Abstract
The purpose of this study was to correlate measures of sagittal spinopelvic alignment [lumbar lordosis (LL), sacral slope (SS), pelvic tilt (PT) and pelvic incidence (PI)] and measures of acetabular coverage [lateral center edge angle (LCEA) and Tonnis angle] in asymptomatic adolescents on standing biplanar radiographs. We hypothesized that subjects with increased pelvic incidence and LL would have increased anterior PT and increased measures of acetabular coverage. Upright anteroposterior and lateral spinopelvic radiographs were obtained using EOS imaging technique. LCEA and Tonnis angle were calculated on the anteroposterior images and the lateral images were analyzed for LL, PI, PT and SS. LL was found to have a strong correlation with SS (rs = 0.786, P < 0.001), moderate correlation with PI (rs = 0.529, P < 0.001), and a poor inverse correlation with PT (rs = −0.167, P = 0.018). However, LCEA was not found to be significantly correlated with PT (rs = 0.084, P = 0.238) and Tonnis angle was not found to be correlated with any of the sagittal spinopelvic measures. Healthy, asymptomatic adolescents with increased pelvic incidence and lumbar lordosis did not have increased anterior PT or increased measures of acetabular coverage. The correlations identified in previous cadaveric studies or clinical studies evaluating changes between supine and standing radiographs are not supported in this healthy adolescent population. Our findings may suggest that an individual’s acetabulum develops as a dynamic adaptation to one's particular sagittal spinopelvic alignment to optimize femoral head coverage. Level III. Diagnostic – Investigating a diagnostic test.
INTRODUCTION
Prior cadaveric studies have shown that pelvic tilt (PT) influences radiographic measures of acetabular retroversion and dysplasia for a given pelvis [1, 2], and that PT varies when someone is standing or supine [3]. This has led some authors to recommend obtaining a standardized supine anteroposterior (AP) pelvis radiograph to accurately assess hip pathology [1]. However, significant variations in pelvic morphologic parameters [PT, pelvic incidence, sacral slope (SS), lumbar lordosis] have been demonstrated in healthy young adult populations [1, 4, 5]. Taken together, this makes accurate assessment of acetabular version, coverage and dysplasia for a given individual challenging on a supine anteroposterior radiograph.
Getting an accurate measure of acetabular coverage is of critical importance for guiding surgical decision making. In the case of femoroacetabular impingement, there is decreased clearance between the head neck junction and the acetabular rim. With hip flexion and internal rotation, the femoral neck has been shown to abut the labrum resulting in damage [6]. Over time, this repetitive impact theoretically results in degeneration of the labrum and surrounding articular cartilage, ultimately causing degenerative hip disease [7, 8]. Surgical treatment including arthroscopy and surgical dislocation have been shown to be effective in improving pain and function [9–14]. In more severe cases such as those with significant acetabular retroversion periacetabular osteotomy is thought to be a viable option [15].
Some investigators have suggested that attempts should be made to standardize PT on supine AP radiographs [1]. It is known that variations in pelvic parameters of sagittal alignment for an individual correlate with changes in AP radiographic measures of acetabular version and dysplasia. Standardizing PT alters an individual's sagittal alignment and therefore has an effect on their coverage measurements on the AP view. Standardizing in this manner assumes a correlation between sagittal alignment and AP radiographic measurements for the population as a whole. Therefore, the purpose of this study was to assess the relationship between sagittal spinopelvic alignment and measures of acetabular coverage in asymptomatic adolescents. Based on the previously published studies [1–3], we hypothesized that subjects with increased pelvic incidence and lumbar lordosis would have increased anterior PT and increased measures of acetabular coverage.
METHODS
This is an IRB approved retrospective radiographic evaluation of children presenting to our scoliosis clinic for evaluation of spinal asymmetry. Subjects were identified between 2009 and 2013. Subjects were excluded if they: had a spinal deformity magnitude greater than 15º, had a congenital anomaly such as a hemivertebrae, were less than 13 years of age, had a history of hip pathology (or their chart was missing and we were unable to confirm patient history), or they had a radiograph that did not capture the bottom of the acetabular teardrop. All subjects had simultaneous AP and lateral weight-bearing radiographs of the spine and pelvis obtained using the EOS imaging technique.
EOS is a validated imaging technique that uses two perpendicular X-ray beams collimated in two thin, horizontal, fan-shaped beams along with two variable gaseous detectors which allow for detection in a line-by-line manner with very low radiation exposure [16–18]. The fan-beam X-rays and detectors are mounted on a C-arm and scan all or part of the patient’s body and allow for frontal and lateral X-rays of a patient to be carried out simultaneously.
AP radiographs were analysed and the lateral center edge angle (LCEA) and Tonnis angle were calculated. LCEA is defined as an angle formed by a line drawn vertically from the center of the femoral head and a second line drawn from the center of the femoral head to the lateral edge of the sourcil. Angles less than 20º are indicative of hip dysplasia, while values between 20 and 25º represent borderline dysplasia [19]. A value greater than 40º signifies acetabular overcoverage [20]. For the purpose of this study, we will consider values between 25 and 40º to be normal.
The Tonnis angle measures the slope of the acetabular sourcil, which corresponds to the weight-bearing surface of the acetabulum. It is formed by subchondral osseous condensation in the acetabular roof [21]. The Tonnis angle is formed by a line connecting the medial and lateral edge of the acetabular sourcil and a line parallel to the horizontal plane. A Tonnis angle greater than 14º is considered consistent with hip dysplasia and an angle less than −8º represents acetabular overcoverage [22].
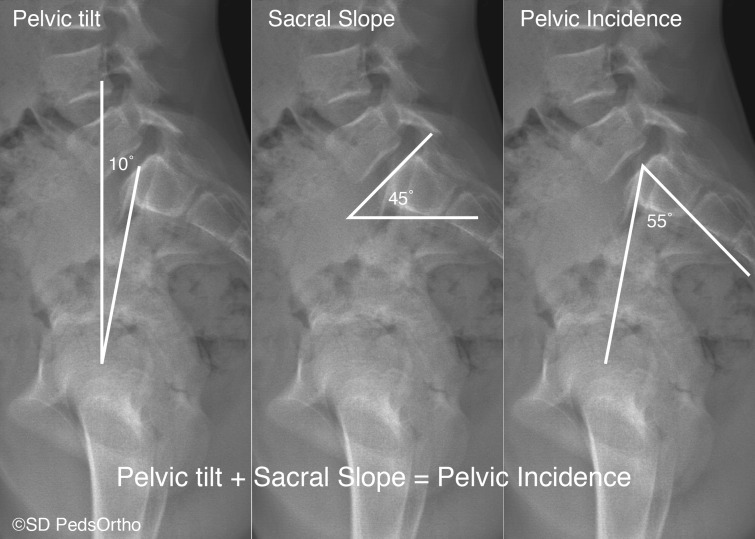
Lateral radiographs were analysed for lumbar lordosis (LL), pelvic incidence (PI), PT, and sacral slope (SS) (Fig. 1) using the methods outlined in the Spinal Deformity Study Group Radiographic Measurement Manual [23]. These measurements have been reported to be reliable and reproducible despite relatively minor difficulties identifying some of the bony landmarks used in these measures [24]. All measurements were made on digital radiographs using MergePACS measurement tools (version 6.5.6; Merge Healthcare, Chicago, IL, USA).
Fig. 1.
Lateral radiograph indicating the method of measurement for Pelvic tilt, Sacral slope, and Pelvic incidence. Note that pelvic tilt + sacral slope = pelvic incidence.
The intraclass correlation coefficient (ICC) was used to evaluate measurement agreement among authors for each measure prior to data collection. ICC was found to be acceptable among observers ranging from 0.77 (LCEA) to 0.97 (PT) (P ≤ 0.001). Data was tested for normality using the Shapiro Wilk test and found to be non-normal, therefor Spearman’s rho (rs) was used to analyse data for significant correlations between the sagittal and coronal measurements. Statistical significance was defined as P < 0.05. All statistical analysis was conducted using SPSS (version 12; SPSS, Chicago, IL, USA).
RESULTS
Ninety-nine subjects were included in this study after the exclusion criteria were applied. Gender and age distribution are listed in Table I. Descriptive analysis of radiographic measurements are listed in Table II.
Table I.
Gender and age distribution
| Gender | N | Mean age (years ± Std. dev.) | Min age | Max age |
|---|---|---|---|---|
| Female | 53 | 15.7±1.4 | 13.1 | 18.75 |
| Male | 46 | 15.2±1.5 | 13.2 | 18.75 |
| Total | 99 | 15.4±1.5 | 13.1 | 18.75 |
Table II.
Descriptive statistics of radiographic measurements
| Mean ± std. Dev. | 95% CI | Minimum | Maximum | Range | |
|---|---|---|---|---|---|
| LCEA | 31.9 ± 6 | 31.1–32.8 | 10 | 49 | 39 |
| Tonnis angle | 2 ± 5.8 | 1.2–2.8 | −17 | 15 | 32 |
| Lumbar lordosis | 41.9 ± 14.6 | 39.9–44 | 3 | 75 | 72 |
| Pelvic incidence | 46.8 ± 11.1 | 45.2–48.3 | 21 | 80 | 59 |
| Pelvic tilt | 7.8 ± 8.1 | 6.6–8.9 | −12 | 26 | 38 |
| Sacral slope | 38.8 ± 9.4 | 37.5–40.1 | 11 | 71 | 60 |
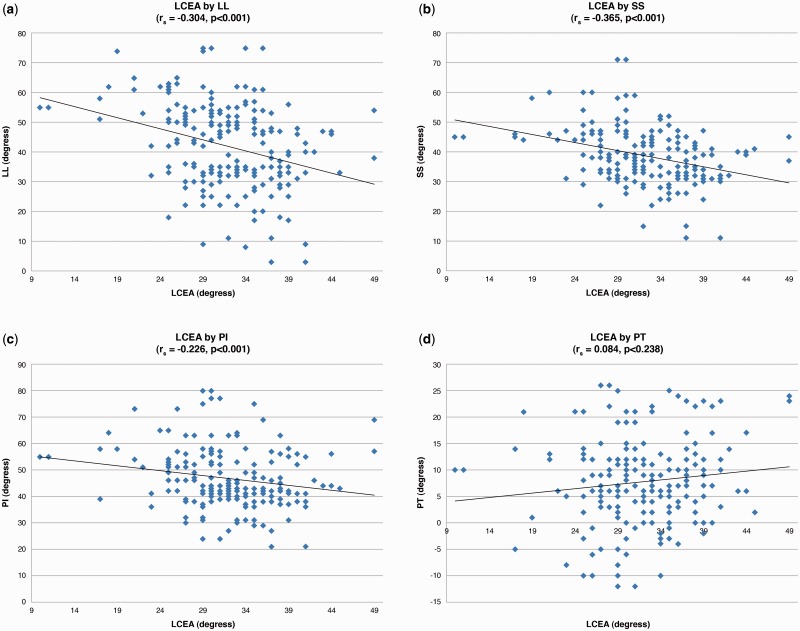
LCEA was found to have a weak inverse correlation with LL (rs = −0.304, P < 0.001) (Fig. 2a) and SS (rs = −0.365, P < 0.001) (Fig. 2b). LCEA was found to have a poor inverse correlation with PI (rs = −0.226, P = 0.001) (Fig. 2c). LCEA was not found to be significantly correlated with PT (rs = 0.084, P = 0.238) (Fig. 2d). Tonnis angle was not found to be correlated with any of the sagittal measurements. A complete list of rs values can be found in Table III.
Fig. 2.
(a) This is a scatterplot showing the relationship between lumbar lordosis (LL) and lateral center edge angle (LCEA). (b) This is a scatterplot showing the relationship between sacral slope (SS) and LCEA. (c) This is a scatterplot showing the relationship between pelvic incidence (PI) and LCEA. (d) This is a scatterplot showing the relationship between pelvic tilt (PT) and LCEA.
Table III.
Correlation results
| Lumbar lordosis | Pelvic incidence | Pelvic tilt | Sacral slope | ||
|---|---|---|---|---|---|
| LCEA | rs | −0.304 | −0.226 | 0.084 | −0.365 |
| P values | <0.001 | 0.001 | 0.238 | <0.001 | |
| Tonnis angle | rs | 0.046 | 0.02 | −0.015 | −0.001 |
| P values | 0.517 | 0.782 | 0.834 | 0.987 |
LCEA, lateral center edge angle. Value in bold are significant at P = 0.05.
PI was found to have a moderate correlation with PT (rs = 0.549, P < 0.001) and SS (rs = 0.612, P < 0.001). PT was found to have a poor inverse correlation with SS (rs = −0.237, P = 0.001) (Table IV). LL was found to have a strong correlation with SS (rs = 0.786, P < 0.001), moderate correlation with PI (rs = 0.529, P < 0.001), and a poor inverse correlation with PT (rs = −0.167, P = 0.018) (Table V).
Table IV.
Correlation results for sagittal pelvic parameters
| Pelvic incidence | Pelvic tilt | Sacral slope | ||
|---|---|---|---|---|
| Pelvic incidence | rs | 1 | 0.549 | 0.612 |
| P values | . | <0.001 | <0.001 | |
| Pelvic tilt | rs | 0.549 | 1 | −0.237 |
| P values | <0.001 | . | 0.001 | |
| Sacral slope | rs | 0.612 | −0.237 | 1 |
| P values | <0.001 | 0.001 | . |
Table V.
Correlation results for lumbar lordosis and our sagittal pelvic parameters
| Pelvic incidence | Pelvic tilt | Sacral slope | ||
|---|---|---|---|---|
| Lumbar lordosis | rs | 0.529 | −0.167 | 0.786 |
| P values | <0.001 | 0.018 | <0.001 |
LCEA was found to be abnormal in 28 hips (14%). Tonnis angle was found to be abnormal in 13 hips (7%). Four hips (2%) were found to have both abnormal LCEA and Tonnis angles.
DISCUSSION
Based on this analysis, we reject our hypothesis that subjects with increased pelvic incidence and lumbar lordosis have increased anterior PT and increased measures of acetabular coverage. As previously published [25, 26], significant correlations between lumbar lordosis and the sagittal pelvic measures of sacral slope (rs = 0.786, P < 0.001), PT (rs = 0.786, P < 0.001) and pelvic incidence (rs = 0.529, P < 0.001) were identified in the current analysis. Additionally, as previously published27, significant correlations between the three pelvic measures were also identified. However, contrary to previous publications [28], measures of acetabular coverage (LCEA and Tonnis angle) were not found to be correlated to PT in this analysis.
We theorize that this lack of correlation in a healthy, asymptomatic adolescent population suggests that acetabular orientation may develop as an adaptation to one’s particular standing spinopelvic sagittal alignment. This makes intuitive sense as the development of the acetabulum depends on the ossification of the laterally based acetabular cartilage complex after initiation of ambulation [29, 30]. The pattern of ossification and eventual shape of the bony acetabulum depends on forces exerted across the joint. Therefore, the specific standing sagittal profile of an individual may determine the pattern of ossification of the acetabular cartilage complex such that femoral head coverage is maximized in the standing position at maturity.
Our findings are in contrast to the work that Siebenrock et al. [1] and Monazzam et al. [31] have done in cadaveric models. Siebenrock et al. evaluated four pelves for signs of retroversion including cross-over sign and posterior wall sign. The pelves were mounted on a jig that allowed the AP radiographs to be sequentially taken in 3º increments through a range of 9º of inclination to 12º of reclination. At 6º of reclination, none of the acetabula had signs of retroversion while at 9º of inclination toward the X-ray beam all acetabula showed both signs of retroversion [1].
These findings were corroborated by Monazzam et al. who looked at the effect of pelvic rotation and inclination relative to the x-ray source [31]. The authors also used a jig to rotate or tilt a cadaveric pelvis in 5º increments. They found that rotation of the hip away from the beam source and/or increased anterior tilt falsely increased all coverage parameters including Lateral center-edge angle, Sharp angle, crossover sign and retroversion index. They found that an individual pelvis tilted towards an X-ray beam increased LCEA by 0.4º for each additional degree of tilt [31].
It has also been shown that in clinical practice, whether the patient’s pelvic films are taken in the standing or supine position can affect radiographic assessment of acetabular coverage. In a study of 50 consecutive symptomatic hips, Pullen et al examined measures of acetabular coverage on standardized supine and weight bearing AP pelvic radiographs [32]. The authors found that the weight-bearing position typically correlates with a decrease in the pubic symphysis to sacrococcygeal distance (PSSC), or a decrease in anterior PT, and that this decrease in PSSC results in decreased LCEA relative to standard supine films, which corroborates the findings of Siebenrock et al. [1] and Monazzam et al. [31] in a clinical cohort.
Watanabe et al. [28] evaluated acetabular coverage in adult patients with decreased lumbar lordosis due to pathologic lumbar degenerative spine disease. A small subset of these patients also had supine and standing pelvis radiographs. They found that patients with decreased lumbar lordosis had increased posterior pelvic inclination (P < 0.01) and decreased anterior acetabular femoral head coverage (P < 0.001). Also, standing resulted in further increased posterior pelvic inclination and decreased femoral head coverage. This study supports previous findings, however, is different from our current analysis that evaluated healthy asymptomatic adolescent patients.
Unlike previous publications that assessed the spinopelvic relationships in supine and standing positions, our analysis attempted to identify these relationships in standing radiographs across a large, healthy cohort. If the previous observations held true, subjects with decreased lordosis would have posterior PT and decreased acetabular coverage. This was, however, not the case. We identified a large range of PT (−12º to 26º) in this asymptomatic adolescent cohort and the acetabular coverage measures were within normal limits for the vast majority of patients (greater than 80%). This leads us to believe that evaluating acetabular coverage with a standing pelvis radiograph gives a more physiologic understanding of hip position and function rather than a standardized supine radiograph.
Our study had several limitations. First, it was retrospective in nature, and only looked at standing EOS radiographs. It would have been useful to also have standardized supine films to see if individuals who had normal parameters in the standing view would change to abnormal with standardization and vice versa. However, due to the additional radiation exposure this would not be feasible in a healthy adolescent population. A second limitation of our present study is that all of the included subjects were asymptomatic for hip pathology (impingement or dysplasia). It would be useful to know if measures of acetabular overcoverage or undercoverage correlated with symptomatology. A study in which symptomatic and asymptomatic patients had both standing and standardized supine AP films would also be illuminating. This design would allow one to see if there is a difference in correlation between acetabular overcoverage and symptomatology between the standing and standardized supine views.
Although not proven in this study, our findings suggest that an individual’s acetabulum potentially develops as an adaptation to one's particular sagittal spinal alignment. Further longitudinal studies should be done to evaluate this theory in the future.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res 2003; 407: 241–8. [DOI] [PubMed] [Google Scholar]
- 2.Henebry A, Gaskill T. The effect of pelvic tilt on radiographic markers of acetabular coverage. Am J Sports Med 2013; 41: 2599–603. [DOI] [PubMed] [Google Scholar]
- 3.Konishi N, Mieno T. Determination of acetabular coverage of the femoral head with use of a single anteroposterior radiograph. A new computerized technique. J Bone Joint Surg Am 1993; 75: 1318–33. [DOI] [PubMed] [Google Scholar]
- 4.Janssen MMA, Drevelle X, Humbert L, et al. Differences in male and female spino-pelvic alignment in asymptomatic young adults: a three-dimensional analysis using upright low-dose digital biplanar X-rays. Spine (Phila Pa 1976) 2009; 34: E826–32. [DOI] [PubMed] [Google Scholar]
- 5.Vialle R, Levassor N, Rillardon L. et al. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am 2005; 87: 260–7. [DOI] [PubMed] [Google Scholar]
- 6.Ito K, Minka MA, Leunig M. et al. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br 2001; 83: 171–6. [DOI] [PubMed] [Google Scholar]
- 7.Leunig M, Beck M, Woo A. et al. Acetabular rim degeneration: a constant finding in the aged hip. Clin Orthop Relat Res 2003; 413: 201–7. [DOI] [PubMed] [Google Scholar]
- 8.Leunig M, Casillas MM, Hamlet M. et al. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand 2000; 71: 370–5. [DOI] [PubMed] [Google Scholar]
- 9.Beck M, Leunig M, Parvizi J. et al. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res 2004; 67–73. [PubMed] [Google Scholar]
- 10.Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and débridement in young adults. J Bone Joint Surg Am 2006; 88: 1735–41. [DOI] [PubMed] [Google Scholar]
- 11.Espinosa N, Rothenfluh DA, Beck M. et al. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am 2006; 88: 925–35. [DOI] [PubMed] [Google Scholar]
- 12.Matsuda DK, Carlisle JC, Arthurs SC. et al. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy 2011; 27: 252–69. [DOI] [PubMed] [Google Scholar]
- 13.Clohisy JC, St John LC, Schutz AL. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clin Orthop Relat Res 2010; 468: 555–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stevens MS, Legay DA, Glazebrook MA. et al. The evidence for hip arthroscopy: grading the current indications. Arthroscopy 2010; 26: 1370–83. [DOI] [PubMed] [Google Scholar]
- 15.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am 2003; 85-A: 278–86. [DOI] [PubMed] [Google Scholar]
- 16.Bittersohl B, Freitas J, Zaps D. et al. EOS imaging of the human pelvis: reliability, validity, and controlled comparison with radiography. J Bone Joint Surg Am 2013; 95: e581–9. [DOI] [PubMed] [Google Scholar]
- 17.Rousseau M-A, Brusson A, Lazennec J-Y. Assessment of the axial rotation of the pelvis with the EOS® imaging system: intra- and inter-observer reproducibility and accuracy study. Eur J Orthop Surg Traumatol 2014; 24: 891–5. [DOI] [PubMed] [Google Scholar]
- 18.Sigmann M-H, Delabrousse E, Riethmuller D. et al. An evaluation of the EOS X-ray imaging system in pelvimetry. Diagn Interv Imaging 2014; 95: 833–8. [DOI] [PubMed] [Google Scholar]
- 19.Wiberg G. Shelf operation in congenital dysplasia of the acetabulum and in subluxation and dislocation of the hip. J Bone Joint Surg Am 1953; 35A: 65–80. [PubMed] [Google Scholar]
- 20.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis–what the radiologist should know. AJR Am J Roentgenol 2007; 188: 1540–52. [DOI] [PubMed] [Google Scholar]
- 21.Beltran LS, Rosenberg ZS, Mayo JD. et al. Imaging evaluation of developmental hip dysplasia in the young adult. AJR Am J Roentgenol 2013; 200: 1077–88. [DOI] [PubMed] [Google Scholar]
- 22.Schmitz MR, Bittersohl B, Zaps D. et al. Spectrum of radiographic femoroacetabular impingement morphology in adolescents and young adults: An EOS-based double-cohort study. J Bone Joint Surg Am 2013; e90: 1–8. [DOI] [PubMed] [Google Scholar]
- 23.O’Brien MF, Kuklo TR, Blanke KM. et al. eds. Spinal Deformity Study Group Radiographic Measurement Manual. Medtronic Sofamor Danek USA, Inc, 2008. [Google Scholar]
- 24.Yamada K, Aota Y, Higashi T. et al. Accuracies in Measuring Spinopelvic Parameters in Full-Spine Lateral Standing Radiograph. Spine (Phila Pa 1976) 2015; 40: E640–6. [DOI] [PubMed] [Google Scholar]
- 25.Rajnics P, Templier A, Skalli W. et al. The association of sagittal spinal and pelvic parameters in asymptomatic persons and patients with isthmic spondylolisthesis. J Spinal Disord Tech 2002; 15: 24–30. [DOI] [PubMed] [Google Scholar]
- 26.Mac-Thiong J-M, Berthonnaud E, Dimar JR. et al. Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976) 2004; 29: 1642–7. [DOI] [PubMed] [Google Scholar]
- 27.Upasani VV, Tis J, Bastrom T. et al. Analysis of sagittal alignment in thoracic and thoracolumbar curves in adolescent idiopathic scoliosis: how do these two curve types differ? Spine (Phila Pa 1976) 2007; 32: 1355–9. [DOI] [PubMed] [Google Scholar]
- 28.Watanabe W, Sato K, Itoi E. et al. Posterior pelvic tilt in patients with decreased lumbar lordosis decreases acetabular femoral head covering. Orthopedics 2002; 25: 321–4. [DOI] [PubMed] [Google Scholar]
- 29.Strayer LM. Embryology of the human hip joint. Clin Orthop Relat Res 1971; 74: 221–40. [PubMed] [Google Scholar]
- 30.Laurenson RD. Development of the acetabular roof in the fetal hip; an arthrographic and histological study. J Bone Joint Surg Am 1965; 47: 975–83. [PubMed] [Google Scholar]
- 31.Monazzam S, Agashe M, Hosalkar HS. Reliability of overcoverage parameters with varying morphologic pincer features: comparison of EOS® and radiography. Clin Orthop Relat Res 2013; 471: 2578–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pullen WM, Henebry A, Gaskill T. Variability of acetabular coverage between supine and weightbearing pelvic radiographs. Am J Sports Med 2014; 42: 2643–8. [DOI] [PubMed] [Google Scholar]