Abstract
Background:
Despite relatively high number of women who attend antenatal care (ANC) in Cameroon, there is an ever-increasing maternal mortality ratio, and pregnancy outcomes remain inadequate. A new suggested Optimal ANC Package includes attending ANC in the first trimester. This study assesses the overall ANC coverage, the percentage, and pregnancy outcomes among women who attended and did not attend ANC in the first trimester in the Buea Regional Hospital (BRH) in Cameroon.
Methods:
A cross-sectional study was carried out among 200 consenting pregnant women presenting for delivery at the BRH. A bivariate analysis was used to compare the frequencies of various pregnancy outcomes within the the two categories of women who attended and who did not attend first trimester ANC.
Results:
Ninety-six percent of the women attended at least 1 ANC visit with 20.5% of these women attending ANC in the first trimester and 60.2% attending at least 4 visits. Sociodemographic and obstetric factors were not found to be associated with attending ANC in the first trimester. Also, there was no statistically significant association between all the late pregnancy outcomes assessed and attending ANC in the first trimester.
Conclusions and Global Health Implications:
Trends in most sub-Saharan countries seem to suggest that most women do not attend first trimester ANC. This could have negative consequences on overall perinatal outcome. More user-friendly educational programs for women of childbearing age is required in such regions to address this situation.
Keywords: Antenatal Care, Optimal Antenatal Care Package, First Trimester Antenatal Care, Buea Regional Hospital, Cameroon
Background
Cameroon has good antenatal care (ANC) coverage with 82% of pregnant women attending at least one ANC in 2007 and 60% of these women attending at least 4 visits.[1,2] However, despite such coverage, Maternal mortality ratio (MMR) increased from 680 to 872 deaths per 100,000 from 2003-2012 and pregnancy outcomes are still inadequate.[2] This remains a major impediment towards the overall achievement of the fifth Millenuium Development Goal (MDG)—improving maternal health.[3] Adequate and optimal ANC has been proposed as one of the strategies to combat increasing MMR and to improve pregnancy outcomes.[4] The World Health Organization (WHO) advocates that adequate ANC should include at least four visits for any pregnancy.[5] However, recent studies have suggested that adequate and effective ANC should be upgraded to include the following four components which make up an Optimal ANC Package: 1) at least four ANC visits; 2) with the first visit in the first trimester; 3) the last visit in the third trimester and 4) with all the visits supervised by a skilled professional.[6, 7] These authors stressed the need for the attendance of four visits as stipulated by WHO and also the commencement of these visits as early as possible in the first trimester.[7] The authors further suggested that the definition of optimal ANC should be changed to include the above four components especially in developing countries like Cameroon[6,7] inorder to adapt to the ever increasing MMR. These changes were finally accepted in a WHO updated report in 2002.[5] One of these components (commencing first visit in the first trimester) is aimed at assessment of the health of the woman to ensure that she is as healthy as possible during the pregnancy and delivery.[7] During this first trimester visit, remedial actions and treatment of previous medical conditions are undertaken so as to improve pregnancy outcomes. The overall aim of this study was therefore to determine if commencing ANC in the first trimester as proposed by this package, and later adopted by WHO, was associated with better pregnancy and delivery outcomes in a suburban population of pregnant women in Cameroon. The study assessed the prevalence of women who attended at least four ANC visits in the BRH. It also determined the prevalence of women who commenced ANC in the first trimester, the sociodemographic and clinical factors associated with commencing ANC in this trimester, and the late pregnancy and delivery outcomes in women who started ANC in the first trimester of pregnancy as opposed to women who did not.
Methods
Study design and setting
A cross-sectional study was carried out at the Buea Regional Hospital (BRH). The BRH is situated in the Buea Health District (BHD) which is part of the Fako Division, South-West Region, Cameroon. The BRH acts as the reference hospital in the health district and performs more deliveries than all the other health facilities in the district. The hospital has all the standard units of general medicine. One Obstetrician runs the maternity.[8]
Participants and sampling
All pregnant women-newborn pairs who attended the BRH during the period of the study were included. Women who delivered at a gestational age below 28 weeks, those who had multiple gestations and those who did not provide consent to take part in the study were excluded.
Data collection, variables and measurements
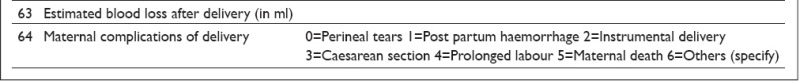
The study was carried out over a period of three months, from January 2 to March 23, 2013. Women who were about to put to birth were monitored throughout their labor. Their hospital records were assessed to obtain the following information:[8]
Socio-demographic characteristics including socioeconomic status, and level of education divided into low (no education and primary education) and high (secondary and university education).
Obstetric history (gravidity, parity, year of first pregnancy, previous birth weight, antenatal care (ANC) history for the current pregnancy, and history of anaemia, fever and malaria during the current pregnancy.
Past medical history (history of chronic illness like HIV, history of pregnancy related illnesses like pre-eclampsia/eclampsia and gestational hypertension and pre-pregnancy weight).
Toxicological history (alcohol intake, cigarette smoking, other substance abuse and recreational drug use).
Participants’ weight to the nearest kilogram (kg) and height to the nearest centimetre (cm) were measured using a Camry bathroom scale and a locally made stadiometer calibrated to the Butterfly brand measuring tape respectively. A standard physical examination was performed. Throughout the labor, the fetus was monitored for the presence of acute fetal distress (i.e., fetal heart rate < 120 beats per minute and/or green meconium-stained amniotic fluid at delivery). After delivery, the neonates were assessed for viability (breathing, beating of the heart, pulsation of the umbilical cord or definite movements of voluntary muscles), and their APGAR scores at the first, fifth and tenth minutes were assessed. The baby’s weight was measured to the nearest gram using a Holtex+ digital baby scale. The newborns were monitored for the presence of respiratory distress (respiratory grunting, nasal flaring, intercostal recessions, sub-xyphoid recession, thoraco-abdominal asynchrony, and respiratory rate < 40 or > 60 breaths per minute). Stillbirths and in-hospital neonatal deaths were recorded. The mother was informed of the entire study before labor and her consent was requested at the end of the labor process to reduce the possibility of coercion due to labor pains. Only those who agreed to participate in the study post-labor were included after they signed the inform consent form. All the data collected was then entered into a survey questionnaire (attached below). Minors and their guardians signed assent and guardian consent forms respectively.[8]
Data management and statistical analysis
The data were stored securely in a private location and kept confidential. Participants were referred to only by their identification numbers. Identifiable information (consent forms) was kept separate from the questionnaires and it was only possible to link both through a coding sheet which was available only to the principal investigator. Data were analysed using Epi Info version 3.5.4. Means (standard deviations) were used to summarise continuous variables and frequencies for categorical variables. Frequencies were compared using Fisher’s exact tests. Statistical significance was set at p < 0.05.
Ethical considerations
Ethical approval was obtained from the Institutional Review Board of the Faculty of Health Sciences, University of Buea.
Results
ANC attendance
Of the 200 participants, 96% attended at least one ANC visit, 60.2% attended at least four ANC visits and 20.5% commenced ANC visits in the first trimester.
Socio-demographic and obstetrical characteristics of mothers
The mean age of the mothers was 26.4 ± 5.8 years; 57.0% were married; 50.5% were unemployed; 79.9% of them had a high level of education; and 6.6% of the women reported spending less than $1 (United States dollar) a day. Women who were married, had a high level of education, multiparous, multigravidas, employed, non-teens and those who spent more than $1 (USD) a day were not more likely to commence ANC in the first trimester (Table 1).
Table 1.
Socio-demographic characteristics and obstetric history of mothers delivering in the Buea Regional Hospital, January – March 2013
| Socio-demographic factor | Groups | ANC FT* N | (%) | No ANC FT† N | (%) | N | p value |
|---|---|---|---|---|---|---|---|
| Marital status (N=200) | Married | 22 | 19.3 | 92 | 80.7 | 114 | 0.4 |
| Single | 19 | 22.1 | 67 | 77.9 | 86 | ||
| Occupation (N=200) | Unemployed | 20 | 19.8 | 81 | 80.2 | 101 | 0.5 |
| Employed | 21 | 21.2 | 78 | 78.8 | 99 | ||
| Level of education (N=199) | Low | 5 | 12.5 | 35 | 87.5 | 40 | 0.1 |
| High | 36 | 22.6 | 123 | 77.4 | 159 | ||
| Age groups (N=200) | Teenagers | 4 | 13.3 | 26 | 86.7 | 30 | 0.2 |
| Non-teens | 37 | 21.8 | 133 | 78.2 | 170 | ||
| Daily income (N=200) | <1USD‡ | 3 | 12.5 | 21 | 87.5 | 24 | 0.2 |
| ≥1USD | 35 | 22.5 | 123 | 77.8 | 158 | ||
| Gravidity (N=200) | <5 | 34 | 19.9 | 137 | 80.1 | 171 | 0.4 |
| ≥5 | 7 | 24.1 | 22 | 75.9 | 29 | ||
| Parity (N=200) | Nulliparous | 20 | 22.2 | 70 | 77.8 | 90 | 0.4 |
| Multiparous | 21 | 19.1 | 89 | 80.9 | 110 | ||
Women who attended ANC in the first trimester;
Women who did not attend ANC in the first trimester;
USD: United States dollars
Pregnancy outcomes
Late pregnancy outcomes were divided into maternal and fetal pregnancy outcomes. Maternal pregnancy outcomes included: weight gain during pregnancy, BMI at delivery, preterm delivery, caesarean delivery, prolonged labor and post-partum hemorrhage. Fetal pregnancy outcomes included: fetal distress, neonatal asphyxia, respitatory distress, low birth weight (LBW) and high birth weight (HBW). Other pregnancy outcomes assessed were: malaria and anemia in pregnancy.
There was no statistically significant differences in the following pregnancy outcomes between women who commenced ANC in the first trimester and those who did not: poor weight gain, malaria in pregnancy, anemia in pregnancy, delivery BMI, preterm delivery, caesarean delivery, neonatal asphyxia, fetal distress, respiratory distress, neonatal death, shoulder dystocia, prolonged labor, post-partum hemorrhage, LBW and HBW (Table 2).
Table 2.
Pregnancy outcomes of women who attended antenatal care visits in the first trimester in the Buea Regional Hospital, January – March 2013
| Pregnancy outcomes | ANC FT* n | (%) | No ANC FT†n | (%) | Total | p-value |
|---|---|---|---|---|---|---|
| Weight gain | ||||||
| ≤10 kg | 11 | 32.4 | 35 | 36.1 | 46 | 0.4 |
| >10 kg | 23 | 67.6 | 62 | 63.9 | 85 | |
| Malaria in pregnancy | ||||||
| Yes | 13 | 31.7 | 43 | 27.0 | 56 | 0.3 |
| No | 28 | 68.3 | 116 | 73.0 | 114 | |
| Anaemia in pregnancy | ||||||
| Yes | 19 | 46.3 | 54 | 34.0 | 73 | 0.1 |
| No | 22 | 53.7 | 105 | 66.0 | 127 | |
| Delivery BMI‡ | ||||||
| <25 kg/m2 | 5 | 12.5 | 25 | 15.7 | 30 | 0.4 |
| ≥25 kg/m2 | 35 | 87.5 | 134 | 84.3 | 169 | |
| Preterm delivery | ||||||
| Yes | 9 | 22.0 | 28 | 17.6 | 37 | 0.3 |
| No | 32 | 78.0 | 131 | 82.4 | 163 | |
| Caesarean delivery | ||||||
| Yes | 6 | 14.6 | 19 | 11.9 | 25 | 0.4 |
| No | 35 | 85.4 | 140 | 88.1 | 175 | |
| Asphyxia (1st minute) | ||||||
| Yes | 17 | 41.5 | 55 | 35.7 | 72 | 0.3 |
| No | 24 | 58.5 | 99 | 64.3 | 123 | |
| Asphyxia (5th minute) | ||||||
| Yes | 4 | 9.8 | 29 | 18.5 | 33 | 0.1 |
| No | 37 | 90.2 | 128 | 81.5 | 165 | |
| Asphyxia (10th minute) | ||||||
| Yes | 2 | 4.9 | 16 | 10.2 | 18 | 0.2 |
| No | 39 | 95.1 | 141 | 89.8 | 180 | |
| Fetal distress | ||||||
| Yes | 8 | 19.5 | 31 | 19.5 | 39 | 0.6 |
| No | 33 | 80.5 | 128 | 80.5 | 161 | |
| Respiratory distress | ||||||
| Yes | 3 | 7.3 | 11 | 6.9 | 14 | 0.6 |
| No | 38 | 92.7 | 148 | 93.1 | 186 | |
| Neonatal death | ||||||
| Yes | 3 | 7.3 | 13 | 8.2 | 16 | 0.6 |
| No | 38 | 92.7 | 146 | 91.8 | 184 | |
| Shoulder dystocia | ||||||
| Yes | 2 | 4.9 | 5 | 3.1 | 7 | 0.4 |
| No | 39 | 95.1 | 154 | 96.9 | 193 | |
| Prolonged labor | ||||||
| Yes | 13 | 31.7 | 45 | 28.8 | 58 | 0.4 |
| No | 28 | 68.3 | 111 | 71.2 | 139 | |
| Post-partum hemorrhage | ||||||
| Yes | 2 | 4.9 | 8 | 5.0 | 10 | 0.7 |
| No | 39 | 95.1 | 151 | 95.0 | 190 | |
| Low birth weight | ||||||
| Yes | 10 | 24.4 | 28 | 17.6 | 38 | 0.2 |
| No | 31 | 75.6 | 131 | 82.4 | 162 | |
| High birth weight | ||||||
| Yes | 6 | 14.6 | 22 | 13.8 | 28 | 0.3 |
| No | 35 | 85.4 | 137 | 86.2 | 172 | |
Women who attended ANC in the first trimester;
Women who did not attend ANC in the first trimester;
BMI: Body mass index
Discussion
The aim of this study was to assess the overall ANC coverage in the BRH and to determine the pregnancy and delivery outcomes of women who commenced ANC visits in the first trimester. We determined that 96% of the women attended at least 1 ANC visit with 20.5% of this women starting their visits in the first trimester. However, there was no significant differences in the late pregnancy and delivery outcomes of women who commenced visists in the first trimester when compared to women who did not.
In this study, all the pregnancy outcomes assessed were not associated with early ANC attendance. However, most of the factors were assessed after viability of the fetus (after 28 weeks of gestation) hence this study was able to assess only the late pregnancy and delivery outcomes. The study did not therefore assess the early pregnancy outcomes in women in the BRH. Further studies are therefore necessary to assess the effects of first trimester ANC in suburban Cameroon especially concerning crucial factors like the risk of abortions in the first and second trimesters of pregnancy. Studies carried out elsewhere have shown varied results. A similar study in Nigeria suggested that as a single component, early booking for ANC was a poor predictor of delivery and pregnancy outcomes.[9] These findings were similar to our study. Both studies assessed similar pregnancy outcomes: operative deliveries, delivery complications and LBW. In contrast, Temple et al in the UK showed that prepregnancy care was associated with early booking, good glycemic control in early pregnancy and reduced adverse outcomes like: spontaneous abortions, malformations, perinatal death and premature delivery.[10] Furthermore, other authors have advocated for the success of the first trimester ANC in the diagnosis of early congenital malformations, control of anaemia, and prevention of malaria complications.[11, 12] Also, the authors who proposed the Optimal ANC Package,[4, 6] suggested its use for screening against malaria, anaemia, HIV and diabetes, screening three major risks during delivery: uterine scar, breach presentation and premature rupture of membranes and finally warning the pregnant woman on danger signs during delivery.[13] These factors were expected to improve pregnancy and delivery outcomes. Nontheless, using this component of the Optimal ANC Package alone as shown in our study and others[9] may not be an adequate predictor of adverse late pregnancy outcomes in suburban populations. Therefore more research is needed to establish the benefits of: commencing ANC as early as the first trimester and the other components of the Optimal ANC Package as a combination, on early and late pregnancy outcomes and delivery outcomes.
A 96% ANC coverage was obtained for women who attended at least 1 visit in this study. This is higher than the national ANC coverage in Cameroon obtained in 2007 where 82% attended at least one ANC visit.[1] The ANC attendance rate in our study (96%) was also similar to that obtained in the Buea Health District (91.3%) in 2010.[14] This shows that there is a general high ANC attendance rate in Buea. Furthermore, the ANC attendance rate in our study was quite similar to that obtained in other countries in Subsaharan Africa (SSA) where rates of 92.5% and 90% were obtained in Equitorial Guinea and Kenya respectively.[15, 16] However, only 20.5% of the participants in this study commenced ANC in the first trimester despite this component being placed in the package for optimal ANC.[6, 13] This percentage was similar to the 21.6% obtained in the rural districts of Zimbabwe in 1999 but quite higher than those obtained in Nigeria in 2008 (7.6%), Uganda in 2007 (16%) and Malawi in 2010 (9.0%).[17-20] Nontheless, in Eastern Sudan a higher proportion of 31% of women commenced ANC in the first trimester.[21] This low prevalence of women who commence ANC in the first trimester from all the above studies seems to show a trend across SSA where women do not book early for ANC.
This study, however, did not identify any factors that could explain the tendency for women not to book early for ANC in the first trimester. All the sociodemographic factors assessed had no significant association with ANC attendance in the first trimester. Marital status, level of education, parity, gravidity, employment status, age and income levels did not have any influence on commencing ANC in the first trimester. Other studies in Cameroon however showed a relationship between optimal ANC and wealth, education, and place of residence.[6] In a study done in the Muea health area, a rural community in Cameroon, participants’ education level was shown to be a significant predictor for booking early for ANC services.[22] In Nigeria, ignorance and misconceptions of the purpose of, and right time to commence, ANC were the main reasons presented by a majority of the women for late booking for ANC.[23]
Overall, the study results suggest that total ANC attendance in the BRH is adequate (96%) with 20.5% of these women attending ANC in the first trimester. The prevalence of first trimester ANC attendance in the BRH is low. This calls for population health education amongst women of childbearing age emphasizing the need for continuous follow-up during pregnancy and early booking for ANC. Even though ANC attendance in the first trimester was not shown to influence late pregnancy outcomes in this study, further studies are neded to establish the benefits of this component of the Optimal ANC Package on early pregnancy outcomes in this suburban population.
Global Health Implications
Trends in sub-Saharan countries seem to suggest that most women do not attend first trimester ANC. Hence most regions do not satisfy the provision of adequate ANC proposed in the Optimal ANC Package. This could have negative consequences on overall perinatal outcomes in women and their children hence increasing morbidity and mortality. More user-friendly educational programs targeting women of childbearing age is required in such regions to address this situation.
Key Messages.
Overall antenatal care in the Buea Regional Hospital is adequate with 96% of women attending at least 1 ANC visit, and 60.2% of women attending at least 4 visits during pregnancy.
However only 20.5% of these women fulfill one of the components of Optimal Antenatal Care Package, that is ANC attendance in the first trimester.
ANC attendance in the first trimester when used alone was not a useful predictor of late pregnancy outcomes in this suburban population.
Trends around Subsaharan Africa suggest low ANC visits in the first trimester suggesting the need for more user-friendly educational programs for women of childbearing age.
Acknowledgements
The author is grateful to Dr. Julius Atashili for teaching him the basis of scientific writing.
Appendix
APPENDIX 1
SURVEY QUESTIONNAIRE
SECTION A: IDENTIFICATION
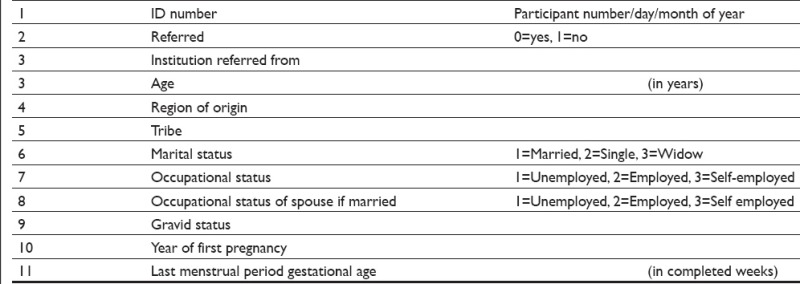
SECTION B: PAST MEDICAL HISTORY
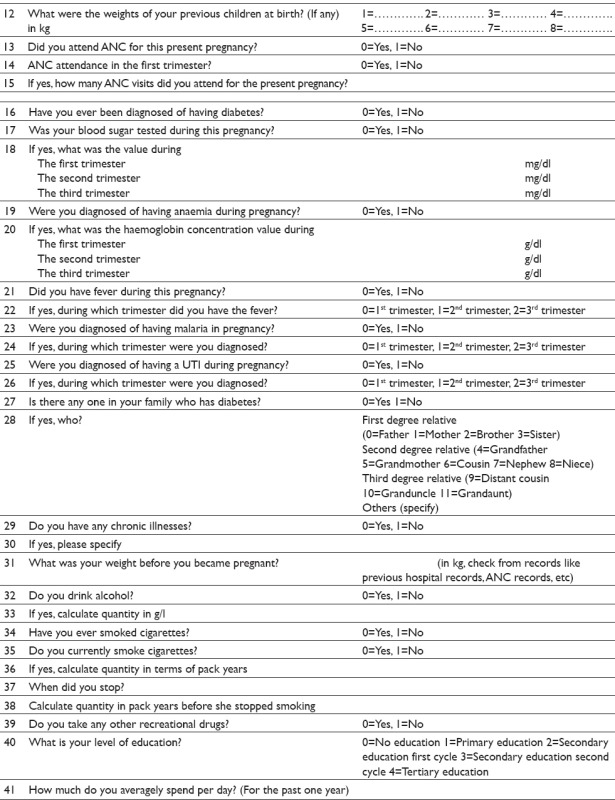
SECTION C: PHYSICAL EXAMINATION
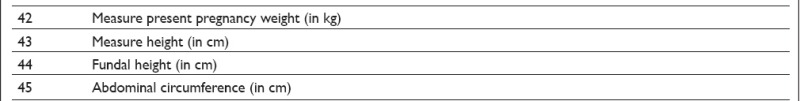
SECTION D: LABOUR PHASE
SECTION E: NEWBORN ASSESSMENT
SECTION F: MATERNAL ASSESSMENT
Footnotes
Conflict of Interest: The author declares no conflict of interests.
References
- 1.World Health Organisation. Trends in maternal mortality 1990 – 2010. Geneva, Switzerland: World Health Organisation; 2010. [Google Scholar]
- 2.Edie GE, Obinchemti TE, Tamufor EN, Njie MM, Njamen TN, Achidi EA. Perceptions of antenatal care services by pregnant women attending government health centres in the Buea Health District, Cameroon: a cross sectional study. Pan African Medical Journal. 2015;21:45. doi: 10.11604/pamj.2015.21.45.4858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United Nations. The Millennium Development Goals Report. New York, USA: United Nations; 2010. [Google Scholar]
- 4.Villar J, Ba’aqeel H, Piaggio G, Lumbiganon P, Miguel Belizan J, Farnot U, et al. WHO antenatal care randomised trial for the evaluation of a new model of routine antenatal care. Lancet. 2001;357(9268):1551–64. doi: 10.1016/s0140-6736(00)04722-x. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Antenatal care randomized trial: manual for implementation of the new model. Geneva: World Health Organisation; 2002. [Google Scholar]
- 6.Mbuagbaw LC, Gofin R. A new measurement for optimal antenatal care: determinants and outcomes in Cameroon. Maternal and Child Health Journal. 2011;15(8):1427–34. doi: 10.1007/s10995-010-0707-3. [DOI] [PubMed] [Google Scholar]
- 7.Carroli G, Villar J, Piaggio G, Khan-Neelofur D, Gulmezoglu M, Mugford M, et al. WHO systematic review of randomised controlled trials of routine antenatal care. Lancet. 2001;357(9268):1565–70. doi: 10.1016/S0140-6736(00)04723-1. [DOI] [PubMed] [Google Scholar]
- 8.Njim T, Atashili J, Mbu R, Choukem SP. Low birth weight in a sub-urban area of Cameroon: an analysis of the clinical cut-off, incidence, predictors and complications. BMC Pregnancy and Childbirth. 2015;15:288. doi: 10.1186/s12884-015-0723-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Okunlola MA, Owonikoko KM, Fawole AO, Adekunle AO. Gestational age at antenatal booking and delivery outcome. African Journal of Medicine and Medical Sciences. 2008;37(2):165–9. [PubMed] [Google Scholar]
- 10.Temple RC, Aldridge VJ, Murphy HR. Prepregnancy care and pregnancy outcomes in women with type 1 diabetes. Diabetes Care. 2006;29(8):1744–9. doi: 10.2337/dc05-2265. [DOI] [PubMed] [Google Scholar]
- 11.Lincetto O, Mothebesoane-Anoh S, Gomez P, Munjanja SP. Antenatal care. In: Joy L, Kate K, editors. Opportunities for Africa’s newborns: Practical data, policy and programmatic support for newborn care in Africa. Cape Town: PMNCH; 2006. [Google Scholar]
- 12.Nicolaides KH. Turning the pyramid of prenatal care. Fetal Diagnosis and Therapy. 2011;29(3):183–96. doi: 10.1159/000324320. [DOI] [PubMed] [Google Scholar]
- 13.Bonono RC, Ongolo-Zogo P. Optimizing the Use of Antenatal Care Services in Cameroon. Yaounde: Central Hospital Yaounde; 2012. [Google Scholar]
- 14.Buea District Health Service. Report of Health Activities in Buea Health District January to March 2010. Buea: Buea District Health Service; 2010. [Google Scholar]
- 15.Jimoh AA. Utilisation of antenatal services at the Provincial Hospital, Mongomo, Guinea Equatoria. African Journal of Reproductive Health. 2003;7(3):49–54. [PubMed] [Google Scholar]
- 16.van Eijk AM, Bles HM, Odhiambo F, Ayisi JG, Blokland IE, Rosen DH, et al. Use of antenatal services and delivery care among women in rural western Kenya: a community based survey. Reproductive Health. 2006;3:2. doi: 10.1186/1742-4755-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kambarami RA, Chirenje MZ, Rusakaniko S. Antenatal care patterns and factors associated with perinatal outcome in two rural districts in Zimbabwe. Central African Journal of Medicine. 1999;45(11):294–9. doi: 10.4314/cajm.v45i11.8503. [DOI] [PubMed] [Google Scholar]
- 18.Aluko JO, Oluwatosin A. Pattern and outcome of antenatal care among women attending a Catholic mission hospital in Ibadan, Nigeria. African Journal of Medicine and Medical Sciences. 2008;37(3):231–8. [PubMed] [Google Scholar]
- 19.National Statistical Office, ICF Macro. Malawi Demographic and Health Survey Final Report. Zomba, Malawi and ICF Macro, Calverton, Maryland, USA: NSO and ICF Macro; 2010. [Google Scholar]
- 20.Tann CJ, Kizza M, Morison L, Mabey D, Muwanga M, Grosskurth H, et al. Use of antenatal services and delivery care in Entebbe, Uganda: a community survey. BMC Pregnancy and Childbirth. 2007;7:23. doi: 10.1186/1471-2393-7-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ali AA, Osman MM, Abbaker AO, Adam I. Use of antenatal care services in Kassala, eastern Sudan. BMC Pregnancy and Childbirth. 2010;10:67. doi: 10.1186/1471-2393-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Halle-Ekane GE, Obinchemti TE, Nzang JN, Mokube NM, Njie MM, Njamen TN, et al. Assessment of the Content and Utilization of Antenatal Care Services in a Rural Community in Cameroon: A Cross-Sectional Study. Open Journal of Obstetrics and Gynecology. 2014;4:846–56. [Google Scholar]
- 23.Ebeigbe PN, Igberase GO. Reasons given by pregnant women for late initiation of antenatal care in the niger delta, Nigeria. Ghana Medical Journal. 2010;44(2):47–51. [PMC free article] [PubMed] [Google Scholar]


