Abstract
We investigated the gastrointestinal colonization rate and antibiotic resistance patterns of Extended-Spectrum Beta-Lactamase (ESBL)- producing Escherichia coli and Klebsiella pneumoniae in hospitalized patients admitted at Ethiopia’s largest tertiary hospital. Fecal samples/swabs from 267 patients were cultured on chrome agar. ESBL. Bacterial species identification, verification of ESBL production and antibiotic susceptibility testing were done using Vitek 2 system (bioMérieux, France). Phenotype characterization of ESBL-E.coli and ESBL- K.pneumoniae was done using Neo-Sensitabs™. ESBL positivity rate was much higher in K. pneumoniae (76%) than E. coli (45%). The overall gastrointestinal colonization rate of ESBL producing Enterobacteriaceae (ESBL-E) in hospitalized patients was 52% (95%CI; 46%–58%) of which, ESBL-E. coli and K.pneumoniae accounted for 68% and 32% respectively. Fecal ESBL-E carriage rate in neonates, children and adults was 74%, 59% and 46% respectively. Gastrointestinal colonization rate of ESBL-E.coli in neonates, children and adults was 11%, 42% and 42% respectively. Of all E. coli strains isolated from adults, children and neonates, 44%, 49% and 22% were ESBL positive (p = 0.28). The prevalence of ESBL-K.pneumoniae carriage in neonates, children and adults was 68%, 22% and 7% respectively. All K. pneumoniae isolated from neonates (100%) and 88% of K. pneumoniae isolated from children were ESBL positive, but only 50% of K.pneumoniae isolated from adults were ESBL positive (p = 0.001). Thirteen patients (5%) were carriers of both ESBL-E.coli and ESBL-KP. The overall carrier rate of ESBL producing isolates resistant to carbapenem was 2% (5/267), all detected in children; three with E.coli HL cephalosporinase (AmpC), resistant to ertapenem and two with K. pneumoniae Carbapenemase (KPC) resistant to meropenem, ertapenem and impenem. We report a high gastrointestinal colonization rate with ESBL-E and the emergence of carbapenems-resistant K. pneumoniae in Ethiopia. Urgent implementation of infection control measures, and surveillance are urgently needed to limit the spread within healthcare facilities and further to the community.
Introduction
Antimicrobial resistance (AMR) in healthcare facilities is a global public health problem causing prolonged hospital stay, high cost of therapy and increased mortality [1]. Mobility of people, contaminated food and animals are main factors in the globalization of public health threats including spreading of resistant organisms [2]. Most importantly international travel, particularly to Africa, India and south East Asia appears to be a risk factor for colonization with ESBL-producing E. coli [3–5]. Although AMR is a global problem`, the impact is higher in Sub-Saharan Africa (SSA) due to limited available resources for healthcare infrastructure and wide irrational use of antimicrobial agents. Of all those who take antibiotics`, more than one-third do not get prescriptions from a doctor`, and about a quarter obtain antibiotics from an informal dispenser [6]. Although AMR is a global problem, the impact is higher in Sub-Saharan Africa (SSA) due to limited available resources for healthcare infrastructure and wide irrational use of antimicrobial agents. Of all those who take antibiotics, more than one-third do not get prescriptions from a doctor, and about a quarter obtain antibiotics from an informal dispenser [6]
ESBL-producing Enterobacteriaceae (ESBL-E), particularly Escherichia coli (ESBL-E.coli) and Klebsiella pneumoniae (ESBL-KP) are of major concerns due to concomitant multidrug resistance. The recent WHO report on AMR global surveillance indicate very high rates of resistant bacteria that cause common health-care associated and community-acquired infections worldwide [1]. The burden of ESBL-E and their respective antimicrobial resistance patterns are intensively studied in developed countries. However, data on the colonization rate with ESBL producing isolates, particularly on antibacterial resistance from developing countries particularly from sub Saharan Africa is yet limited mainly due to resource constrains [1, 7]. Available reports indicate that ESBL-producing Enterobacteriaceae in hospital and community settings in Africa is common, and the reported colonization rates as well as the resistance pattern vary between different countries with in the continent [8–12]. Considering the limited diagnostic and treatment possibilities in resource-poor countries, reliable surveillance data on antibacterial resistance in different African countries including Ethiopia is urgently required to raise awareness, map the burden and the resistance pattern for effective intervention measures, treatment recommendations and to identify emerging threats.
Transmission of antimicrobial resistant pathogens in healthcare facilities from former patients, visitors and healthcare providers may lead to outbreaks and spread to the community. In Ethiopia, initial studies reported high prevalence of hospital-acquired infections manly due to multi drug resistant pathogens at the countries’ largest tertiary referral Hospital [13, 14]. Majority of the isolated bacteria were gram-negative mostly resistant to the commonly used antimicrobials. Later a high level (63%) of hospital acquired multi-drug resistant bacterial infection was detected for many years [15]. Indeed, in the same hospital where we performed the current study and other hospitals in Ethiopia, infection outbreaks including neonatal sepsis due to multi-drug resistant bacteria, particularly in the neonatal units with a high mortality rate (41%) has been reported [16–18].
Surveillance and antimicrobial resistance data on ESBL-E is imperative, particularly in hospital environment to identify and prevent outbreaks. Furthermore the emergence and spread of carbapenem-resistant ESBL-E has become a growing threat globally and data from sub-Saharan Africa countries, including Ethiopia is lacking [1, 19, 20]. The objectives of this cross-sectional point prevalence study were, therefore, i) to investigate the gastrointestinal colonization rates and risk factors for ESBL producing Enterobacteriaceae in hospitalized patients ii) to identify the antimicrobial resistance profile of ESBL producing and non-ESBL producing E.coli and Klebsiella species iii) to perform phenotype characterization of ESBL producing Enterobacteriaceae strains particularly E. coli and K. pneumoniae in patients admitted at Ethiopia’s largest tertiary referral Hospital.
Methods
Study Design and Population
This cross-sectional descriptive point surveillance study was conducted during December 2012 at Tikur Anbessa Specialized Hospital (TASH), a 500-bed tertiary university teaching Hospital in Addis Ababa, Ethiopia. TASH is the biggest teaching University affiliated Hospital in Ethiopia, where patients from different parts of the country are refereed for further management. The Hospital provides service to both outpatients and inpatients admitted to medical, surgical, obstetric & gynecologic, orthopedic, neonatal and pediatric wards. All available in patient wards, including neonatal and ICUs as well as acute care wards and emergency clinics, where patients were admitted for ≥ 48 hours were eligible for study ward inclusion.
Inclusion criteria for study participants were; all hospitalized patients including neonates (newborn infants under 28 days of age), infants, children and adult patients who were admitted for ≥ 48 hours. Patients undergoing same day treatment or surgery during the survey date, patients seen at the outpatient department, patients in the emergency room monitored for < 48 hours, patients in long-term care wards and nursing homes were excluded.
The study protocol, including the consent procedure, received ethics approval from Institutional Review Boards (IRBs) of the College of Health Sciences, Addis Ababa University and Karolinska Institutet in Stockholm, Sweden. Written informed consent was obtained from both adult study participants as well as from parents or guardians on the behalf of the children and newborn infants who participated in the study. The study was conducted as per guidelines laid in the International Conference of Harmonization for Good Clinical Practice.
ESBL Identification and Antimicrobial Susceptibility Testing
A single fecal sample/swab was collected from 267 hospitalized patients who were hospital admitted for ≥ 48 hours. All samples were cultured on CHROMagar™ ESBL (CHROMagar, Paris, France). Bacterial identification and antibiotic susceptibility testing were performed using the Vitek-2 system (bioMérieux, France). Susceptibility testing for 16 antimicrobials, namely ceftazidime (CAZ), cefotaxime (CTX), ciprofloxacin (CIP), cephalexin (CN), amoxicillin/clavulanic acid (AMC), amikacin (AN), aztreonam (ATM), ertapenem (ETP), cefoxitin (FOX), gentamicin (GM), imipenem (IPM), meropenem (MEM), tigecycline (TGC), tobramycin (TM), trimethoprim (TMP), piperacillin/tazobactam (TZP), was performed by using VITEK-2 AST card (AST-N218), which also has screening for ESBL. Interpretation of AST result was done according to EUCAST guidelines. E.coli ATCC 25922 and K. pneumoniae ATCC 700603 were used for quality control.
Phenotype Characterization
Phenotypic characterization and categorization of ESBL positive E. coli and K. pneumoniae—was done using Neo-Sensitabs™ (Rosco, Denmark) according to the user′s guide. Briefly, Mueller Hinton agar plates were inoculated with a 0.5 McFarland adjusted suspension in 0.9% NaCl, streaked with cotton swabs using a plate rotator (bioMérieux S.A., Marcy l′Etoile, France), and incubated overnight at 35°C for 16–18 h. Differences in zones of inhibitions between a β-lactam alone compared with the combination with a β-lactamase inhibitor, as well as subjective synergy observations were determined for all ESBL positive isolates from Vitek-2 characterized Enterobacteriaceae strains.
All ESBL positive isolates resistant to CTX and CAZ were tested for ESBLA- using cefotaxime (CTX30), cefotaxime + clavulanic acid (CTX+C), ceftazidime (CAZ30) and ceftazidime + clavulanic acid (CAZ + CL). All ESBL positive isolates resistant to CTX or CAZ and FOX were tested for ESBLM–test, AmpC (Neo-Sensitabs confirm ID KIT ROSC98007) containing cefotaxime (CTX30), cefotaxime + cloxacillin (CTXCX), ceftazidime (CAZ30) and ceftazidime + cloxacillin (CAZCX).
The detection of putative carbapenemase production was first based on an initial phenotypic screen for carbapenem resistance, followed by the phenotypic characterization using ROSCO Neo-Sensitabs as a confirmatory test (Neo-Sensitabs confirm ID KIT ROSC98006), which consists of Meropenem (MRP10), Meropenem + Dipicolinic acid (MRPDP), Meropenem + Boronic acid (MRPBO) and Meropenem + cloxacillin (MRPCX). K. pneumoniae CCUG 56233, K. pneumoniae CCUG 56233 and K. pneumoniae CCUG 58547 were used as positive control strains for AmpC and porin loss, K. pneumoniae carbapenemase (KPC) and Metallo-β-lactamase (MBL) respectively. K. pneumoniae ATCC 25955 was used as negative control in all phenotype tests.
Statistical Analyses
Multidrug resistance (MDR) in Enterobacteriaceae were defined as non-susceptible to ≥1 agent in >3 antimicrobial categories as listed by the international expert proposal for interim standard definitions [21]. Prevalence of ESBL producing isolates along with the corresponding 95% CI stratified by age group is presented by calculating frequencies and percentages. Chi-square test was used with appropriate correction for the observation. Pearson Correlations test and logistic regression analysis were used to identify risk factors for colonization by ESBL-E. Statistical analyses were performed using SPSS Statistics (IBM Corporation, Somers, NY) software, version 22.0. P values < 0.05 were considered to be statistically significant.
Results
All adults, children and neonatal (newborn infants under 28 days of age) patients hospitalized at TASH (n = 398) during 10–20 December 2012 was approached to participate in this study. A total of 347 hospitalized patients fulfilled the study inclusion criteria, of which 267 patients (77%; 128 women and 139 men) who were willing to participate and able to provide fecal sample or rectal swab were enrolled. There were 154 adults (age span = 14 to 75 years old, median = 35 years, inter quartile range = 26 to 50 years), 94 children (age span = 1 month to 12 years old, median = 7 years, inter quartile range = 2 to 8 years old) and 19 neonates (age span 3 to 23 days; median = 9 days, inter quartile range = 4 to 13 days).
A total of 295 E.coli and Klebsiella species were isolated from 267 fecal samples. E.coli was the most common gram-negative organism identified (n = 235, 79.7%) followed by K.pneumoniae (n = 58, 19.7%) and K.oxytoca (n = 2, 0.7%). Of all ESBL-E isolates, 151 (51.2%) were ESBL positive, of which 70.2% (n = 106) were E.coli, 29.1% (n = 44) were K.pneumoniae and 0.7% (n = 1) were K. oxytoca.
Out of the total 235 E. coli strains isolated from fecal samples, 106 (45%) of them were ESBL-producing E. coli (95% CI = 39%–56%). Of all E. coli strains isolated from adults and children, 44% (65/147) and 49% (39/79) respectively were ESBL ESBL-producing E. coli. In contrast only 22% (2/9) of E. coli strains isolated from neonates were ESBL-producing E. coli (p = 0.28). On the other hand the distribution of ESBL-producing KP among the different age groups was quite different from what was observed for ESBL-producing E. coli. The overall prevalence of ESBL positivity among the 58 K. pneumoniae isolates was 75.9% (44/58), 95% CI = 63.6%-85.6%. All K. pneumoniae isolated from neonates (100%, 12/12) and 88% (21/24) of K. pneumoniae isolated from children were ESBL producing K.pneumoniae, but in adults only 50% (11/22) of K.pneumoniae were ESBL producing K.pneumoniae (p = 0.001).
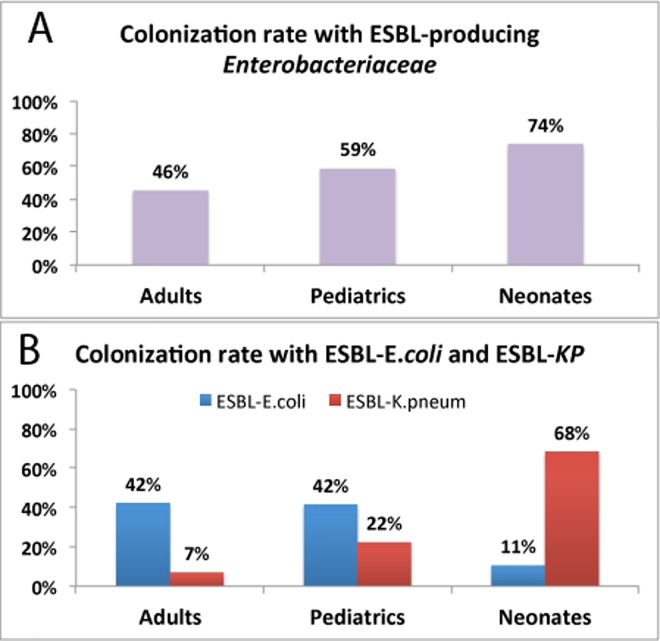
One hundred thirty-nine patients (52.1%; 95% CI = 46.1%–58.0%) out of 267 were carrier of ESBL producing Enterobacteriaceae. Comparison of rates of total ESBL producing isolates (positive for ESBL producing E.coli or K. pneumoniae) among adult, children and neonates is presented in Table 1 and Fig 1A. Out of the 139 patients, who were tested positive for ESBL-E, 95 of them (68.3%; 95% CI = 60.6%–76.0%) were colonized by ESBL-E. coli, 43 (31.0%; 95% CI = 23.3%–38.7%) by ESBL-K. pneumoniae, and 1 (0.4%) by ESBL-K. oxytoca. Prevalence of colonization with ESBL-E was significantly (p = 0.02) higher in neonates (74%) followed by children (59%) than in adults (46%). Logistic regression analysis indicted that having lower age as a significant risk factor for colonization by ESBL-E (p = 0.02). Neonates (p = 0.02, odds ratio = 3.360, 95% CI for odds ratio = 1.153 to 6.788) and children (p = 0.047, odds ratio = 1.692, 95% CI for odds ratio = 1.008 to 2.843) had a higher risk for being colonized by ESBL-E compared to adult patients.
Table 1. Gastrointestinal colonization rate of ESBL positive (ESBL+ve) and negative (ESBL-ve) isolates in hospitalized patients and stratified by patient age group, at Tikur Anbessa Specialized hospital, December 2012.
| Organism | ESBL positivity | All (n = 267) | Patient age group | p value | ||
|---|---|---|---|---|---|---|
| Adult (n = 154) | Children (n = 94) | Neonates (n = 19) | ||||
| Total | ESBL -ve | 128 (47.9%) | 84 (54.5%) | 39 (41.5%) | 5 (26.3%) | 0.02 |
| ESBL +ve | 139 (52.1%) | 70 (45.5%) | 55 (58.5%) | 14 (73.7%) | ||
| E. coli | ESBL -ve | 161 (60.3%) | 89 (57.8%) | 55 (58.5%) | 17 (89.5%) | 0.026 |
| ESBL +ve | 106 (39.7%) | 65 (42.2%) | 39 (41.5%) | 2 (10.5%) | ||
| K. pneumoniae | ESBL -ve | 222 (83.1%) | 143 (92.9.0%) | 73 (77.7%) | 6 (31.6%) | < 0.0001 |
| ESBL +ve | 45 (16.9%) | 11 (7.1%) | 21 (22.3%) | 13 (68.4%) | ||
Fig 1.
Colonization rate of ESBL producing Enterobacteriaceae (Top) and distribution of ESBL positive E. coli and K. pneumonia (bottom) in fecal samples collected from 267 hospitalized patients (154 adults, 94 children and 19 neonates). Thirteen out of 267 patients (5%) were carriers of both ESBL producing K.pneumoniae and E. coli (7 adults, 5 children and 1 neonates).
Fecal colonization rate of ESBL producing Enterobacteriaceae in hospitalized patients stratified by ward specialty is presented in Table 2. Gastrointestinal colonization rates by ESBL-E were much higher for patients admitted at intensive care unit, medical and emergency wards. There was a significant positive correlations of high colonization rates by ESBL-E with higher maximum bed capacity per room and increasing number of patients admitted in single room and (Pearson Correlations test p < 0.0001). Having more than two patients in a single room was a significant risk factor for being colonized by ESBL-E (p < 0.0001, odds ratio = 4.017, 95% CI for odds ratio = 2.255 to 5.348).
Table 2. Fecal colonization rate of ESBL producing Enterobacteriaceae in hospitalized patients stratified by ward specialty during December 2012 at Tikur Anbessa Specialized Hospital in Addis Ababa, Ethiopia.
| Patents age group | Ward specialty | ESBL producing Enterobacteriaceae | |||
|---|---|---|---|---|---|
| Negative | Positive | ||||
| N | % | N | % | ||
| Adult | Emergency | 0 | 0.0% | 2 | 100.0% |
| Gynecology & obstetrics | 27 | 79.4% | 7 | 20.6% | |
| Medical general | 16 | 30.2% | 37 | 69.8% | |
| Medical ICU | 0 | 0.0% | 1 | 100.0% | |
| Orthopedics | 11 | 42.3% | 15 | 57.7% | |
| Oncology | 12 | 85.7% | 2 | 14.3% | |
| Surgery | 18 | 75.0% | 6 | 25.0% | |
| Neonates | Neonates | 5 | 26.3% | 14 | 73.7% |
| Pediatrics | Emergency | 7 | 31.8% | 15 | 68.2% |
| ICU | 0 | 0.0% | 2 | 100.0% | |
| Medical general | 10 | 23.8% | 32 | 76.2 | |
| Surgical | 22 | 78.6% | 6 | 21.4% | |
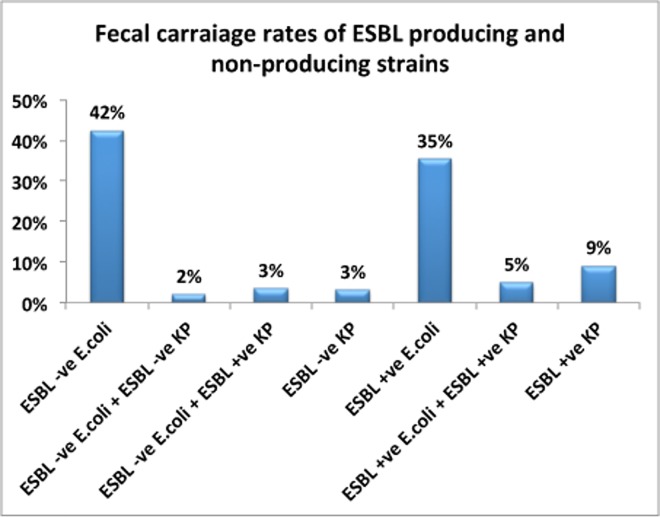
The overall prevalence of colonization by ESBL positive E.coli (ESBL-E.coli) among 267 hospitalized patients was 40% (95% CI = 34.1%–45.9% whereas 45 patients (17%; 95% CI = 12.5%–21.5%) were carriers of ESBL-K.pneumoniae (p < 0.0001). There was a significant difference between age groups and type of ESBL producing strains (Fig 1B). Colonization with ESBL-E.coli was more common in adults (42%) and children (42%) than neonates (11%). In contrast, colonization with ESBL positive K. pneumoniae (ESBL-KP) was much higher (p < 0.0001) in neonates (68%) than in children (22%) or adults (7%). All Klebsiella species isolated from neonates were ESBL positive. Where as 64% and 50% of all Klebsiella species isolated from children and adults were ESBL positive respectively. Distribution of gastrointestinal E. coli and K.pneumoniae carriage rates stratified by presence and or absence of ESBL producing isolates in all hospitalized patients is presented in Fig 2. Twenty-eight patients (10%) were carriers of both E. coli and K. pneumoniae, and 13 patients (5%) were carriers of both ESBL positive K. pneumoniae and ESBL-E.coli (seven adults, five children and one neonate).
Fig 2. Distribution of gastrointestinal colonization rates of E. coli and K.pneumoniae stratified by presence (+ve) and or absence (-ve) of ESBL producing isolates in all hospitalized patients (n = 267).
Antimicrobial Susceptibility of ESBL-E.coli and K.pneumoniae
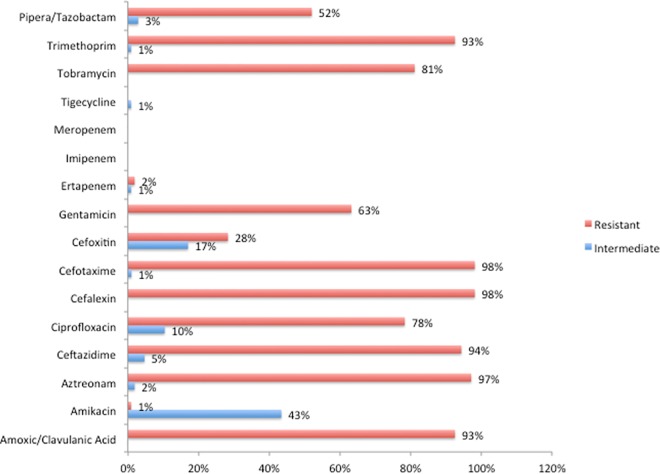
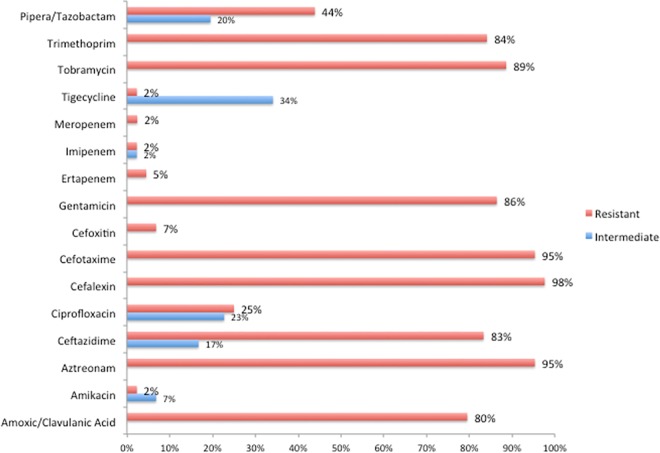
Fig 3 shows the antimicrobial resistance pattern for ESBL positive (n = 106) E.coli isolates. All ESBL-E.coli were 100% sensitive to meropenem and imipenem, while 3% were resistant or intermediate resistant to ertapenem. Non-ESBL producing E. coli strains were more often resistant to amoxicillin/clavulanic acid, trimethoprim, and piperacillin/tazobactam. The highest resistance in ESBL negative isolates was seen for TMP (38%), amoxicillin/clavulanic acid (17%), and 12% were resistant to both drugs. All ESBL-E. coli were MDR but only 2% (4 out of the 175) of the non-ESBL-E.coli (n = 129; p < 0.0001). Fig 4 shows the comparison of antimicrobial resistance pattern for ESBL positive K. pneumoniae. All non-ESBL producing K. pneumoniae isolates were sensitive to all antimicrobial tested for, while all ESBL-KP were MDR (p < 0.0001).
Fig 3. Antimicrobial resistance pattern of ESBL producing (n = 106) E.coli strains isolated from hospitalized patients fecal samples/swab.
The over all prevalence of ESBL positivity among the 235 E.coli isolates was 45.1% (106/235).
Fig 4. Antimicrobial resistance pattern of ESBL positive (n = 44) K.pneumoniae strains isolated from hospitalized patients fecal samples/swab.
The prevalence of ESBL positivity among the 58 K.pneumoniae isolates was 76% (44/58).
Prevalence of ESBL Producing and Carbapenem Resistant Enterobacteriaceae
Five children (1.9%, 5/267) were colonized with ESBL positive and carbapenem resistant Enterobacteriaceae (ESBL-CARBA). Two children were colonized by ESBL and carbapenemase producing K. pneumoniae (KPC) with MBL+KPC: One child was colonized by ESBL producing K. pneumoniae isolate resistant to all antibiotics including ertapenem, imipenem, meropenem and the other child was colonized with K. pneumoniae resistant to both ertapenem and imipenem but sensitive to meropenem. The remaining three children were colonized by ESBL and carbapenemase producing E.coli with HL cephalosporinase (AmpC) phenotype. All ESBL-CARBA E. coli isolates were resistant to ertapenem but sensitive to imipenem and meropenem.
Discussion
In the present study, we investigated gastrointestinal carriage rate and antimicrobial resistance pattern of ESBL producing Enterobacteriaceae in hospitalized patients admitted to Ethiopia’s largest tertiary hospital. We found high rates of colonization with ESBL-E (52%), of which, ESBL-E.coli accounted for 68% and the rest by ESBL-KP (31%). Although E. coli was the most frequently isolated than K. pneumoniae, ESBL production was more prevalent in K. pneumoniae. Among E. coli isolates, 40% were ESBL positive, while the corresponding figure for K. pneumoniae was 76%. Our result indicates having lower age and higher number of beds in a single room as a risk factor for being colonized by ESBL-E.
Fecal carriage of ESBL producing organisms in hospitalized patients has shown large variations worldwide [8–12, 22, 23]. The overall fecal carriage rates of ESBL-producing Enterobacteriaceae in our study from Ethiopia’s largest referral hospital (52%) is comparable to the overall pooled ESBL proportion estimate for East African hospitals (42%) [11], Cameron (55.3%)[24] and Ghana (49.3%) [25], but it is much higher than reports from Europe (5.4–25%) and the United States (1–25%) [22, 23]. However the colonization rates of ESBL-producing Enterobacteriaceae among hospitalized neonates (74%) and children (59%) in this study is much higher than reports from other paediatric or neonatal clinics from elsewhere, including other African countries [7] such as Gabon (45% in children) [26], Ghana (65.1% in neonates) [25], Guinea-Bissau (32.6% in children)[27] and Ecuador (56% in neonates) [28]. Recently a high rate of fecal carriage of ESBL-E (59%) in healthy children from Bangui, Central African Republic is reported [10]. Previously based on a systematic review of old data, Tansarli et.al, reported that proportion of ESBL-producing Enterobacteriaceae may not be high in Africa [7]. However the available recent data from different African courtiers including ours indicates a much higher burden ESBL-E colonization rate in African countries than previously reported by Tansarli et al, [7].
ESBL-producing Enterobacteriaceae infections is a growing threats to infants and children [29]. Treatment of neonatal sepsis has become a challenge with the emergence of carbapenemase-producing bacteria [30]. In our study, K. pneumoniae isolated from neonates and children less than five years of age had a significantly higher proportion of ESBL positivity than those isolated from adults. We found a significant association between a lower age and high colonization rate with ESBL producing K. pneumoniae. Therefore longer stay at neonatal or pediatric unit could be risk factor for colonization with ESBL-KP at TASH. Hospital-borne babies in developing countries are at high risk of neonatal infections because of poor compliance to intrapartum and postnatal infection-control practices [31]. Previous reports indicate that ESBL producing E. coli colonized mothers colonized with ESBL producing E. coli are an independent risk factor and potential reservoir for transmission of ESBL-E to neonates [9, 32]. Outbreaks caused by ESBL-producing bacteria such as K. pneumoniae in neonatal intensive care units are well described [33]. Indeed, in the same hospital where we performed the current study, infection outbreaks including neonatal sepsis due to multi-drug resistant bacteria, particularly in the neonatal units with a high neonatal mortality (41%) has been reported [16–18]. ESBL-E colonized children and other patients with underlying conditions could also act as vectors of microorganisms between the hospital and the community [34].
The antimicrobial resistance profile between the different isolates (Figs 3 and 4) is quite comparable and this may suggests local transmission of resistant strains with in the hospital. High levels of resistances for aztreonam, amoxicillin/clavulanic acid, aztreonam, cefotaxime, cefalexin, ceftazidime, trimethoprim and tobramycin were observed for both ESBL producing E. coli and K. pneumoniae. Poor hand hygiene practice, infection control measures, multi-bed rooms and crowded patients in a single rooms that were noticed during the study period might have contributed for cross-transmission of resistant strains with in the Hospital. Treatment of severe infections caused by ESBL producing E. coli and K. pneumoniae in hospitalized patients rely on carbapenems, which are the last resort to treat life-threatening infections. Infections with carbapenemase-producing Enterobacteriaceae are most difficult to manage and associated with high mortality rates [35]. The recent WHO report on AMR global surveillance indicates the identification of K. pneumoniae resistant to carbapenems in most of the countries that provided data, with reported proportions of resistance reaching up to 54% [1]. To the best of our knowledge this is the first report to indicate the emergence of colonization with carbapenems resistant ESBL producing strains in Ethiopia. Our finding of ESBL producing K. pneumoniae isolates resistant to all other antibiotics effective for treatment including carbapenems is worrisome. These extensively resistant isolates were susceptible only to tigecycline, a newer glycylcycline, recommended as option for the management of infections with carbapenems-resistant Enterobacteriaceae. However, tigecycline is currently not available in public Hospitals in Ethiopia, which poses a great challenge for patient management. Currently the burden of carbapenem resistant ESBL strains is not known and needs to be further investigated.
The emergence and spread of AMR pathogens is a threat for many African countries including Ethiopia. ESBL colonization may predispose the patient to recurrent infections and cross-transmission to others [9, 32, 36, 37]. Patients colonized with ESBL are at increased risk for invasive infections compared with non-colonized patients [36, 38]. The two children colonized with carbapenem-resistant ESBL-KP were admitted with other sick children in the same room with close proximity. If hand hygiene is not applied as recommended, these resistant bacteria can spread from one patient to another via healthcare workers contaminated hands. In hospitals, identification of patients colonized or infected with ESBL and adoption of subsequent preventive measures (isolation in a single-patient room) is suggested to prevent cross-transmission and reduce morbidity and healthcare costs.[39, 40] However, screening and contact isolation of patients colonized with ESBL in developing countries is usually not feasible due to resource constrain. Thus, effective intervention measures such as hand hygiene to prevent cross-contamination and rational use of antimicrobial are the priority options in Ethiopia.
Antimicrobial susceptibility testing (AST) is the best method to guide antimicrobial prescription. But it is not available routinely outside of tertiary referral hospitals in most African countries including Ethiopia. Furthermore, patients have to pay out of their pocket for the analysis, which further hampers its implementation in clinical management. As a result data on antimicrobial susceptibility pattern in hospital and community acquired infections are very scarce, despite their potential to reduce neonatal and children mortality [41]. Even in tertiary hospitals, the current practice of identifying infection is by clinical symptoms and in most cases the medical doctors prescribe antibiotics without prior culture and AST results due to lack of resources. Our result provides valuable data on the resistance pattern of ESBL producing E. coli and K. pneumoniae in Ethiopia.
The prevalence of infections caused by ESBL- producing bacteria is increasing worldwide. Thus Global AMR surveillance is needed, since population mobility is the main factor for its spread [2, 42, 43]. A global surveillance system for antimicrobial resistance is developed by WHO in support of the global action plan against antimicrobial resistance accepted at the World Health Assembly 2015 [44]. To monitor the effect of interventions, AMR surveillance should be integrated in national plans that should be developed to combat AMR, as stipulated in the WHO global action plan [44].
Limitation of the study includes lack of clinical data as a risk factor and molecular characterization of the resistant strains. The primary objective and design of this study was to perform initial baseline surveillance to identify the burden and resistant pattern of ESBL producing Enterobacteriaceae in hospitalized patients. Result from this study provides valuable baseline information to conduct further large prospective study involving molecular characterization of resistant strains to identify the type, source and spread pattern of antimicrobial resistance in the Hospital.
In conclusion, we report high rates of intestinal colonization rate with ESBL producing multi-drug resistant Enterobacteriaceae and the emergence of ESBL-producing carbapenems resistant K. pneumoniae particularly among pediatric patients in Ethiopia. Routine infection preventions strategies such as compliance to hand hygiene principles, rational use of antimicrobial agents and surveillance of AMR are urgently needed to prevent and control the spread of antimicrobial-resistant pathogens in the healthcare facilities.
Acknowledgments
The authors would like to thank the study participants. We acknowledge the Hospital director, infection control team and nurses at TASH for their assistance during the conduct of the study. We are grateful for the valuable support of EUCAST Laboratory for Antimicrobial Susceptibility Testing, Clinical Microbiology, Central Hospital Växjö, Sweden.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The study was supported by grants from Vetenskapsrådet (Swedish research council grants, VR 521-2011-3437; VR 348-2011-7383) to EA and Myndigheten för Samhällsskydd och Beredskap (Swedish civil contingency Agency grant, 2010-7878) to EA.
References
- 1.World Health Organization 2014: Antimicrobial resistance: global report on surveillance WHO Library Cataloguing-in-Publication Data; Available: http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf?ua=1. Accessed 4 August 2016. [Google Scholar]
- 2.MacPherson DW, Gushulak BD, Baine WB, Bala S, Gubbins PO, Holtom P, et al. Population mobility, globalization, and antimicrobial drug resistance. Emerg Infect Dis. 2009;15:1727–32. Epub 2009/11/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reuland EA, Sonder GJ, Stolte I, Al Naiemi N, Koek A, Linde GB, et al. Travel to Asia and traveller's diarrhoea with antibiotic treatment are independent risk factors for acquiring ciprofloxacin-resistant and extended spectrum beta-lactamase-producing Enterobacteriaceae-a prospective cohort study. Clin Microbiol Infect. 2016. 10.1016/j.cmi.2016.05.003 . [DOI] [PubMed] [Google Scholar]
- 4.Barreto Miranda I, Ignatius R, Pfuller R, Friedrich-Janicke B, Steiner F, Paland M, et al. High carriage rate of ESBL-producing Enterobacteriaceae at presentation and follow-up among travellers with gastrointestinal complaints returning from India and Southeast Asia. J Travel Med. 2016;23:tav024 10.1093/jtm/tav024 . [DOI] [PubMed] [Google Scholar]
- 5.Kuenzli E, Jaeger VK, Frei R, Neumayr A, DeCrom S, Haller S, et al. High colonization rates of extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli in Swiss travellers to South Asia- a prospective observational multicentre cohort study looking at epidemiology, microbiology and risk factors. BMC Infect Dis. 2014;14:528 10.1186/1471-2334-14-528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vialle-Valentin CE, Lecates RF, Zhang F, Desta AT, Ross-Degnan D. Predictors of antibiotic use in African communities: evidence from medicines household surveys in five countries. Trop Med Int Health. 2012;17:211–22. Epub 2011/10/18. 10.1111/j.1365-3156.2011.02895.x . [DOI] [PubMed] [Google Scholar]
- 7.Tansarli GS, Poulikakos P, Kapaskelis A, Falagas ME. Proportion of extended-spectrum beta-lactamase (ESBL)-producing isolates among Enterobacteriaceae in Africa: evaluation of the evidence—systematic review. J Antimicrob Chemother. 2014;69:1177–84. 10.1093/jac/dkt500 . [DOI] [PubMed] [Google Scholar]
- 8.Sangare SA, Maiga AI, Guindo I, Maiga A, Camara N, Savadogo S, et al. Prevalence of extended-spectrum beta-lactamase-producing Enterobacteriaceae isolated from blood cultures in Africa. Med Mal Infect. 2015;45:374–82. 10.1016/j.medmal.2015.08.003 . [DOI] [PubMed] [Google Scholar]
- 9.Chereau F, Herindrainy P, Garin B, Huynh BT, Randrianirina F, Padget M, et al. Colonization of Extended-Spectrum-beta-Lactamase- and NDM-1-Producing Enterobacteriaceae among Pregnant Women in the Community in a Low-Income Country: a Potential Reservoir for Transmission of Multiresistant Enterobacteriaceae to Neonates. Antimicrob Agents Chemother. 2015;59:3652–5. 10.1128/AAC.00029-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farra A, Frank T, Tondeur L, Bata P, Gody JC, Onambele M, et al. High rate of faecal carriage of extended-spectrum beta-lactamase-producing Enterobacteriaceae in healthy children in Bangui, Central African Republic. Clin Microbiol Infect. 2016. 10.1016/j.cmi.2016.07.001 . [DOI] [PubMed] [Google Scholar]
- 11.Sonda T, Kumburu H, van Zwetselaar M, Alifrangis M, Lund O, Kibiki G, et al. Meta-analysis of proportion estimates of Extended-Spectrum-Beta-Lactamase-producing Enterobacteriaceae in East Africa hospitals. Antimicrob Resist Infect Control. 2016;5:18 10.1186/s13756-016-0117-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Storberg V. ESBL-producing Enterobacteriaceae in Africa—a non-systematic literature review of research published 2008–2012. Infect Ecol Epidemiol. 2014;4 10.3402/iee.v4.20342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gedebou M, Habte-Gabr E, Kronvall G, Yoseph S. Hospital-acquired infections among obstetric and gynaecological patients at Tikur Anbessa Hospital, Addis Ababa. J Hosp Infect. 1988;11:50–9. Epub 1988/01/01. 0195-6701(88)90039-4 [pii]. . [DOI] [PubMed] [Google Scholar]
- 14.Gedebou M, Kronvall G, Habte-Gabr E, Ringertz S. The bacteriology of nosocomial infections at Tikur Anbessa Teaching Hospital, Addis Ababa. Acta Pathol Microbiol Immunol Scand B. 1987;95:331–6. Epub 1987/12/01. . [DOI] [PubMed] [Google Scholar]
- 15.Ringertz S, Bellete B, Karlsson I, Ohman G, Gedebou M, Kronvall G. Antibiotic susceptibility of Escherichia coli isolates from inpatients with urinary tract infections in hospitals in Addis Ababa and Stockholm. Bull World Health Organ. 1990;68:61–8. Epub 1990/01/01. [PMC free article] [PubMed] [Google Scholar]
- 16.Shitaye D, Asrat D, Woldeamanuel Y, Worku B. Risk factors and etiology of neonatal sepsis in Tikur Anbessa University Hospital, Ethiopia. Ethiop Med J. 2010;48:11–21. Epub 2010/07/09. . [PubMed] [Google Scholar]
- 17.Worku B. Klebsiella oxytoca outbreak at the Ethio-Swedish Children's Hospital (ESCH). Ethiop Med J. 1997;35:177–83. . [PubMed] [Google Scholar]
- 18.Woldehanna TD, Idejene ET. Neonatal mortality in a teaching hospital, North Western Ethiopia. Cent Afr J Med. 2005;51:30–3. Epub 2007/09/26. . [PubMed] [Google Scholar]
- 19.De Rosa FG, Corcione S, Cavallo R, Di Perri G, Bassetti M. Critical issues for Klebsiella pneumoniae KPC-carbapenemase producing K. pneumoniae infections: a critical agenda. Future Microbiol. 2015;10:283–94. 10.2217/fmb.14.121 . [DOI] [PubMed] [Google Scholar]
- 20.Calbo E, Garau J. The changing epidemiology of hospital outbreaks due to ESBL-producing Klebsiella pneumoniae: the CTX-M-15 type consolidation. Future Microbiol. 2015;10:1063–75. 10.2217/fmb.15.22 . [DOI] [PubMed] [Google Scholar]
- 21.Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81. 10.1111/j.1469-0691.2011.03570.x . [DOI] [PubMed] [Google Scholar]
- 22.Hoban DJ, Lascols C, Nicolle LE, Badal R, Bouchillon S, Hackel M, et al. Antimicrobial susceptibility of Enterobacteriaceae, including molecular characterization of extended-spectrum beta-lactamase-producing species, in urinary tract isolates from hospitalized patients in North America and Europe: results from the SMART study 2009–2010. Diagn Microbiol Infect Dis. 2012;74:62–7. 10.1016/j.diagmicrobio.2012.05.024 . [DOI] [PubMed] [Google Scholar]
- 23.Han JH, Nachamkin I, Zaoutis TE, Coffin SE, Linkin DR, Fishman NO, et al. Risk factors for gastrointestinal tract colonization with extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli and Klebsiella species in hospitalized patients. Infect Control Hosp Epidemiol. 2012;33:1242–5. 10.1086/668443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lonchel CM, Melin P, Gangoue-Pieboji J, Assoumou MC, Boreux R, De Mol P. Extended-spectrum beta-lactamase-producing Enterobacteriaceae in Cameroonian hospitals. Eur J Clin Microbiol Infect Dis. 2013;32:79–87. 10.1007/s10096-012-1717-4 . [DOI] [PubMed] [Google Scholar]
- 25.Obeng-Nkrumah N, Twum-Danso K, Krogfelt KA, Newman MJ. High levels of extended-spectrum beta-lactamases in a major teaching hospital in Ghana: the need for regular monitoring and evaluation of antibiotic resistance. Am J Trop Med Hyg. 2013;89:960–4. 10.4269/ajtmh.12-0642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schaumburg F, Alabi A, Kokou C, Grobusch MP, Kock R, Kaba H, et al. High burden of extended-spectrum beta-lactamase-producing Enterobacteriaceae in Gabon. J Antimicrob Chemother. 2013;68:2140–3. 10.1093/jac/dkt164 . [DOI] [PubMed] [Google Scholar]
- 27.Isendahl J, Turlej-Rogacka A, Manjuba C, Rodrigues A, Giske CG, Naucler P. Fecal carriage of ESBL-producing E. coli and K. pneumoniae in children in Guinea-Bissau: a hospital-based cross-sectional study. PLoS One. 2012;7:e51981 10.1371/journal.pone.0051981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nordberg V, Quizhpe Peralta A, Galindo T, Turlej-Rogacka A, Iversen A, Giske CG, et al. High proportion of intestinal colonization with successful epidemic clones of ESBL-producing Enterobacteriaceae in a neonatal intensive care unit in Ecuador. PLoS One. 2013;8:e76597 10.1371/journal.pone.0076597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lukac PJ, Bonomo RA, Logan LK. Extended-spectrum beta-lactamase-producing Enterobacteriaceae in children: old foe, emerging threat. Clin Infect Dis. 2015;60:1389–97. 10.1093/cid/civ020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Datta S, Roy S, Chatterjee S, Saha A, Sen B, Pal T, et al. A five-year experience of carbapenem resistance in Enterobacteriaceae causing neonatal septicaemia: predominance of NDM-1. PLoS One. 2014;9:e112101 10.1371/journal.pone.0112101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zaidi AK, Huskins WC, Thaver D, Bhutta ZA, Abbas Z, Goldmann DA. Hospital-acquired neonatal infections in developing countries. Lancet. 2005;365:1175–88. 10.1016/S0140-6736(05)71881-X . [DOI] [PubMed] [Google Scholar]
- 32.Denkel LA, Schwab F, Kola A, Leistner R, Garten L, von Weizsacker K, et al. The mother as most important risk factor for colonization of very low birth weight (VLBW) infants with extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBL-E). J Antimicrob Chemother. 2014. Epub 2014/04/15. 10.1093/jac/dku097 . [DOI] [PubMed] [Google Scholar]
- 33.Somily AM, Alsubaie SS, BinSaeed AA, Torchyan AA, Alzamil FA, Al-Aska AI, et al. Extended-spectrum beta-lactamase-producing Klebsiella pneumoniae in the neonatal intensive care unit: does vancomycin play a role? Am J Infect Control. 2014;42:277–82. Epub 2014/03/04. 10.1016/j.ajic.2013.09.028 . [DOI] [PubMed] [Google Scholar]
- 34.Gesualdo F, Bongiorno D, Rizzo C, Bella A, Menichella D, Stefani S, et al. MRSA nasal colonization in children: prevalence meta-analysis, review of risk factors and molecular genetics. Pediatr Infect Dis J. 2013;32:479–85. Epub 2013/01/24. 10.1097/INF.0b013e3182864e4c . [DOI] [PubMed] [Google Scholar]
- 35.Ducomble T, Faucheux S, Helbig U, Kaisers UX, Konig B, Knaust A, et al. Large hospital outbreak of KPC-2-producing Klebsiella pneumoniae: investigating mortality and the impact of screening for KPC-2 with polymerase chain reaction. J Hosp Infect. 2015;89:179–85. 10.1016/j.jhin.2014.11.012 . [DOI] [PubMed] [Google Scholar]
- 36.Martins IS, Moreira BM, Riley LW, Santoro-Lopes G. Outbreak of extended-spectrum beta-lactamase-producing Klebsiella pneumoniae infection among renal transplant recipients. J Hosp Infect. 2006;64:305–8. 10.1016/j.jhin.2006.07.011 . [DOI] [PubMed] [Google Scholar]
- 37.Christiaens G, Ciccarella Y, Damas P, Hayette MP, Melin P, Nys M, et al. Prospective survey of digestive tract colonization with enterobacteriaceae that produce extended-spectrum beta-lactamases in intensive care units. J Hosp Infect. 2006;62:386–8. 10.1016/j.jhin.2005.09.014 . [DOI] [PubMed] [Google Scholar]
- 38.Pena C, Pujol M, Ardanuy C, Ricart A, Pallares R, Linares J, et al. Epidemiology and successful control of a large outbreak due to Klebsiella pneumoniae producing extended-spectrum beta-lactamases. Antimicrob Agents Chemother. 1998;42:53–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shitrit P, Gottesman BS, Katzir M, Kilman A, Ben-Nissan Y, Chowers M. Active surveillance for methicillin-resistant Staphylococcus aureus (MRSA) decreases the incidence of MRSA bacteremia. Infect Control Hosp Epidemiol. 2006;27:1004–8. Epub 2006/09/29. 10.1086/507914 . [DOI] [PubMed] [Google Scholar]
- 40.Huang SS, Yokoe DS, Hinrichsen VL, Spurchise LS, Datta R, Miroshnik I, et al. Impact of routine intensive care unit surveillance cultures and resultant barrier precautions on hospital-wide methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2006;43:971–8. Epub 2006/09/20. 10.1086/507636 . [DOI] [PubMed] [Google Scholar]
- 41.Bhutta ZA, Zaidi AK, Thaver D, Humayun Q, Ali S, Darmstadt GL. Management of newborn infections in primary care settings: a review of the evidence and implications for policy? Pediatr Infect Dis J. 2009;28:S22–30. Epub 2009/01/10. 10.1097/INF.0b013e31819588ac . [DOI] [PubMed] [Google Scholar]
- 42.Ostholm-Balkhed A, Tarnberg M, Nilsson M, Nilsson LE, Hanberger H, Hallgren A. Travel-associated faecal colonization with ESBL-producing Enterobacteriaceae: incidence and risk factors. J Antimicrob Chemother. 2013;68:2144–53. Epub 2013/05/16. 10.1093/jac/dkt167 . [DOI] [PubMed] [Google Scholar]
- 43.von Wintersdorff CJ, Penders J, Stobberingh EE, Lashof AM, Hoebe CJ, Savelkoul PH, et al. High rates of antimicrobial drug resistance gene acquisition after international travel, the Netherlands. Emerg Infect Dis. 2014;20:649–57. Epub 2014/03/25. 10.3201/eid.2004.131718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.World health organization: Global Action Plan on Antimicrobial Resistance, 2015. Available: http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_20-en.pdf?ua=1. Accessed 4 August 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.