Abstract
Children with disabilities are thought to have an increased risk of unintentional injuries, but quantitative syntheses of findings from previous studies have not been done. We conducted a systematic review and meta-analysis to assess whether pre-existing disability can increase the risk of unintentional injuries among children when they are compared to children without disability. We searched 13 electronic databases to identify original research published between 1 January 1990 and 28 February 2013. We included those studies that reported on unintentional injuries among children with pre-existing disabilities compared with children without disabilities. We conducted quality assessments and then calculated pooled odds ratios of injury using random-effects models. Fifteen eligible studies were included from 24,898 references initially identified, and there was a total sample of 83,286 children with disabilities drawn from the eligible studies. When compared with children without disabilities, the pooled OR of injury was 1.86 (95 % CI 1.65–2.10) in children with disabilities. The pooled ORs of injury were 1.28, 1.75, and 1.86 in the 0–4 years, 5–9 years, and ≥10 years of age subgroups, respectively. Compared with children without disabilities, the pooled OR was 1.75 (95 % CI 1.26–2.43) among those with International Classification of Functioning (ICF) limitations. When disability was defined as physical disabilities, the pooled OR was 2.39 (95 % CI 1.43–4.00), and among those with cognitive disabilities, the pooled OR was 1.77 (95 % CI 1.49–2.11). There was significant heterogeneity in the included studies. Compared with peers without disabilities, children with disabilities are at a significantly higher risk of injury. Teens with disabilities may be an important subgroup for future injury prevention efforts. More data are needed from low- and middle-income countries.
Keywords: Disability, Injury, Meta-analysis, Children
Review
Introduction
The 2013 State of the World’s Children report is focused on improving the lives of children with disabilities by promoting more inclusive societies where “physical, attitudinal, and political barriers are dismantled” (UNICEF 2013). The Global Burden of Disease estimate that 5.1 % of children worldwide (about 93 million) have moderate or severe disability is often cited (WHO 2011), but this estimate is not reliable given the substantial variation in disability definitions and surveillance/study methodologies (UNICEF 2013). From one country to another, the reported prevalence of disability in children ranges from 0.4 to 18.0 % (Maulik and Darmstadt 2007; Sinclair and Xiang 2008). It has been estimated that around 80 % of children with disabilities live in developing countries (WHO 2011). There is increasing recognition of disparities in health experienced by individuals with disabilities when compared with those without disabilities, including increased risks of violence (Jones et al. 2012) and unintentional injury (WHO et al. 2011). Injury is the leading cause of morbidity and mortality in children, therefore injury prevention rather than overprotection in this special population is important particularly as societies move toward greater inclusion (Wang et al. 2008; Kendrick et al. 2013b; UNICEF 2013).
The risk of violence against individuals with disabilities has been the subject of two meta-analyses (Hughes et al. 2012; Jones et al. 2012), including one among children with disabilities (Jones et al. 2012). Our previous meta-analysis in adults with disabilities demonstrated that they are at increased risk of unintentional injuries when compared with adults without disabilities (Shi et al. 2015). Children with disabilities are also thought to be at greater risk of unintentional injury (Xiang et al. 2014; Yung et al. 2014). Two prior reviews have included children, but neither has elucidated differences across age groups and disability subtypes nor did these studies include meta-analyses and summary measures of risk (Xiang et al. 2014; Yung et al. 2014). Age, because of its relationship to developmental ability and activity participation, is a very important factor when considering injury risk in children. It is not known if disability subtype plays a role in quantifying injury risk. There are substantial differences in the activities and injury patterns between adults and children, as well as considerable variation in the studies examining injury risk among children with disabilities.
We undertook a systematic review and meta-analysis to better quantify the risk and characteristics of injury among children younger than 18 years of age with disabilities. We synthesize the existing evidence to identify knowledge gaps and research priorities, so future injury prevention efforts can better serve children with disabilities.
Methods
Search strategy
A search strategy was developed for 13 potential databases (Medline; Alt Health Watch, CINAHL, ERIC, PsycINFO, and Sport Discus via EBSCO; Scopus; CAB Abstracts, Global Health via CAB Direct; ISI Web of Knowledge; Cochrane Library; and Health Safety Science abstracts and Clinical Key) using the free text or keyword searches in any fields throughout the full texts. We used search terms from two categories related to disability (e.g., “disabilit*,” “limit*,” “disabl*,” “deficien*,” and “handicap*”); and injury (e.g., “injur*,” “hurt*,” “trauma,” “fall*,” and “wound*”). Additional strategies included hand searches of related journals, internet searches, and screening the reference lists of retrieved studies. Our search included all the related studies between 1 January 1990 and 28 February 2013 with English language abstracts. In this analysis, children were those younger than 18 years.
Definition of disability and injury
Disability was defined in a number of different ways in the included studies: (1) developmental disabilities; (2) emotional/mental/cognitive disabilities; (3) physical/sensory disabilities; (4) chronic disease with mention of functional limitations; (5) WHO International Classification of Functioning Disability and Health (ICF) impairments, limitations, and participation restrictions (Srinivasan et al. 2010; Brophy et al. 2008). A team discussion and decision process was utilized to create three subgroups of disability: physical disability, cognitive disability, and ICF-based definitions of disability.
Injury was defined as any injuries requiring medical attention in the 12 months preceding the interview. Not all studies included information about the types of injury, so we could not consider injury subtypes in our pooled analyses.
Literature selection
Details of our selected steps are shown in Fig. 1. All the retrieved studies were read and screened by two of five reviewers (XS, JS, KW, SL, and HX) in the first round of review. Any disagreements between the initial two reviewers were submitted to whole team for discussion and decision.
Fig. 1.
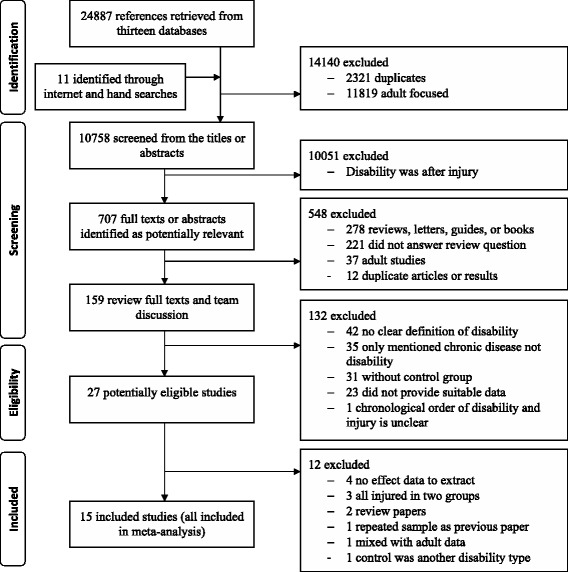
Flowchart of study selection
To be included in our meta-analysis, publications had to meet all the following inclusion criteria: (1) published as an original research article in a peer-reviewed journal with an English abstract; (2) investigated unintentional injuries among individuals with pre-existing disabilities; (3) reported age and a majority of participants were younger than 18 years old; (4) reported odds ratios (OR) or relative risks (RR) and confidence intervals (CI), or provided data so that these could be calculated for the disability variable; and (5) included clear definitions of disability and injury. The majority of the included studies did not specifically mention injury intent. When intentional injuries were mentioned, they were a subset of the total injuries and were excluded from the total injuries.
The following were reasons for exclusion: (1) published as review articles, in books, newspapers, magazines, or other commentaries and lacked original research data; (2) reported only fatal unintentional injuries or focused on intentional injuries (violence, crime, or suicide); (3) lacked a control group; (4) lacked demographic information or sufficient injury risk data; and (5) duplicate publications from the same study sample.
Quality assessment and data extraction
The quality of the included studies was assessed independently by two of the reviewers using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) which has been used by others (Singh et al. 2011). The STROBE checklist contains 22 items which should be covered in epidemiology reports, with an emphasis on research methods (9 items) such as study design, data source, statistical methods, and bias. If an item was appropriately mentioned, a point was assigned (von Elm et al. 2007). After quality assessments, one reviewer (XS) extracted the following data: first author, publication year, study design, age, gender, research region, location at time of injury, the definitions and types of disabilities and injuries, number of disabilities and injuries (OR or RR and their CIs), and injury incidence using a standard data extraction form. A second researcher (JS) then checked data accuracy. When raw data from some studies were not reported, the corresponding authors were contacted to request data. Sufficient data were reported in the included studies for us to calculate the combined ORs by the different age subgroups and by different disability-type subgroups. Some included studies did not provide potential covariate risk factors, such as gender, family economic status, and other health conditions, which are related to disability and injury. These missing details meant that we were not able to estimate the adjusted risks and do a meta-regression analysis.
Data analyses
We first considered the characteristics of the included studies and then conducted heterogeneity tests to determine the appropriate approach for pooling the studies’ results. When heterogeneity (the degree of dissimilarity in the results of selected studies, I2 statistic) was statistically significant, we used random-effects models to compute the pooled ORs as opposed to fixed-effects models. We calculated pooled ORs and 95 % CIs and performed Z tests to evaluate the statistical significance of the pooled effects. We also produced pooled estimates for the different age groups and different types of disabilities (ICF-based disability, physical disability, and cognitive disabilities).
We conducted sensitivity analyses to evaluate the reliability of our results: showing the random-effects model and fixed-effects model results by dropping those studies with the highest and lowest ORs, and by dropping those studies with the largest and smallest sample sizes. Publication bias, i.e., studies with positive results are more likely to be published, was diagnosed by the funnel plot, Egger’s test, and Begg’s tests (Egger et al. 1997; Begg and Mazumdar 1994). We did all analyses using STATA software version 12.0 (StataCorp. TX, USA) with p values ≤0.05 considered significant (two-sided tests).
Results
From 24,898 titles and abstracts, we identified 15 studies (Dunne et al. 1993; Leland et al. 1994; Sherrard et al. 2002; Xiang et al. 2005; Slayter et al. 2006; Chen et al. 2007; Mann et al. 2007; Lee et al. 2008; Sinclair and Xiang 2008; Raman et al. 2009; Ramirez et al. 2010; Brenner et al. 2013; Tsang et al. 2012; Zhu et al. 2012; Othman and Kendrick 2013) eligible for inclusion (Fig. 1). Ten studies used a cross-sectional design (Brenner et al. 2013; Chen et al. 2007; Lee et al. 2008; Mann et al. 2007; Raman et al. 2009; Sinclair and Xiang 2008; Slayter et al. 2006; Tsang et al. 2012; Xiang et al. 2005; Zhu et al. 2012), two studies used a case–control design (Dunne et al. 1993; Othman and Kendrick 2013), and three studies were cohort studies (Leland et al. 1994; Ramirez et al. 2010; Sherrard et al. 2002). Sample sizes ranged from 186 to 8,456,144 with a total sample size of 9,581,553, including 83,286 children with disabilities (not including three studies (Brenner et al. 2013; Sherrard et al. 2002; Ramirez et al. 2010) in which the authors did not provide the exact number of individuals with disability). Across the 15 studies, 2,032,685 children were injured (including 22,306 injured children with disabilities).
All studies had mixed gender samples. A gender difference in injury risk existed and the pooled injury risk for males with disability was a little higher than that for females with disability (OR = 1.20, 95 % CI 1.06–1.36). Most studies used a broad age range, generally from 0 to 18 years, however three studies focused on young children (Leland et al. 1994; Lee et al. 2008; Othman and Kendrick 2013) and five studies focused on school-age children (Sherrard et al. 2002; Raman et al. 2009; Xiang et al. 2005; Ramirez et al. 2010; Tsang et al. 2012) (Table 1). We also included two studies (Slayter et al. 2006; Ramirez et al. 2010) which had small percentages of young adults ages 19 and 20, because these young adults could not be separated in the analysis from those under 18 years. Geographically, the WHO region of the Americas was heavily represented, with ten studies in USA and one in Canada (Raman et al. 2009), and the remaining four studies were from the WHO Asia and Western Pacific region (China, Hong Kong, Iraq, and Australia) (Othman and Kendrick 2013; Sherrard et al. 2002; Tsang et al. 2012; Zhu et al. 2012). No eligible studies were found in the WHO Europe and Africa regions.
Table 1.
Characteristics of included papers
| First author/year | Design | Data source | Age | Definition and type of disability | Pre-existing disability determination | Definition and type of injury | % injured with disabilities/without disabilitiesa | Quality assessmentb |
|---|---|---|---|---|---|---|---|---|
| Dunne RG, 1993 | CC | National Health Interview Survey, 1988 | 0–17 years | Developmental disability, mainly cognitive disability | Developmental delays not likely the result of injury | Injury requiring medical attention in past 12 months reported by care giver | 28.7/26.2 % | 17–19 |
| Leland NL, 1994 | CO | Preschool children in two day care programs | 30–72 months | Medical diagnosis of physical or cognitive disability; 63 % with cognitive disability | Enrolled in one of two day care programs based on disability | Day care injury logs as required by state law | 4.8/2.5 % | 20–21 |
| Sherrard J, 2002 | CO | Australian Child and Adolescent Development program, 1990–1991 and 1995–1996 | 4–18 years | Cognitive disability, intelligence quotient <70 | Biopsychosocial data collected in 1990–1991, injury assessed in 1995–1996 | Medically attended injuries in past 12 months reported by care giver | — | 19–20 |
| Xiang H, 2005 | CS | National Health Interview Survey, 2000–2002 | 5–17 years | ICF—limitations in social activities because of chronic physical or mental conditions | Disabling condition for at least 1 year before the interview | Medically attended injuries in past 3 months | 4.1/2.5 % | 21–21 |
| Slayter EM, 2006 | CS | Medicaid-eligible children in 26 states, 1999 eligibility and claims data | 1–20 years | Cognitive disability, ICD-9-CM codes 317–319 | Cognitive disability codes unrelated to injury | ICD-9-CM injury codes in Medicaid claims data | 36.9/23.5 % | 20–22 |
| Chen G, 2007 | CS | Ohio Medicaid claims data 2002 | 0–12 years | ICF—limitations in social activities because of chronic physical or mental conditions | Medicaid designated disability, limitations as the result of a chronic condition | ICD-9-CM codes for burns 940–949 | 1.03/0.77 % | 20–22 |
| Mann JR, 2007 | CS | South Carolina Medicaid claims data, 2002–2003 | 1–18 years | Hearing loss, ICD-9-CM codes 389.0–389.9 | Hearing loss diagnosis in both 2002 and 2003, injury in 2003 | ICD-9-CM codes for injuries, Barell Matrix categories | 17.7/8.6 % | 21–21 |
| Lee LC, 2008 | CS | National Survey of Children’s Health, 2003–2004 | 3–5 years | Learning disability | Disabilities unrelated to injury | Medically attended injuries in the past year | 16.6/12.2 % | 20–22 |
| Sinclair SA, 2008 | CS | National Health Interview Survey, 1997–2005 | 0–17 years | ICF—limitations in activities, excluding those with multiple disabilities | Excluded children who had an injury less than 1 year before the interview that resulted in a disability | Medically attended injuries in past 3 months | 3.8/2.5 % | 21–21 |
| Raman SR, 2009 | CS | Health behavior in school-age children survey, Canada 2002 | Grades 6–10 | ICF—long-term disability with participation and activity limitations | Disability is reported to be long term, past year injuries with reported consequences | Student self-report of medically attended injuries in the past 12 months | 67.4/51.4 % | 20–20 |
| Ramirez M, 2010 | CO | 35 schools in urban district of Los Angeles, 1994–1998, n = 147,460 | 5–19 years | Qualified for special education services by California Department of Education | Students enrolled for services, subsequent school injuries | Injuries during school activities | 3.8/1.5 % | 19–21 |
| Brenner RA, 2013 | CS | National Electronic Injury Surveillance System, 2006–2007 | 0–17 years | Autism, blindness, cerebral palsy, deafness or trouble hearing, intellectual disability, ADD, ADHD, learning disability | Caregivers surveyed, disabilities unrelated to injury | All non-work unintentional injuries | 10.4/10.5 % | 19–20 |
| Tsang SL, 2012 | CS | Students in 2 mainstream and 3 special schools | 6–12 years | Cognitive disability, intelligence quotient <70 | Caregivers surveyed, disability unrelated to injury | Unintentional household injuries; home | 61.6/32.0 % | 19–19 |
| Zhu HP, 2012 | CS | Registry database of China Disabled Persons’ Federation | 1–14 years | ICF | Causes of limitations were known | All medical attention injuries in the past year; home, school, other locations | 10.2/4.4 % | 20–20 |
| Othman N, 2013 | CC | Burn center and admitted patients in a children’s hospital in Iraq | 0–5 years | Visual or hearing impairment, epileptic seizures, learning disabilities, walking problems | Reason for admission is known, excluded those with previous burn injury | Burns; home | — | 17–18 |
CC case–control study, CO cohort study, CS cross-sectional study, ICF International Classification of Functioning, Disability and Health, ICD-9-CM International Classification of Disease, Ninth Revision, Clinical Modification, ADD attention deficit disorder, ADHD attention deficit hyperactivity disorder
aSome references did not provide the proportion injured or lacked data to calculate percentages
bNumber of items among the 22 items in STROBE checklists judged by two reviewers
Not all of the 15 studies included comparisons regarding the location, activity, or cause of injury. Older studies were less likely to include this information, two papers reported injuries that occurred only at home (Othman and Kendrick 2013; Tsang et al. 2012), two reported only daycare and school injuries (Leland et al. 1994; Ramirez et al. 2010), four included a mix of injury locations (Brenner et al. 2013; Raman et al. 2009; Sinclair and Xiang 2008; Zhu et al. 2012), and seven papers did not clearly mention the location at time of injury (Dunne et al. 1993; Sherrard et al. 2002; Xiang et al. 2005; Slayter et al. 2006; Chen et al. 2007; Mann et al. 2007; Lee et al. 2008). When reported, home was the most common injury location followed by school. Two studies reported similarities in the injury patterns in children with and without disabilities (Brenner et al. 2013; Sinclair and Xiang 2008). Two studies reported higher proportions of burn injury (Sinclair and Xiang 2008), and two studies were focused on burn injuries only (Chen et al. 2007; Othman and Kendrick 2013). Others reported fewer sports-related injuries among children with disabilities compared to those without disabilities (Raman et al. 2009; Zhu et al. 2012; Sinclair and Xiang 2008). Intentional injuries were specifically excluded in three studies (Brenner et al. 2013; Tsang et al. 2012; Zhu et al. 2012), and intent was not mentioned in six of the studies (Chen et al. 2007; Dunne et al. 1993; Leland et al. 1994; Othman and Kendrick 2013; Sinclair and Xiang 2008; Xiang et al. 2005). For those reporting on school injuries (Raman et al. 2009; Ramirez et al. 2010), nearly one third of the injuries were the result of assaults/fights, and one of these studies reported a higher rate of assault/fight-related school injury among children with disabilities (Raman et al. 2009). One of the included studies references a companion paper which describes injury intent; intentional injuries were 15 % of the total injuries, and the rate of intentional injury was higher among those with disabilities (Sherrard et al. 2001). The intentional injuries in these papers were excluded from our pooled estimates.
Thirteen studies reported injury rates in children with disabilities (some papers did not report the exact rates but provided the data so that the rates could be calculated). Injury rates for the children with disabilities ranged from 1.0 to 67.4 % (median 10.4 %), and in the control group ranged from 0.8 to 51.4 % (median 8.6 %). We found large variation and heterogeneity in both groups, so we did not calculate pooled injury percentages. Instead, we calculated pooled ORs of injury to estimate risk.
The characteristics of included studies are listed in Table 1. The quality of studies was assessed using the STROBE checklist, and all the included studies met at least 17 items and most had 19–21 items in the checklist. Items most frequently missing were determination of bias, selection of participants, explanation of the quantitative variables, and how the study sample size was determined.
In our meta-analysis, we used random-effects models to estimate the pooled ORs because all of the p values of Q tests were <0.001 and the I2 results were all greater than 70 %, indicating that heterogeneity should be considered statistically significant. Of the 15 included papers, the I2 was 89.8 %, the combined OR was 1.86 (95 % CI 1.65–2.10), and the Z value was 10.07, p < 0.001 when testing whether the pooled effect was equal to 1 (Table 2 and Fig. 2).
Table 2.
Results of the sensitivity analyses
| Analyzed databases | Detailed databasesa | Included studies | OR and CI | Overall Z test and p value | I 2 and CI (%) |
|---|---|---|---|---|---|
| Overall | All eligible papers | 15 | 1.86(1.65–2.10) | Z = 10.07, p < 0.001 | 89.8(84.8–93.1) |
| All eligible papers (fixed-effects model) | 15 | 1.90(1.87–1.94) | Z = 73.67, p < 0.001 | 89.8(84.8–93.1) | |
| Studies with the most variation in effect were dropped | Excluded max-effect paper | 14 | 1.81(1.61–2.03) | Z = 9.87, p < 0.001 | 89.6(84.3–93.1) |
| Excluded min-effect paper | 14 | 1.92(1.71–2.17) | Z = 10.70, p < 0.001 | 89.5(84.1–93.0) | |
| Excluded max- and min-effect papers | 13 | 1.87(1.67–2.10) | Z = 10.55, p < 0.001 | 89.2(83.4–93.0) | |
| Studies with the most variation in sample size were dropped | Excluded max-sample size paper | 14 | 1.91(1.60–2.28) | Z = 7.22, p < 0.001 | 90.5(85.8–93.6) |
| Excluded min-sample size paper | 14 | 1.82(1.61–2.05) | Z = 9.70, p < 0.001 | 90.1(85.2–93.4) | |
| Excluded max- and min-sample size papers | 13 | 1.85(1.55–2.20) | Z = 6.76, p < 0.001 | 90.9(86.2–93.9) |
OR odds ratio, CI confidence interval, max maximum, min minimum
aRandom-effects models were used to combine the effects unless otherwise specified
Fig. 2.
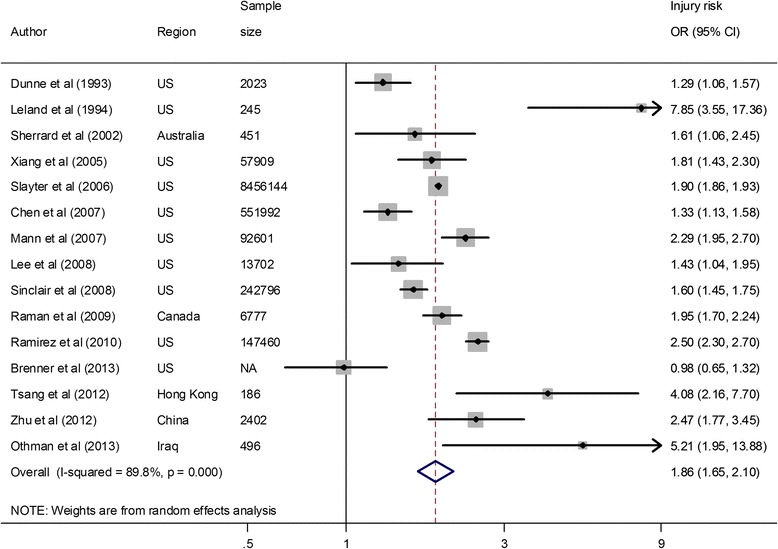
Overall analysis of injury risk against children with disabilities. NA not available, OR odds ratio, CI confidence interval. The ORs and CIs were computed using original numbers of disabilities and injuries. If the original data could not be extracted, we used the crude ORs and CIs rather than adjusted ORs and CIs
Results of the subgroup analyses by age group are shown in Fig. 3. For the four age subgroup analyses, all pooled results are from random-effects models. The overall I2 was 95.9 % (95 % CI 94.8–96.7 %) and the OR was 1.88 (95 % CI 1.65–2.13) which was statistically significant, Z = 9.67, p < 0.001. The I2, the measure of heterogeneity, ranged from 84.0 to 97.5 %. The OR of injuries increased with increasing age. For the 0–4-year-old group, the pooled OR was not significant [1.28 (95 % CI 0.59–2.79), Z = 0.63, p = 0.531]. For the 5–9-year-old group, the pooled OR reached statistical significance [1.75 (95 % CI 1.03–2.99), Z = 2.07, p = 0.039]. For the ≥10-year-old subgroup, the pooled OR was significant [1.86 (95 % CI 1.29–2.67), Z = 3.35, p = 0.001]; similarly, in the mixed-age subgroup (0–18 years old), the combined OR was significant [2.20 (95 % CI 1.75–2.77), Z = 6.68, p < 0.001]. The mixed-age group included data from studies where there were not enough data to separate the subjects into one of the three age subgroups.
Fig. 3.
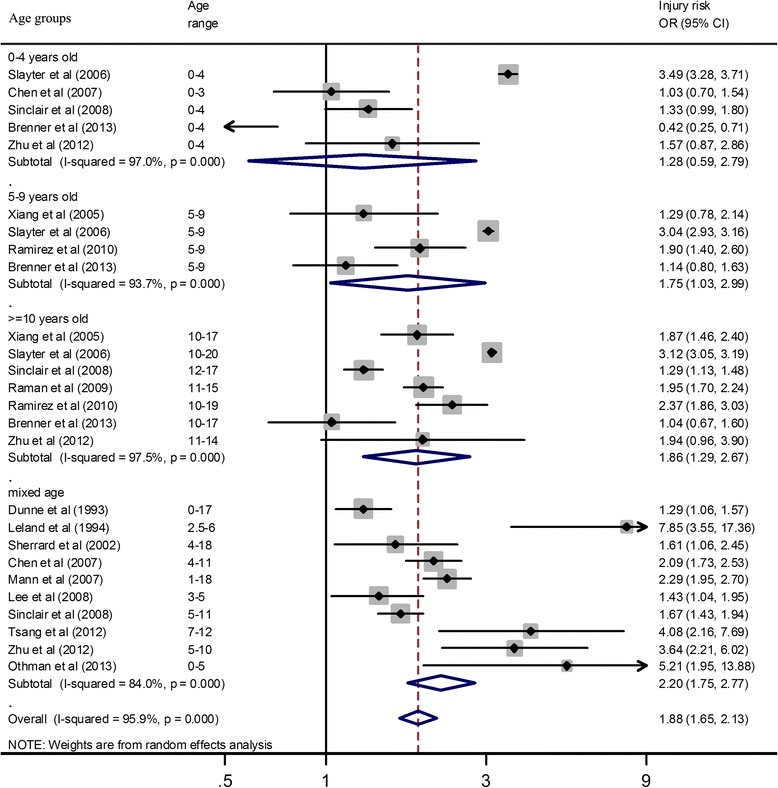
Injury risk estimates in children with disabilities according to age group. OR odds ratio, CI confidence interval. The ORs and CIs were computed using original numbers of disabilities and injuries. If the original data could not be extracted, we used the crude ORs and CIs rather than adjusted ORs and CIs
Subgroup pooled results for different types of disabilities are shown in Fig. 4. For the five studies that used ICF limitation questions, the I2 was 87.0 % (95 % CI 72.0–94.0 %) and the pooled OR was 1.75 (95 % CI 1.26–2.43) [Z = 3.34, p = 0.001]. For the four studies reporting physical disabilities, the I2 was 94.3 % (95 % CI 88.4–97.2 %) and the combined OR was 2.39 (95 % CI 1.43–4.00) [Z = 3.33, p = 0.001]. For the nine studies reporting cognitive disabilities, the I2 was 89.1 % (95 % CI 81.5–93.6 %) and the combined OR was 1.77 (95 % CI 1.49–2.11); Z = 6.40; p < 0.001. Three studies reported both physical disabilities and cognitive disabilities, and those data were included in a separate subgroup analysis (Xiang et al. 2005; Sinclair and Xiang 2008; Ramirez et al. 2010). The overall I2 was 92.8 % (95 % CI 90.1–94.8 %) and the OR was 1.92 (95 % CI 1.65–2.24) [Z = 8.45, p < 0.001]. (Note: The small difference in the overall effects shown in Figs. 3 and 4 was due to different ways the data were grouped. Not all studies were included in both the age and disability subgroup analyses).
Fig. 4.
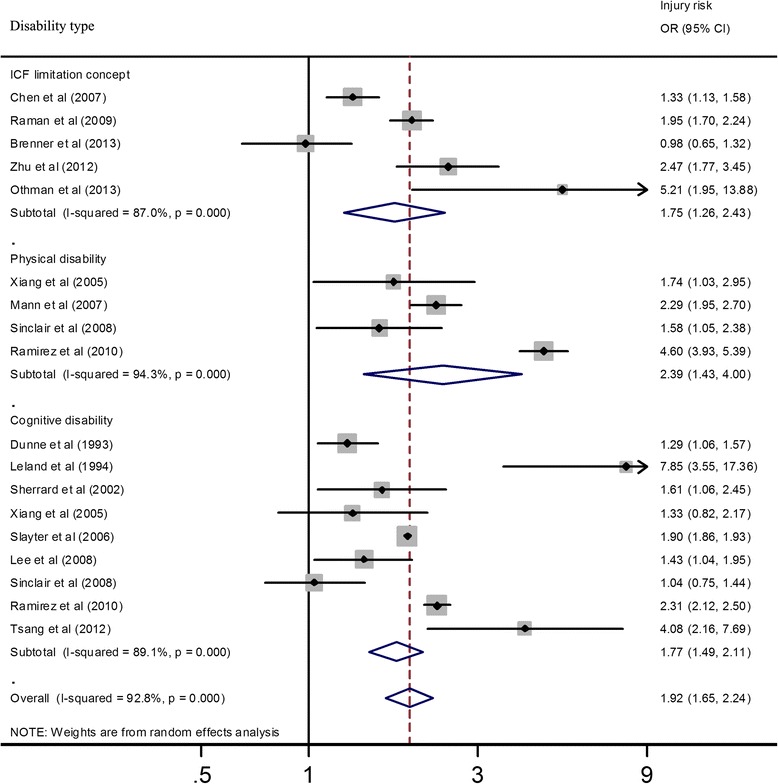
Injury risk in children with disabilities according to disability type. OR odds ratio, CI confidence interval. The ORs and CIs were computed using original numbers of disabilities and injuries. If the original data could not be extracted, we used the crude ORs and CIs rather than adjusted ORs and CIs
To assess the reliability of our results, we conducted sensitivity analyses (Table 2), comparing the pooled estimates produced using two types of models (a random-effects model versus a fixed-effects model). We also calculated the pooled estimates after we excluded those studies with the most variation in effect or sample size. We found that the overall ORs changed little, so our meta-analysis results appeared reliable. We also tested for publication bias among our sample of studies using two approaches. The first approach was the funnel plot; asymmetry in the funnel plot indicates bias (Harbord et al. 2006). We found that there was good symmetry, though some points were out of the area of the CI (figure not shown). The second approach included the Egger’s and Begg’s tests, which conclude that bias exists if the intercept for the regression is different from zero at the 0.05 level (Begg and Mazumdar 1994; Harbord et al. 2006). The result of Begg’s test was Z = 0.89, p = 0.373 in all included studies; while the result of Egger’s test was t = 0.01, p = 0.990. Both plots and tests indicated that publication bias in our meta-analysis was not a substantial issue.
Discussion
Findings from our meta-analysis of 15 studies indicate that children with disabilities are at increased risk of unintentional injuries. The pooled OR of unintentional injuries was higher in individuals with physical disabilities (OR = 2.39) compared with those with cognitive disabilities (OR = 1.77). We also found increased odds of injury with increasing age. Results of this meta-analysis, along with the meta-analysis of violence against children with disabilities, provide evidence that injury prevention among children with disabilities, both unintentional and intentional injury, merits attention in the injury prevention field (Jones et al. 2012). Recent research has documented that in the USA alone, the percentage of children with disabilities rose 16 % between 2001 and 2011 (Houtrow et al. 2014).
Age is well known as an important modifier in injury-related research. Children are not just small adults; their physical and cognitive abilities, degrees of dependence, need for supervision, activities and risk behaviors all change rapidly with their growth. As children develop, their curiosity and wish to explore the world increase significantly while they only have limited capacities to understand or respond to danger (Bartlett 2002). Children’s development and behaviors are therefore highly associated with injury risk. Injury characteristics differ at different ages. Poisoning, for example, is linked to the grasping and mouth-exploratory behaviors of children ages 1–3 years; falls are particularly related to the stage of learning to walk, while burns from hot liquids have previously been found to be higher among children ages 12–18 months (Agran et al. 2003). Our study supports this association between age and injury risk in children with disabilities. We found that the pooled ORs of injury were 1.28, 1.75, and 1.86 in 0–4, 5–9, and ≥10-year-old age subgroups, respectively. Some researchers have reported that among children with disabilities, occurrence of injuries decreased with increasing age (Limbos et al. 2004; Ramirez et al. 2004), but these studies were focused on injuries in the school environment. However, our results are consistent with the study of Petridou and colleagues, who found that the injury OR for children with disabilities increased with increasing age (Petridou et al. 2003). A similar result was also reported in Chen and colleagues’ study of burns risk in children with disabilities younger than 12 years old (Chen et al. 2007).
Similar to our finding in adults with disabilities, children with physical disabilities had the greatest odds of injury (OR = 2.39). Children with ICF limitations and cognitive disabilities had similar ORs (1.75 and 1.77, respectively). Our meta-analysis among adults with disabilities produced inconclusive evidence about injury risk in adults with cognitive limitations (Shi et al. 2015). Ramirez and colleagues’ cohort study of 269,000 school children reported that children with physical disabilities (orthopedic and sensory) were more likely to suffer injuries than those with cognitive disabilities (Ramirez et al. 2010).
In addition to injury risk differences across age groups and disability types, our meta-analysis showed that gender was also a significant modifier. The pooled OR of injury in boys with disabilities was 1.21 times greater than that in girls with disabilities. Reasons for this gender difference may include the fact that boys usually have higher activity levels, more risk behaviors, and are less restrained by parents (WHO, UNICEF 2008).
Our meta-analysis has several limitations. First, other socioeconomic status factors, such as family income and race, also potentially affect the injury risk in children with disabilities; however, we could not examine the pooled effects because only a limited number of original studies included those injury risk factors. A second limitation is the substantial methodological and statistical heterogeneity seen in the selected studies. Much of the methodological heterogeneity was due to the varied definitions of disability among these studies. In the pooled analysis, we estimated injury risk by physical disability, cognitive disability, and ICF disability subgroups. Even within these subgroups, disability definitions varied among different studies. Physical disability included sensory impairments, limb disabilities, and work limitations, while cognitive disability included intellectual disabilities, mental health disabilities, and learning disabilities. Future research in this area should use a consistent definition of disability so results from multiple studies can more readily be compared and pooled. More recent studies have used the ICF disability definition, which includes not only impairments but also activity limitations and participation restrictions (Wasiak et al. 2011). Although ICF concepts and disability definition are still evolving; they can provide a standardized terminology for epidemiological studies to achieve comparability of data. Some other sources of heterogeneity in our meta-analysis were significant variations in sample sizes, research study periods, and the age range of enrolled children. A third limitation is that the included studies came mostly from high-income countries and regions (USA, Canada, Australia, and Hong Kong), while low-income and middle-income countries have 80 % of the world’s disabled population, generally higher rates of injury, and fewer health services than developed countries (WHO et al. 2011). Research about injuries in children with disabilities in low- and middle-income countries is scarce. Although a few included studies were from middle-income countries (China and Iraq), the potential value of additional rigorous data on injury risk in children with disabilities from developing countries should not be ignored. A fourth limitation is related to grey literature (unpublished academic studies such as theses and dissertations). While we attempted to include such studies through internet searches, no such studies were found. Finally, it is not clear from the included studies if there are strong differences between children with disabilities and children without disabilities in the patterns of injury (location, activity, and mechanism of injury). Occupational injuries were considered in our adult study, but we did not find any studies which considered work-related injuries among adolescents.
Despite the heterogeneity of the included studies, several of our implemented research steps should have strengthened the reliability of our results. First, we had strict inclusion and exclusion criteria. Second, our literature selection procedures followed the recommended standard steps of systematic review and meta-analysis (Manchikanti et al. 2009; Moher et al. 2009). We reached selection decisions through two independent rounds of review and one round of team discussion when needed. Third, the two reviewers’ appraisals of original studies were based on the STROBE checklist, which showed that the quality of included studies was moderate to high (17–22 items were mentioned from a total 22 items).
By estimating the pooled injury risk of injuries in children with disabilities, this study highlights the need for interventions. A number of recent systematic reviews (Kendrick et al. 2013a; Kendrick et al. 2013b; Pearson et al. 2012) and reports (WHO, UNICEF 2008; UNICEF 2009) have described child injury prevention strategies. The 2008 World Report on Child Injury Prevention has chapters based on different external causes of injury and possible interventions for use in both high and low resource settings (WHO, UNICEF 2008). Similarly, Kendrick et al. reported on effective parenting interventions (Kendrick et al. 2013a) and home safety interventions (Kendrick et al. 2013b) in two recent systematic reviews. A 2012 systematic review of educational programs aimed at preventing unintentional injury during outdoor play reported mixed results (Pearson et al. 2012). While children with higher risks of injury were considered in these systematic reviews of interventions, children with disabilities were not one of the higher risk groups considered. Sherrard et al. reported on a small number of studies which evaluated injury prevention among both adults and children with cognitive disabilities (Sherrard et al. 2004). Despite the recognition in the disability community of the need for interventional studies (WHO et al. 2011; Xiang et al. 2014; Yung et al. 2014), by and large, rigorous evaluation studies of injury prevention interventions in children with disabilities could not be found in the literature. Some researchers have recommended using national injury surveillance systems to identify those risk factors which might be specific to children with disabilities (Gaebler-Spira and Thornton 2002).
Currently, it is not clear if different prevention strategies are needed for children with disabilities. Specific interventions for children with disabilities might potentially include actions to provide assistive devices and modify inaccessible or hazardous environments (passive interventions). In the former category would be appropriate wheelchairs and other mobility devices, as well as tools to enhance ability to reach. In the latter category would be provision of curb cuts and safe road crossings and barrier removal in the home. UNICEF’s 2013 State of the World’s Children report focused on enhancing societal participation of children with disabilities and calls for universal design in “all children’s environments—early childhood centers, schools, health facilities, public transport, playgrounds, and so on” (UNICEF 2013). Environmental factors, including stairs, curbs, and rough terrain, were identified as injury trigger factors in a study of pediatric mobility aid-related injuries (Barnard et al. 2010). Reducing the use of institutionalization, increasing support for families and involving children with disabilities indecision making are also addressed in the UNICEF report (UNICEF 2013). Future studies considering intervention effectiveness should include children with disabilities. As well, future research should be geared toward enhancing social participation and improving the safety of children’s environments, as opposed to restricting activities. The goal is to improve the quality of life for children with disabilities, and at stake is the principal of equity (UNICEF 2013).
Conclusions
Our systematic review and meta-analysis showed that children with disabilities had a greater risk of unintentional injuries, especially children with physical disabilities. Teens were at a greater risk than younger children with disabilities. Future research on injuries in children with disabilities should focus on passive interventions (Simpson and Nicholls 2012) to prevent both intentional and unintentional injuries. More high-quality intervention and evaluation research is needed so that parents, teachers, healthcare, and other social service providers can choose evidence-based interventions to reduce injury risk in children with disabilities.
Acknowledgements
This study was funded by the National Institute of Occupational Safety and Health, Centers for Disease Control and Prevention, USA (H. Xiang, grant 1R01OH009585-01A1). The findings and conclusions are those of the authors and do not necessarily reflect those of the NIOSH or CDC; Dr. Shi’s effort in this study is partially funded by the Natural Science Foundation of China (X. Shi, grant 81160350 and 81560534).
We thank Sarah Johnson for providing writing assistance.
Abbreviations
- ICF
International Classification of Functioning
- STROBE
Strengthening the Reporting of Observational Studies in Epidemiology
- WHO
World Health Organization
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
HX and XS designed the study; and XS, JS, KW, and HX oversaw its implementation, coordinated the review activities including searches, study selection, data extraction, and quality assessment. XS, JS, KW, and HX assisted with the initial inclusion and exclusion of abstracts. XS planned and did the meta-analyses and subgroup analysis. XS wrote the first draft and KW, JS, GS, HX, LS, TS, and SA revised the report. All authors reviewed the study findings. All authors read and approved the final manuscript.
Contributor Information
Xiuquan Shi, Email: xqshi2008@126.com.
Junxin Shi, Email: Junxin.shi@nationwidechildrens.org.
Krista K. Wheeler, Email: Krista.wheeler@nationwidechildrens.org
Lorann Stallones, Email: Lorann.Stallones@ColoState.EDU.
Shanthi Ameratunga, Email: s.ameratunga@auckland.ac.nz.
Tom Shakespeare, Email: Tom.Shakespeare@uea.ac.uk.
Gary A. Smith, Email: Gary.Smith@nationwidechildrens.org
Huiyun Xiang, Phone: (614) 355-5850, Email: Huiyun.Xiang@nationwidechildrens.org.
References
- Agran PF, Anderson C, Winn D, Trent R, Walton-Haynes L, Thayer S. Rates of pediatric injuries by 3-month intervals for children 0 to 3 years of age. Pediatrics. 2003;111(6 Pt 1):e683–92. doi: 10.1542/peds.111.6.e683. [DOI] [PubMed] [Google Scholar]
- Barnard AM, Nelson NG, Xiang H, McKenzie LB. Pediatric mobility aid-related injuries treated in US emergency departments from 1991 to 2008. Pediatrics. 2010;125(6):1200–7. doi: 10.1542/peds.2009-3286. [DOI] [PubMed] [Google Scholar]
- Bartlett SN. The problem of children’s injuries in low-income countries: a review. Health Policy Plan. 2002;17(1):1–13. doi: 10.1093/heapol/17.1.1. [DOI] [PubMed] [Google Scholar]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- Brenner RA, Taneja GS, Schroeder TJ, Trumble AC, Moyer PM, Louis GM. Unintentional injuries among youth with developmental disabilities in the United States, 2006–2007. Int J Inj Contr Saf Promot. 2013;20(3):259–65. doi: 10.1080/17457300.2012.696662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brophy M, Zhang X, Xiang H. Injuries among US adults with disabilities. Epidemiology. 2008;19(3):465–71. doi: 10.1097/EDE.0b013e31816932ba. [DOI] [PubMed] [Google Scholar]
- Chen G, Smith GA, Ranbom L, Sinclair SA, Xiang H. Incidence and pattern of burn injuries among children with disabilities. J Ttrauma. 2007;62(3):682–6. doi: 10.1097/01.ta.0000203760.47151.28. [DOI] [PubMed] [Google Scholar]
- Dunne RG, Asher KN, Rivara FP. Injuries in young people with developmental disabilities: comparative investigation from the 1988 National Health Interview Survey. Ment Retard. 1993;31(2):83–8. [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaebler-Spira D, Thornton LS. Injury prevention for children with disabilities. Phys Med Rehabil Clin N Am. 2002;13(4):891–906. doi: 10.1016/S1047-9651(02)00023-2. [DOI] [PubMed] [Google Scholar]
- Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med. 2006;25(20):3443–57. doi: 10.1002/sim.2380. [DOI] [PubMed] [Google Scholar]
- Houtrow AJ, Larson K, Olson LM, Newacheck PW, Halfon N. Changing trends of childhood disability, 2001–2011. Pediatrics. 2014;134(3):530–8. doi: 10.1542/peds.2014-0594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes K, Bellis MA, Jones L, Wood S, Bates G, Eckley L, et al. Prevalence and risk of violence against adults with disabilities: a systematic review and meta-analysis of observational studies. Lancet. 2012;379(9826):1621–9. doi: 10.1016/S0140-6736(11)61851-5. [DOI] [PubMed] [Google Scholar]
- Jones L, Bellis MA, Wood S, Hughes K, McCoy E, Eckley L, et al. Prevalence and risk of violence against children with disabilities: a systematic review and meta-analysis of observational studies. Lancet. 2012;380(9845):899–907. doi: 10.1016/S0140-6736(12)60692-8. [DOI] [PubMed] [Google Scholar]
- Kendrick D, Mulvaney CA, Ye L, Stevens T, Mytton JA, Stewart-Brown S. Parenting interventions for the prevention of unintentional injuries in childhood. Cochrane Database Syst Rev. 2013;3 doi: 10.1002/14651858.CD006020.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, et al. Home safety education and provision of safety equipment for injury prevention (Review) Evid Based Child Health. 2013;8(3):761–939. doi: 10.1002/ebch.1911. [DOI] [PubMed] [Google Scholar]
- Lee LC, Harrington RA, Chang JJ, Connors SL. Increased risk of injury in children with developmental disabilities. Res Dev Disabil. 2008;29(3):247–55. doi: 10.1016/j.ridd.2007.05.002. [DOI] [PubMed] [Google Scholar]
- Leland NL, Garrard J, Smith DK. Comparison of injuries to children with and without disabilities in a day-care center. J Dev Behav Pediatr. 1994;15(6):402–8. doi: 10.1097/00004703-199412000-00002. [DOI] [PubMed] [Google Scholar]
- Limbos MA, Ramirez M, Park LS, Peek-Asa C, Kraus JF. Injuries to the head among children enrolled in special education. Arch Pediatr Adolesc Med. 2004;158(11):1057–61. doi: 10.1001/archpedi.158.11.1057. [DOI] [PubMed] [Google Scholar]
- Manchikanti L, Datta S, Smith HS, Hirsch JA. Evidence-based medicine, systematic reviews, and guidelines in interventional pain management: part 6. Systematic reviews and meta-analyses of observational studies. Pain physician. 2009;12(5):819–50. [PubMed] [Google Scholar]
- Mann JR, Zhou L, McKee M, McDermott S. Children with hearing loss and increased risk of injury. Ann Fam Med. 2007;5(6):528–33. doi: 10.1370/afm.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulik PK, Darmstadt GL. Childhood disability in low- and middle-income countries: overview of screening, prevention, services, legislation, and epidemiology. Pediatrics. 2007;120(Suppl 1):S1–55. doi: 10.1542/peds.2007-0043B. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Othman N, Kendrick D. Risk factors for burns at home in Kurdish preschool children: a case–control study. Inj Prev. 2013;19(3):184–90. doi: 10.1136/injuryprev-2012-040412. [DOI] [PubMed] [Google Scholar]
- Pearson M, Hunt H, Garside R, Moxham T, Peters J, Anderson R. Preventing unintentional injuries to children under 15 years in the outdoors: a systematic review of the effectiveness of educational programs. Inj Prev. 2012;18(2):113–23. doi: 10.1136/injuryprev-2011-040043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petridou E, Kedikoglou S, Andrie E, Farmakakis T, Tsiga A, Angelopoulos M, et al. Injuries among disabled children: a study from Greece. Inj Prev. 2003;9(3):226–30. doi: 10.1136/ip.9.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raman SR, Boyce WF, Pickett W. Associations between adolescent risk behaviors and injury: the modifying role of disability. J Sch Health. 2009;79(1):8–16. doi: 10.1111/j.1746-1561.2008.00368.x. [DOI] [PubMed] [Google Scholar]
- Ramirez M, Peek-Asa C, Kraus JF. Disability and risk of school related injury. Inj Prev. 2004;10(1):21–6. doi: 10.1136/ip.2003.002865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez M, Fillmore E, Chen A, Peek-Asa C. A comparison of school injuries between children with and without disabilities. Acad Pediatr. 2010;10(5):317–22. doi: 10.1016/j.acap.2010.06.003. [DOI] [PubMed] [Google Scholar]
- Sherrard J, Tonge BJ, Ozanne-Smith J. Injury in young people with intellectual disability: descriptive epidemiology. Inj Prev. 2001;7(1):56–61. doi: 10.1136/ip.7.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherrard J, Tonge BJ, Ozanne-Smith J. Injury risk in young people with intellectual disability. J Intellect Disabil Res. 2002;46(Pt 1):6–16. doi: 10.1046/j.1365-2788.2002.00346.x. [DOI] [PubMed] [Google Scholar]
- Sherrard J, Ozanne-Smith J, Staines C. Prevention of unintentional injury to people with intellectual disability: a review of the evidence. J Intellect Disabil Res. 2004;48(Pt 7):639–45. doi: 10.1111/j.1365-2788.2003.00570.x. [DOI] [PubMed] [Google Scholar]
- Shi X, Wheeler KK, Shi J, Stallones L, Ameratunga S, Shakespeare T, et al. Increased risk of unintentional injuries in adults with disabilities: a systematic review and meta-analysis. Disabil Health J. 2015;8(2):153–64. doi: 10.1016/j.dhjo.2014.09.012. [DOI] [PubMed] [Google Scholar]
- Simpson JC, Nicholls J. Preventing unintentional childhood injury at home: injury circumstances and interventions. Int J Inj Contr Saf Promot. 2012;19(2):141–51. doi: 10.1080/17457300.2011.635208. [DOI] [PubMed] [Google Scholar]
- Sinclair SA, Xiang H. Injuries among US children with different types of disabilities. Am J Public Health. 2008;98(8):1510–6. doi: 10.2105/AJPH.2006.097097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh M, Holmes DR, Dehmer GJ, Lennon RJ, Wharton TP, Kutcher MA, et al. Percutaneous coronary intervention at centers with and without on-site surgery a meta-analysis. JAMA. 2011;306(22):2487–94. doi: 10.1001/jama.2011.1790. [DOI] [PubMed] [Google Scholar]
- Slayter EM, Garnick DW, Kubisiak JM, Bishop CE, Gilden DM, Hakim RB. Injury prevalence among children and adolescents with mental retardation. Ment Retard. 2006;44(3):212–23. doi: 10.1352/0047-6765(2006)44[212:IPACAA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Srinivasan K, Vaz M, Thomas T. Prevalence of health related disability among community dwelling urban elderly from middle socioeconomic strata in Bangaluru. India. Indian J Med Res. 2010;131:515–21. [PubMed] [Google Scholar]
- Tsang SL, Gao Y, Chan EY. A pilot study on unintentional household injury among children with intellectual disability in Hong Kong. Injury Medicine. 2012;1(1):25–32. [Google Scholar]
- United Nations Children’s Fund (UNICEF). Progress for children: a report card on child protection. 2009. http://www.unicef.org/publications/files/Progress_for_Children-No.8_EN_081309.pdf. Accessed 20 Aug 2013.
- United Nations Children’s Fund (UNICEF). The state of the world’s children: children with disabilities. 2013. http://www.refworld.org/docid/51cbe6074.html. Accessed 8 September 2014.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- Wang SY, Li YH, Chi GB, Xiao SY, Ozanne-Smith J, Stevenson M, et al. Injury-related fatalities in China: an under-recognised public-health problem. Lancet. 2008;372(9651):1765–73. doi: 10.1016/S0140-6736(08)61367-7. [DOI] [PubMed] [Google Scholar]
- Wasiak J, McMahon M, Danilla S, Spinks A, Cleland H, Gabbe B. Measuring common outcome measures and their concepts using the International Classification of Functioning, Disability and Health (ICF) in adults with burn injury: a systematic review. Burns. 2011;37(6):913–24. doi: 10.1016/j.burns.2011.02.012. [DOI] [PubMed] [Google Scholar]
- World Health Organization, UNICEF. World report on child injury prevention. WHO Press. 2008:http://whqlibdoc.who.int/publications/2008/9789241563574_eng.pdf. Accessed 20 Aug 2013.
- World Health Organization, The World Bank. World report on disability. In: WHO Press. 2011. http://www.who.int/disabilities/world_report/2011/en/. Accessed 20 Aug 2013.
- World Health Organization. Global burden of disease. Disease and injury regional estimates. 2011. http://www.who.int/healthinfo/global_burden_disease/estimates_regional_2000_2011/en/. Accessed 19 Aug 2013.
- Xiang H, Stallones L, Chen G, Hostetler SG, Kelleher K. Nonfatal injuries among US children with disabling conditions. Am J Pub Health. 2005;95(11):1970–5. doi: 10.2105/AJPH.2004.057505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang H, Wheeler KK, Stallones L. Disability status: a risk factor in injury epidemiologic research. Ann Epidemiol. 2014;24(1):8–16. doi: 10.1016/j.annepidem.2013.10.014. [DOI] [PubMed] [Google Scholar]
- Yung A, Haagsma JA, Polinder S. A systematic review on the influence of pre-existing disability on sustaining injury. Accid Anal Prev. 2014;62:199–208. doi: 10.1016/j.aap.2013.09.024. [DOI] [PubMed] [Google Scholar]
- Zhu HP, Xia X, Xiang HY, Yu CH, Du YK. Disability, home physical environment and non-fatal injuries among young children in China. PLoS One. 2012;7(5) doi: 10.1371/journal.pone.0037766. [DOI] [PMC free article] [PubMed] [Google Scholar]


