Abstract
Purpose
Immediate loading of dental implants has been proved to be feasible in partially edentulous jaws. The purpose of this retrospective investigation was to assess the feasibility of immediately loading dental implants in fully edentulous jaws.
Methods
A total of 24 patients aged between 53 and 89 years received a total of 154 implants in their edentulous maxillae or mandibles. Among the implants, 45 were set in fresh extracted sockets and 109 in consolidated alveolar bones. The implants were provisionally managed with chair-side made provisional resin bridges and exposed to immediate loading. Implants were followed up for 1–8 years, including radiographic imaging. Marginal bone levels were evaluated based on radiographic imaging.
Results
A total of 148 out of the 154 implants survived over the follow-up period of 1 to 8 years, giving a survival rate of 96%. The time or region of the implantation, the pre-implant augmentation, and the length and diameter of the implants had no statistically significant influence on the survival or the success rate. The marginal bone level remained stable with only minimal loss of 0.3 mm after 60 months of loading.
Conclusions
Within the limitations of this study, immediate loading is feasible for dental implants in edentulous jaws.
Keywords: Dental implants; Immediate dental implant loading; Jaw, edentulous
Graphical Abstract
INTRODUCTION
A stress-free healing period of several months has been considered as essential for the satisfactory integration of dental implants [1]. Premature loading of implants was thought to produce fibrous tissue at the bone-implant interface, which interferes with the integration of the implant. Consequently, a conventional dental implantation is a two-stage procedure [2].
In 1983, a stress-free submerged healing protocol for dental implants was reported to achieve undisturbed osseointegration and predictable success [1]. Since then, studies have revealed excellent aesthetic and functional results with immediately loaded implants [3,4,5,6,7,8,9,10]. The bone loss and the soft tissue stability of immediately loaded implants are reported to be compatible with conventionally delayed loaded implants [5,9,11,12]. Immediate loading has even been reported to have a favourable effect on papillary retention [13]. However, there are also studies reporting unfavourable consequences from immediate loading, such as disturbed alveolar remodelling and vertical alveolar bone loss [14,15]. It must be emphasised that there are strict criteria for immediate loading, including an intact extraction socket, lack of inflammation, and sufficient bone quality [16]. The interforaminal area is the most suitable region for the immediate loading of implant-supported restorations in edentulous mandibles [17]. Due to the density and quality of the bone and the stable vertical and bucco-lingual structure of this area, three to four implants can be immediately loaded in many cases [18]. In particular, the maxilla has limited horizontal and vertical bone availability, low maxillary sinus floor and poor quality of bone in the posterior area. In these cases, bone grafts are frequently required prior to implantation [19]. The issue therefore remains to be addressed whether implants in completely edentulous jaws can also be loaded immediately. Another issue is whether immediate loading is equally feasible for implants on consolidated alveolar bones as well as for implants in freshly extracted sockets.
The objective of this retrospective study was to evaluate the long-term outcomes of immediately loaded implants on completely edentulous maxillae and mandibles. Our hypothesis was that the survival and success rates of immediate-placement, immediate-loading dental implants are equal to the survival and success rates of delayed-placement, immediate-loading implants in edentulous jaws.
MATERIALS AND METHODS
Case selection
This study was designed as a single-centre retrospective cohort study. The radiographic and record data of patients receiving dental implant placement in edentulous jaws between October 2003 and April 2010 in a private clinic were assessed for eligibility for the present retrospective evaluation. All patients were at least 18 years old and able to provide informed consent.
The inclusion criteria were as follows: (1) presence of an edentulous mandible and/or edentulous maxilla; (2) receiving at least 4 implants in the mandible or at least 6 implants in the maxilla; (3) insertion torque ≥25 N/cm; (4) receiving chair-side provisional resin bridges; and (5) immediate loading of all implants and available follow-up data including dental radiographs [8,20].
The exclusion criteria were: (1) irradiated bone; (2) severe diabetes mellitus, haemorrhagic conditions, immuno-compromising, or other severe systemic diseases; (3) heavy smoking; and (4) bisphosphonate treatment [21].
All immediately placed and loaded implants fulfilled the criteria for immediate loading, which are [8,22,23]: (1) an intact extraction socket or alveolar bone; (2) sufficient bone quality and availability for primary stability of the implants (D1–D3 in general and D4 only in minor cases); (3) insertion torque ≥25 N/cm; and (4) no clinical sign of inflammation.
A total of 24 patients (13 female and 11 male) aged between 53 and 89 years (average age, 69.5) were included in this retrospective evaluation study. No patients had to be excluded, and no patients dropped out. Patients were examined at scheduled annual recalls. According to specific risk factors, local conditions, and unexpected events, additional visits were offered. All patients received XiVE® implants (Dentsply Friadent, Mannheim, Germany). Implants were provisionally restored with chair-side made provisional resin bridges and subjected to immediate loading. Final restoration was carried out 5 months after implant placement.
Surgical procedure
After crestal incision, the bone cavity was extended gradually, according to the intended implant diameter, following the manufacturer’s instructions (Dentsply Friadent, Mannheim, Germany). In general, inserted implants were placed 0.5 mm subcrestally. The mucoperiosteal flaps were sutured with monofilament, nonresorbable sutures (Ethilon 5-0, Ethicon, Norderstedt, Germany). Analgesics (600 mg of ibuprofen) were given dependent on the local conditions. Antibiotics (1,000 mg of amoxicillin, three times a day, or 600 mg of clindamycin, three times a day in case of penicillin allergy) were given for 5 days. Final wound inspection, suture removal, and occlusal adjustments were performed 7–10 days after surgery.
Immediate loading protocol
Immediately after the placement, implants received provisionally splinted resin bridges, which were fixed using temporary cement (Tempbond®, Kerr Dental, Rastatt, Germany). The occlusal surfaces were flattened to reduce lateral shear forces. Patients were instructed to take only soft food for the first 12 weeks. Occlusion was checked and corrected weekly in the first month to ensure an equal distribution of load over all implants.
Follow-up and data extraction
The follow-up period ranged from 1 year to 8 years. The average follow-up period was 4.1 years. Data for the study were extracted from medical records and radiographs and anonymised in accordance with the World Medical Association Declaration of Helsinki (64th WMA General Assembly, October 2013).
Outcome measurements
To assess clinical success, implants were categorised into groups I through IV [24]. Group I was defined by the characteristics of zero mobility, pain, tenderness, or exudate and <2 mm radiographic bone loss for all implants, and classified as “full success.” Group II was defined by implants with no mobility, pain, or tenderness but 2–4 mm of radiographic bone loss, and classified as “satisfactory survival.” Group III was defined by implants with no mobility and radiographic bone loss >4 mm but less than half of the implant length, and classified as “compromised survival.” In this group, implants may have sensitivity at loading, a history of exudate, and probing depths up to 7 mm. In group IV, implant failures were recorded with any of the following: mobility, pain on loading, uncontrolled exudate, or radiographic bone loss greater than half the length of the implant.
Radiographic measurements
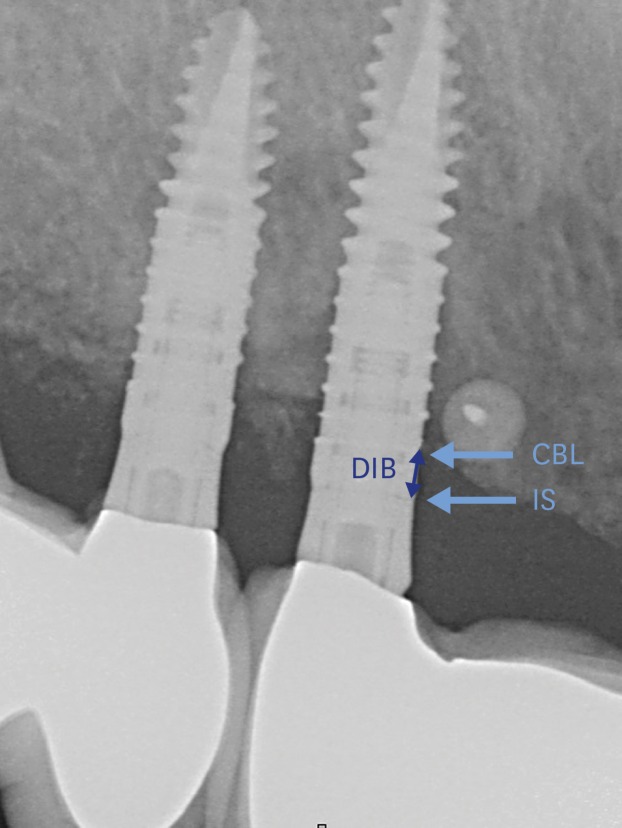
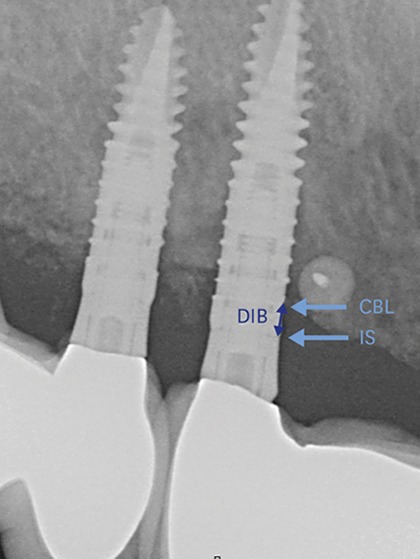
Periapical radiographs were taken before and directly after surgery using the parallel technique with position holders. Postoperative radiographs served as a baseline. All radiographs were taken with Sirona Heliodent® plus (Sirona Dental Systems, Bensheim, Germany) and processed by Duerr VistaScan® (Duerr Dental Systems, Bietigheim-Bissingen, Germany). All radiographs of the patients were analysed digitally (Sidexis XG, Sirona Dental Systems, Bensheim, Germany) by 2 dental researchers, who did not participate in the surgical procedures. Measurements were carried out in a darkened room on a 27" diagnostic monitor (MDview 271, NEC, Tokyo, Japan). The crestal bone level (CBL) was defined as the most coronal, direct bone-to-implant contact. The distance from implant shoulder (IS) to the first bone contact point along the implant (DIB) was measured mesially and distally and the mean was taken [25] (Figure 1). The bone level at each follow-up examination was subtracted from the baseline to obtain the changes in bone level.
Figure 1.
The change in bone level. Defining crestal bone level (CBL), implant shoulder (IS) and the distance between both (DIB).
Statistical analysis
For power calculation of the success rate of the implants, the test value was set at 99% and the alpha-error level at 5%. The correlation of the survival rate and marginal bone loss with the time of implant placement, the localisation of the implants, the pre- and peri-implant augmentation, the sinus floor elevation, the type of prosthetic restoration, and the length and diameter of the implants were tested by Cox regression. The level of significance was set at 95% (P≤0.05). Inter- and intra-observer reliability were assessed with an intraclass correlation coefficient for consistency and absolute agreement of the data in a two-way mixed model [26]. The confidence interval (CI) was set at 95%. Statistical analysis was performed with SPSS® version 22.0 (IBM Corp., Armonk, NY, USA).
RESULTS
Descriptive data
A total of 154 implant placements were carried out in 24 patients, 81 (53%) in maxillae and 73 (47%) in mandibles. Ten of the patients presented complete edentulism of the mandible and/or maxilla. The other 14 had a total of 45 residual teeth, which were extracted directly before dental implant placement. Among the 154 implant placements, 109 (71%) were placed in consolidated or partially consolidated alveolar bones, and the remaining 45 were placed in alveolar sockets immediately after tooth extraction. The majority of non-consolidated alveolar bones were prepared for implantation by surgical debridement of infected sockets, grafting by external sinus floor elevation, and/or peri-implant bone augmentations with autologous particulated bone and/or bone substitutes. In selected cases, bone grafting and implant placement were carried out in one procedure. In 76% of the cases, fixed prostheses were used for final restoration. In 24% of the cases, removable prostheses supported by bars or tapered crowns were used.
Success
Among a total of 154 implants, 148 were successful over the whole follow-up period, up to 8 years, giving a general survival and success rate of 96% (95% CI, 93%–99%). Setting the test value at 99% and the alpha-error level at 5%, the power was 82%. This success rate remains the same for the 81 maxillary implants as well as for the 73 mandibular implants. Except for 2 delayed-placement implants that had >3 mm of radiographic bone loss (group II), the remaining 146 successful implants (in total, 95%) met the criteria for “full success,” that is, no mobility, no pain, no tenderness, no exudate, and <3 mm of radiographic bone loss (Table 1).
Table 1. The success rates of implants.
| Groups | Immediate-placement implants | Delayed-placement implants | Total |
|---|---|---|---|
| Group I | 40 (93.0%) | 105 (94.6%) | 145 |
| Group II | 0 | 3 (2.7%) | 3 |
| Group III | 0 | 0 | 0 |
| Group IV | 3 (7.0%) | 3 (2.7%) | 6 |
| Total | 43 (100%) | 111 (100%) | 154 |
Group I, full success; Group II, satisfactory survival; Group III, compromised survival; Group IV, failure.
Failures
A total of 6 (4%) implants failed within the entire follow-up period of up to 8 years (Table 2). Three of them required removal 2 months after placement because of the mobility of the implants due to massive peri-implant bone loss. The fourth implant was in the posterior maxilla and the failure was due to bacterial infection and abscess formation 3 months after implant placement. The last 2 failed implants were located in the posterior maxilla. They required removal 5 and 7 years after placement because of chronic peri-implant disease, which could not be treated successfully. The patients had chronic pain and inflammation at the implant sites, and the vertical bone loss was massive. Two short-term failures occurred in 1 patient (No. 23), on 2 distanced implants at positions 32 and 42. This patient had a total of 5 implants; the other 3 survived with full success. The 2 peri-implant disease-related failures caused increased bone loss (>3 mm) for 2 neighbouring implants, which survived, but were rated as less satisfactory. However, the other 16 implants (8 in each of these 2 patients) met the criteria for full success.
Table 2. The characterization of the 6 failed implants.
| Patient No./Sex | Age (yr) | Failure | Delayed placement | External sinus floor elevation | Final prosthetic restoration | Other implants in the patient | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Time (mon) | Reason | Position | Size (mm) | Survived | Total | |||||
| 2/F | 62 | 2 | Failed osseo-integration | 26 | 4.5×15 | Yes | Algipore® and autologous bone | No | 9 (Full success) | 10 |
| 11/M | 57 | 2 | Failed osseo-integration | 42 | 3.8×11 | No | No | No | 3 (Stable, 1–1.5-mm bone loss) | 5 |
| 32 | ||||||||||
| 14/M | 58 | 3 | Chronic bacterial infection | 31 | 3.4×13 | No | No | No | 3 (All satisfactory) | 4 |
| 23/F | 50 | 65 | Peri-implant disease | 25 | 3.8×18 | Yes | Algipore® and autologous bone | Fixed single crown | 9 (3-mm bone loss for implant at position), 26 (Other 8 satisfactory) | 10 |
| 25/M | 57 | 85 | Peri-implant disease | 16 | 3.8×15 | Yes | Algipore® and autologous bone | Fixed bridge | 9 (>3-mm bone loss for implant at position), 17 (Other 8 successful) | 10 |
F, female; M, male.
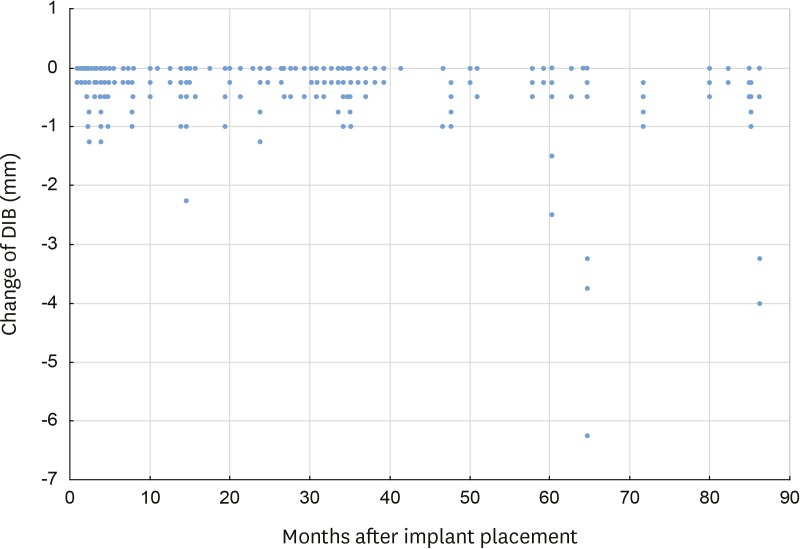
Crestal bone level
The decrease in bone level was minimal (mean, <0.3 mm) over a period of 60 months. Remarkably, the decrease in the average marginal bone level during the first 12 months was −0.28 mm. After 12–24 months, there were no significant changes up to 60 months. The average maximum bone level decrease was never in excess of −0.5 mm, but the standard deviation was very high for the recalls at 72 and 84 months (Table 3, Figure 2).
Table 3. The bone-level decrease at various time points after implant placement.
| Month(s) after implant placement | Sample size | Bone-level change | |
|---|---|---|---|
| Mean | Standard deviation | ||
| 3 | 104 | −0.08 | 0.22 |
| 6 | 143 | −0.10 | 0.22 |
| 9 | 32 | −0.14 | 0.25 |
| 12 | 9 | −0.14 | 0.22 |
| 24 | 83 | −0.17 | 0.37 |
| 36 | 153 | −0.09 | 0.19 |
| 48 | 54 | −0.14 | 0.24 |
| 60 | 30 | −0.10 | 0.16 |
| 72 | 39 | −0.45 | 0.88 |
| 84 | 30 | −0.33 | 0.61 |
Figure 2.
The original data of bone level change (against post-implant placement baseline) for each implant at each follow-up examination. Note that most measurements were during the period up to 48 months.
Statistical results
The consistency and absolute agreement of the data indicated a high inter- and intra-observer reliability for the measurements (Table 4). No correlation was found between survival and marginal bone loss for immediate- and delayed-placement dental implants concerning localisation, implant length and diameter, peri-implant augmentation, or sinus floor elevation (Table 5). Even the type of prosthetic restoration (fixed or removable prostheses) and the time of implant placement (immediate or delayed placement) showed no influence on survival or marginal bone loss.
Table 4. The reliability of the data.
| Variables | Consistency of data | Absolute agreement of data |
|---|---|---|
| Inter-observer reliability | 0.93 (95% CI: 0.92; 0.93) | 0.93 (95% CI: 0.92; 0.94) |
| Intra-observer reliability | 0.95 (95% CI: 0.94; 0.96) | 0.95 (95% CI: 0.95; 0.96) |
Table 5. The results of Cox regression.
| Variables | P-values of Cox regression, level of significance 95% |
|---|---|
| Localisation of implants | 0.80 |
| Implant length | 0.94 |
| Implant diameter | 0.98 |
| Peri-implant augmentation | 1.00 |
| Sinus floor elevation | 0.99 |
| Type of prosthetic restoration | 0.95 |
| Time of implant placement | 0.99 |
DISCUSSION
Immediately loaded implants in edentulous jaws achieved an excellent general survival and success rate of 96%. No statistically significant differences were found between immediate-placement and delayed-placement, immediate-loading implants. Within its limits, the present study shows that immediate loading (with soft food for the first 3 months) can be feasible for implants in edentulous jaws, provided that the criteria for immediate loading are fulfilled, including sufficient bone quality, quantity, and insertion torque of at least 25 N/cm.
The peri-implant bone level decreased only slightly by a mean of <0.3 mm over a period of 5 years, which is remarkably low. In comparison, up to 1.5 mm of bone loss has been reported for implants with delayed loading [27,28]. The increased bone loss after 6 years may be due to a biased overestimation, since most patients with successful implants did not regularly come to follow-ups.
A recent systematic review reported a lack of evidence that teeth extraction, implant position (anterior/posterior/maxillary/mandibular), or loading type has any significant effect on the implant survival rate [29]. Another retrospective study reported nearly equal 2-year survival rates for immediately loaded implants in the anterior (99.4%) and the posterior (97%) mandibles [30]. In a recent retrospective analysis of 13,147 implants in 4,316 patients at the Academy for Oral Implantology in Vienna, overall implant survival was 97% and was not associated with implant length, implant diameter, jaw location, implant position, local bone quality, previous bone augmentation, or other patient-related factors like osteoporosis, age, or diabetes mellitus [31]. In concordance with these results, our success and survival rates did not differ regarding the time or position of the implant and the pre-implant treatment, such as external sinus floor elevation.
Six implants out of 154 (4%) failed in this study. One of them failed due to bacterial infection, and another 2 due to inflammation; these failures were therefore unlikely to be directly related to the immediate loading protocol. The other 3 failures were due to failed osseo-integration, which was possibly, but not necessarily related to immediate loading. One possible reason for the failure was the insufficient alveolar bone quality, since these 3 failed implants were placed in cortical bone (D4) in the anterior mandible. These implants, therefore, may have failed even with delayed loading. In any case, caution is advised for such implants. Other parameters, such as site and size of the implants, did not have a detectable effect on the survival of the immediately loaded implants in this study. It is also possible that the patients did not follow the instructions for optimal outcomes in immediate loading and that the failed implants were overloaded. However, the polygonal support of the provisional resin bridges also enabled an optimal distribution of mastication forces on all implants and therefore may have contributed to the avoidance of overloading on single implants.
The survival and success rate of 96% in this study is comparable to those rates of immediately loaded implants in recent publications [4,32]. These results are also in accordance with those of other studies, in that similar long-term survival and success rates can be achieved for immediately loaded and for conventionally loaded dental implants [9,33,34]. In a recent retrospective analysis of implant survival, biological complications, and success in implants that supported immediately loaded, implant-based rehabilitations, Francetti et al. [35] reported a 100% implant survival rate 5 years after loading. However, the cumulative success rate in this study according to Misch et al. [24] was only 76%. Patients with upright and tilted implants supporting full-arch rehabilitations were included. The main reason for the low success rate was the resorption of marginal bone over time, which was, however, not associated with peri-implant infectious disease. They found no statistically significant differences between tilted- and upright-placement implants. One reason for the differences in both studies concerning success could be the number of implants per patient: 6.4 on average per patient in the present study versus 4.6 per patient in the cited study. Higher load per implant might be a reason for higher marginal bone resorption over time. However, it must be mentioned that two-dimensional radiographs can only indirectly assess quantitative three-dimensional changes in the marginal bone level. The frequency of follow-up intervals was not reported in the cited study. In the present study, data after 60 months were only available for a small number of patients as can be seen in the large standard deviation. Due to a very low number of failed implants, statistic evaluations must also be examined critically.
To conclude, immediate loading of dental implants may be a safe and reliable treatment option for dental rehabilitation of edentulous jaws. However, well-designed, randomised, controlled, prospective studies are needed to confirm the long-term stability of immediately loaded dental implants in edentulous jaws.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Brånemark PI. Osseointegration and its experimental background. J Prosthet Dent. 1983;50:399–410. doi: 10.1016/s0022-3913(83)80101-2. [DOI] [PubMed] [Google Scholar]
- 2.Esposito M, Grusovin MG, Maghaireh H, Worthington HV. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev. 2013:CD003878. doi: 10.1002/14651858.CD003878.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chiapasco M, Gatti C, Rossi E, Haefliger W, Markwalder TH. Implant-retained mandibular overdentures with immediate loading. A retrospective multicenter study on 226 consecutive cases. Clin Oral Implants Res. 1997;8:48–57. doi: 10.1111/j.1600-0501.1997.tb00007.x. [DOI] [PubMed] [Google Scholar]
- 4.Degidi M, Nardi D, Piattelli A. 10-year prospective cohort follow-up of immediately restored XiVE implants. Clin Oral Implants Res. 2016;27:694–700. doi: 10.1111/clr.12642. [DOI] [PubMed] [Google Scholar]
- 5.Ganeles J, Wismeijer D. Early and immediately restored and loaded dental implants for single-tooth and partial-arch applications. Int J Oral Maxillofac Implants. 2004;19(Suppl):92–102. [PubMed] [Google Scholar]
- 6.Mozzati M, Arata V, Gallesio G, Mussano F, Carossa S. Immediate postextractive dental implant placement with immediate loading on four implants for mandibular-full-arch rehabilitation: a retrospective analysis. Clin Implant Dent Relat Res. 2013;15:332–340. doi: 10.1111/j.1708-8208.2011.00412.x. [DOI] [PubMed] [Google Scholar]
- 7.Peñarrocha M, Boronat A, Garcia B. Immediate loading of immediate mandibular implants with a full-arch fixed prosthesis: a preliminary study. J Oral Maxillofac Surg. 2009;67:1286–1293. doi: 10.1016/j.joms.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 8.Romanos GE. Present status of immediate loading of oral implants. J Oral Implantol. 2004;30:189–197. doi: 10.1563/1548-1336(2004)30<189:PSOILO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Romanos GE, Aydin E, Locher K, Nentwig GH. Immediate vs. delayed loading in the posterior mandible: a split-mouth study with up to 15 years of follow-up. Clin Oral Implants Res. 2016;27:e74–9. doi: 10.1111/clr.12542. [DOI] [PubMed] [Google Scholar]
- 10.Horiuchi K, Uchida H, Yamamoto K, Sugimura M. Immediate loading of Brånemark system implants following placement in edentulous patients: a clinical report. Int J Oral Maxillofac Implants. 2000;15:824–830. [PubMed] [Google Scholar]
- 11.Paolantonio M, Dolci M, Scarano A, d'Archivio D, di Placido G, Tumini V, et al. Immediate implantation in fresh extraction sockets. A controlled clinical and histological study in man. J Periodontol. 2001;72:1560–1571. doi: 10.1902/jop.2001.72.11.1560. [DOI] [PubMed] [Google Scholar]
- 12.Schropp L, Kostopoulos L, Wenzel A. Bone healing following immediate versus delayed placement of titanium implants into extraction sockets: a prospective clinical study. Int J Oral Maxillofac Implants. 2003;18:189–199. [PubMed] [Google Scholar]
- 13.De Rouck T, Collys K, Cosyn J. Immediate single-tooth implants in the anterior maxilla: a 1-year case cohort study on hard and soft tissue response. J Clin Periodontol. 2008;35:649–657. doi: 10.1111/j.1600-051X.2008.01235.x. [DOI] [PubMed] [Google Scholar]
- 14.Araújo MG, Sukekava F, Wennström JL, Lindhe J. Tissue modeling following implant placement in fresh extraction sockets. Clin Oral Implants Res. 2006;17:615–624. doi: 10.1111/j.1600-0501.2006.01317.x. [DOI] [PubMed] [Google Scholar]
- 15.Araújo MG, Wennström JL, Lindhe J. Modeling of the buccal and lingual bone walls of fresh extraction sites following implant installation. Clin Oral Implants Res. 2006;17:606–614. doi: 10.1111/j.1600-0501.2006.01315.x. [DOI] [PubMed] [Google Scholar]
- 16.Kawahara H, Kawahara D, Hayakawa M, Tamai Y, Kuremoto T, Matsuda S. Osseointegration under immediate loading: biomechanical stress-strain and bone formation--resorption. Implant Dent. 2003;12:61–68. doi: 10.1097/01.id.0000034394.75768.e3. [DOI] [PubMed] [Google Scholar]
- 17.Testori T, Meltzer A, Del Fabbro M, Zuffetti F, Troiano M, Francetti L, et al. Immediate occlusal loading of Osseotite implants in the lower edentulous jaw. A multicenter prospective study. Clin Oral Implants Res. 2004;15:278–284. doi: 10.1111/j.1600-0501.2004.01013.x. [DOI] [PubMed] [Google Scholar]
- 18.Brånemark PI, Engstrand P, Ohrnell LO, Gröndahl K, Nilsson P, Hagberg K, et al. Brånemark Novum: a new treatment concept for rehabilitation of the edentulous mandible. Preliminary results from a prospective clinical follow-up study. Clin Implant Dent Relat Res. 1999;1:2–16. doi: 10.1111/j.1708-8208.1999.tb00086.x. [DOI] [PubMed] [Google Scholar]
- 19.Gross JS. Bone grafting materials for dental applications: a practical guide. Compend Contin Educ Dent. 1997;18:1013–1018. 1020–1012. [PubMed] [Google Scholar]
- 20.Kornmann F. Sofortige provisorische Versorgung bzw. Belastung nach Sofort- und/oder Spätimplantation. Quintessenz. 2010;61:699–707. [Google Scholar]
- 21.Buser D, von Arx T, ten Bruggenkate C, Weingart D. Basic surgical principles with ITI implants. Clin Oral Implants Res. 2000;11(Suppl 1):59–68. doi: 10.1034/j.1600-0501.2000.011s1059.x. [DOI] [PubMed] [Google Scholar]
- 22.Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9:332–343. [PubMed] [Google Scholar]
- 23.Lazzara RJ. Effect of implant position on implant restoration design. J Esthet Dent. 1993;5:265–269. doi: 10.1111/j.1708-8240.1993.tb00791.x. [DOI] [PubMed] [Google Scholar]
- 24.Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, et al. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008;17:5–15. doi: 10.1097/ID.0b013e3181676059. [DOI] [PubMed] [Google Scholar]
- 25.Buser D, Weber HP, Lang NP. Tissue integration of non-submerged implants. 1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res. 1990;1:33–40. doi: 10.1034/j.1600-0501.1990.010105.x. [DOI] [PubMed] [Google Scholar]
- 26.Kim HY. Statistical notes for clinical researchers: Evaluation of measurement error 1: using intraclass correlation coefficients. Restor Dent Endod. 2013;38:98–102. doi: 10.5395/rde.2013.38.2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Canullo L, Fedele GR, Iannello G, Jepsen S. Platform switching and marginal bone-level alterations: the results of a randomized-controlled trial. Clin Oral Implants Res. 2010;21:115–121. doi: 10.1111/j.1600-0501.2009.01867.x. [DOI] [PubMed] [Google Scholar]
- 28.Canullo L, Goglia G, Iurlaro G, Iannello G. Short-term bone level observations associated with platform switching in immediately placed and restored single maxillary implants: a preliminary report. Int J Prosthodont. 2009;22:277–282. [PubMed] [Google Scholar]
- 29.Lang NP, Pun L, Lau KY, Li KY, Wong MC. A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Implants Res. 2012;23(Suppl 5):39–66. doi: 10.1111/j.1600-0501.2011.02372.x. [DOI] [PubMed] [Google Scholar]
- 30.Kacer CM, Dyer JD, Kraut RA. Immediate loading of dental implants in the anterior and posterior mandible: a retrospective study of 120 cases. J Oral Maxillofac Surg. 2010;68:2861–2867. doi: 10.1016/j.joms.2010.05.086. [DOI] [PubMed] [Google Scholar]
- 31.Busenlechner D, Fürhauser R, Haas R, Watzek G, Mailath G, Pommer B. Long-term implant success at the Academy for Oral Implantology: 8-year follow-up and risk factor analysis. J Periodontal Implant Sci. 2014;44:102–108. doi: 10.5051/jpis.2014.44.3.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schindjalova R. Immediate implantation in retrospect – a study regarding success and failure of implantations. Z Zahnärztl Implantol. 2015;31:132–139. [Google Scholar]
- 33.Imburgia M, Del Fabbro M. Long-term retrospective clinical and radiographic follow-up of 205 Brånemark System Mk III TiUnite implants submitted to either immediate or delayed loading. Implant Dent. 2015;24:533–540. doi: 10.1097/ID.0000000000000265. [DOI] [PubMed] [Google Scholar]
- 34.Moraschini V, Porto Barboza E. Immediate versus conventional loaded single implants in the posterior mandible: a meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg. 2016;45:85–92. doi: 10.1016/j.ijom.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 35.Francetti L, Rodolfi A, Barbaro B, Taschieri S, Cavalli N, Corbella S. Implant success rates in full-arch rehabilitations supported by upright and tilted implants: a retrospective investigation with up to five years of follow-up. J Periodontal Implant Sci. 2015;45:210–215. doi: 10.5051/jpis.2015.45.6.210. [DOI] [PMC free article] [PubMed] [Google Scholar]