritis |
| 356.9 | Idiopathic peripheral neuropathy |
| 718.91 | Joint derangement shoulder |
| 719.02 | Joint effusion upper arm |
| 719.41 | Joint pain – shoulder |
| 719.42 | Joint pain – upper arm |
| 721.0 | Cervical spondylosis |
| 721.8 | Spinal disorder NOS |
| 722.0 | Cervical disc displacement |
| 722.71 | Cervical disc disease with myelopathy |
| 723.1 | Cervicalgia |
| 723.4 | Brachial neuritis |
| 729.5 | Pain in limb |
| E003.1 | Activities involving ice hockey |
| E006 | Activities involving other sports and athletics played individually |
| E008.1 | Activities involving wrestling |
| E017.9 | Activities involving roller coasters and other types of external motion |
| E029.9 | Other activity |
| E030 | Unspecific activity |
| E812 | Other motor vehicle traffic accident involving collision with motor vehicle |
| E813 | Motor vehicle traffic accident involving collision with other vehicle |
| E814 | Motor vehicle traffic accident involving collision with pedestrian |
| E815 | Other motor vehicle traffic accident involving collision on the highway |
| E816 | Motor vehicle traffic accident due to loss of control without collision on the highway |
| E818 | Other noncollision motor vehicle traffic accident |
| E819 | Motor vehicle traffic accident of unspecified nature |
| E820 | Nontraffic accident involving motor-driven snow vehicle |
| E821 | Nontraffic accident involving other off-road motor vehicle |
| E823 | Other motor vehicle nontraffic accident involving collision with stationary object |
| E824 | Other motor vehicle nontraffic accident while boarding and alighting |
| E826 | Pedal cycle accident |
| E870 | Accidental cut puncture perforation or hemorrhage during medical care |
| E878 | Surgical operation and other surgical procedures as the cause of abnormal reaction of patient or of later complication without mention of misadventure at the time of operation |
| E879 | Other procedures without mention of misadventure at the time of procedure as the cause of abnormal reaction of patient or of later complication |
| E880 | Accidental fall on or from stairs or steps |
| E881 | Accidental fall on or from ladders or scaffolding |
| E882 | Accidental fall from or out of building or other structure |
| E884 | Other accidental falls from one level to another |
| E885 | Accidental fall on same level from slipping tripping or stumbling |
| E888 | Other and unspecified fall |
| E892 | Conflagration not in building or structure |
| E897 | Accident caused by controlled fire not in building or structure |
| E899 | Accident caused by unspecified fire |
| E908 | Accident due to cataclysmic storms and floods resulting from storms |
| E916 | Struck By Falling Object |
| E917 | Striking against or struck accidentally by objects or persons |
| E918 | Caught accidentally in or between objects |
| E920 | Accidents caused by cutting and piercing instruments or objects |
| E924 | Accident caused by hot substance or object caustic or corrosive material and steam |
| E925 | Accident caused by electric current |
| E927 | Overexertion and strenuous movements |
| E928 | Other and unspecified environmental and accidental causes |
| E929 | Late effects of accidental injury |
| E956 | Suicide and self-inflicted injury by cutting and piercing instrument |
| E960 | Fight brawl rape |
| E963 | Assault by hanging and strangulation |
| E965 | Assault by firearms and explosives |
| E966 | Assault by cutting and piercing instrument |
| E968 | Assault by other and unspecified means |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jack Baty, Email: jack@wustl.edu.
Mohammed J Saeed, Email: msaeed@DOM.wustl.edu.
Margaret A. Olsen, Email: MOLSEN@DOM.wustl.edu.
Daniel A. Osei, Email: oseid@wudosis.wustl.edu.
References
- 1.Shin AY, Spinner RJ, Steinmann SP, Bishop AT. Adult traumatic brachial plexus injuries. J Am Acad Orthop Surg. 2005;13(6):382–396. doi: 10.5435/00124635-200510000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Giuffre JL, Kakar S, Bishop AT, Spinner RJ, Shin AY. Current concepts of the treatment of adult brachial plexus injuries. J Hand Surg. 2010;35A(4):678–88. doi: 10.1016/j.jhsa.2010.01.021. quiz 688. [DOI] [PubMed] [Google Scholar]
- 3.Birch R. Timing of surgical reconstruction for closed traumatic injury to the supraclavicular brachial plexus. J Hand Surg. 2015;40E(6):562–567. doi: 10.1177/1753193414539865. [DOI] [PubMed] [Google Scholar]
- 4.Hems TE. Timing of surgical reconstruction for closed traumatic injury to the supraclavicular brachial plexus. J Hand Surg. 2015;40E(6):568–572. doi: 10.1177/1753193414540074. [DOI] [PubMed] [Google Scholar]
- 5.Kato N, Htut M, Taggart M, Carlstedt T, Birch R. The effects of operative delay on the relief of neuropathic pain after injury to the brachial plexus: a review of 148 cases. J Bone Joint Surg. 2006;88B(6):756–759. doi: 10.1302/0301-620X.88B6.16995. [DOI] [PubMed] [Google Scholar]
- 6.Etzioni DA, Fowl RJ, Wasif N, Donohue JH, Cima RR. Distance bias and surgical outcomes. Med Care. 2013;51(3):238–244. doi: 10.1097/MLR.0b013e318270bbfa. [DOI] [PubMed] [Google Scholar]
- 7.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Yurkovich M, Avina-Zubieta JA, Thomas J, Gorenchtein M, Lacaille D. A systematic review identifies valid comorbidity indices derived from administrative health data. J Clin Epidemiol. 2015 Jan;68(1):3–14. doi: 10.1016/j.jclinepi.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 9.Jarque CM, Bera AK. A Test for Normality of Observations and Regression Residuals. International Statistical Review. 1987 Aug;55(2):164–172. doi: 10.2307/1403192. [DOI] [Google Scholar]
- 10.Franzblau LE, Maynard M, Chung KC, Yang LJ. Medical treatment decision making after total avulsion brachial plexus injury: a qualitative study. J Neurosurg. 2015;122(6):1413–1420. doi: 10.3171/2015.2.JNS132686. [DOI] [PubMed] [Google Scholar]
- 11.Barrie KA, Steinmann SP, Shin AY, Spinner RJ, Bishop AT. Gracilis free muscle transfer for restoration of function after complete brachial plexus avulsion. Neurosurg Focus. 2004;16(5):E8. doi: 10.3171/foc.2004.16.5.9. [DOI] [PubMed] [Google Scholar]
- 12.Hustedt JW, Bohl DD, Champagne L. The Detrimental Effect of Decentralization in Digital Replantation in the United States: 15 Years of Evidence From the National Inpatient Sample. J Hand Surg. 2016 May;41A(5):593–601. doi: 10.1016/j.jhsa.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 13.Midha R. Epidemiology of brachial plexus injuries in a multitrauma population. Neurosurgery. 1997 Jun;40(6):1182–8. doi: 10.1097/00006123-199706000-00014. discussion 1188–9. [DOI] [PubMed] [Google Scholar]
- 14.Dy CJ, Marx RG, Ghomrawi HM, Pan TJ, Westrich GH, Lyman S. The potential influence of regionalization strategies on delivery of care for elective total joint arthroplasty. J Arthroplasty. 2015;30(1):1–6. doi: 10.1016/j.arth.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 15.Peterson BC, Mangiapani D, Kellogg R, Leversedge FJ. Hand and microvascular replantation call availability study: a national real-time survey of level-I and level-II trauma centers. J Bone Joint Surg. 2012A;94(24):e185. doi: 10.2106/JBJS.K.01167. [DOI] [PubMed] [Google Scholar]