Abstract
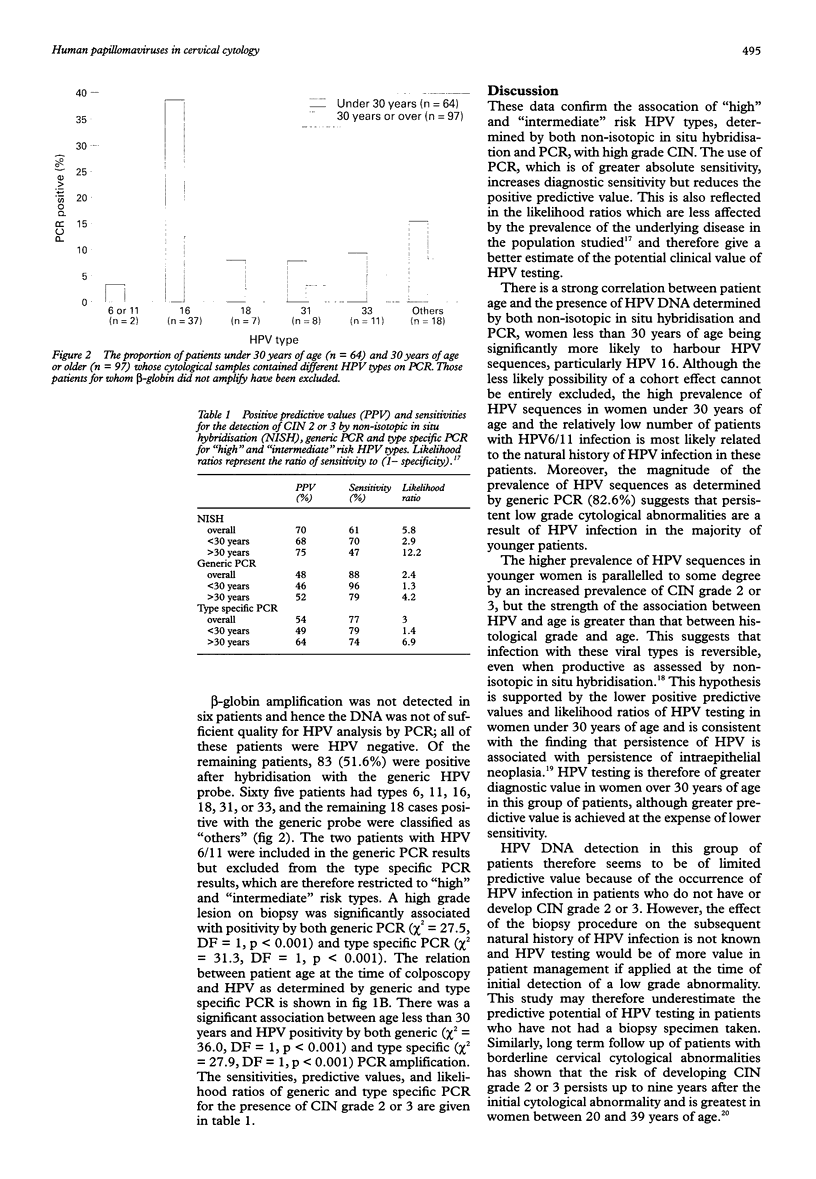
AIM: To assess the diagnostic performance of human papillomavirus (HPV) analysis in predicting cervical intraepithelial neoplasia (CIN) grades 2 and 3 in patients with persistent low grade cervical cytological abnormalities. METHODS: Cervical smears from 167 women referred for colposcopy with persistent borderline, wart virus or mildly dyskaryotic changes on cervical screening were analysed by Papanicolaou staining, non-isotopic in situ hybridisation and generic and type specific polymerase chain reaction (PCR) amplification of HPV sequences. Follow up was by cytological and, where appropriate, histological analysis. RESULTS: CIN grade 2 or 3 was identified in 46 patients after a median follow up of 27 months. HPV positivity by both techniques was associated with high grade CIN and with age less than 30 years (median age 33 years). Non-isotopic in situ hybridisation was more predictive but less sensitive than either generic or type specific PCR, but prediction was greater using either molecular technique in women over 30 years of age. CONCLUSIONS: Although the degree of prediction found is of only limited clinical value, the strong association of HPV positivity with both high grade CIN and patient age suggests that further studies of HPV testing in this patient group are warranted.
Full text
PDF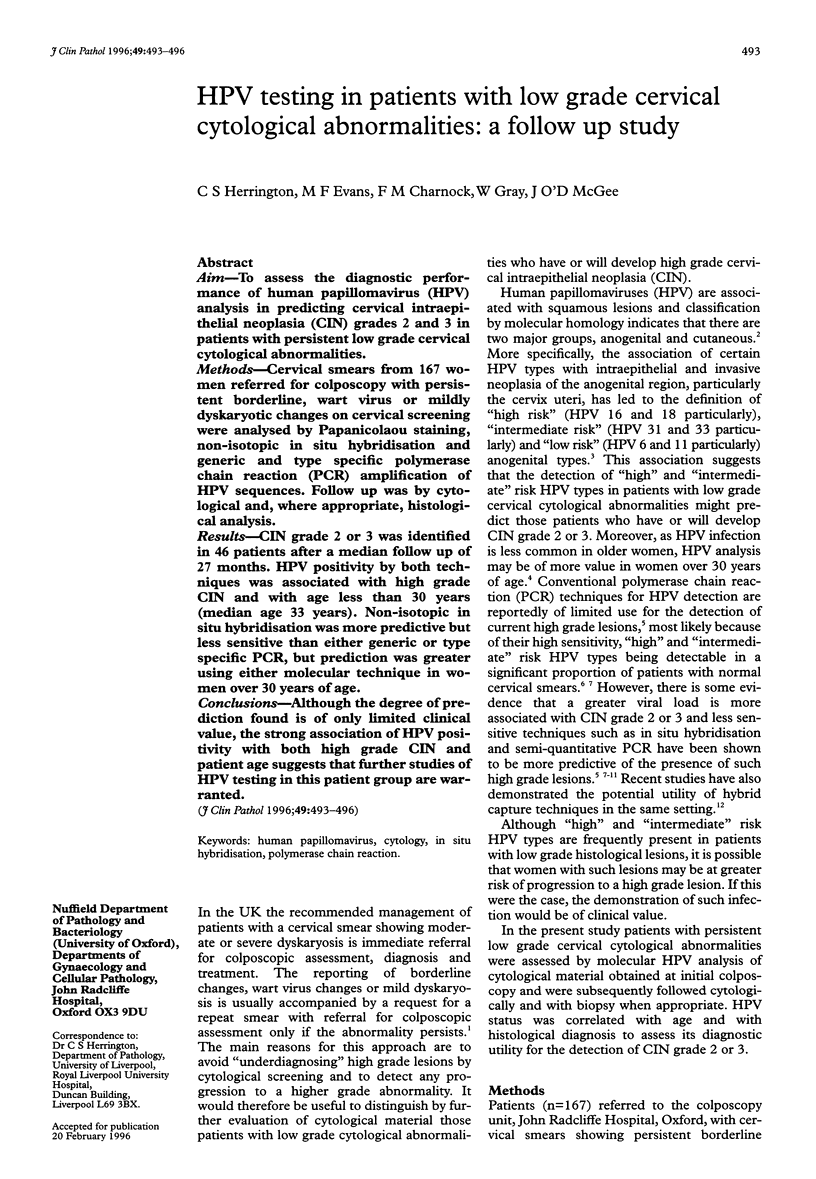

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bavin P. J., Giles J. A., Deery A., Crow J., Griffiths P. D., Emery V. C., Walker P. G. Use of semi-quantitative PCR for human papillomavirus DNA type 16 to identify women with high grade cervical disease in a population presenting with a mildly dyskaryotic smear report. Br J Cancer. 1993 Mar;67(3):602–605. doi: 10.1038/bjc.1993.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox J. T., Lorincz A. T., Schiffman M. H., Sherman M. E., Cullen A., Kurman R. J. Human papillomavirus testing by hybrid capture appears to be useful in triaging women with a cytologic diagnosis of atypical squamous cells of undetermined significance. Am J Obstet Gynecol. 1995 Mar;172(3):946–954. doi: 10.1016/0002-9378(95)90026-8. [DOI] [PubMed] [Google Scholar]
- Cuzick J., Szarewski A., Terry G., Ho L., Hanby A., Maddox P., Anderson M., Kocjan G., Steele S. T., Guillebaud J. Human papillomavirus testing in primary cervical screening. Lancet. 1995 Jun 17;345(8964):1533–1536. doi: 10.1016/s0140-6736(95)91086-7. [DOI] [PubMed] [Google Scholar]
- Cuzick J., Terry G., Ho L., Hollingworth T., Anderson M. Human papillomavirus type 16 in cervical smears as predictor of high-grade cervical intraepithelial neoplasia [corrected]. Lancet. 1992 Apr 18;339(8799):959–960. doi: 10.1016/0140-6736(92)91532-d. [DOI] [PubMed] [Google Scholar]
- Cuzick J., Terry G., Ho L., Hollingworth T., Anderson M. Type-specific human papillomavirus DNA in abnormal smears as a predictor of high-grade cervical intraepithelial neoplasia. Br J Cancer. 1994 Jan;69(1):167–171. doi: 10.1038/bjc.1994.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrington C. S., Evans M. F., Hallam N. F., Charnock F. M., Gray W., McGee J. D. Human papillomavirus status in the prediction of high-grade cervical intraepithelial neoplasia in patients with persistent low-grade cervical cytological abnormalities. Br J Cancer. 1995 Jan;71(1):206–209. doi: 10.1038/bjc.1995.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrington C. S. Human papillomaviruses and cervical neoplasia. I. Classification, virology, pathology, and epidemiology. J Clin Pathol. 1994 Dec;47(12):1066–1072. doi: 10.1136/jcp.47.12.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrington C. S., de Angelis M., Evans M. F., Troncone G., McGee J. O. Detection of high risk human papillomavirus in routine cervical smears: strategy for screening. J Clin Pathol. 1992 May;45(5):385–390. doi: 10.1136/jcp.45.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschowitz L., Raffle A. E., Mackenzie E. F., Hughes A. O. Long term follow up of women with borderline cervical smear test results: effects of age and viral infection on progression to high grade dyskaryosis. BMJ. 1992 May 9;304(6836):1209–1212. doi: 10.1136/bmj.304.6836.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho G. Y., Burk R. D., Klein S., Kadish A. S., Chang C. J., Palan P., Basu J., Tachezy R., Lewis R., Romney S. Persistent genital human papillomavirus infection as a risk factor for persistent cervical dysplasia. J Natl Cancer Inst. 1995 Sep 20;87(18):1365–1371. doi: 10.1093/jnci/87.18.1365. [DOI] [PubMed] [Google Scholar]
- Lorincz A. T., Reid R., Jenson A. B., Greenberg M. D., Lancaster W., Kurman R. J. Human papillomavirus infection of the cervix: relative risk associations of 15 common anogenital types. Obstet Gynecol. 1992 Mar;79(3):328–337. doi: 10.1097/00006250-199203000-00002. [DOI] [PubMed] [Google Scholar]
- Meijer C. J., van den Brule A. J., Snijders P. J., Helmerhorst T., Kenemans P., Walboomers J. M. Detection of human papillomavirus in cervical scrapes by the polymerase chain reaction in relation to cytology: possible implications for cervical cancer screening. IARC Sci Publ. 1992;(119):271–281. [PubMed] [Google Scholar]
- Schiffman M. H., Bauer H. M., Hoover R. N., Glass A. G., Cadell D. M., Rush B. B., Scott D. R., Sherman M. E., Kurman R. J., Wacholder S. Epidemiologic evidence showing that human papillomavirus infection causes most cervical intraepithelial neoplasia. J Natl Cancer Inst. 1993 Jun 16;85(12):958–964. doi: 10.1093/jnci/85.12.958. [DOI] [PubMed] [Google Scholar]
- Schiffman M. H. Recent progress in defining the epidemiology of human papillomavirus infection and cervical neoplasia. J Natl Cancer Inst. 1992 Mar 18;84(6):394–398. doi: 10.1093/jnci/84.6.394. [DOI] [PubMed] [Google Scholar]