Abstract
Avascular necrosis (AVN) of femoral head needs to be addressed early in the course of the disease, to prevent progression to osteoarthritis. A revascularizing procedure which can help preserve the head should be considered in young adults to alleviate the need for total hip arthroplasty. We included 40 cases (53 hips) of AVN of femoral head operated with Sartorius muscle pedicle iliac bone grafting, done by the senior author. Early post-operative rehabilitation was done. The weight bearing was delayed for 6 weeks. All the patients were followed clinically and radiologically at regular intervals. The operated femoral heads, were grouped according to Ficat’s staging: 24 in stage IIA (45.3%), 22 in stage IIB (41.5%) and 07 in stage III (13.2%). The average duration of surgery was 85 min (range: 55–130 min). The total duration of follow-up was average 4.2 years (range: 2.2–15 years).The Harris hip score was excellent (>90) in 18 hips (33.96%), good (80–89) in 24 hips (45.28%), fair (70–79) in 9 hips (17%) and poor (<70) in 2 hips (3.7%). AVN of the femoral head is a painful and disabling condition in young adults. Sartorius muscle pedicle bone graft technique allows adequate decompression, re vascularization and osteogenesis of the femur head in Ficat’s stage IIa, IIb and III, in young adults. This is an effective and easy technique to adopt with excellent to good results in 80% cases and is associated with only minimal complications.
INTRODUCTION
Avascular necrosis (AVN) of the femoral head is a painful and disabling condition. It mostly affects the people in third and fifth decade of the life [1]. AVN is mostly idiopathic, but it may also be associated with alcohol, corticosteroid abuse, hemoglobinopathies, coagulopathies and certain renal, hepatic and skin disorders [2]. Various hypotheses like vascular interruptions or abnormalities, elevated bone marrow pressure, cellular toxicity, fat emboli etc. have been proposed, but none of them clearly explains its exact aetiopathogenesis [3]. Early clinical and radiological diagnosis is usually difficult, but if done in time, it may prevent further collapse of the femur head and is important for the favorable outcome of the disease [4]. The treatment of AVN is done according to the staging of the disease. The Ficat grading system that is based on the plain X-rays is the most commonly used classification in clinical practice [5]. In the initial stages of the disease, the head preserving surgeries, which aim at reducing the intraosseous pressure and enhancing the vascular supply of the femur head, are preferred. Among these, the core decompression of the femur head is the preferred treatment in Ficat stage I and IIa [6]. Core decompressions reduce intraosseous pressure and thus decrease the pain, but it does not enhance the vascularization of necrosed head adequately, especially in an advanced stage of the disease. Therefore, it is better supplemented with various bone grafting or muscle pedicle grafting techniques, to enhance vascularity and healing of the lesion. There are several techniques described to enhance the vascularization of the femur head, like core decompression with vascularized and non-vascularized bone grafting, various types of muscle pedicle grafts, etc. These procedures have shown favorable results in stages IIa, IIb and III [7].
We present 40 cases (in 53 hips) of core decompression of the femoral head along with Sartorius pedicle bone graft. The procedure involved creating a cortical window at the head and neck junction (‘Light Bulb’ technique) [8], curettage of sclerotic dead bone and fixation of the muscle pedicle bone graft in the cortical window of the neck with cannulated cancellous screws (for Ficat’s stage IIa, IIb and III AVN).
MATERIALS AND METHODS
In this retrospective study, we analysed 47 cases of AVN of femoral head treated with core decompression and Sartorius pedicle bone graft. Seven patients were lost to follow-up and hence were excluded from this study. We had included 40 cases with 53 hips affected with AVN of femur head (of Ficat stage IIa, IIb and III), occurring due to alcoholism, corticosteroid abuse, post-traumatic and idiopathic. We had excluded the cases due to hemoglobinopathies (sickle cell disease and other blood disorders), and Ficat stages I and IV osteonecrosis cases. In all the cases, surgery was performed by the senior author (R.V.). In bilateral cases, surgery was done in single sitting on the fracture table. Post-operatively active and passive range of exercises was started on the second post-operative day, and early non-weight bearing mobilization with a walking aid was allowed. The Harris hip score was evaluated at the final follow-up in all 40 patients. The weight bearing was delayed for 6 weeks. The patients were evaluated by subjective Harris hip scoring for hip function. All the patients were followed clinically and radiologically at regular intervals.
SURGICAL TECHNIQUE
The patient was positioned supine on a fracture table so that image intensifier can be easily used. We used the anterior approach, as described by Smith-Petersen [9]. Lateral femoral cutaneous nerve of the thigh was identified first, in the deep fascia medial to the anterior superior iliac spine (ASIS) and protected with a rubber tape (Fig. 1). Intermuscular plain between tensor fascia lata muscle and Sartorius was then dissected. The ascending branch of the lateral circumflex femoral artery was identified, as it may be injured in this approach. A 2 × 2 cm rectangular bone from ASIS was osteotomized with the help of an oscillating saw, along with the attached Sartorius muscle. The capsule was exposed and incised to reach the hip joint. A rectangular window (slightly smaller than the harvested bone graft) was created in the anterior cortex of neck of the femur, at head and neck junction known as ‘light bulb procedure’. The exact position of the cortical window was confirmed on the image intensifier. The drill holes were carefully made only in the anterior cortex, so as to avoid the stress riser on the posterior neck. Also, special care was taken to preserve a safe distance for 8–10 mm from the infero-medial part of the neck. Multiple drill holes were done with 4.5-mm drill bit into the necrosed area of the femur head through the window, under image intensifier control, and necrotic bone was curetted out with angled curettes (Fig. 2). The harvested Sartorius muscle pedicle was lifted along with a block of ASIS and was delivered beneath the straight head of rectus femoris into the window. The graft was secured temporarily with two guide wires and then fixed with, one or two, 4 mm cannulated cancellous screws. Precaution was taken to avoid violating the medial cortex of the femur and the region around calcar. The placement of screws was done ∼8–10 mm lateral to the medial cortex.
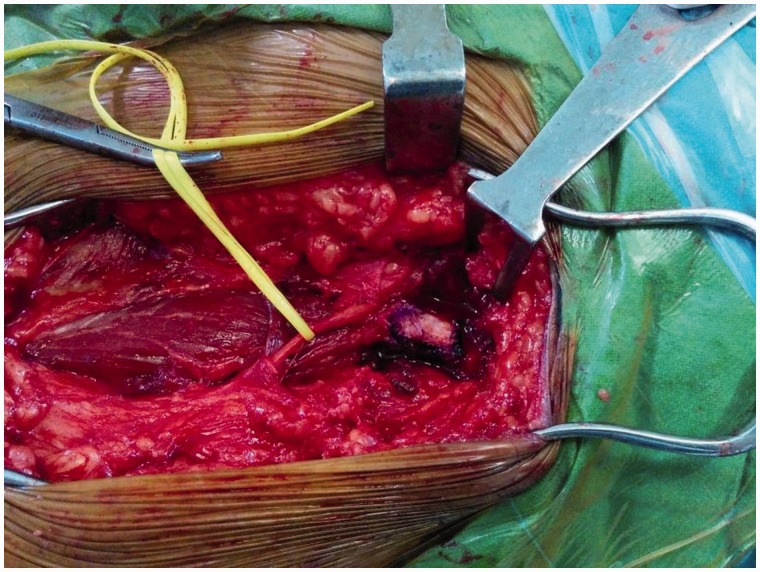
Fig. 1.
Anterior approach to hip (Smith-Petersen), lateral femoral cutaneous nerve of thigh retracted with rubber tape medial to the anterior superior iliac spine.
Fig. 2.
A 3.2-mm drill bit is used for core decompression through window at head neck junction under image intensifier guidance.
RESULTS
We had analysed 53 femoral head in 40 operated patients with AVN, out of which 27 were unilateral (17 right sides and 10 left sides) (Fig. 3) while 13 cases were bilateral. There were 32 males and eight females in this study, with an average age of 31.8 years (range 24–53 years). The main underlying cause of AVN was alcoholism (19 cases), followed by corticosteroid abuse (8 cases) and post-traumatic (7 cases). In 6 cases, the cause was undetermined (idiopathic) (Table I). The operated femoral heads, according to Ficat’s staging were 24 in stage IIA (45.3%), 22 in stage IIB (41.5%) and 7 in stage III (13.2%) (Table II). The average duration of surgery was 85 min (range: 55–130 min). The total duration of follow-up was average 4.2 years (range: 2.2–15 years) (Fig. 4). It was excellent (>90) in 18 hips (33.96%), good (80–89) in 24 hips (45.28%), fair (70–79) in 9 hips (17%) and poor (<70) in 2 hips (3.7%) (Table III). The correlation between the Ficat’s stages and Harris hip score have shown that the majority of hips were showing excellent and good scores belonged to stage IIA and B while the hips with fair and poor score mainly belonged to stage III and IIB (Table IV). To test the hypothesis whether the patient’s Harris’s hip score is independent of their Ficat’s stage at 0.05 significance level. We have used the Pearson’s Chi-squared test. We got P values of 0.004204 and as the P values is less than the 0.05 significance level, we reject the hypothesis that the patients Harris’s hip score is independent of their Ficat’s stage (i.e. they are dependent or related). From the above table, it is clear that higher percentage of patients with Ficat’s stage IIA reported Excellent Score (54.2%) as compared with patients with Ficat’s stage IIB (22.7%) and with Ficat’s stage III (0%).
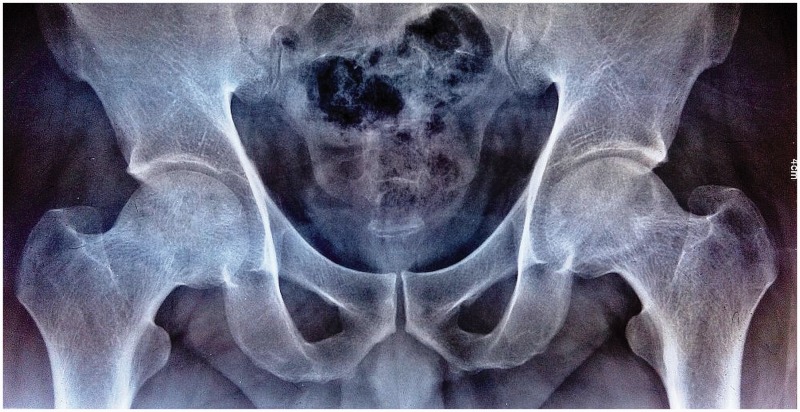
Fig. 3.
X-ray pelvis AP view showing Ficat’s IIa stage of AVN in left femoral head.
Table I.
Distribution of study cases according to etiology
| Cause of AVN | No. of cases | Percentage |
|---|---|---|
| 1. Alcoholism | 19 | 47.5 |
| 2. Corticosteroid abuse | 8 | 20.0 |
| 3. Post-traumatic | 7 | 17.5 |
| 4. Idiopathic | 6 | 15.0 |
Table II.
Distribution of study cases according to Ficat’s staging
| Ficat’s staging of AVN | No. of hips | Percentage |
|---|---|---|
| IIA | 24 | 45.3 |
| IIB | 22 | 41.5 |
| III | 07 | 13.2 |
Fig. 4.
AP view showing 2-year follow-up of the AVN of left femur head operated with Sartorius muscle pedicle bone graft.
Table III.
Evaluation of Harris hip score in study cases
| Harris’s hip score | Result | No. of hips | Percentage |
|---|---|---|---|
| 90–100 | Excellent | 18 | 33.96 |
| 80–89 | Good | 24 | 45.28 |
| 70–79 | Fair | 9 | 16.98 |
| <70 | Poor | 2 | 3.7 |
Table IV.
Correlation of Ficat’s stage with the Harris’s hip score
| Ficat stages | Excellent score (no. of hips) | Good score (no. of hips) | Fair score (no. of hips) | Poor score (no. of hips) |
|---|---|---|---|---|
| IIA | 13 | 10 | 1 | 0 |
| IIB | 5 | 12 | 4 | 1 |
| III | 0 | 2 | 4 | 1 |
In only two femoral heads (3.77%), the AVN progressed from stage IIb and staged III to stage IV, after this surgical procedure. The most common complication of the surgery was an injury to the lateral cutaneous nerve of the thigh which was transient in four cases and recovered fully within three months. One patient had permanent injury to the nerve that failed to recover. There was no case of wound dehiscence, infection or iatrogenic fracture neck of the femur. In two patients, the AVN progressed from stages IIb and III, respectively to stage IV (Table V).
Table V.
Complications in study cases and their frequency distribution
| Complications | No. of cases | Percentage |
|---|---|---|
| Transient injury to lateral cutaneous of thigh | 4 | 7.54 |
| Permanent injury to lateral cutaneous of thigh | 1 | 1.88 |
| Infection/wound dehiscence | 0 | 0.00 |
| Fracture neck of femur | 0 | 0.00 |
| Progression to osteoarthritis (stage IV) | 2 | 3.77 |
DISCUSSION
AVN of the femoral head is a major musculoskeletal problem of younger individuals (Figs. 5 and 6) [10, 11]. If it is left untreated it may progresses to subchondral collapse of the femoral head and secondary hip joint arthritis. The natural progression of the disease is inevitable after the subchondral collapse, and joint space reduction has happened. Therefore, early diagnosis and treatment of AVN may result in the favorable outcome of this disease (Figs. 7 and 8). Medical management of AVN is usually ineffective, although some studies have shown the efficacy of bisphosphonates in the early AVN with the small necrotic lesion [12]. In early stages of the disease, various head preserving surgeries have been described but no treatment has proved completely effective in arresting the disease process. In the advanced stages of AVN, the only satisfactory option remains is total hip arthroplasty (THA) [13].
Fig. 5.
X-ray pelvis AP view showing AVN femoral head, right side with Ficat’s stage IIA and left side with Ficat’s IIB.
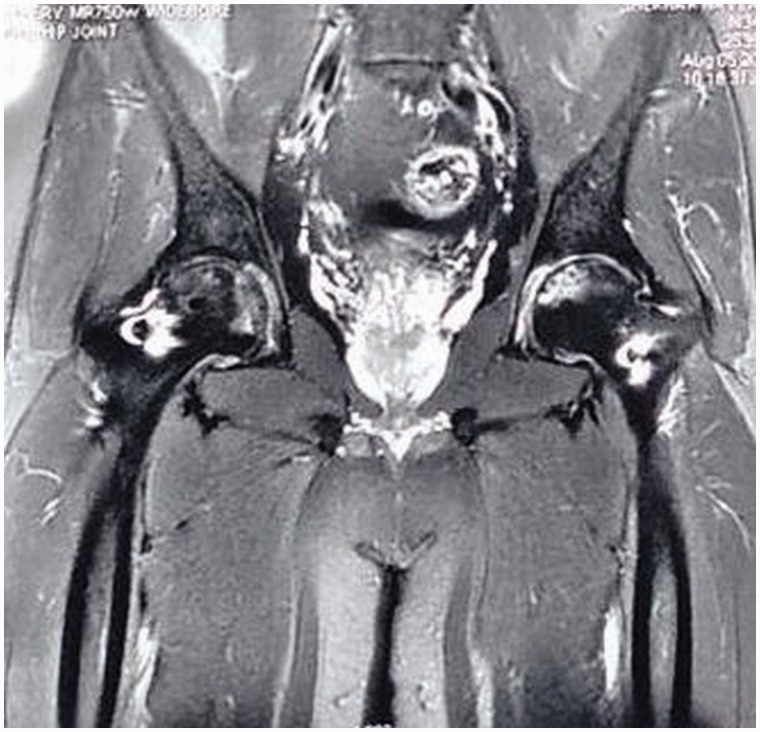
Fig. 6.
MRI both hip joints showing AVN of both femur heads.
Fig. 7.
X-ray pelvis AP view showing 3-year follow-up of AVN both femur head operated with Sartorius muscle pedicle bone graft.
Fig. 8.
X-ray R hip AP view showing 15-year follow-up of AVN femoral head operated with Sartorius muscle pedicle bone graft.
The etiology of AVN has been described to be multi-factorial and may be associated with various risk factors. All the risk factors have an additive effect on the disease progression. Those without any risk factors and obvious cause are labeled as ‘idiopathic AVN’ [14]. In this study, the associated risk factors of alcoholism was found to be (47.5%) while corticosteroid abuse in (20%), traumatic (17.5%), idiopathic (15%). Alcoholism (consuming up to 400 ml per week) has been reported as a major risk factor for AVN of the femoral head [15]. Exposure to alcohol consumption and corticosteroid account for 90% of all causes of AVN has been reported in [16]. The sickle cell hemoglobinopathy is a microangiopathic disease that causes necrosis of the femur head due to occlusion of the intraosseous blood vessels by the sickle-shaped red blood cells [17]. Also, the disease causes obstruction of the small vessels of the surrounding soft tissue and muscles, thus reducing the effectiveness of the surrounding muscle pedicle grafts and hence sickle cell disease patients were excluded from our study.
The classification or the staging system of AVN of the femoral head is important to plan its treatment. There are various described classification systems for AVN of the femoral head. The most commonly used classification in clinical practice is Ficat’s classification system. We have used Ficat’s classification since it is simple, easy to use and has good reproducibility. It grades the disease process into four stages [18].
The aim of treatment in early stages of AVN of the femoral head is to perform the head-preserving procedure by reducing the intraosseous pressure and enhancing the vascular supply of the femur head. A commonly done procedure of core decompression of the head was reported with a promising result, initially by Hungerford [19]. It is done with the aim, to decrease the intraosseous pressure in the early disease process, but its results are much less predictable in more advanced disease (stages IIb and III).The effectiveness of core decompression has always been a controversy in the literature. The long-term results have shown that core decompression gives only temporary relief in pain but does not prevent the progression of the collapse of femoral head [20]. Hence, its use, in isolation, to revascularize the femoral head in AVN is questionable and cannot rely upon.
Buckley et al. [21] have reported good outcomes, with the use of cortico-cancellous bone graft along with core decompression in Ficat stages I and IIA. They used tibial autogenous graft, fibular autogenous and fibular allograft. However, they have shown poor outcome in advanced stage (IIA and III). Also, these are associated with complications like perforation of the subchondral bone during drilling or graft impaction, injury to the common peroneal nerve [22].
Various free vascularized grafts for the treatment of AVN of femoral head have been described to achieve adequate vascularization in the necrosed femoral head. Urbanaik et al. [23] have used fibula (with peroneal vascular pedicle), while Babulkar et al. [24] had used iliac crest (using deep circumflex iliac vessel). These procedures require preoperative angiography to confirm the presence of patent artery for anastomosis. They have shown good clinical and radiological outcome with free vascularized bone grafts have in Ficat stages IIb, III and IV. However, these procedures are technically demanding, tedious and time-consuming and may not be feasible bilaterally, in one sitting [25].
To overcome the shortcomings of vascularized grafts, various types of muscle pedicle grafting procedures, (after core decompression) have been described. These procedures have shown favorable outcomes in early stages of the disease, with revascularization of the femoral head and prevention of collapse. The described muscle pedicle graft technique includes Meyer’s procedure (using quadratus femoris muscle pedicle along with free cancellous bone graft) [26]. This technique has good outcome in early stages but has a poor outcome in advanced stages. Moreover, use of cancellous bone graft does not provide structural support to the subchondral bone. Baksi’s procedure uses tensor fascia lata graft along with iliac crest bone graft [27], after decompression of necrosed femur head with multiple holes. The shortcoming of graft slippage has been reported in other studies as it does not include fixation of the graft.
Sartorius muscle pedicle bone graft for the revascularization of the necrosed femur head is relatively unknown technique in the literature and has only been studied by Li et al. [28]. In this study, we found that Sartorius muscle pedicle bone graft is an effective and easy surgery to perform. Additionally, the bilateral hip can be operated at the same sitting, and no changing of position is required after operating one side hip, this significantly reduces operating time. Sartorius’ muscle has a good blood supply, in the form of series of equal size and segmental pedicles that enter the muscle along its course [29]. Therefore, transposition of the muscle flap along with bone chip of ASIS does not hamper its blood supply and provide an adequate vascular bed to the femur head. Also, adequate length of the muscle flap can be transposed without any tension on its arteries (Table VI). The core decompression was done through the cortical window created at head and neck junction known as ‘light bulb’ technique. The term ‘light bulb’ procedure was introduced by Rosenwasser et al. [30], who attempted to perform this procedure of curettage and grafting through neck head junction. Multiple drilling provides decompression of the avascular lesion and removal of the necrotic bone in order to interrupt the cycle of ischaemia and interosseous hypertension. Intra-operative image intensifier along with clinical judgment is used is to check the extent of necrotic bone removal.
Table VI.
Pros and cons of various muscle pedicle grafts around the hip
| Sartotius | Tensor fascia lata | Quadrtus femoris | |
|---|---|---|---|
| Harvesting of graft | Easy | Tedious | Tedious |
| Length of the graft | Good | Just sufficient | Just sufficient |
| Nature of graft | Cortical | Cortical | Cancellous |
| Complication rate | Low | Average | Not documented |
This allowed sufficient decompression by adequate removal of the necrotic subchondral bone of the head of the femur at the weight bearing area. Another distinguishing feature reported in our study is the fixation of the graft with one or two 4-mm cannulated cancellous screws; this prevents slippage of the graft from the femoral neck window and has not been discussed in any other studies of the muscle pedicle bone graft (Table VII). The procedure provides decompression of the avascular lesion and removal of the necrotic bone in order to interrupt the cycle of ischaemia and interosseous hypertension. Grafting of the defect with Sartorius muscle pedicle bone introduces a scaffold for repair and remodeling of subchondral bone. This procedure has been more appealing than that of a vascularized graft because it is less technically demanding and may reduce donor-site morbidity.
Table VII.
Comparison of studies done for muscle pedicle graft in AVN of femur head
| Studies | Graft used | Results excellent to good | Poor results |
|---|---|---|---|
| Meyer et al. | Quadratusfemoris Muscle pedicle graft | 57% success rate (Harris hip score was not used) | Not mentioned |
| Bakshi et al. | TFL muscle pedicle bone graft | Excellent: 31% | Poor: 6% |
| Good: 53% | |||
| Fair: 10.3% | |||
| (Harris hip score was not used) | |||
| Li et al. | Sartorius muscle pedicle iliac bone graft | Excellent: 33% | Poor: 2.9% |
| Good: 48.5% | |||
| Fair: 14.7% | |||
| Urbanaik et al. | Free vascularized fibular graft | Avg. Harris hip score improved in all case (P ≤ 0.0001) compared with pre-operative values. | Not mentioned |
| Vaishya et al. (present series) | Sartorius muscle pedicle iliac bone graft | Excellent: 33.96% | Poor: 3.7% |
| Good: 45.28% | |||
| Fair: 16.98% |
The newer techniques describing the use of autologous stem cells from the iliac crest and Platelet-rich plasma, for the necrosed area of the femoral head, have shown very good results in early stages (pre-collapse) of the disease. There results in advanced stage (post-collapse) of the disease are unsatisfactory [31]. A randomized control study is needed to compare their result with other treatment modalities in AVN of the femoral head [32]. Due to ethical and biological reasons the clinical application of the progenitor cells in musculoskeletal system is limited to autologous stem cells while the totipotent embryonic stem cells are used only in experimental studies [33].
Although THA has been shown to give excellent results in the late stages of AVN, the limited life span of these prostheses in younger patients with AVN remains a cause for concern. Thus, a revascularizing procedure that can help preserve the head will help postpone or alleviate the need for THA (Fig. 9). Coincidentally, with increased awareness of the treating physician and improved diagnostic modalities, more and more patients are being diagnosed with early stage AVN where the head preserving surgeries can have a definite role. Thus, the identification of an ideal procedure for the early stage AVN can help in decreased morbidity and improved outcomes. To conclude, Sartorius pedicle graft in AVN of femur head after drilling through cortical window is characterized by simple surgical technique, low incidence of complication and a short duration of operation. It has the advantage of addressing both the issues of decompression of femoral head as well as providing vascularized bone graft.
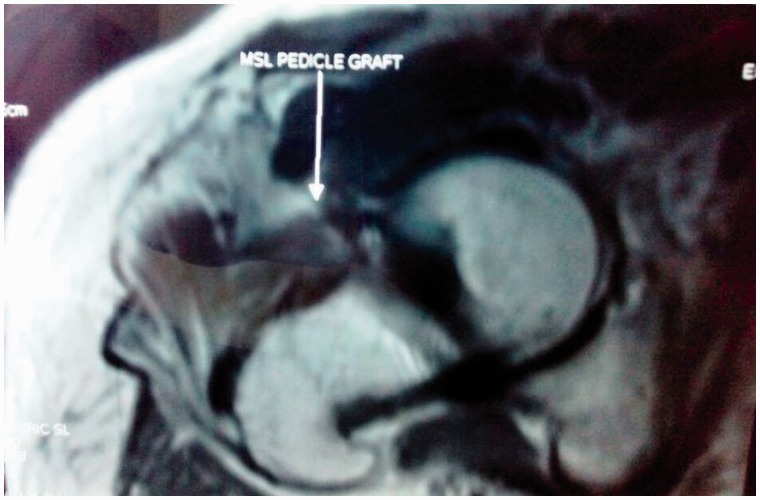
Fig. 9.
MRI of Right hip showing intact muscle pedicle with viable femoral head in a 15-year follow-up patient.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Herndon JH, Aufranc OE. Avascular necrosis of the femoral head in the adult. A review of its incidence in a variety of conditions. Clin Orthop 1972; 86: 43–62. [DOI] [PubMed] [Google Scholar]
- 2.Glimcher MJ, Kenzora JE. The biology of osteonecrosis of the human femoral head and its clinical implications: part III. Discussion of the etiology and genesis of the pathological sequelae; comments on treatment. Clin Orthop 1979; 140: 273–312. [PubMed] [Google Scholar]
- 3.Dabov G. Osteonecrosis. In: Canale ST, Beaty JH, editors. Campbell’s Operative Orthopaedics. 11th edn. Philadelphia: Mosby;2008. p.1032–40. [Google Scholar]
- 4.Tripathy SK, Goyal T, Sen RK. et al. Management of femoral head osteonecrosis: Current concepts. Indian J Orthop 2015; 49:28–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jawad MU, Haleem A, Scully SP. Ficat Classification: Avascular Necrosis of the Femoral Head. Clin Orthop Relat Res 2012; 470: 2636–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fairbank AC, Bhatia D, Jinnah RH. et al. Long-term results of core decompression for ischaemic necrosis of the femoral head. J Bone Joint Surg Br 1994; 76-B: 42–9. [PubMed] [Google Scholar]
- 7.Mont MA, Hungerford DS. Non traumatic avascular necrosis of femoral head. J Bone Joint Surg Am 1995; 77A: 459–74. [DOI] [PubMed] [Google Scholar]
- 8.Rosenwasser MP, Garino JP, Kiernan HA. et al. Long term followup of through debridement and cancellous bone grafting of the femoral head for avascular necrosis. Clin Orthop Relat Res 1994;306:17–27. [PubMed] [Google Scholar]
- 9.Smith-Petersen MN. Approach to and exposure of the hip joint for mold arthroplasty. J Bone Joint Surg Am 1949; 31A: 40–6. [PubMed] [Google Scholar]
- 10.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures. Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969; 51: 737–55. [PubMed] [Google Scholar]
- 11.Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg 2014; 22: 455–64. [DOI] [PubMed] [Google Scholar]
- 12.Luo RB, Lin T, Zhong HM. et al. Evidence for using alendronate to treat adult avascular necrosis of the femoral head: a systematic review. Med Sci Monit 2014; 20: 2439–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Issa K, Pivec R, Kapadia BH. et al. Osteonecrosis of the femoral head: the total hip replacement solution. Bone Joint J 2013; 95-B: 46–50. [DOI] [PubMed] [Google Scholar]
- 14.Patterson RJ, Bickel WH, Dahlin DC. et al. Idiopathic avascular necrosis of the head of the femur. J Bone Joint Surg Am 1964; 46: 267–82. [PubMed] [Google Scholar]
- 15.Matsuo K, Hirokata T, Sugioka Y. et al. Influence of alcohol intake cigarette smoking and occupational status on idiopathic osteonecrosis of the femoral head. Clin.Orthop 1988; 234: 115–23. [PubMed] [Google Scholar]
- 16.Cruess RL. Steroid-induced osteonecrosis: a review. Can J Surg 1981; 24:567–71. [PubMed] [Google Scholar]
- 17.Milner PF, Kraus AP, Sebes JI. et al. Sickle cell disease as a cause of osteonecrosis of the femoral head. N Engl J Med 1991; 325: 1476–81. [DOI] [PubMed] [Google Scholar]
- 18.Ficat RP. Idiopathic bone necrosis of the femoral head, early diagnosis and treatment. J Bone Joint Surg Br 1985; 67B: 3–9. [DOI] [PubMed] [Google Scholar]
- 19.Hungerford DS. Response: the role of core decompression in the treatment of ischemic necrosis of the femoral head. Arthritis Rheum 1989; 32: 801–6. [DOI] [PubMed] [Google Scholar]
- 20.Koo KH, Kim R, Ko GH. et al. Preventing collapse in early osteonecrosis of the femoral head: a randomized clinical trial of core decompression. J Bone Joint Surg Br 1995; 77: 870–4. [PubMed] [Google Scholar]
- 21.Buckley PD, Gearen PF, Petty RW. Structural bone-grafting for early atraumatic avascular necrosis of the femoral head. J Bone Joint Surg Am 1991; 73: 1357–64. [PubMed] [Google Scholar]
- 22.Keizer SB, Kock NB, Dijkstra PDS. et al. Treatment of avascular necrosis of the hip by a non-vascularised cortical graft. J Bone Joint Surg [Br] 2006; 88-B: 460–6. [DOI] [PubMed] [Google Scholar]
- 23.Urbaniak JR, Coogan PG, Gunneson EB. et al. Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting. A long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am 1995; 77: 681–94. [DOI] [PubMed] [Google Scholar]
- 24.Babhulkar SS. Osteonecrosis of femoral head. Treatment by core decompression and vascular pedicle grafting. Indian J Orthop 2009; 43: 27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Babhulkar S. Osteonecrosis femoral head treatment by core decompression and iliac crest-TFL muscle pedicle grafting. In: Zorzi A, editors. Bone Grafting. 1st edn. Croatia: InTech; 2012. p. 108–124. [Google Scholar]
- 26.Meyers MH. The treatment of osteonecrosis of the hip with fresh osteochondral allografts and with the muscle-pedicle graft technique. Clini Orthop 1978; 130: 202–9. [PubMed] [Google Scholar]
- 27.Baksi DP. Treatment of osteonecrosis of the femoral head by drilling and muscle pedicle bone grafting. J Bone Joint Surg Br 1991; 73B: 241–5. [DOI] [PubMed] [Google Scholar]
- 28.Zhou L, Tan J, Li Y. Treating avascular necrosis of femoral head in young adult by grafting sartorius muscle iliac bone flap. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2007; 21: 814–6. [PubMed] [Google Scholar]
- 29.Ng D, Vesely M. The free sartorius flap: clinical cases and anatomical study. J Plast Reconstr Aesthet Surg 2012; 65: 1671–7. [DOI] [PubMed] [Google Scholar]
- 30.Rosenwasser MP, Garino JP, Kiernan HA. et al. Long term follow-up of thorough debridement and cancellous bone grafting of the femoral head for avascular necrosis. Clin Orthop Relat Res 1994; 306: 17–27. [PubMed] [Google Scholar]
- 31.Hernigou P, Beaujean F. Treatment of osteonecrosis with autologus bone marrow grafting. Clin Orthop Relat Res 2002;405: 14–23. [DOI] [PubMed] [Google Scholar]
- 32.Yan ZQ, Chen YS, Li WJ. et al. Treatment of osteonecrosis of the femoral head by percutaneous decompression and autologus bone marrow mononuclear cell infusion. Chin J Traumatol 2006; 9: 3–7. [PubMed] [Google Scholar]
- 33.Jager M, Hernigou P, Zilkens C. et al. Cell therapy in bone healing disorders. Orthop Rev 2010; 2: e20. 79-87. [DOI] [PMC free article] [PubMed] [Google Scholar]