Abstract
Background
Although many orthodontists have no doubts about the effectiveness of functional appliances for mandibular advancement, the impact on the temporomandibular joint (TMJ) is still in dispute. The objective of this systematic review is to examine the main effects on the TMJ of using functional appliances, both in healthy patients and in patients with a pre-existing disorder.
Material and Methods
A systematic review of the literature was conducted in accordance with the PRISMA guidelines. Only systematic reviews, meta-analyses, randomized clinical trials (RCTs), case-control studies and cohort studies were included. A detailed language-independent electronic search was conducted in the Pubmed, Scopus, Cochrane Library and Embase databases. All studies published between 2000 and 2015 were included.
Results
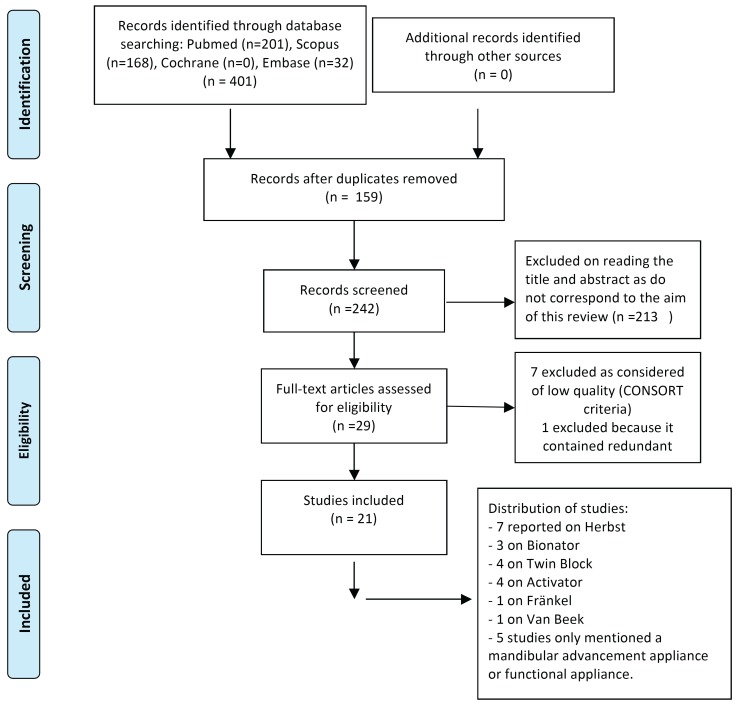
A total of 401 articles were identified. Of these, 159 were duplicates and were excluded. On reading the title and abstract, 213 articles were excluded because they did not answer the research question, leaving a total of 29 articles. These articles were read and assessed. Following critical reading of the full text, eight articles were excluded: seven because they were considered of low quality and one because it published redundant data. As a result, 21 articles were included.
Conclusions
After treatment with functional appliances, the condyle was found to be in a more advanced position, with remodelling of the condyle and adaptation of the morphology of the glenoid fossa. No significant adverse effects on the TMJ were observed in healthy patients and the appliances could improve joints that initially presented forward dislocation of the disk.
Key words:Temporomandibular joint, TMJ, orthodontic appliances, functional, mandibular advancement, herbst appliance, bionator.
Introduction
The use of a mandibular advancement appliance to correct skeletal malocclusions associated with mandibular retrognathism is indicated during the first stage of orthodontic treatment (1). The objective is to stimulate mandibular growth and correct the sagittal misalignment by bringing the condyles forward and downward within the glenoid fossa (2,3), as well as remodelling the condyle and glenoid fossa, causing anterior rotation of the mandible and consequently projecting it forwards (4). During this first stage, mandibular retrognathism can be treated with either fixed or removable functional appliances (3,5). The treatment period lasts approximately 6 to 9 months (4).
When the functional appliance is inserted, the condyles are moved to a higher position in the articular eminence, which is capable of adaptation, so it could be hypothesized that some morphological changes may take place (6).
Although many orthodontists have no doubts about the effectiveness of functional appliances, their impact on the TMJ is still considered a subject of debate. It is therefore of clinical and scientific interest to investigate the most relevant effects of different functional appliances on the TMJ, particularly with current diagnostic methods. Many authors assert that treatment with these devices does not increase the prevalence of temporomandibular disorders (1,7-9). Another important aspect is the positive or negative effect that functional appliances may have on the TMJ of patients with a preexisting disorder (1).
The main objective of this systematic review is to examine the main effects on the TMJ of different functional appliances for mandibular advancement, both in healthy patients and in patients with a pre-existing disorder.
Material and Methods
A systematic review of the bibliography was carried out in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) recommendations (10) and CONSORT criteria (11).
- Eligibility criteria
The selection criteria for inclusion in the review were: articles, articles in press and reviews. Only the following types of study were accepted: systematic reviews, meta-analyses, randomized clinical trials (RCTs), case-control studies and cohort studies. Both retrospective and prospective studies were included. The articles that met these criteria and studied changes in the temporomandibular joint following the use of functional appliances for mandibular advancement were included in the review.
- Search strategy and screening
To identify the relevant studies, irrespective of language, a thorough electronic search was conducted in the Pubmed, Scopus, Cochrane Library and Embase databases. All studies published between 2000 and 2015 were included. The search was updated on 4 July 2015.
The search strategy was implemented through a combination of the following 6 MeSH terms: “Temporomandibular joint”, “TMJ”, “Functional orthodontic appliances”, “Mandibular advancement”, “Herbst appliance”, “Bionator” and “Activator appliances”, and others: “Fränkel Function Regulator”, “Orthodontic Appliances”, “Activator”, “Function Activator”, “Bionator Appliance”, “Functional Orthodontic” and “Twin Block”. The TMJ related terms were combined using the OR Boolean operator, as well as those related to the mandibular advancement devices. Both groups were combined using the AND Boolean operator. Hand-searching in the reference lists of the articles assessed for the review was also carried out.
Two independent reviewers assessed the titles and abstracts of all the articles selected. In the event of their disagreeing, a third reviewer was consulted. If the abstract did not provide sufficient information for a decision, the reviewers read the full article before taking the final decision. The reviewers then read the full text of all the resulting articles.
- Data extraction
For each article assessed, the following variables were recorded: author, year published, type of study (retrospective, prospective, controlled, not controlled), sample size, dropouts, demographic variables (gender, age), type of appliance used, type of advancement (sequential or otherwise), presence or otherwise of preexisting TMJ disorders, length of treatment, type of radiographic study used to study the changes, follow-up time for each study and quality of the articles accepted ( Table 1). The articles were classified as being of high, medium or low quality according to the CONSORT criteria (11) adapted by Mattos et al. (12) and used by Fernández-Ferrer et al. and Serra-Torres et al. (13,14). The quality of the systematic reviews was assessed in accordance with the PRISMA guidelines (10).
Table 1. Articles included, with information from each.
Results
A thorough search identified 201 articles in Medline, 168 in Scopus, none in the Cochrane Library and 32 in Embase, making a total of 401 articles. 159 duplicates were removed, leaving 242. After reading the title and abstract, 213 were removed because they did not answer the research question, leaving a total of 29 articles. These were read and carefully assessed. Detailed critical reading of the full text resulted in the exclusion of 8 articles, 7 because of their low quality (Fig. 1) and 1 because it published redundant data. Consequently, 21 articles that met all the inclusion criteria and were of medium to high quality were included in the review. It should be mentioned that the manual search did not identify any relevant articles.
Figure 1.
Flow diagram.
Regarding the type of study reported in the 21 articles, 1 was a systematic review, 1 was a retrospective study and 19 were prospective studies. Of the prospective studies, 8 were controlled and 11 were not controlled ( Table 1).
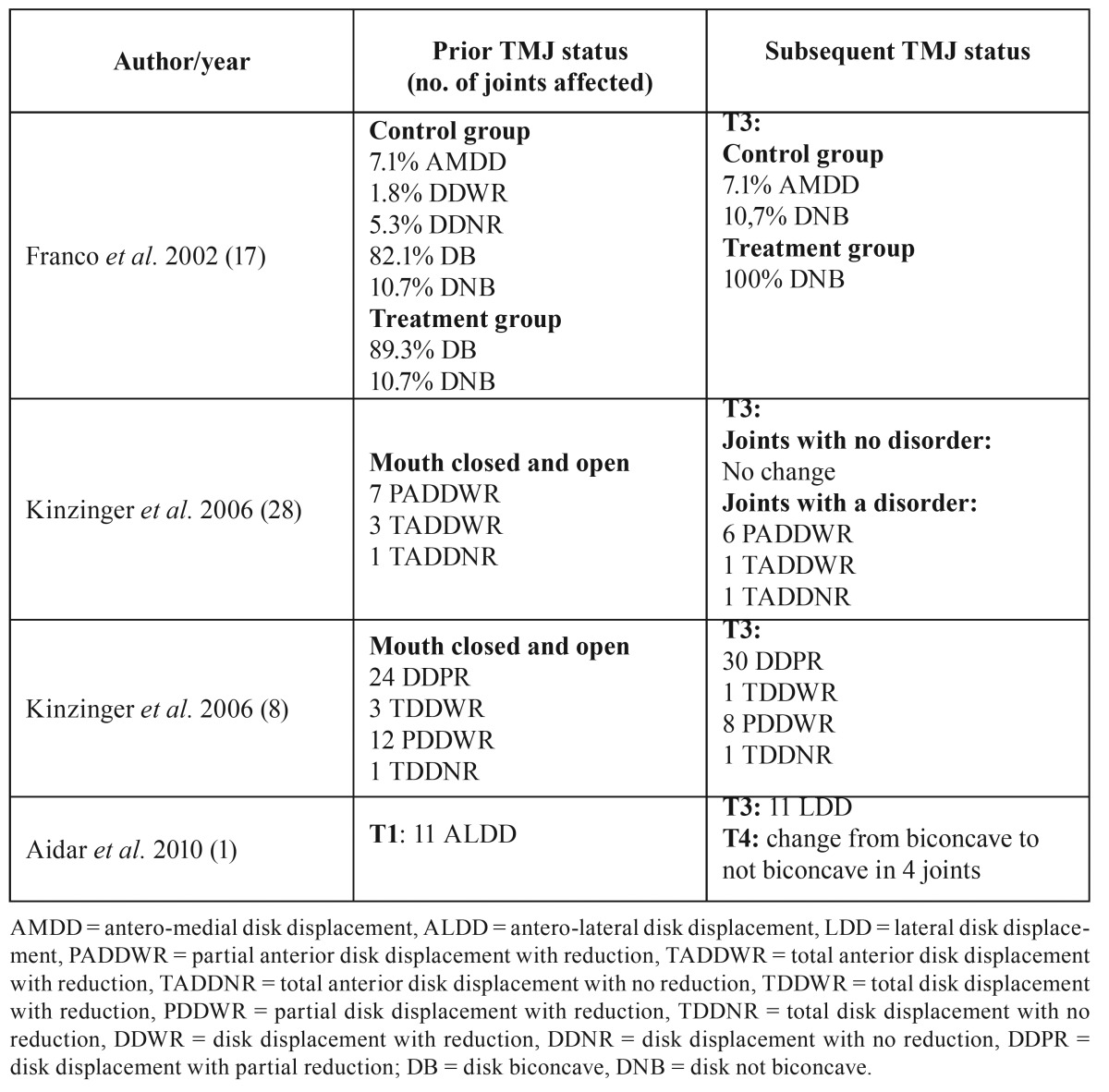
Concerning the state of the joint immediately prior to treatment, leaving aside the systematic review, only 8 of the studies explicitly mentioned its condition. Of these, 4 studied healthy joints and 4 studied joints with certain disorders ( Table 2). The remaining 12 studies made no mention of joint status.
Table 2. Articles included, with information on pre-existing conditions.
With regard to the type of appliance used, 7 studies used the Herbst appliance. Of these, 5 did not use control groups, 1 compared it with a functional advancement device and 1 with the Activator. The Bionator was studied in 3 articles, comparing it with the Twin Block in 2 cases. Two studies concerned the Twin Block alone, a further two the Activator alone and one the Fränkel, while another compared the Activator with the Van Beek. Three other articles did not name the type of appliance, mentioning only a functional or mandibular advancement appliance.
Only three studies specified the type of mandibular advancement (sequential or one-step).
In relation to the type of diagnostic study, 8 used magnetic resonance, 2 CBCT, 1 SPECT (single-proton emission computed tomography), 6 cephalometric tracing, 1 magnetic resonance together with manual examination, 1 magnetic resonance as well as cephalometric tracing and wrist radiographs, and 1 used magnetic resonance and teleradiography.
Regarding the quality of the articles, 19 were of moderate quality and one of high quality. The systematic review was considered of high quality. The main conclusions drawn by the authors of the studies included in the present review are shown in Table 3.
Table 3. Studies by observations.
Discussion
- Changes in disk shape and position
According to Wadhawan et al. (15), the anterior repositioning of the condyle in the glenoid fossa caused by functional appliances results in stretching of the retrodiscal tissue that could lead to changes in the shape of the disk or its posterior displacement, which agrees with the study by Chavan et al. (16). However, Aidar et al. (1) found no significant changes in disk position after treatment with the Herbst appliance. Franco et al. (17) observed no changes in comparison with the control group whether in healthy patients or in patients with antero-medial disk displacement, coinciding with the systematic review by Popowich et al. (18) and the study by Chintakanon et al. (19). Aidar et al. (9), in a previous study, made the same observation following 12 months’ use of the Herbst appliance in adolescents whose disks were within the normal limits prior to treatment. In patients with prior disk displacement, these authors observed that it was not recaptured. However, Kinzinger et al. (20), using magnetic resonance, observed significant improvements in joints with an initial forward disk dislocation, agreeing with Kinzinger et al. (8), who also observed a lack of adverse effects in patients with a good initial condyle-disk relationship, as did Katsavrias et al. (6). Pancherz et al. (21) performed the same observation and indicated that the improvement in disk position depended on the extent of the initial displacement.
Concerning disk shape, Aidar et al. (9) reported a lack of adverse effects on articular disk morphology. Subsequently, the same authors (1) reached the same conclusion despite finding adverse effects in some patients at the end of the treatment, such as a change in disk shape from biconcave to not biconcave. Franco et al. (17), using magnetic resonance, observed that at the end of the treatment the number of biconcave discs had increased significantly in the patients treated with Fränkel appliances. As a result, they indicated that the use of this appliance at the beginning of the growth stage could help avoid future intra-TMJ problems.
- Changes in condyle size and position
In a case-control study of treatment with the Herbst appliance, Le Cornu et al. (3) observed forward adaptive displacement of the condyles followed by remodelling of the glenoid fossa, compared with a control group that was only treated with fixed devices and class II elastic bands. These findings agree with those of Chintakanon et al. (19) and Chavan et al. (16). The latter conducted a controlled study using magnetic resonance and observed a more forward condyle position, although they recommended long-term follow-up to investigate the stability of their findings. In the same way, Pancherz et al. (22) observed that changes in condyle growth were greater in men than in women and highlighted that treatment with the Herbst appliance temporarily stimulated condyle growth. A year later, in a new study of 118 patients classified according to their growth pattern, Pancherz et al. (22) concluded that condyle growth took place and was more posterior in hyperdivergent than in hypodivergent subjects.
In contrast to the above observations, Kinzinger et al. (20) found no significant differences in the glenoid fossa-condyle relationship before and after treatment. Wadhawan et al. (15), using magnetic resonance, observed that the condyle and disk were displaced during treatment but returned to their initial position when the treatment ended. The systematic review by Popowich et al. (18) also concluded that the changes in condyle position were not clinically significant.
- Changes in the glenoid fossa
Pancherz et al. (21) observed antero-inferior displacement of the glenoid fossa as a reaction to the Herbst treatment. These authors asserted that the Herbst had an effect on the physiological growth of the fossa, temporarily displacing it forwards. However, the review by Popowich et al. (18) concluded that remodelling of the glenoid fossa had not been established, which agrees with the findings of Chintakanon et al. (19). Focusing on patients with different growth patterns, Pancherz et al. (22) concluded that there were no significant changes in the glenoid fossa between hyper- and hypodivergent subjects.
- Changes in the articular eminence and other changes
Reports on adaptations of the articular eminence caused by functional appliances are scarce. Katsavrias et al. (6) highlighted that the height of the articular eminence was not affected and that its angle suffered minor changes, but that these were insignificant.
With regard to other changes that may take place, according to the study by Le Cornu et al. (3) the Herbst appliance wearers exhibited restricted maxillary growth compared to the control group. Also, no great differences were found in the mandibular body and the growth of the ramus, in condyle flexibility or in changes in gonial angle. In contrast, Yildirim et al. (23) observed that treatment with the Twin Block increased the volume of the condyle, the length of the mandible and the inter-condyle distance due to stimulation of condyle growth upwards and backwards.
- Limitations of this review
The scientific evidence collected on changes in the TMJ following the use of functional appliances was not abundant despite the thorough systematic search for articles that met the strict inclusion criteria and presented medium to high quality according to the CONSORT criteria.
TMJ status is a particularly important subject, yet this review has shown a lack of randomized controlled trials with long-term follow-up using diagnostic tests such as magnetic resonance and computed tomography to establish the effects of the functional appliance in a reliable way.
The articles included in the review show a lack of methodological homogeneity. For instance, Aidar et al. (9), Kinzinger et al. (20) and Wadhawan et al. (15) used magnetic resonance as a diagnostic method, while others such as Le Cornu et al. (3) and Arici et al. (24) used CBCT. Yet others, like Baltromejus et al. (5) and Güner et al. (2), used cephalometric tracing. Many others, such as Arat et al. (25), preferred to use several methods to increase the accuracy of the results.
They also employed different appliances: while the great majority used the Herbst, others studied removable appliances such as Twin Block, Bionator (15,16), Fränkel (17) or Activator (25). Only one of the studies (5) compared fixed and removable appliances, namely Activator and Herbst, concluding that the Herbst appliance corrected the sagittal problems in less time than the Activator.
Additionally, the sample size was small in most of these studies: Le Cornu et al. (3) studied 14 patients, Ruf et al. (26) 40 patients and Katsavrias et al. (6) 35 patients. Watted et al. (27) and Kinzinger et al. (28) studied 15 patients. The study with the largest sample size was Baltromejus et al. (5), with 138 cases.
Conclusions
• Following this review, it may be concluded that observations after treatment with functional appliances for mandibular advancement have found the condyle in a more advanced position, condyle remodelling and adaptation of the morphology of the glenoid fossa.
• No significant adverse events concerning the temporomandibular joint have been found in healthy patients, and this treatment could improve joints that initially presented forward disk dislocation.
Acknowledgments
The authors have no funding, financial relationships, or conflicts of interest to disclose. The manuscript was translated into English by Mary Georgina Hardinge.
References
- 1.Aidar LA, Dominguez GC, Yamashita HK, Abrahão M. Changes in temporomandibular joint disc position and form following Herbst and fixed orthodontic treatment. Angle Orthod. 2010;80:843–52. doi: 10.2319/093009-545.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Güner D, Öztürk Y, Sayman HB. Evaluation of the effects of functional orthopaedic treatment on temporomandibular joint with single- proton emission computerized tomography. Eur J Orthod. 2003;25:9–12. doi: 10.1093/ejo/25.1.9. [DOI] [PubMed] [Google Scholar]
- 3.Le Cornu M, Cevidanes LHS, Zhu H, Wu C, Larson B, Nguyenf T. Three-dimensional treatment outcomes in Class II patients treated with the Herbst appliance: A pilot study. Am J Orthod Dentofacial Orthop. 2013;144:818–30. doi: 10.1016/j.ajodo.2013.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Serbesis-Tsarudis C, Pancherz H. ''Effective'' TMJ and chin position changes in Class II treatment. Angle Orthod. 2008;78:813–8. doi: 10.2319/082707-391.1. [DOI] [PubMed] [Google Scholar]
- 5.Baltromejus S, Ruf S, Pancherz H. Effective temporomandibular joint growth and chin position changes: Activator versus Herbst treatment. A cephalometric roentgenographic study. Eur J Orthod. 2002;24:627–37. doi: 10.1093/ejo/24.6.627. [DOI] [PubMed] [Google Scholar]
- 6.Katsavrias EG. The effect of mandibular protrusive (activator) appliances on articular eminence morphology. Angle Orthod. 2003;73:647–53. doi: 10.1043/0003-3219(2003)073<0647:TEOMPA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Kinzinger G, Roth A, Gülden N, Bucker A, Diedrich P. Effects of orthodontic treatment with fixed functional orthopaedic appliances on the condyle-fossa relationship in the temporomandibular joint: a magnetic resonance imaging study (Part I) Dentomaxillofac Radiol. 2006;35:339–46. doi: 10.1259/dmfr/53048233. [DOI] [PubMed] [Google Scholar]
- 8.Kinzinger GS, Roth A, Gülden N, Bücker A, Diedrich PR. Effects of orthodontic treatment with fixed functional orthopaedic appliances on the disc-condyle relationship in the temporomandibular joint: a magnetic resonance imaging study (Part II) Dentomaxillofac Radiol. 2006;35:347–56. doi: 10.1259/dmfr/70972585. [DOI] [PubMed] [Google Scholar]
- 9.Aidar LAA, Dominguez GC, Abrahao M, Yamashita HK, Vigorito JW. Effects of Herbst appliance treatment on temporomandibular joint disc position and morphology: A prospective magnetic resonance imaging study. Am J Orthod Dentofacial Orthop. 2009;136:412–24. doi: 10.1016/j.ajodo.2007.12.027. [DOI] [PubMed] [Google Scholar]
- 10.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mattos CT, Vilani GNL, Sant'Anna EF, Ruellas ACO, Maia LC. Effects of orthognathic surgery on oropharyngeal airway: a meta-analysis. Int J Oral Maxillofac Surg. 2011;40:1347–56. doi: 10.1016/j.ijom.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 13.Fernández-Ferrer L, Montiel-Company JM, Pinho T, Almerich-Silla JM, Bellot-Arcís C. Effects of mandibular setback surgery on upper airway dimensions and their influence on obstructive sleep apnoea - a systematic review. J Craniomaxillofac Surg. 2015;43:248–53. doi: 10.1016/j.jcms.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 14.Serra-Torres S, Bellot-Arcís C, Montiel-Company JM, Marco-Algarra J, Almerich-Silla JM. Effectiveness of mandibular advancement appliances in treating obstructive sleep apnea syndrome: A systematic review. Laryngoscope. 2016;126:507–14. doi: 10.1002/lary.25505. [DOI] [PubMed] [Google Scholar]
- 15.Wadhawan N, Kumar S, Kharbanda OP, Duggal R, Sharma R. Temporomandibular joint adaptations following two-phase therapy: an MRI study. Orthod Craniofac Res. 2008;11:235–50. doi: 10.1111/j.1601-6343.2008.00436.x. [DOI] [PubMed] [Google Scholar]
- 16.Chavan S, Bhad W, Doshi U. Comparison of temporomandibular joint changes in Twin Block and Bionator appliance therapy: a magnetic resonance imaging study. Prog Orthod. 2014;15:57. doi: 10.1186/s40510-014-0057-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Franco A, Yamashita H, Lederman H, Cevidanes LHS, Proffit W, Vigorito JW. Fränkel appliance therapy and the temporomandibular disc: A prospective magnetic resonance imaging study. Am J Orthod Dentofacial Orthop. 2002;121:447–57. doi: 10.1067/mod.2002.122241. [DOI] [PubMed] [Google Scholar]
- 18.Popowich KDMD, Nebbe B. Effect of Herbst treatment on temporomandibular joint morphology: A systematic literature review. Am J Orthod Dentofacial Orthop. 2003;123:388–94. doi: 10.1067/mod.2003.89. [DOI] [PubMed] [Google Scholar]
- 19.Chintakanon K, Sampson W, Wilkinson T, Townsend T. A prospective study of Twin-block appliance therapy assessed by magnetic resonance imaging. Am J Orthod Dentofacial Orthop. 2000;118:494–504. doi: 10.1067/mod.2000.109839. [DOI] [PubMed] [Google Scholar]
- 20.Kinzinger G, Kober C, Diedrich P. Topography and Morphology of the Mandibular Condyle during Fixed Functional Orthopedic Treatment -a Magnetic Resonance Imaging Study. J Orofac Orthop. 2007;68:124–47. doi: 10.1007/s00056-007-0650-0. [DOI] [PubMed] [Google Scholar]
- 21.Pancherz H, Fischer S. Amount and Direction of Temporomandibular Joint Growth Changes in Herbst Treatment: A Cephalometric Long-Term Investigation. Angle Orthod. 2003;73:493–501. doi: 10.1043/0003-3219(2003)073<0493:AADOTJ>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Pancherz H, Michailidou C. Temporomandibular joint growth changes in hyperdivergent and hypodivergent Herbst subjects. A long-term roentgenographic cephalometric study. Am J Orthod Dentofacial Orthop. 2004;126:153–61. doi: 10.1016/j.ajodo.2003.07.015. [DOI] [PubMed] [Google Scholar]
- 23.Yildirim E, Karacay S, Erkan M. Condylar response to functional therapy with Twin-Block as shown by cone-beam computed tomography. Angle Orthod. 2014;84:1018–25. doi: 10.2319/112713-869.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arici S, Akan H, Yakubov K, Arici N. Effects of fixed functional appliance treatment on the temporomandibular joint. Am J Orthod Dentofacial Orthop. 2008;133:809–14. doi: 10.1016/j.ajodo.2006.07.035. [DOI] [PubMed] [Google Scholar]
- 25.Arat Z, Gökalp H, Erdem D, Erden I. Changes in the TMJ disc–condyle–fossa relationship following functional treatment of skeletal Class II Division 1 malocclusion: A magnetic resonance imaging study. Am J Orthod Dentofacial Orthop. 2001;119:316–9. doi: 10.1067/mod.2001.110245. [DOI] [PubMed] [Google Scholar]
- 26.Ruf S, Bendeus M, Pancherz H, Hägg U. Dentoskeletal Effects and ''Effective'' Temporomandibular Joint, Maxilla and Chin Changes in Good and Bad Responders to van Beek Activator Treatment. Angle Orthod. 2007;77:64–72. doi: 10.2319/120605-425R.1. [DOI] [PubMed] [Google Scholar]
- 27.Watted N, Witt E, Kenn W. The temporomandibular joint and the disc-condyle relationship after functional orthopaedic treatment: a magnetic resonance imaging study. Eur J Orthod. 2001;23:683–93. doi: 10.1093/ejo/23.6.683. [DOI] [PubMed] [Google Scholar]
- 28.Kinzinger G, Gülden N, Roth A, Diedrich P. Disc-condyle Relationships during Class II Treatment with the Functional Mandibular Advancer (FMA) J Orofac Orthop. 2006;67:356–75. doi: 10.1007/s00056-006-0626-5. [DOI] [PubMed] [Google Scholar]