Abstract
Purpose
Dehydration is a very common condition among elderly people. Till date there is not yet a fast and easy method to determine a state of dehydration in the emergency department. In the literature there are some exploratory studies that have tried to establish the relationship between some widely used laboratory values and ultrasound for the purpose of diagnosing dehydration. The primary aim of this study is to verify the correlation between two measures derived by ultrasound (caval index and expiratory diameter of inferior vena cava) and blood urea nitrogen (BUN)/creatinine ratio. The relationship between vital signs and BUN/creatinine ratio has also been explored.
Methods
An observational cohort study of patients aged 70 years or more, all examined in our ED. The population was divided on the basis of the BUN/creatinine ratio greater or lower than 20.
Results
A total of 270 patients have been considered. No vital sign correlated with an increased BUN/creatinine ratio. Both the diameter of the inferior vena cava in expiratory and the percentage of its collapsibility in inspiratory (caval index) have revealed a correlation with a BUN/creatinine ratio greater than 20. Areas under the curve are, respectively, 76 % (95 % CI 70–82) and 80 % (95 % CI 75–86). Sensitivity, specificity, positive predictive value and negative predictive value are, respectively, 85.5 % (95 % CI 79.4–90.4); 100 % (95 % CI 97–100); 100 % (95 % CI 97.5–100); 82.9 % (95 % CI 75.9–88.7) and 99.3 % (95 % CI 96.3–99.9); 100 % (95 % CI 97–100); 100 % (95 % CI 97.5–100); 99.2 % (95 % CI 95.6–99.9).
Conclusions
Ultrasound has proved to be useful to diagnose dehydration in elderly people while in the emergency department. Vice versa the vital signs have shown to be unrelated to the hydration state of elderly patients.
Keywords: Dehydration, Ultrasound, Elderly, Emergency, Vena cava
Sommario
Scopo
la disidratazione è una condizione molto comune tra gli anziani. Al giorno d'oggi non esiste ancora un metodo diagnostico rapido e facile che consenta di rilevare uno stato di disidratazione di questi pazienti, specialmente in Pronto Soccorso. In letteratura esistono alcuni studi esplorativi che hanno cercato di stabilire la relazione tra alcuni valori di laboratorio, ampiamente utilizzati, e alcune misure ecografiche. Lo scopo primario di questo studio è di verificare la correlazione tra due misure derivate da metodiche ecografiche (il diametro espiratorio della Vena Cava inferiore e la percentuale di collassabilità in inspirio o Caval Index, di quest'ultima) e il rapporto tra l'azoto ureico ematico (BUN) e la creatinina (BUN/creatinina). Abbiamo anche indagato il rapporto tra i parametri vitali e BUN/creatinina.
Metodo
Studio osservazionale di coorte su pazienti con più di 70 anni, visitati presso il nostro Pronto Soccorso. La popolazione è stata suddivisa in base ad un rapporto BUN/creatinina maggiore o inferiore a 20. Sono stati considerati 270 pazienti. Nessun parametro vitale ha dimostrato di correlare con un rapporto BUN/creatinina >20. Invece, sia il diametro della Vena Cava inferiore in espirio, sia il Caval Index hanno mostrato una correlazione significativa con BUN/creatinina >20. Le AUC (area sotto la curva ROC) sono rispettivamente del 76% (95% CI 70-82) e dell'80% (95% CI 75-86). Sensibilità, specificità, valore predittivo positivo e valore predittivo negativo sono, rispettivamente, 85,5% (95% CI 79,4-90,4); 100% (95% CI 97-100); 100% (95% CI 97,5-100); 82,9% (95% CI 75,9-88,7) e 99,3% (95% CI 96,3-99,9); 100% (95% CI 97-100); 100% (95% CI 97,5-100); 99,2% (95% CI 95,6-99,9).
Conclusioni
L'ecografia ha dimostrato di essere utile nella diagnosi di disidratazione presso una popolazione anziana, in Pronto Soccorso. Viceversa i parametri vitali non hanno mostrato alcun rapporto con lo stato di idratazione.
Introduction
Dehydration is the loss of total water content of the body. It mainly affects the elderly people and for several reasons, such as loss of physiological functions, reduction of thirst and intake of certain types of drugs [1, 2].
Currently, the most used tests for the determination of dehydration are laboratory values. In particular, blood urea nitrogen/creatinine (BUN/creatinine) ratio has proved to be a valuable aid in the diagnosis of dehydration and it is one of the most widely used tests in literature for this purpose. The rationale seems to be based on the wider reabsorption of BUN compared with the larger molecule creatinine, in particular during a condition of renal hypoperfusion [3].
In emergency medicine the ultra-sonographic measure of inferior vena cava (IVC) diameter and its collapsibility have been used to estimate blood volume. Even if it has some limitations, bedside ultrasound seems to be a rapid, easily reproducible and fairly accurate method in determining the volume status of patient [4–9].
Nevertheless, nowadays, the role of ultrasound in the diagnosis of dehydration has not yet been widely studied. In fact, laboratory values take time which potentially delays the management of patient care.
To our knowledge, only one study in literature has taken into account the bedside ultrasound for the diagnosis of dehydration. Riccardi and his colleagues have achieved a good degree of correlation between laboratory and ultrasound [10].
Our aim was to verify the correlation between caval index and the expiratory diameter of IVC and BUN/creatinine ratio.
We have also tried to determine the correlation between vital signs and BUN/creatinine ratio.
Materials and methods
Study design
Observational cohort study.
Population
We collected data of consecutive patients who visited in our ED from March to August 2013 and between March and April 2014. The inclusion criteria were the age greater than 70 years and the need (in the view of the physician on duty) to perform a blood test. We considered only the elderly because dehydration is much more common in this range of patients.
The exclusion criteria were based on the presence of acute bleeding (especially gastrointestinal bleeding which is a well-known cause of increase in BUN even in the absence of dehydration), the inability to display the IVC by the long-axis/subxiphoid view (see “Measurements“ section) and the presence of an obvious right ventricular dysfunction (established on the basis of an enlargement of the right chambers of the heart or irregular motion of the cardiac wall of the right ventricle by inspection with ultrasound), such as to suspect an increase in pulmonary artery pressure.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. We asked routinely consent to manage personal data from every patient coming in our emergency department.
Due to the observational nature of the study, our institute did not require a formal authorization from the Ethics Committee who was informed anyway.
Measurements
For each patient we recorded:
Age, gender;
Blood pressure (systolic and diastolic arterial pressure), mean arterial pressure (MAP) heart rate, and shock index (heart rate/systolic blood pressure).
Blood urea nitrogen, creatinine and BUN/creatinine ratio.
Expiratory IVC diameter and inspiratory collapsibility of IVC as caval index [(maximum diameter − minimum diameter)/maximum diameter]. The measurements by ultrasound were made viewing the inferior vena cava with a “convex-array” probe, according to the long-axis view in the subxiphoid window. The measurements were taken using the M-mode, 2 cm from the junction between the right atrium and the inferior vena cava. The evaluation of cardiac function was instead performed with a “sector” probe, according to a four-chamber view through the apical window.
Due to the delay in getting the blood tests, the physician performing the ultrasound examination was not aware of the BUN/creatinine ratio during the evaluation of IVC and right ventricle. In any case, the physician was not aware of the purpose of this study. The measurements carried out were part of a routine evaluation of patients in our ED.
We considered the cut-off of 20 for the BUN/creatinine ratio, in accordance with Riccardi et al. because in the literature a higher value indicates an advanced dehydration. The value of 20 allows to determine a condition of impending but still reversible dehydration.
Statistical
We analyzed the clinical and instrumental data collected at enrollment. Data were expressed as mean ± standard deviation for continuous variables and as percentages for discrete variables. The comparison between continuous variables was performed with Mann–Whitney U test, while the ratio of discrete variables was performed with the Chi-square test. The results were considered significant for values of p ≤ 0.05. ROC (receiver operating characteristics) analysis and AUC (area under curve) were used to examine the performance of the used tests. A linear regression model was used to verify the distribution of continuous variables with respect to the reference variable. We calculated sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) based on the values with the best sensitivity and specificity identified by ROC curve. All analyses were performed with IBM SPSS Statistics (version 21.0. Armonk, NY: IBM Corp).
Results
We evaluated 294 patients older than 70, who met the inclusion criteria. Two patients were excluded for the presence of gastric bleeding, six were excluded for a right ventricular dysfunction according to the exclusion criteria previously described, three were excluded for the impossibility to visualize the IVC by ultrasound, 13 cases were excluded for the lack of data.
So we finally considered 270 cases. 55 % of the population had a BUN/creatinine ratio greater than 20. Dividing the population for BUN/creatinine ratio greater than 20, we found there is no difference in the average age of the two groups. We noticed an imbalance in gender distribution in the two groups (see “Limits” section).
We found no difference between the two groups regarding the systolic blood pressure, diastolic blood pressure, mean arterial pressure, heart rate or for the shock index.
We found the average expiratory diameter of IVC was significantly lower in the group of patients with dehydration (1.3 ± 0.5 cm) than the group of not dehydrated patients (1.7 ± 0.4 cm) (p value <0.001).
We also found the caval index (in percent) to be greater in the group of patients with dehydration than non-dehydrated (75 vs. 40 %) (p value = 0.01). Results are summarized in Table 1.
Table 1.
Characteristics of the two groups (Group 1: BUN/creatinine ratio ≥20; Group 2: BUN/creatinine <20) divided for dehydration
| Group 1 | Group 2 | p value (between the two groups) | |
|---|---|---|---|
| N = 148 (55 %) | N = 122 (45 %) | ||
| Age (mean ± SD) | 82 ± 7 | 81 ± 6 | 0.684 |
| Gender (male), n (%) | 56 (38) | 68 (56) | 0.050* |
| SAP (mmHg) | 145 ± 31 | 145 ± 33 | 0.669 |
| DAP (mmHg) | 76 ± 16 | 78 ± 18 | 0.166 |
| MAP (mmHg) | 97 ± 21 | 101 ± 21 | 0.251 |
| HR (bpm) | 85 ± 21 | 87 ± 26 | 0.466 |
| Shock index | 0.61 ± 0.22 | 0.62 ± 0.24 | 0.558 |
| IVC exp. diameter (cm) | 1.3 ± 0.5 | 1.7 ± 0.4 | 0.000* |
| Caval index (%) | 75 ± 28 | 40 ± 27 | 0.010* |
| BUN/creatinine ratio | 28 ± 8 | 16 ± 3 | 0.000* |
SAP systolic arterial pressure, DAP diastolic arterial pressure, MAP mean arterial pressure, HR heart rate
* p value ≤0.05
Figure 1 shows the ROC curve for the caval index. AUC was 80 % (95 % CI 75–86). The best cut-off value for caval index was 48 %.
Fig. 1.
ROC curve for caval index. AUC = 0.80 (St Er 0.03; 95 % CI 0.75–0.86); p value <0.001
Figure 2 shows the ROC curve with respect to the expiratory diameter of the IVC. AUC was 76 % (95 % CI 70–82). The best cut-off value for diameter of IVC was 1.55 cm.
Fig. 2.
ROC curve for expiratory diameter of IVC. AUC = 0.76 (St Er 0.03; 95 % CI 0.70–0.82); p value <0.001
Based on these cut-off values, we calculated the sensitivity, specificity and positive/negative predictive values for both tests. The results are summarized in Table 2.
Table 2.
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) for expiratory diameter of IVC and caval index
| Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|
| IVC diameter | 85.5 (79.4–90.4) | 100 (97–100) | 100 (97.5–100) | 82.9 (75.9–88.7) |
| Caval index | 99.3 (96.3–99.9) | 100 (97–100) | 100 (97.5–100) | 99.2 (95.6–99.9) |
Considered cut-offs, on the basis of the coordinates in the ROC curve were, respectively, 1.55 cm and 48 %
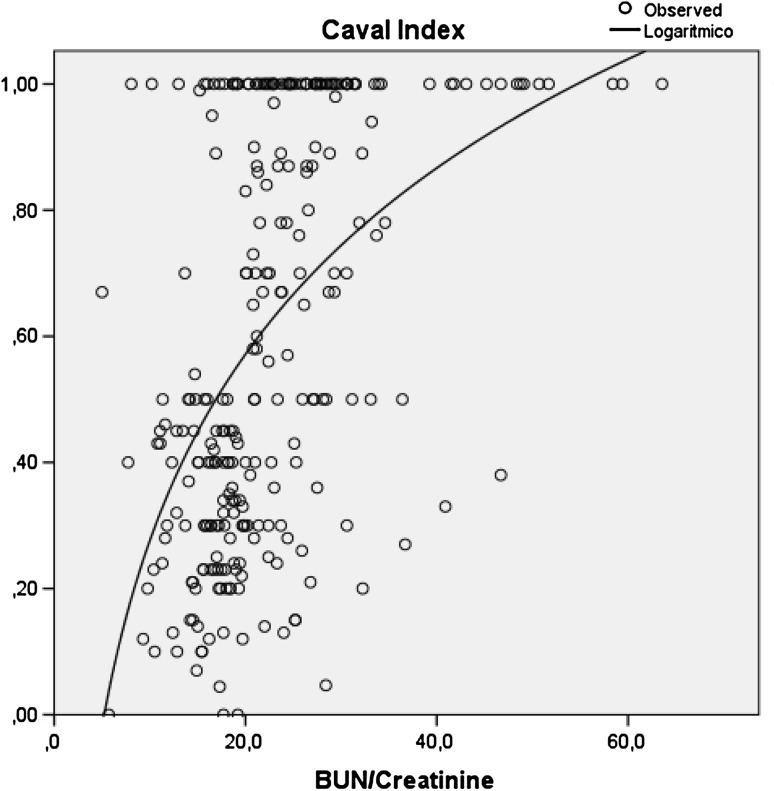
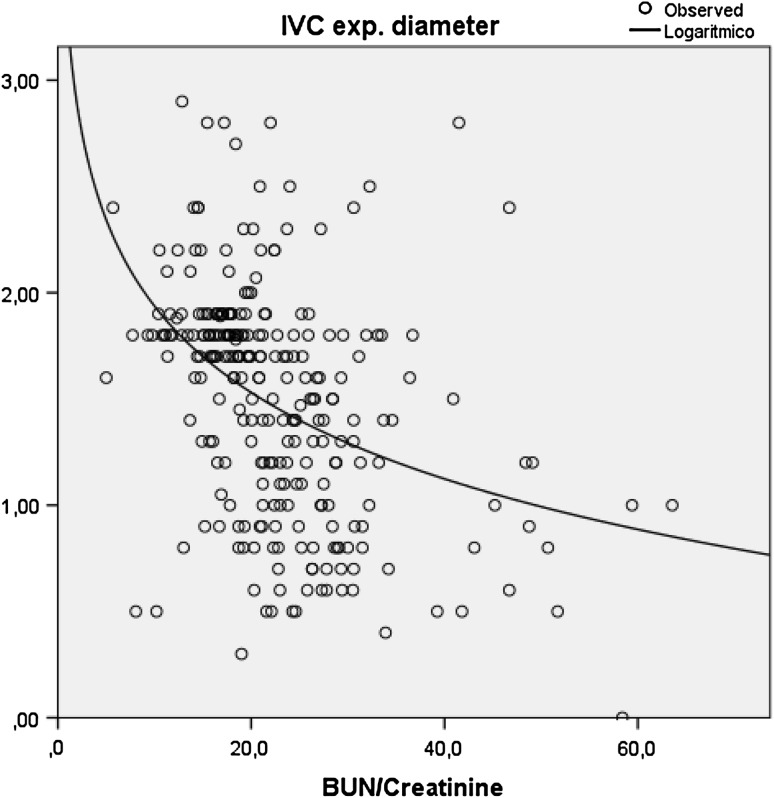
The best fitted function describing the relationship between BUN/creatinine ratio, expiratory diameter of IVC and caval index is a logarithmic type, as shown in Figs. 3 and 4.
Fig. 3.
Logarithmic regression for caval index in respect of BUN/creatinine ratio (R 2 = 0.24; ANOVA F = 84.59; p value <0.001)
Fig. 4.
Logarithmic regression for expiratory diameter of IVC in respect of BUN/creatinine ratio (R 2 = 0.16; ANOVA F = 52.67; p value <0.001)
Discussion
Dehydration should be distinguished from hypovolemia. While dehydration is a loss of total content of body water, hypovolemia is just the loss of the intravascular compartment. This constitutes no more than 10 % of the total content of body water [11]. Experimental studies have shown that a loss of intracellular water entails a modification of the extracellular component too, in particular of intravascular compartment. This means an increase in plasma osmolarity that determines a consequent reduction of the central venous pressure (CVP) [12]. According to this correlation, Riccardi and colleagues examined the relationship between ultrasound, which is based on the determination of the CVP, and dehydration [10].
Despite the numerous limitations in using the ultrasound methods, on which Marik et al. [13] expressed their view, the literature indicates that in patients with spontaneous ventilation, the expiratory diameter of the IVC and its collapsibility determined by bedside ultrasound is correlated with hypovolemia [5–9].
Although dehydration is a very common condition among the elderly, there is no exam to this date that can be considered as the diagnostic gold standard [14]. The evaluation of BUN/creatinine ratio is often used for determining a dehydration condition [4]. Such examination is certainly not optimal and it suffers from a range of confounding factors such as gastric bleeding, but nowadays it seems to be one of the most useful tests in the determination of dehydration [15].
On the other hand, in the ED there is the need for a non-invasive, easily reproducible test which can immediately give directions regarding the therapy to undertake.
Our study confirms the results obtained by previous studies [10]: inspiratory collapsibility of the IVC shows a good correlation with a BUN/creatinine ratio greater than 20. In particular, the PPV and NPV are almost optimal in ensuring that the determination of caval index is particularly accurate in the diagnosis of dehydration.
Compared to Riccardi et al. [10], our study shows that even the expiratory diameter of IVC is useful in the diagnosis of dehydration. Even though the accuracy is very good in this case study, it seems that this test performs less well than caval index. This finding is probably related to conditions of increased CVP not properly excluded by ultrasound “eyeball” evaluation, such as an increase in pulmonary arterial pressure in a grade not so obvious to be determined without any measurement with Doppler. In any case, in our study we are not able to verify this hypothesis.
Compared to the literature, we observed a higher sensitivity of the caval index in identifying a dehydration state. This difference could be due to the fact that we excluded patients with gastrointestinal bleeding as it is a well-known cause of increased BUN even without dehydration. It seems though that Riccardi and colleagues, did not exclude causes that could potentially increase the BUN even without dehydration [10].
Furthermore, our population was significantly older than the one considered by Riccardi et al., in accordance with the inclusion criteria of each study.
As shown in several studies in the literature, vital signs are totally unreliable in determining volume depletion [16]. This is probably linked to different factors such as drug therapy. It is not excluded that this result is also linked to physiological adaptation systems.
A recent review done by the Cochrane Database Group took into consideration all the tests routinely used to diagnose dehydration [17]. None of these tests appeared to have a sufficient accuracy to be used alone. However, this review did not take into account ultrasound. We believe the bedside ultrasound could be a non-invasive, reproducible and an accurate enough test to identify a state of dehydration in a population of elderly patients.
We found that the bedside ultrasound quickly allows to establish the state of hydration of elderly patients in the ED.
Limits
We are aware the system of blinding is not optimal. Nevertheless, the physician performing the measurements was not informed about the purpose of the study. The use of ultrasound was part of a routine procedure that would still be carried out even outside of this study.
We considered a convenience sample, because of scarcity of additional data in the literature. This was probably the cause of the incorrect balance between the two considered groups regarding gender. Despite this, the sample was large enough to reveal a significant difference between the ultrasound measures and the laboratory values. A very recent study in older people regarding dehydration has taken in account a comparable sample size [18]. A further yet unpublished study has calculated the sample size needed to a standard error no more than 0.05 (considering a dehydration prevalence of 40 %) for a Kappa value in excess of 0.75, in the order of 180 patients. So our study had more patients than required for having a good estimated diagnostic accuracy with an adequate statistic power [19].
We are also aware that BUN/creatinine ratio is not the gold standard for the diagnosis of dehydration. It is probably an index of renal hypoperfusion rather than an index of hydration status altogether. Nonetheless, it is one of the most frequently used parameters both in clinical practice and in the literature. We believe it is a good reference when comparing ultrasound methods as it is very widely used in clinical practice and also because we are still experiencing the absence of any gold standard.
The ultrasound measurements were carried out by experts using ultrasound with at least 5 years of experience in using it on a daily basis. We do not know if our result can be generalized to other groups. Nevertheless, previous studies have shown that the inter-individual reproducibility is very good for at least the items taken as reference (viewing IVC).
The identification of patients with a high pulmonary arterial pressure carried out with the only use of the ultrasound inspection evaluation is not optimal. In any case, on the basis of the obtained results, we believe there have been few cases of pulmonary hypertension unidentified through this method.
Conclusion
Caval index and expiratory diameter of IVC determined by bedside ultrasound are useful as a rule in dehydration of elderly patients in ED. Vital signs instead have not proven useful in this particular population, with regard to this purpose.
Authors’ contributions
All authors contributed equally to the realization of this study. All authors read and approved the final draft of this study.
Compliance with ethical standards
Conflict of interests
All authors declare that they have no conflict of interest. No financing has been released for the conduct of this study.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). All patients provided written informed consent to enrolment in the study and to the inclusion in this article of information that could potentially lead to their identification.
Human and animal studies
The study was conducted in accordance with all institutional and national guidelines for the care and use of laboratory animals.
References
- 1.Thomas DR, Cote TR, Lawhorne L, Levenson SA, Rubenstein LZ, Smith DA, Stefanacci RG, Tangalos EG, Morley JE, The Dehydration Council Understanding clinical dehydration and its treatment. J Am Med Dir Assoc. 2008;9:292–301. doi: 10.1016/j.jamda.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Hooper L, Bunn D, Jimoh FO, Fairweather-Tait SJ. Water-loss dehydration and aging. Mech Ageing Dev. 2014;136–137:50–58. doi: 10.1016/j.mad.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Thomas DR, Tariq SH, Makhdomm S, Haddad R, Moinuddin A. Physician misdiagnosis of dehydration in older adults. J Am Dir Assoc. 2003;4:251–254. doi: 10.1016/S1525-8610(04)70368-0. [DOI] [PubMed] [Google Scholar]
- 4.Copetti R, Copetti P, Reissig A. Clinical integrated ultrasound of the thorax including causes of shock in nontraumatic critically ill patients. A practical approach. Ultrasound Med Biol. 2012;38(3):349–359. doi: 10.1016/j.ultrasmedbio.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 5.Dipti A, Soucy Z, Surana A, Chandra S. Role of inferior vena cava diameter in assessment of volume status: a meta-analysis. Am J Emerg Med. 2012;30:1414–1419. doi: 10.1016/j.ajem.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Z, Xu X, Ye S, Xu L. Ultrasonographic measurement of the respiratory variation in the inferior vena cava diameter is predictive of fluid responsiveness in critically ill patients: systematic review and meta-analysis. Ultrasound Med Biol. 2014;40:845–853. doi: 10.1016/j.ultrasmedbio.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 7.Nagdev AD, Merchant RC, Tirado-Gonzalez A, Sisson CA, Murphy MC. Emergency Department bedside ultrasonographic measurement of the Caval Index for noninvasive determination of low central venous pressure. Ann Emerg Med. 2010;55:290–295. doi: 10.1016/j.annemergmed.2009.04.021. [DOI] [PubMed] [Google Scholar]
- 8.Stawicki SP, Braslow BM, Panebianco NL, Kirkpatrick JN, Gracias VH, Hyaden GE, Dean AJ. Intensivist use of hand-carried ultrasonography to measure IVC collapsibility in estimating intravascular volume status: correlations with CVP. J Am Coll Surg. 2009;209:55–61. doi: 10.1016/j.jamcollsurg.2009.02.062. [DOI] [PubMed] [Google Scholar]
- 9.Muller L, Bobbia X, Toumi M, Louart G, Molinari N, Ragonnet B, Quintard H, Leone M, Zoric L, Lefrant JY, The AzuRea group Respiratory variations of inferior vena cava diameter to predict fluid responsiveness in spontaneously breathing patients with acute circulatory failure: need for a cautious use. Crit Care. 2012;16:R188. doi: 10.1186/cc11672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riccardi A, Chiarbonello B, Minuto P, Guiddo G, Corti L, Lerza R. Identification of the hydration state in emergency patients: correlation between Caval Index and BUN/creatinine ratio. Eur Rev Med Pharmacol Sci. 2013;17:1800–1803. [PubMed] [Google Scholar]
- 11.Bhave G, Neilson EG. Volume depletion versus dehydration: how understanding the difference can guide therapy. Am J Kidney Dis. 2011;58:302–309. doi: 10.1053/j.ajkd.2011.02.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Charkoudian N, Eisenach JH, Joyner MJ, Roberts SK, Wick DE. Interactions of plasma osmolality with arterial and central venous pressures in control of sympathetic activity and heart rate in humans. Am J Physiol Heart Circ Physiol. 2005;289:2456–2460. doi: 10.1152/ajpheart.00601.2005. [DOI] [PubMed] [Google Scholar]
- 13.Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? a systemic review of the literature and the tale of seven mares. Chest. 2008;134:172–178. doi: 10.1378/chest.07-2331. [DOI] [PubMed] [Google Scholar]
- 14.Armstrong LE. Assessing hydration status: the elusive gold standard. J Am Coll Nutr. 2007;26(S5):575–584. doi: 10.1080/07315724.2007.10719661. [DOI] [PubMed] [Google Scholar]
- 15.Robinson BE, Weber H. Dehydration despite drinking: beyond the BUN/creatinine ratio. J Am Med Dir Assoc. 2004;5(S2):S67–S71. doi: 10.1016/S1525-8610(04)70099-7. [DOI] [PubMed] [Google Scholar]
- 16.Wo CC, Shoemaker WC, Appel PL, Bishop MH, Kram HB, Hardin E. Unreliability of blood pressure and heart rate to evaluate cardiac output in emergency resuscitation and critical illness. Crit Care Med. 1993;21:218–223. doi: 10.1097/00003246-199302000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Hooper L, Abdelhamid A, Attreed NJ, et al. Clinical symptoms, signs and tests for identification of impending and current water-loss dehydration in older people. Cochrane Database Syst Rev. 2015;4:CD009647. doi: 10.1002/14651858.CD009647.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hooper L, Bunn DK, Downing A et al. Which frail older people are dehydrated? The UK DRIE Study. J Gerontol A Biol Sci Med Sci. 2015; pii: glv205. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 19.Hooper L. DRIE 2 (Dehydration recognition in our elders re-test) Trial; ISRCTN58315094; doi:10.1186/ISRCTN58315094. http://www.isrctn.com/ISRCTN58315094. Accessed 23 Dec 2015