Abstract
Objective
Self-reports of “hearing handicap” are available, but a comprehensive measure of health-related quality of life (HRQOL) for individuals with adult-onset hearing loss (AOHL) does not exist. Our objective was to develop and evaluate a multidimensional HRQOL instrument for individuals with AOHL.
Design
The Impact of Hearing Loss Inventory Tool (IHEAR-IT) was developed using results of focus groups, a literature review, Advisory Expert Panel input, and cognitive interviews.
Study Sample
The 73-item field-test instrument was completed by 409 adults (22-91 years old) with varying degrees of AOHL and from different areas of the US.
Results
Multitrait scaling analysis supported four multi-item scales and five individual items. Internal consistency reliabilities ranged from 0.93 to 0.96 for the scales. Construct validity was supported by correlations between the IHEAR-IT scales and scores on the 36-Item Short Form Health Survey, Version 2.0 (SF-36v2) Mental Composite Summary (r’s = 0.32 – 0.64) and the Hearing Handicap Inventory for the Elderly/Adults (HHIE/HHIA) (r’s > −0.70).
Conclusions
The field test provide initial support for the reliability and construct validity of the IHEAR-IT for evaluating HRQOL of individuals with AOHL. Further research is needed to evaluate the responsiveness to change of the IHEAR-IT scales and identify items for a short-form.
Keywords: hearing loss, health-related quality of life, functioning, well-being
Hearing loss has been identified as a primary contributor to the global burden of chronic disability in the United States (US Burden of Disease Collaboration, 2013). Adverse effects on physical, emotional, cognitive, behavioral, occupational, and social function have been reported (e.g., Chia et al., 2007; Dalton et al., 2003; Genther et al., 2013; Helvik et al., 2013; Mulrow et al., 1990). Even when the actual hearing loss according to audiometric measures is categorized as “mild,” some individuals report significant associated disabling effects (Monzani et al., 2008; Mulrow et al., 1990; Newman et al., 1997). Hence, audiometric measures alone yield insufficient information about an individual’s disability (Hallberg et al., 2008). Psychosocial and environmental factors, functional impairments, and perceived consequences of the disability must also be considered (Ferrans et al., 2005).
The World Health Organization (WHO) emphasized that health is “a state of complete physical, mental, and social well-being and not merely an absence of disease and infirmity” (WHO, 1948). More recently, Healthy People 2020 (U.S. Department of Health and Human Services, 2010), a 10-year national objective for improving the health of Americans, identified improvement in health-related quality of life (HRQOL) as one of the initiative’s four primary goals.
HRQOL is a multidimensional construct that encompasses the effects of disease or disability on an individual’s physical, psychological, and social functioning and well-being (Spilker, 1996). Although a number of self-report questionnaires have been developed to assist clinicians and researchers assess the impact of hearing loss on an individual’s communication functioning and hearing disability, the most commonly used measure is the Hearing Handicap Inventory for the Elderly (HHIE; Ventry & Weinstein, 1982). The HHIE was originally developed to quantify the psychosocial effects of hearing loss in older adults, but researchers have used it and its shorter screening version, the HHIE-S, as a hearing-targeted measure of HRQOL.
The HHIE is easily administered and provides information on a broad range of social and emotional factors impacted by hearing loss but it does not capture all important aspects of HRQOL. In addition, the HHIE was designed for use with older individuals experiencing hearing loss. An alternative version, the HHIA, targets younger individuals by replacing three items from the HHIE with questions that the authors deemed to be relevant to persons younger than 65 years of age (Newman et al., 1990).
The aim of the present study was to develop a comprehensive measure of HRQOL targeted at individuals with AOHL and provide initial evaluation of its psychometric properties. This paper describes the development of the instrument, including its conceptual framework, item generation and item reduction, scale formation, and reliability and validity.
Methods
Field Test Instrument Development
The hearing-targeted HRQOL field test instrument was designed as a self-report measure for individuals 21 years and older with AOHL. The development of this instrument was consistent with recommended guidelines on patient-reported outcomes measure development issued by the U.S. Food and Drug Administration (FDA; 2009) and procedures endorsed by the International Society for Quality of Life Research (Reeve et al., 2012). Ethics approval for the study was obtained from the San Diego State University, Institutional Review Board (IRB) prior to any subject’s participation in any phase of this research (IRB Project Number: 01642).
Conceptual Framework
The initial seeds for the conceptual framework came from a study investigating the impact of hearing loss on a variety of aspects of daily life, including family relationships, social interactions and activities, employment, use of assistive technology, and general psychosocial well-being (Stika, 1997a; 1997b; Trybus et al., 2004). Thirteen 2-hour focus groups were held in six different locations (Washington, DC; Allentown, PA; San Diego, CA; Thousand Oaks, CA; Long Beach, CA; Whittier, CA.), with a total of 107 individuals with hearing loss participating. To explore the impact of hearing loss on daily life from the perspective of the family member, five focus groups involving 37 hearing family members were also conducted.
A second component of the instrument development was a comprehensive literature search using the following keywords: “hearing disability,” “quality of life,” “health-related quality of life,” “adult hearing loss,” and “well-being.” The aim of the literature search was to identify existing HRQOL instruments used with individuals with hearing loss, and to examine information obtained by these measures. Instruments designed for use with other disabilities and health conditions were also reviewed to determine whether they might contain relevant content areas and items that could be adapted and included in the field test of individuals with AOHL.
Item Generation
An initial item pool was drafted based on themes identified from content analysis of the focus group transcripts, literature review, and discussions with the Expert Advisory Panel. The seven-member Expert Advisory Panel was comprised of researchers in the fields of psychology, audiology, otolaryngology, aural rehabilitation, survey instrument development and psychometrics, vocational rehabilitation, and hearing loss advocacy. In addition to being national renowned leaders in their respective fields, the majority of these individuals had AOHL themselves. Questionnaire items were written following guidelines suggested in the literature for wording and designing HRQOL instruments (Mullin et al., 2000). Each item was formulated following a question stem with a 5-point response scale (e.g., never, rarely, sometimes, often, always). Some items, such as those pertaining to work or intimate/sexual relationships, included a “not applicable” response option. A timeframe of “during the past four weeks” was included to anchor the respondent’s evaluation of his or her experiences (e.g., “During the past four weeks, did you hold back from participating in conversations and discussions because you were unsure whether you heard what people had said?”). If the respondent used hearing aids or had a cochlear implant, they were instructed to answer items based on their daily experiences with the hearing device on.
Item reduction
The drafted items were organized and listed under headings that noted the content of the intended target domain and associated subdomain. Using a method described by Cunningham et al. (1999) for rating relevancy of HRQOL items to a specific population, members of the Expert Advisory Panel were asked to review the list and (a) judge each item in terms of its relevance to the HRQOL of an individual with AOHL, and (b) note items that seemed redundant, ambiguous, or lengthy, or contained jargon terms. Feedback from the Expert Advisory Panel resulted in the elimination of several items, a consolidation of others, and a rewording of a few. This process yielded an initial item pool of 87 items.
Next, face-to-face cognitive interviews and respondent debriefings were conducted with five adults with AOHL. For the interviews, respondents were asked to read each item silently and then “think aloud” as they determined their responses. Follow-up debriefing allowed for probing of respondents’ opinions regarding the questionnaire, including its visual format, clarity, comprehensiveness, and ease in completing. As a result of these pretesting techniques, 14 items were omitted and several items were reworded to enhance their clarity. A final set of 73 items were selected for inclusion in the field test. Also included were two global questions that asked: “How would you rate your overall quality of life?” and “To what extent does your hearing loss impact your quality of life?”
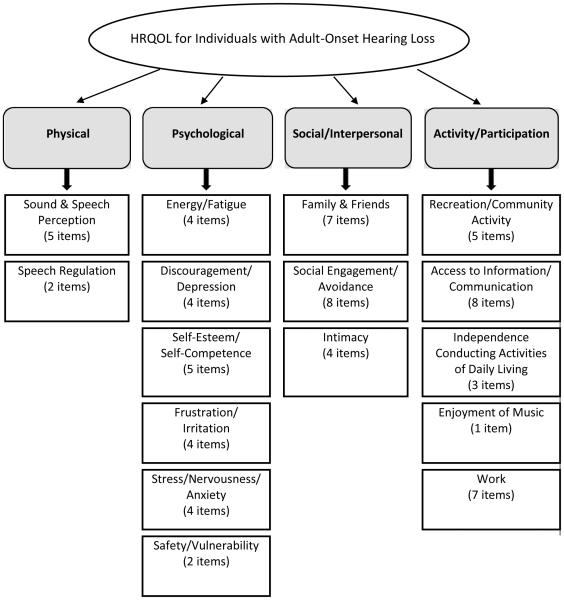
The final field test instrument, the Impact of Hearing Loss Inventory Tool (IHEAR-IT), consisted of four hypothesized global domains (Physical, Psychological, Social/Interpersonal, and Activity/Participation) and 16 associated subdomains. (See Figure 1)
Figure 1.
Diagram of the hypothesized domains and subdomains of the field testing instrument.
Existing measures and other variables
Existing (“legacy”) measures were included to evaluate the construct validity of the new measure, including the 36-Item Short Form Health Survey, Version 2.0 (SF-36v2; Ware et al., 2000) and either the HHIE or the HHIA, depending on the participant’s age. The SF-36v2 is a generic measure of HRQOL consisting of 36 questions and 8 derived scales that assess physical functioning, role limitations due to physical health problems, role limitations due to emotional problems, social functioning, emotional well-being, pain, energy/fatigue, and general health perceptions. Two summary scores normed on the U.S. general population (mean = 50, SD = 10) are calculated: a physical component summary (PCS) score and a mental component summary (MCS) score. The SF-36v2 was selected because of its widespread use in medical and healthcare research, including research involving individuals with disabilities.
The HHIE is a 25-item self-assessment measuring perceived psychosocial consequences of hearing loss for adults age 65 years and older. The respondent is asked to answer “yes,” “sometimes,” or “no” to each question, with answers scored as 4, 2, or 0, respectively. Two scale scores are calculated: 1) emotional (13 items, 0-52 possible range), and 2) social/situational (12 items, 0-48 possible range). A 25-item overall HHIE score (0-100 possible range) is also calculated and classified into three categories of self-perceived hearing handicap: a total score of ≤16 indicates no handicap; 17-42 suggests mild to moderate handicap, and > 42 is considered a significant handicap. The HHIA was designed for use with adults younger than 65 years of age and is identical to the original HHIE except that it includes the substitution of three questions which focus on occupational and social situations more commonly experienced by younger adults (i.e., “Does a hearing problem cause you difficulty in the movies or theater?”; “Does a hearing problem cause you difficulty hearing/understanding coworkers”?; “Does a hearing problem cause you to feel frustrated when talking to coworkers, clients, or customer?”) (Newman et al., 1990). The HHIA is scored and interpreted in a similar fashion as the HHIE.
Questions were included in the field test to gather information about the respondent’s age, education, income, additional medical conditions, hearing loss, use of hearing aids and/or cochlear implants, and satisfaction with benefits obtained from assistive hearing technologies if used. Also included were items that addressed personal and environmental factors that might influence the functional performance of the individual with hearing loss (e.g., “My family makes special effort to ensure that I am following conversations and discussions.”; “I am uncomfortable asking others to make special effort for me because of my hearing loss.”). In addition, potentially positive outcomes of experiencing hearing loss during adulthood were addressed (e.g., “As a result of my hearing loss, I have a greater appreciation for the challenges faced by people who have disabilities.”). Hence, throughout construction of the field test instrument, careful attention was given to broadening the conceptualization of “hearing disability” beyond a traditional deficit model and incorporating elements consistent with the WHO International Classification of Functioning, Disability and Health (ICF) theoretical framework (2001), whereby environmental and personal factors that influence the disabling process are also considered (Hays et al., 2002; Tate & Pledger, 2003).
Sample
Individuals invited to participate were 21 years or older, with an onset of diagnosed hearing loss at 18 years of age or older. Excluded were individuals whose hearing loss was diagnosed prior to the age of 18, persons with serious health conditions or other sensory impairments that could potentially affect their daily functioning, and individuals unable to read and understand English. The reason for excluding individuals with a known hearing loss onset prior to adulthood is that hearing loss diagnosed later in life typically results in a very different set of issues and adjustment demands than when it occurs during childhood (Thomas, 1984). Individuals who are diagnosed with hearing loss during adulthood have already established a solid foundation in communication skills, a sense of self and social identity, vocational placement, and financial responsibilities. Moreover, they have come to rely on their ability to hear in order to function optimally in their personal lives and social relationships, and at work.
Subjects were recruited both locally and nationally using a variety of procedures, including flyers distributed through private and hospital audiology clinics, and notices placed on Internet bulletin boards, listservs, and consumer organizations' websites (e.g., Hearing Loss Association of America).
Data Collection
Questionnaire packets were mailed to individuals who indicated a desire to participate in the study, met the inclusion criterion, and had signed and returned an informed consent document. Participants were asked to provide a copy of their most recent audiogram conducted within the last three years to examine associations of audiometric test results with self-reported levels of hearing loss. Subjects were mailed a $20 gift card to a store of their choice (Home Depot, Target, or Starbucks) after the research packet was returned and judged complete, regardless of whether a copy of a recent audiogram was included.
Psychometric analyses
Items were grouped according to hypothesized domains and subdomains based upon an a priori theoretical framework and item content. The responses categories were recoded and transformed linearly to a possible range of 0 to 100, with higher scores indicative of a better HRQOL.
Next, multitrait scaling analysis was used to evaluate item discrimination across the hypothesized scales (Hays & Fayers, 2005). Item discrimination refers to the extent to which an item correlates significantly higher with the scale that it is intended to measure than it does with any of the other scales. Item discrimination was supported when the correlation of an item with its hypothesized scale was at least two standard errors higher than correlations with other scales. If an item showed a higher correlation with a scale other than its hypothesized scale, then the item was moved to another scale and the multitrait scaling analysis was run again. Items that correlated equally with multiple scales and items that failed to have an item-scale correlation with their hypothesized scale greater than 0.35 were considered individual items rather than associated with a particular scale. A series of iterations of multitrait scaling analyses were conducted until a satisfactory “fit” for each item was achieved. Scores on the IHEAR-IT were computed by adding together item scores for each scale, and then dividing the total score by the number of items that comprise the scale. This yielded scales with a possible range of 0 to 100, with higher scores indicating better HRQOL.
The Work scale items were not included in the multitrait scaling analysis due to the relatively small subset of participants indicating that they were currently employed (n = 162; 40%). Similarly, items from the Intimacy/Sexual Relations scale were excluded from this analysis, as about one-third of the sample indicated that they were not in an intimate or sexual relationship. The psychometric properties for these two scales are discussed separately from the multitrait scaling analysis.
Content validity refers to the extent to which an item reflects the breadth and depth of the construct of interest (Hays & Revicki, 2005). Content validity was enhanced by having members of the Expert Advisory Panel rate the extent to which items, scales, and subscales reflected common experiences associated with AOHL and HRQOL. In addition, extensive use of focus groups and cognitive interview methodology during the development of the instrument maximized its content validity.
Construct validity refers to the extent to which an instrument actually measures the target construct in ways that it purports it does. Construct validity was evaluated by examining the strength of the correlations between scores on the IHEAR-IT scales and scores on the HHIE/HHIA, and the SF-36v2 PCS and MCS. We hypothesized that the new scales would show a negative correlation with the HHIE/HHIA Total Score and a positive correlation with the MCS from the SF-36v2, but not correlate with the PCS from the SF-36v2. In addition, based on previous research (Chia et al., 2007; Dalton et al., 2003), we anticipated that severity of hearing loss would be associated with poorer HRQOL. Further, we hypothesized that younger individuals and women would report worse HRQOL. Finally, we hypothesized that the IHEAR-IT scales would explain unique variance beyond the HHIE/HHIE in global ratings of overall quality of life and the impact of hearing loss on quality of life. Following the criteria suggested by Cohen (1992), correlation coefficient values of 0.1 – 0.23 were regarded as a small effect size, 0.24 – 0.36 as a medium effect size, and 0.37 or higher as a large effect size.
Multitrait scaling analyses were performed using SAS® (Hays & Wang, 1992) while all other analyses were conducted using IBM SPSS version 22 (IBM Corp., Released 2013).
Results
Sample Characteristics
A total of 443 individuals expressed interest in participating in the study and signed and returned the informed consent; 412 individuals completed and returned the questionnaire packet (response rate = 93%). Three individuals who returned their completed questionnaires were ineligible for participation because they indicated their hearing loss was diagnosed before 18 years of age. Approximately half of the study group (51%) provided a copy of their audiogram.
The average age of the 409 study participants was 63 years (range: 22—91 years, SD = 14.0), with 66% being women. The male participants tended to be older (M = 68 years, SD = 12.8) than the female participants (M = 61 years, SD = 14.0), t(407) = 5.32, p < .001). The average reported age of clinical diagnosis of hearing loss was 43 years for women and 52 years for men. Duration of hearing loss for the participants, based on age at time of diagnosis, ranged from less than 1 year to 65 years (M = 17.3; SD = 12.7), with 26% of the participants reporting having had a hearing loss for 6 years or less. There was no significant difference between men and women on self-reported duration of hearing loss, t(405) = 1.36, p = .175. However, women reported obtaining a diagnosis sooner after first noticing problems with hearing (M = 3.6 years, SD = 6.1) than did men (M = 5.4 years, SD = 7.5), t(401) = 2.62, p < .01).
The sample included persons in 44 states, with a majority of the participants (31%) from California, followed by 9% living in Florida. Fifty-three percent judged their health to be either “excellent” or “very good.” Additional sociodemographic information for the sample, including race/ethnicity, marital status, educational level, employment status, and income is provided in Table 1.
Table 1.
Demographic characteristics of study participants (N = 409)
| Characteristic | n | % |
|---|---|---|
| Gender | ||
| Male | 141 | 34 |
| Female | 268 | 66 |
| Age, years | ||
| >20 and ≤35 | 6 | 2 |
| >35 and ≤50 | 73 | 18 |
| >50 and ≤65 | 159 | 39 |
| >65 and ≤80 | 122 | 30 |
| >80 and ≤91 | 49 | 11 |
| Race/Ethnicity | ||
| White (not of Hispanic origin) | 381 | 93 |
| White (Hispanic or Latino) | 13 | 3 |
| Black or African American | 6 | 2 |
| Asian/Pacific Islander | 6 | 1 |
| Native American or Alaskan Native | 3 | 1 |
| Marital Status | ||
| Single – never married | 37 | 9 |
| Married or living as married | 238 | 58 |
| Separated | 5 | 1 |
| Divorced | 68 | 17 |
| Widowed | 60 | 15 |
| Education | ||
| < High school | 6 | 2 |
| High school graduate | 32 | 8 |
| Vocational school or some college | 92 | 22 |
| 4-year college degree | 123 | 30 |
| Professional or graduate degree | 156 | 38 |
| Employment Status | ||
| Working full-time | 126 | 31 |
| Working part-time | 36 | 9 |
| Unemployed | 23 | 5 |
| Retired | 199 | 49 |
| Full-time homemaker | 21 | 5 |
| Volunteer worker | 4 | 1 |
| Total household income | ||
| < $15,000 | 14 | 3 |
| $15,000--$25,000 | 31 | 8 |
| $25,001--$50,000 | 104 | 25 |
| $50,001--$75,000 | 80 | 20 |
| $75,001--$100,000 | 40 | 10 |
| >$100,000 | 79 | 19 |
| I prefer not to say | 61 | 15 |
Twenty-four percent described their unaided hearing loss in their better ear as “profound,” 33% as “severe,” 28% as “moderate,” 10% as “mild,” and 4% as “normal” (i.e., unilateral). There was no significant difference between self-reported levels of hearing loss for those who provided audiograms (n = 209) and those who did not (n = 200), z = − 1.39, p = .16. Cohen’s k for agreement between self-reported levels of unaided hearing loss in the better ear and audiometric classifications indicated “fair” agreement (Landis & Koch, 1977), k = .350 (95% CI, .26 to .44), p < .0005, with self-reported ratings suggesting generally greater hearing impairment than audiometric findings, z = − 7.58, p < .0005. The study sample was negatively skewed as assessed by Shapiro-Wilk’s test (p < .05), with a significantly larger proportion of the participants describing their hearing loss as being in the severe or profound range. In addition, the women tended to describe their hearing loss as being more severe than the men (z = −3.26, p < .01).
The majority of the participants reported using some form of an assistive hearing device on a regular basis, with 70% reporting that they used either one or two hearing aids and 17% noting that they used either one or two cochlear implants. Thirteen percent reported that they did not use either a hearing aid or a cochlear implant. Among this latter subset of individuals, 50% described the level of hearing loss in their better ear as “normal” or “mild.” Fifty-three percent of the participants who indicated using an assistive hearing device reported being either “satisfied” or “very satisfied” with benefits derived from their hearing device, while 25% reported being either “dissatisfied” or “very dissatisfied” (see Table 2). Reported level of satisfaction was not associated to a statistically significant degree with severity of hearing loss, based on either self-reports or audiometric measures (r’s = 0.03 and − 0.10, respectively).
Table 2.
Audiologic characteristics of the study participants
| Characteristic | n | % |
|---|---|---|
| Severity of Hearing Loss in the Better Ear (Self-Report) (n = 409) | ||
| Normal (unilateral hearing loss) | 18 | 4 |
| Mild | 41 | 10 |
| Moderate | 116 | 28 |
| Severe | 133 | 33 |
| Profound | 97 | 24 |
| I don’t know | 4 | 1 |
| Severity of Hearing Loss in the Better Ear (Audiogram) (n = 199) | ||
| Normal (unilateral hearing loss) (PTA4 < 20 dB HL) | 7 | 3 |
| Mild (PTA4 = 20–40 dB HL) | 37 | 19 |
| Moderate (PTA4 = 41–70 dB HL) | 93 | 47 |
| Severe (PTA4 = 71–90 dB HL) | 39 | 20 |
| Profound (PTA4 > 90 dB HL) | 23 | 11 |
| Type of Hearing Devise Used (n = 409) | ||
| No hearing aid or cochlear implant | 54 | 13 |
| 1 hearing aid | 52 | 13 |
| 2 hearing aids | 233 | 57 |
| 1 cochlear implant | 37 | 9 |
| 2 cochlear implants | 11 | 3 |
| 1 cochlear implant, 1 hearing aid | 22 | 5 |
| Satisfaction with Assistive Hearing Device Benefits (n = 352) | ||
| Very satisfied | 45 | 13 |
| Satisfied | 142 | 40 |
| Neutral | 76 | 22 |
| Dissatisfied | 73 | 21 |
| Very Dissatisfied | 16 | 4 |
Note. PTA4 = Pure-tone average of hearing thresholds at 500 Hz, 1000 Hz, 2000 Hz, and 4000 Hz.
Descriptive Statistics and Reliability
We performed 10 iterations of multitrait scaling on questionnaires completed with no missing data or “not applicable” responses (n = 376), resulting in four subscales which we labeled: Psychological/Emotional (20 items), Social/Interpersonal (14 items), Activity/Community Participation (8 items), and Access to Information/Communication (13 items). Item-scale correlations for five items showed that they did not belong in any one scale, so these were treated as stand-alone items. A list of the IHEAR-IT scales and their corresponding items are presented in the Supplemental Materials (Supplementary Appendix A to be found online at http://informahealthcare.com http://informahealthcare.com/loi/ija).
Table 3 provides mean scores, standard deviations, floor and ceiling effects (scores of 0 or 100, respectively) for the four multi-item scales and five single items, and internal consistency reliability estimates for the four scales. Mean scale scores ranged from 45.1 (Access to Information/Communication) to 69.8 (Psychological/Emotional). Floor and ceiling effects were generally small for the four subscales, with less than 1% of the sample obtaining the lowest possible score (0) on any of the scales, and at most 7% of the sample achieving the highest possible score (100) on one scale (Activity/Community Participation). The five individual items had greater floor effects, ranging from 13% (effort involved compensating for hearing loss) to 22% (enjoyment of music), and ceiling effects, ranging from 4% (satisfaction with ability to understand information presented in lectures and meetings) to 20% (effort required to compensate for hearing loss).
Table 3.
Descriptive statistics and reliability estimates for the IHEAR-IT scales and items in the field test (n = 376)
| Scales/Individual Items | Number of Items |
Mean Score |
SD | % Scoring at the Floor |
% Scoring at the Ceiling |
Cronbach’s α |
|---|---|---|---|---|---|---|
| Psychological/Emotional | 20 | 69.8 | 18.7 | 0.0 | 0.0 | 0.96 |
| Social/Interpersonal | 14 | 56.5 | 22.6 | 0.0 | 0.5 | 0.95 |
| Activity/Community Participation | 8 | 62.4 | 26.4 | 0.8 | 7.2 | 0.93 |
| Access to Information and Communication | 13 | 45.1 | 23.5 | 0.3 | 0.0 | 0.94 |
| Effort compensating for hearing loss (Q3m) | 1 | 53.8 | 32.8 | 12.8 | 19.7 | NA |
| Stress when talking on the phone (Q3p) | 1 | 49.7 | 34.4 | 18.6 | 18.6 | NA |
| Satisfaction listening to lectures (Q4g) | 1 | 39.6 | 27.5 | 16.0 | 4.0 | NA |
| Satisfaction attending movies/plays (Q4h) | 1 | 39.5 | 29.6 | 19.1 | 6.1 | NA |
| Satisfaction listening to music (Q41) | 1 | 45.0 | 33.5 | 22.1 | 11.2 | NA |
|
| ||||||
| Worka (n = 162) | 7 | 65.1 | 24.2 | 0.0 | 5.0 | 0.89 |
| Intimacyb (n = 239) | 4 | 60.9 | 26.9 | 3.3 | 8.8 | 0.85 |
Note. All scales are scored with a possible range of 0 to 100, with lower scores reflecting poorer quality of life and higher scores indicating better functioning NA = not applicable; SD = standard deviation.
Only participants who indicated being actively employed completed items that comprise the Work scale. Responses on these items were not included in the larger multitrait scaling analysis.
Only participants who indicated being currently in an intimate relationship completed items that comprise the Intimacy/Sexual Relations scale. Responses on these items were analyzed separate from the larger multitrait scaling analysis.
Cronbach’s alpha for the multi-items scales ranged from 0.93 to 0.96. Three of the four scales were negatively skewed; the exception being Access to Information/Communication, which was positively skewed (0.22). Four of the individual items were positively skewed (range 0.02 to 0.39).
Work and Intimacy/Sexual Relations Scales
Both the Work scale (7 items) and the Intimacy/Sexual Relations scale (4 items) demonstrated high internal consistency reliability (α = 0.89 and 0.85, respectively), were slightly negatively skewed, had a wide spread in scores, and showed small floor and ceiling effects. (see Table 3)
Construct Validity
Table 4 shows descriptive statistics for scores obtained on the SF-36v2 and the HHIE/HHIA. Mean SF-36v2 scores were about the same as for the U.S. general population, ranging from 49 to 51 on the T-score metric.
Table 4.
Means and standard deviations for scores on the SF-36v2 and HHIE/HHIA (n = 376)
| Scales | Mean Score | SD | % Scoring at the Floor |
% Scoring at the Ceiling |
|---|---|---|---|---|
| SF-36v2a | ||||
| Physical functioning | 48.8 | 9.1 | 0.3 | 24.5 |
| Role—physical | 49.1 | 8.9 | 0.5 | 36.4 |
| Bodily pain | 50.5 | 9.3 | 0.3 | 22.1 |
| General health | 50.0 | 8.9 | 0.0 | 4.0 |
| Vitality | 51.1 | 9.8 | 0.8 | 1.3 |
| Social functioning | 49.2 | 9.3 | 0.0 | 46.0 |
| Role—emotional | 48.8 | 9.8 | 0.5 | 52.9 |
| Mental health | 50.1 | 9.8 | 0.0 | 4.3 |
| PCS | 49.6 | 9.0 | 0.0 | 0.0 |
| MCS | 49.9 | 10.6 | 0.0 | 0.0 |
| HHIE/HHIA | ||||
| Total Scoreb | 53.0 | 23.9 | 0.3 | 1.1 |
| Emotionalc | 25.6 | 13.6 | 2.1 | 2.9 |
| Sociald | 27.4 | 11.4 | 0.5 | 2.1 |
Note: Descriptive statistics reflect scores for participants included in the multitrait scaling analyses and not the entire study sample.
The SF-36v2 scales are normed to national data and have a mean of 50 and a standard deviation of 10, with lower scores reflecting poorer quality of life and higher scores indicating better functioning.
The HHIE/HHIA Total Score has a possible range of 0 to 100, with higher scores reflecting greater hearing handicap and lower scores indicating better functioning.
This subscale has a possible range of 0 to 52; higher scores indicate greater hearing handicap.
This subscale has a possible range of 0 to 48; higher scores indicate greater hearing handicap. SD = standard deviation.
Table 5 presents correlations between the IHEAR-IT four subscales, the SF-36v2, and the HHIE/HHIA. For comparison purposes, correlations between the HHIE/HHIA Total Score and the SF-36v2 component scores are also shown. As hypothesized, significant positive (“medium” to “large”) correlations were found between scores on the new scales and scores on the SF-36v2 MCS (r’s = 0.32 – 0.64). None of the IHEAR-IT scales correlated significantly with the SF-36v2 PCS. Further, consistent with our hypotheses, significant negative (“large”) correlations were found between the HHIE/HHIA Total Score and scores on the new scales (r ≥ −0.70), such that higher levels of self-reported hearing handicap, as measured by the HHIE/HHIA, were associated with poorer HRQOL on the IHEAR-IT. The IHEAR-IT Psychological/Emotional scale correlated strongly with the SF-36v2 MCS (r = 0.64). Of lesser magnitude was the association between the Access to Information and Communication scale and the MCS (r = 0.32). Not surprisingly, the correlations of greatest strength emerged between the HHIE/HHIA Total Score and the Social/Interpersonal and the Psychological/Emotional scales of the IHEAR-IT (r = −0.84 and −0.80, respectively).
Table 5.
Pearson correlations of the IHEAR-IT scales with the SF-36v2 summary scores and the HHIE/HHIA Total Score (n = 376)
| SF-36v2 PCS |
SF-36v2 MCS |
HHIE/HHIA Total Score |
|
|---|---|---|---|
| IHEAR-IT Scales | |||
| Psychological/Emotional | −0.02 | 0.64** | −0.80** |
| Social/Interpersonal | 0.01 | 0.48** | −0.84** |
| Activity/Community Participation | 0.10 | 0.34** | −0.70** |
| Access to Information and Communication | 0.04 | 0.32** | −0.75** |
| Worka (n = 162) | 0.08 | 0.36** | −0.65** |
| Intimacyb (n = 239) | −0.01 | 0.39** | −0.62** |
| SF-36v2 PCS | 1.00 | −0.09 | 0.04 |
| SF=36v2 MCS | −0.09 | 1.00 | −0.47** |
| HHIE/HHIA Total Score | 0.04 | −0.47** | 1.00 |
| HHIE/HHIA Social/Situational Score | 0.03 | −0.38** | 0.95** |
| HHIE/HHIA Emotional Score | 0.06 | −0.49** | 0.96** |
Note. PCS = physical component score; MCS = mental component score; HHIE/HHIA = Hearing Handicapped Inventory for the Elderly/Hearing Handicapped Inventory for Adults. Correlations without a superscript are not significant (p > 0.05).
p < 0.01.
Only participants who indicated being actively employed were included in the Work scale.
Only participants who indicated being currently in an intimate relationship were included in the Intimacy/Sexual Relations scale.
Examining associations between IHEAR-IT scale scores and demographic variables
Table 6 shows correlations between select demographic variables and scores on the IHEAR-IT. Consistent with our hypotheses, three subscales were significantly associated with age (small to medium strength) (Psychological/Emotional, r = 0.31, p < .001; Social/Interpersonal, r = 0.20, p < .001; and Access to Information/Communication, r = 0.12, p < .05), but the correlation was not significant for the Activity/Community Participation scale (r = 0.02, p > .05). Similarly, age showed significant positive (small to medium strength) correlations with four of the five individual items (r = 0.12 to 0.30), with older individuals generally reporting better HRQOL than younger individuals. Further, both self-reports of hearing loss level and audiometric findings showed significant relationships with the IHEAR-IT scales, including negative correlations of medium strength with the Psychological/Emotional scale (r’s = −0.27 and −0.29, respectively), and negative correlations of large magnitude with the other three subscales (r’s = −0.39 to −0.52).
Table 6.
Associations of IHEAR-IT scales and individual items with demographic variables and hearing loss
| Scales/Individual Items | Age | Annual Income |
Highest Educational Level |
Self-reported hearing loss levela |
Audiometric hearing loss levelb |
|---|---|---|---|---|---|
| Psychological/Emotional | 0.31** | 0.08 | 0.04 | − 0.27** | − 0.29** |
| Social/Interpersonal | 0.20** | 0.10 | 0.08 | − 0.39** | − 0.46** |
| Activity/Community Participation | 0.02 | 0.16** | 0.11* | − 0.49** | − 0.51** |
| Access to Information and Communication | 0.12* | 0.07 | 0.01 | − 0.44** | − 0.46** |
| Effort compensating for hearing loss (Q3m) | 0.30** | 0.08 | −0.03 | − 0.34** | − 0.35** |
| Stress when talking on phone (Q3p) | 0.21** | 0.09 | 0.07 | − 0.43** | − 0.39** |
| Satisfaction listening to lectures (Q4g) | 0.12* | 0.07 | 0.07 | − 0.33** | − 0.49** |
| Satisfaction attending movies/plays (Q4h) | 0.08 | 0.05 | −0.03 | − 0.36** | − 0.41** |
| Satisfaction listening to music (Q4i) | 0.20** | 0.09 | 0.01 | − 0.44** | − 0.34** |
Note.
n = 376.
n = 183.
Correlations without a superscript were not significant (p > 0.05).
p < 0.05.
p ≤ 0.01.
After controlling for age, duration of hearing loss showed significant negative correlations of small to medium strength with all four IHEAR-IT scales and individual items, indicating that individuals who had lived with a hearing loss for longer periods of time reported higher levels of HRQOL than individuals whose hearing loss had occurred more recently. Annual household income and educational level correlated significantly with the Activity/Community Participation scale (r’s = 0.16 and 0.11, respectively), but not with any other IHEAR-IT scale or individual item.
Females reported significantly lower HRQOL than men on two of the four IHEAR-IT scales (Psychological/Emotional and Access to Information), as well as on two of the five individual items (“effort required to compensate for hearing loss” and “stress when talking on the phone to an unfamiliar person”). However, the strength of these associations was small, with the exception of the Psychological/Emotional scale, which was of medium strength (t(374) = 5.08, p < .001, d = 0.56).
A series of multivariate ANOVAs were conducted to determine the effect of hearing device (i.e., hearing aid versus cochlear implant) on IHEAR-IT scores. After controlling for age and gender, there was a statistically significant difference for hearing device across the dependent variables (F(9, 314) = 5.67, p < .001; Wilks Lamba = .860). However, follow-up univariate F tests showed no significant differences between cochlear implant and hearing aid users for scores on the IHEAR-IT subscales. Only one of the five individual items yielded a significant group difference, with individuals with cochlear implants reporting that they experienced significantly less satisfaction listening to music (M = 28.0, SD = 30) than individuals with hearing aids (M = 46.9, SD = 33.2). Similar ANOVAs were conducted to examine the effect of hearing device on the HHIE/HHIA Total Score and subscale scores, and also the SF-36v2 PCS and MCS. Findings indicated nonsignificant associations between hearing device and scores on either measure.
Multiple regression analysis
Multivariate ordinary least squares regression analyses were performed to determine whether the IHEAR-IT explained unique variance in the participant’s global rating of quality of life and appraisal of the impact of hearing loss on his/her quality of life. Global rating of overall quality of life and attribution of the impact of hearing loss on quality of life were each assessed by a one-item index from the IHEAR-IT. The HHIE/HHIA Social/Situational and Emotional scales were significantly associated with global ratings of quality of life, F(2,309) = 39.16, p < .001, and explained 20% of the adjusted variance. However, the addition of significant IHEAR-IT scales (Psychological/Emotional and Social/Interpersonal), resulted in 28% adjusted variance (8% additional unique variance explained). The strongest predictor of the global rating of quality of life was the IHEAR-IT Psychological/Emotional scale (standardized regression coefficients followed by zero-order correlations: β = 0.33, p < 0.01; r = 0.52), followed by the IHEAR-IT Social/Interpersonal scale (β = 0.30, p < 0.01; r = 0.48). The HHIE/HHIA Social/Situational scale (β = 0.24, p < 0.05; r = −0.35) also had a significant unique association with the global rating of quality of life, but the regression coefficient was a suppression effect (zero order correlation was negative but beta was positive). The HHIA/HHIA Emotional scale was not significantly, uniquely associated with the participants’ global rating of quality of life (β = −0.14, p = .17; r = −0.45).
The HHIE/HHIA scales were significantly associated with the global rating of the impact of hearing loss on overall quality of life, F(2,309) = 110.32, p < .001, accounting for 41% of the adjusted variance. However, adding significant IHEAR-IT scales and items yielded an adjusted R2 of 50% (9% unique variance explained). The IHEAR-IT Social/Interpersonal scale and the HHIE/HHIA Emotional scale accounted for equal amounts of unique variance (β = 0.30, p < .001; r = 0.64 and β = 0.30, p < .01; r = 0.66, respectively); followed by the IHEAR-IT Access to Information scale (β = 0.16, p < .05; r = 0.59); and finally, one IHEAR-IT individual item (“effort required to compensate for hearing loss” [q3m] (β = 0.18, p < .01; r = 0.53). The HHIA/HHIA Social/Situational scale was not significantly, uniquely associated with rating of impact of hearing loss on quality of life (p = .11).
Discussion
This paper describes the development, field testing, and preliminary psychometric evaluation of the IHEAR-IT, a HRQOL instrument for individuals with AOHL. Although other HRQOL measures for individuals with hearing impairment exist, the IHEAR-IT is unique in that it is a multidimensional HRQOL measure. Furthermore, while the IHEAR-IT and the HHIE/HHIA overlap in some content, regression models demonstrated that the IHEAR-IT was significantly uniquely associated with the participants’ global rating of quality of life and appraisal of the impact of hearing loss on everyday life activities and well-being beyond the HHIE/HHIA.
The development of the IHEAR-IT followed stringent procedures recommended by the HRQOL research community (Hays & Revicki, 2005; Reeve et al, 2012) and set forth by the FDA Guidance to Industry (2009). Concerted effort was made to include the perspective and advice of individuals with AOHL and various professionals who serve them. Consistent with the study’s aim, the IHEAR-IT provides a comprehensive assessment of the impact of AOHL, which is linked to current conceptual models of HRQOL and guided by the WHO-ICF theoretical framework. In addition, the IHEAR-IT targets themes and domains identified by individuals with AOHL as important and relevant to their lives.
The 73-item IHEAR-IT was completed by a diverse sample of 409 individuals with varying degrees of AOHL, who resided in different geographic areas of the United States. Multitrait scaling techniques provided support for four multi-item scales and five individual items. Findings indicate that the IHEAR-IT demonstrates excellent internal consistency reliability, with coefficient alpha easily exceeding the 0.70 minimum for group comparisons (Nunnally & Bernstein, 1994). Support for the construct validity of the four scales was found based on correlations with the SF-36v2 (MCS) and the HHIE/HHIA.
Construct validity was further demonstrated by confirmation of hypothesized patterns of associations between the IHEAR-IT scale scores and individual characteristics. Consistent with research on general populations (e.g., Hanmer et al., 2007) and specific to individuals with hearing loss (Hallberg et al., 2008; Helvik et al., 2006; Nachtegaal et al., 2009; Tambs, 2004), women and younger individuals in our study reported poorer HRQOL on the IHEAR-IT than did males and older individuals. Further, as anticipated, the IHEAR-IT scales and its five individual items correlated significantly with hearing loss severity, such that greater hearing loss was associated with poorer HRQOL. This finding is consistent with previous research, including several large epidemiological studies (e.g., Chia et al., 2007; Dalton et al., 2003), though correlations reported have often been small. That the associations between hearing impairment and HRQOL found in this study are stronger than correlations identified in other studies may be due to the use of self-reports of hearing loss level rather than audiometric measures. If so, these findings are in keeping with those reported by Tambs (2004), in which self-reported hearing loss explained self-reported mental health and subjective well-being much better than did measured hearing loss.
Consistent with our expectations, the IHEAR-IT correlated significantly with the SF-36v2 MCS but not with the PCS; however, the mean scores for the two scales were similar to those for the U.S. general population. Studies that have used the SF-36v2 to evaluate HRQOL for individuals with hearing loss have reported varied findings, with some showing an association between greater hearing loss and poorer scores on both the SF-36 PCS and MCS (e.g., Chia et al., 2007; Dalton et al., 2003), other studies reporting no significant relationships (e.g., Chew & Yeak, 2010; Hickson et al., 2008; Hua et al., 2013; Parving et al, 2001), and yet others, like ours, reporting significant associations only with the MCS (e.g., Abrams et al., 2002). Since hearing loss is considered a communication disability rather than a physical disability or disease, it is not surprising that the SF-36v2 MCS would be more sensitive to the daily experiences and challenges for individuals with AOHL than would the PCS. On the other hand, a growing body of research is identifying significant associations between hearing loss in older individuals and cognitive decline, falls, and impaired activities of daily living (Gopinath, et al., 2011; Gurgel et al., 2014; Lin et al., 2013; Peracino, 2014). However, for the general population of individuals with hearing loss, especial younger individuals and individuals who are otherwise physically heathy, the SF-36v2 and other generic HRQOL measures, have been reported to lack sensitivity and specificity in assessing the impact of hearing loss on HRQOL (Bess, 2000; Chew & Yeak, 2010; Mo et al., 2004). Findings from this study support this conclusion, which underscores the need for a robust, condition-specific HRQOL such as the IHEAR-IT.
There are a number of limitations to this study that should be acknowledged. First, the study sample was significantly skewed with respect to hearing loss level, with a greater proportion of the participants reporting hearing loss in the severe and profound ranges than in the mild and moderate ranges. As such, these participants are not representative of the general population of adults with hearing loss in the United States, in which the majority (62%) report having “a little trouble hearing” (Zelaya et al., 2015). In addition, the participants were recruited from the community using flyers distributed in hearing clinics and notices placed on Internet bulletin boards, listservs, and consumer organizations' websites. These recruitment strategies and locations possibly attracted individuals who experience more adjustment problems related to their hearing loss than the general population, and, as such, there may be an issue with sampling bias. Additionally, some participants were members of consumer organizations such as Hearing Loss Association of America, which likely means that these individuals are more aware of their hearing loss and the impact it has on their life. Compared to the general population, these individuals may be more proactive regarding the use of assistive technologies and accommodations that can help reduce hearing disability. The study sample was also predominantly Caucasian, educated, and financially secure. Although empirical data are limited, findings from some studies suggest that different race/ethnic groups and cultures may experience the impact of hearing loss differently (Marcus-Bernstein, 1986; Wong & Cheng, 2012). Given the characteristics of the study sample, findings from this study may not be generalizable.
Another limitation of the study was the relatively small number of individuals who were employed and, therefore, able to answer questions about the impact of their hearing loss in the work environment (60%). Focus groups used to generate relevant items to be included in the field test instrument identified employment as an area significantly impacted by hearing loss. Many of the focus group participants who were employed reported experiencing elevated levels of psychosocial distress, anxiety, and fatigue related to carrying out their job responsibilities. Some indicated a reluctance to inform supervisors and coworkers of their hearing loss, fearing negative stigmatization and limited opportunities for career advancement. Almost all reported expending extra effort at work to compensate for their hearing loss. Similar findings have been reported in other studies (e.g., Danermark, 2005; Helvick et al., 2013; Hua et al., 2013; Kramer et al., 2008; Williams et al., 2015). Future plans for the IHEAR-IT include administration to young adults with AOHL to gather additional data about this important domain of HRQOL.
Items addressing intimacy in the field test instrument were completed by a relatively small proportion of the participants. Younger adults in the focus groups and those completing the field test instrument often identified “intimacy” and “dating” as areas significantly impacted by their hearing loss. Concerns were noted regarding the difficulty of socializing in large groups and meeting potential life-partners. Some participants commented about the perceived “un-sexiness” of hearing aids and cochlear implants. Several respondents mentioned experiencing uncertainty about what to do with their hearing aids or cochlear implants during sexual activity: “Should I keep my cochlear implant processor on or take it off? If I take it off, I can’t hear! If I keep it on, it gets in the way. It really is awkward!” This is a significant concern for some individuals with hearing loss, especially younger individuals with AOHL who are at a stage in life when they are attempting to establish intimate relationships. Although published research on the effects of hearing loss on sexual health is rare, a recent study by Ozler and Ozler (2013) and another by Bakir, Penbegul, and Gun (2012) both found that acquired sensorineural hearing loss can adversely affect men’s sexual health, including sexual desire, erectile function, and sexual satisfaction. No published studies have focused on the impact of acquired hearing loss on female sexual health and HRQOL. Clearly this is an area that warrants further investigation.
We were able to obtain a recent audiogram for only half of the sample. We have no way of knowing whether these audiograms reflect the individual’s current hearing status, as some records were as much as three years old. For those who did not provide audiograms, we had to rely on self-reports regarding the participants’ degree of hearing loss, which of course limits our confidence in the accuracy of our reports. Although analysis of a subset of our sample indicated “fair” agreement between self-reported levels of hearing loss in the better ear and audiometric classifications, future research in the development and application of this HRQOL instrument should obtain audiometric measures of the participant’s hearing around the same time that the test instrument is completed.
Finally, although participants noted that the IHEAR-IT was easy to complete and captured relevant areas impacted by hearing loss, the length of the IHEAR-IT (73 items) may compromise its practicality and feasibility for use in both clinical and research settings. The next step in the development of this measure is to reduce the number items it contains and examine its test-retest reliability and responsiveness to change. Additional research will be needed to establish the value of the IHEAR-IT for evaluating individual with varying degrees of hearing loss and different populations. Further, in keeping with the WHO-ICF paradigm of functioning, disability, and health, future research with the IHEAR-IT will investigate the potential contributions of environmental, social, and personality factors on HRQOL for individuals with AOHL.
Conclusion
The aim of the present study was to develop a comprehensive measure of HRQOL targeted at individuals with AOHL and provide initial evaluation of its psychometric properties. We are currently planning the next iterative phase of instrument development, which involves development and field testing a shorter version of the IHEAR-IT and evaluating the instrument’s feasibility, test-retest reliability, and responsiveness to change. Despite limitations noted, the IHEAR-IT shows promising potential. We anticipate that our future research endeavors will produce a valuable tool that can enhance our understanding of the functioning and well-being of individuals with AOHL. Moreover, we believe the IHEAR-IT will be valuable in quantifying benefits of treatment and interventions, and ultimately better inform health policy efforts.
Supplementary Material
Acknowledgements
This work was supported by a grant from the U.S. Dept. of Education, National Institute on Disability and Rehabilitation Research (NIDRR), Field Initiated Research Grant# H133G030191. Ron Hays was supported in part by a grant from the National Cancer Institute (NCI), 1U2-CCA186878-01. We would like to express thanks to members of the Expert Advisory Panel for their helpful suggestions. We especially would like to thank Hearing Loss Association of America for its support and assistance in recruiting subjects for this study.
Abbreviations
- AOHL
Adult-onset hearing loss
- FDA
U.S. Food and drug administration
- HHIE
Hearing handicapped inventory for the elderly
- HHIA
Hearing handicapped inventory for adults
- HRQOL
Health-related quality of life
- SF-36v2
36-Item Short Form Health Survey, Version 2.0
- PCS
Physical component summary
- MCS
Mental component summery
Footnotes
Supplementary material available online
Supplementary Appendix A available online at http://informahealthcare.com/loi/ija.
References
- Abrams H, Chisolm TH, McArdle R. A cost-utility analysis of adult group audiologic rehabilitation: Are the benefits worth the cost? J Rehabil Res Dev. 2002;39(5):549–558. [PubMed] [Google Scholar]
- Bakir S, Penbegul N, Gun R. Relationship between hearing loss and sexual dysfunction. J Laryngol Otol. 2012;20:1–6. doi: 10.1017/S0022215112002952. [DOI] [PubMed] [Google Scholar]
- Bess F. The role of generic health-related quality of life measures in establishing audiological rehabilitation outcomes. Ear Hear. 2000;21(4Suppl):74–79. doi: 10.1097/00003446-200008001-00009. [DOI] [PubMed] [Google Scholar]
- Chew HS, Yeak S. Quality of life in patients with untreated age-related hearing loss. J Laryngol Otol. 2010;124(8):835–41. doi: 10.1017/S0022215110000757. [DOI] [PubMed] [Google Scholar]
- Chia EM, Wang JJ, Rochtchina E, Cumming RR, Newall P, Mitchell P. Hearing impairment and health-related quality of life: the Blue Mountains Hearing Study. Ear Hear. 2007;28(2):187–195. doi: 10.1097/AUD.0b013e31803126b6. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Cunningham WE, Burton TM, Hawes-Dawson J, Kington RS, Hays RD. Use of relevancy ratings by target respondents to develop health-related quality of life measures: An example with African-American elderly. Qual Life Res. 1999;8(8):749–768. doi: 10.1023/a:1008966817515. [DOI] [PubMed] [Google Scholar]
- Dalton DS, Cruickshanks KJ, Klein BE, Klein R, Wiley TL, et al. The impact of hearing loss on quality of life in older adults. Gerontologist. 2003;43(5):661–668. doi: 10.1093/geront/43.5.661. [DOI] [PubMed] [Google Scholar]
- Danermark B. A review of the psychosocial effects of hearing impairment in the working age population. In: Stephens, Jones, editors. The Impact of Genetic Hearing Impairment. Whurr; London: 2005. pp. 106–136. [Google Scholar]
- FDA Guidance for Industry Patient-reported outcome measures: Use in medical product development to support labeling claims [online] 2009 doi: 10.1186/1477-7525-4-79. available from: http://www.fda.gov/downloads/Drugs/Guidances/UCM193282.pdf [accessed March 20, 2015] [DOI] [PMC free article] [PubMed]
- Ferrans CE, Zerwic JJ, Wilbur JE, Larson JL. Conceptual model of health-related quality of life. J Nurs Scholarsh. 2005;37(4):336–342. doi: 10.1111/j.1547-5069.2005.00058.x. [DOI] [PubMed] [Google Scholar]
- Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;309(22):2322–2324. doi: 10.1001/jama.2013.5912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopinath B, Schneider J, McMahon CM, Teber E, Leeder SR, Mitchell P. Severity of age-related hearing loss is associated with impaired activities of daily living. Age & Aging. 2012;41:195–200. doi: 10.1093/ageing/afr155. [DOI] [PubMed] [Google Scholar]
- Gurgel RK, Ward PD, Schwartz S, Norton MC, Foster NL, Tschanz JT. Relationship of hearing loss and dementia: A prospective, population-based study. Otol Neurotol. 2014;35(5):775–781. doi: 10.1097/MAO.0000000000000313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallberg LR, Hallberg U, Kramer SE. Self-reported hearing difficulties, communication strategies and psychological general well-being (quality of life) in patients with acquired hearing impairment. Disabil Rehabil. 2008;30(3):203–212. doi: 10.1080/09638280701228073. [DOI] [PubMed] [Google Scholar]
- Hanmer J, Hays RD, Fryback DG. Mode of administration is important in US national estimates of health-related quality of life. Med Care. 2007;45(12):1171–1179. doi: 10.1097/MLR.0b013e3181354828. [DOI] [PubMed] [Google Scholar]
- Hays RD, Hahn H, Marshall G. Use of the SF-36 and other health-related quality of life measures to assess persons with disabilities. Arch Phys Med Rehabil. 2002;83:S4–S9. doi: 10.1053/apmr.2002.36837. [DOI] [PubMed] [Google Scholar]
- Hays RD, Revicki D. Reliability and validity (including responsiveness) In: Fayers, Hays, editors. Assessing Quality of Life in Clinical Trials: Second Edition. Oxford University Press; New York: 2005. pp. 25–39. [Google Scholar]
- Hays RD, Fayers P. Evaluating multi-item scales. In: Fayers, Hays, editors. Assessing Quality of Life in Clinical Trials: Second Edition. Oxford University Press; New York: 2005. pp. 9–23. [Google Scholar]
- Hays RD, Wang E. Multitrait Scaling Program: MULTI; Proceedings of the Seventeenth Annual SAS Users Group International Conference.Apr, 1992. pp. 1151–1156. [Google Scholar]
- Healthy People 2020 . The Vision, Mission, and Goals of Healthy People 2020. Overarching goals. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion; Washington, DC: Healthy People 2020 Framework. www.healthypeople.gov/sites/default/files/HP2020Framework.pdf. [accessed April 5, 2015] [Google Scholar]
- Helvik AS, Jacobsen G, Hallberg LR. Psychological well-being of adults with acquired hearing impairment. Disabil Rehabil. 2006;28(9):535–545. doi: 10.1080/09638280500215891. [DOI] [PubMed] [Google Scholar]
- Helvik AS, Krokstad S, Tambs K. Hearing loss and risk of early retirement. The HUNT study. Eur J Pub Health. 2013;23(4):617–622. doi: 10.1093/eurpub/cks118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickson L, Allen J, Beswick R, Flton M, Wolf D, Worrall L, Scarinci N. Relationships between hearing disability, quality of life and wellbeing in older community-based Australians. The Australian and Zealand Journal of Audiology. 2008;30(2):99–112. [Google Scholar]
- Hua H, Karlsson J, Widen S, Moller C, Lyxell B. Quality of life, effort and disturbance perceived in noise: A comparison between employees with aided hearing impairment and normal hearing. Int J Audiol. 2013;52:642–649. doi: 10.3109/14992027.2013.803611. [DOI] [PubMed] [Google Scholar]
- IBM Corp. Released 2013 . IBM SPSS Statistics for Windows. IBM Corp; Armonk, NY: Version 22.0. [Google Scholar]
- Kramer SE, Kapteyn TS, Houtgast T. Occupational performance: Comparing normally-hearing and hearing-impaired employees using the Amsterdam Checklist for Hearing and Work. Int J Audiol. 2006;45(9):503–512. doi: 10.1080/14992020600754583. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- Lin FR, Yaffe K, Xia J, Xue QL, Harris TB, Purchase-Helzner E, Satterfield S, Ayonayon HN, Ferrucci L, Simonsick EM. Health ABC Study Group: Hearing loss and cognitive decline among older adults. JAMA Int Med. 2013;173:293–299. doi: 10.1001/jamainternmed.2013.1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus-Bernstein C. Audiologic and nonaudiologic correlates of hearing handicap in Black elderly. J Speech Lang Hear Res. 1986;29(3):301–312. doi: 10.1044/jshr.2903.301. [DOI] [PubMed] [Google Scholar]
- Mo B, Harris S, Lindbaek M. Cochlear implants and health status: a comparison with other hearing-impaired patients. Ann Otol Rhinol Laryngol. 2004;113(11):914–21. doi: 10.1177/000348940411301111. [DOI] [PubMed] [Google Scholar]
- Monzani D, Galeazzi G, Genovese E, Marrara A, Martini A. Psychological profile and social behaviour of working adults with mild or moderate hearing loss. Acta Otorhinolaryngol Ital. 2008;28(2):61–66. [PMC free article] [PubMed] [Google Scholar]
- Mullin PA, Lohr KN, Bresnahan BW, McNulty P. Applying cognitive design principles to formatting HRQOL instruments. Qual Life Res. 2000;9(1):13–27. doi: 10.1023/a:1008923301313. [DOI] [PubMed] [Google Scholar]
- Mulrow CD, Aguilar C, Endicott JE, Tuley MR, Velez R, et al. Quality-of-life changes and hearing impairment: A randomized trial. Ann Intern Med. 1990;113(3):188–194. doi: 10.7326/0003-4819-113-3-188. [DOI] [PubMed] [Google Scholar]
- Nachtegaal J, Smit JH, Smits C, Bezemer PD, van Beek JH, et al. The association between hearing status and psychosocial health before the age of 70 years: results from an internet-based national survey on hearing. Ear Hear. 2009;30(3):302–312. doi: 10.1097/AUD.0b013e31819c6e01. [DOI] [PubMed] [Google Scholar]
- Newman CW, Jacobson GP, Hug GA, Sandridge SA. Perceived hearing handicap of patients with unilateral or mild hearing loss. Ann Otol Rhinol Laryngol. 1997;106(3):210–214. doi: 10.1177/000348949710600305. [DOI] [PubMed] [Google Scholar]
- Newman CW, Weinstein BE, Jacobson GP, Hug GA. The hearing handicap inventory for adults: Psychometric adequacy and audiometric correlates. Ear Hear. 1990;11(6):430–433. doi: 10.1097/00003446-199012000-00004. [DOI] [PubMed] [Google Scholar]
- Nunnally JC, Bernstein IH, editors. Psychometric Theory. 3rd McGraw-Hill, Inc; New York: 1994. [Google Scholar]
- Ozler GS, Ozler S. Quality of social and sexual life in males with hearing loss. Int Adv Otol. 2013;9(2):211–218. [Google Scholar]
- Parving A, Parving I, Erlendsson A, Christensen B. Some experiences with hearing disability/handicap and quality of life measures. Int J Audiol. 2001;40:208–214. [PubMed] [Google Scholar]
- Peracino A. Hearing loss and dementia in the aging population. Audiol Neurotol. 2014;19(suppl 1):6–9. doi: 10.1159/000371595. [DOI] [PubMed] [Google Scholar]
- Reeve BB, Wyrwich KW, Wu AW, Velikova G, Terwee BB, et al. ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Qual Life Res. 2013;22(8):1889–1905. doi: 10.1007/s11136-012-0344-y. [DOI] [PubMed] [Google Scholar]
- Spilker B. Introduction. In: Spilker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials: Second Edition. Lippincott-Raven; Philadelphia: 1996. pp. 1–10. [Google Scholar]
- Stika CJ. Living with hearing loss – Focus group results: Part I: Family relationships and social interaction. Hearing Loss. l997a;18(5):22–28. [Google Scholar]
- Stika CJ. Living with hearing loss – Focus group results: Part II: Career developments and work experiences. Hearing Loss. l997b;18(6):29–32. [Google Scholar]
- Tambs K. Moderate effects of hearing loss on mental health and subjective well-being: Results from the Nord-Trøndelag hearing loss study. Psychosom Med. 2004;66(5):776–782. doi: 10.1097/01.psy.0000133328.03596.fb. [DOI] [PubMed] [Google Scholar]
- Tate DG, Pledger C. An integrative conceptual framework of disability: New directions for research. Am Psychol. 2003;58(4):289–295. doi: 10.1037/0003-066x.58.4.289. [DOI] [PubMed] [Google Scholar]
- Thomas AJ. Acquired hearing loss: Psychological and psychosocial implications. Academic Press; London: 1984. [Google Scholar]
- Trybus R, Stika C, Goulder J. Final Project Report: Rehabilitation Research and Training Center for Persons Who Are Hard of Hearing or Late Deafened. U.S. Dept. of Education, National Institute on Disability and Rehabilitation Research; Washington, DC: Apr, 2004. [Google Scholar]
- US Burden of Disease Collaboration The state of US Health, 1990-2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310(1):591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventry I, Weinstein B. The hearing handicap inventory for the elderly: A new tool. Ear Hear. 1982;3(3):128–134. doi: 10.1097/00003446-198205000-00006. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Dewey JE. How to score version two of the SF-36 Health Survey. Quality Metric, Incorporated; Lincoln, RI: 2000. [Google Scholar]
- Williams KC, Falkum E, Martinsen EW. Fear of negative evaluation, avoidance and mental distress among hearing-impaired employees. Rehabil Psychol. 2015;60(1):51–58. doi: 10.1037/rep0000028. [DOI] [PubMed] [Google Scholar]
- Wong LL, Cheng LK. Quality of life in older Chinese-speaking adults with hearing impairment. Disabil Rehabil. 2012;34(8):655–664. doi: 10.3109/09638288.2011.619614. [DOI] [PubMed] [Google Scholar]
- World Health Organization Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference; New York. Jun 19-22, 1946. signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organizations, no. 2, p. 100) and entered into force on 7 April 1948. www.who.int/about/en [accessed January 5, 2015] [Google Scholar]
- World Health Organization . WHO International Classification of Functioning, Disability and Health (WHO-ICF) Author; Geneva: 2001. [Google Scholar]
- Zelaya CE, Lucas JW, Hoffman H,J. NCHS data brief, no 214. National Center for Health Statistics; Hyattsville, MD: 2015. Self-reported hearing trouble in adults aged 18 and over: United States, 2014. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.