Abstract
Objectives:
We examined the extent to which area- and individual-level socioeconomic inequalities in cardiovascular-disease (CVD), heart disease, and stroke mortality among United States men and women aged 25-64 years changed between 1969 and 2011.
Methods:
National vital statistics data and the National Longitudinal Mortality Study were used to estimate area- and individual-level socioeconomic gradients in mortality over time. Rate ratios and log-linear and Cox regression were used to model mortality trends and differentials.
Results:
Area socioeconomic gradients in mortality from CVD, heart disease, and stroke increased substantially during the study period. Compared to those in the most affluent group, individuals in the most deprived area group had, respectively 35%, 29%, and 73% higher CVD, heart disease, and stroke mortality in 1969, but 120-121% higher mortality in 2007-2011. Gradients were steeper for women than for men. Education, income, and occupation were inversely associated with CVD, heart disease, and stroke mortality, with individual-level socioeconomic gradients being steeper during 1990-2002 than in 1979-1989. Individuals with low education and incomes had 2.7 to 3.7 times higher CVD, heart disease, and stroke mortality risks than their counterparts with high education and income levels.
Conclusions and Global Health Implications:
Although mortality declined for all US groups during 1969-2011, socioeconomic disparities in mortality from CVD, heart disease and stroke remained marked and increased over time because of faster declines in mortality among higher socioeconomic groups. Widening disparities in mortality may reflect increasing temporal areal inequalities in living conditions, behavioral risk factors such as smoking, obesity and physical inactivity, and access to and use of health services. With social inequalities and prevalence of smoking, obesity, and physical inactivity on the rise, most segments of the working-age population in low- and middle-income countries will likely experience increased cardiovascular-disease burden in terms of higher morbidity and mortality rates.
Keywords: CVD mortality, Heart Disease, Stroke, Deprivation, SES, Work force
Introduction
Cardiovascular diseases (CVD), including heart disease and stroke, have been the leading cause of death in the United States for the past eight decades.[1] They currently account for almost a quarter of all deaths among working-age Americans, exceeded only by cancer.[1-3] Declines in the prevalence of key risk factors such as smoking have led to a 70% drop in CVD mortality among those aged 25-64.[1-3] Yet, substantial social inequalities in CVD mortality remain, with black Americans and those in lower socioeconomic groups continuing to experience higher CVD morbidity and mortality risks.[1-3]
Monitoring health inequalities and their social determinants is an essential step toward development and implementation of public policies to meet national health goals, such as achieving health equity.[4,5] Although time trends in age, sex, and racial/ethnic disparities in health outcomes are widely analyzed, monitoring health inequalities, particularly those in mortality, by socioeconomic status (SES), is relatively uncommon in the US.[1-3,6-8] This is primarily because the national mortality database contains limited and unreliable socioeconomic data for the decedents, which makes it difficult to compute mortality rates by socioeconomic characteristics.[2,3,7,8] However, linkages of national mortality data with census data at an area level, such as at the county level, have allowed several US studies to examine differentials in CVD mortality according to area-based socioeconomic deprivation level.[6-10] Moreover, prospective linkages of census and current population survey records with national death records have permitted estimation of mortality differentials by individual-level SES characteristics such as education, income, and occupation.[11-14]
Health inequalities in the working-age population are generally greater than those in the general population.[7,8,14,15] Compared to the general population, those in the prime working ages between 25 and 64 years are much more vulnerable to adverse social conditions such as unemployment, marital disruption, lack of labor market opportunities, economic recession, inadequate housing, unfavorable work environment, lack of autonomy and control in the workplace, low job satisfaction, high job stress, and low social support.[8,16] These adverse social conditions are associated with increased risks of adult premature mortality, particularly due to cardiovascular conditions.[8,16] Few studies have explored temporal socioeconomic disparities in all-cause and cause-specific mortality among working-age populations in the US.[7,8] A previous analysis showed marked and increasing inequalities in CVD mortality by deprivation levels among Americans aged 25-64 between 1969 and 1998.[8] The present study extends and updates that analysis by examining area socioeconomic disparities in CVD mortality from 1969 through 2011. Unlike the previous analysis, we also analyze temporal socioeconomic patterns in mortality from two main component causes, heart disease and stroke. Additionally, we estimate changes in individual-level socioeconomic inequalities in CVD, heart disease, and stroke mortality among working-age Americans between 1979 and 2002 using national longitudinal data. Temporal analysis allows us to track progress toward reducing health inequalities among those at higher risks of morbidity and mortality. It also provides important insights into the role of health-policy and medical interventions and behavioral risk factors such as such as smoking, obesity, physical inactivity, and unhealthy diet.[5,7,8]
Methods
Use of National Vital Statistics and Census Databases to Compute Mortality Rates by Deprivation Level
To analyze temporal inequalities in CVD mortality, we used the national vital statistics mortality database.[1-3,17] Since the vital-statistics-based national mortality database lacks reliable SES data, socioeconomic patterns in CVD mortality were derived by linking the 1990 and 2000 census-based county-level deprivation indices to the age-sex-race-county-specific mortality statistics from 1969 through 2011.[7,8,15,18]
Area Deprivation Indices for the United States
We used previously published factor-based deprivation indices from the 1990 and 2000 decennial US censuses.[7,8,18] The 1990 deprivation index consisted of 17 census-based socioeconomic indicators, which may be viewed as broadly representing educational opportunities, labor force skills, economic, and housing conditions in a given county.[7,8] Selected indicators of education, occupation, wealth, income distribution, unemployment rate, poverty rate, and housing quality were used to construct the 1990 index.[7,8] The factor loadings (correlations of indicators with the index) for the 1990 index ranged from 0.92 for 150% of the poverty rate to 0.45 for household plumbing.[7,8] The 2000 deprivation index consisted of 22 socioeconomic indicators, including five additional measures of income distribution, wealth, and housing quality.[18] The factor loadings for the 2000 index varied from 0.92 for 150% of the poverty rate to 0.39 for household plumbing.[18] The common indicators in the 1990 and 2000 deprivation indices generally had similar factor loadings or relative weights.[7,8,18] The correlation between the 1990 and 2000 deprivation indices was 0.97, indicating a fairly stable geographical distribution of deprivation in the US over time. Substantive and methodological details of the US deprivation indices are provided elsewhere.[7,8,18]
In order to compute mortality rates by deprivation level, we used the weighted population quintile distribution of the deprivation index that classified all 3,141 US counties into 5 groups of approximately equal population size.[7,8,18] The groups thus created ranged from being the most-deprived (first quintile) to the least-disadvantaged (fifth quintile) population groups.[7,8,18] Each of the 3,141 counties in the mortality database was assigned one of the 5 deprivation quintiles. The 1990 index was used to compute deprivation-specific mortality rates from 1969 to 1998, whereas the 2000 index was used to compute mortality rates by deprivation level from 1999 to 2011.
Cause-specific mortality rates according to county deprivation levels were computed annually between 1969 and 1998 and for the following time periods: 1999-2001, 2002-2006, and 2007-2011. Our trend analysis included 7,374,628 CVD deaths, 6,084,622, heart disease deaths, and 960,673 stroke deaths that occurred among those aged 25-64 between 1969 and 2011.
Mortality rates for each area- and individual-level socioeconomic group were age-adjusted by the direct method using the age-composition of the 2000 US population as the standard.[1-3,7,8,19,20] Log-linear regression models were used to estimate annual rates of decrease in cause-specific mortality for race, sex, and deprivation groups.[7,8,15] Specifically, the logarithm of mortality rates were modeled as a linear function of time (calendar year), which yielded annual exponential rates of change in mortality rates.[7,8,15] Disparities in mortality by deprivation level were described by rate ratios (relative risks) and rate differences (absolute inequalities), which were tested for statistical significance at the 0.05 level.
National Longitudinal Mortality Study (NLMS)
To examine variations in CVD, heart disease, and stroke mortality risks according to individual-level socioeconomic characteristics, we used the 1979-2002 NLMS data. The NLMS is a longitudinal dataset for examining socioeconomic, occupational, and demographic factors associated with all-cause and cause-specific mortality in the United States.[11-14,21] The NLMS is conducted by the National Heart, Lung, and Blood Institute (National Institutes of Health [NIH]) in collaboration with the US Census Bureau, the National Cancer Institute (NIH), the National Institute on Aging (NIH), and the National Center for Health Statistics (Centers for Disease Control and Prevention).[11-14,21] The NLMS consists of 30 Current Population Survey (CPS) and census cohorts between 1973 and 2002 whose survival (mortality) experiences were studied between 1979 and 2002.[21] The CPS is a sample household and telephone interview survey of the civilian non-institutionalized population in the United States and is conducted by the US Census Bureau to produce monthly national statistics on unemployment and the labor force. Data from death certificates on the fact of death and the cause of death are combined with the socioeconomic and demographic characteristics of the NLMS cohorts by means of the National Death Index.[11-14,21] Detailed descriptions of the NLMS have been provided elsewhere.[12,13,21]
The full NLMS consists of approximately 3 million individuals drawn from 30 CPS and census cohorts whose mortality experience has been followed from 1979 through 2002, with the total number of deaths during the 23-year follow-up being 341,343.[21] For this study, we used the public-use NLMS file to derive cohort-based mortality risks during 1979-1989 and 1990-2002.[21] The two sets of CPS cohorts in the 1980s and 1990s were considered for a maximum mortality follow-up of 6 years.[21] Education, income/poverty level, and occupational differentials in mortality risks were adjusted by multivariate Cox proportional hazards regression for age and for additional covariates such as sex, race/ethnicity, marital status, and place of residence.[11,22] The NLMS sample for 1979-1989 included 513,991 individuals at the baseline and 5,668 CVD deaths, 4,792 heart disease deaths, and 646 stroke deaths during the 6-year mortality follow-up. The 1990-2002 sample included 305,794 individuals at the baseline and 2,336 CVD deaths, 1,962 heart disease deaths, and 268 stroke deaths during the 6-year mortality follow-up. In estimating the mortality risk, all those surviving beyond the 6-year follow-up (measured in days) and those dying from causes other than CVD, heart disease, or stroke during the follow-up period were treated as right-censored observations. The Cox models were estimated by the SAS PHREG procedure.[22]
Results
Changes in Leading Causes of Death among Working-Age Americans
In 1969, cardiovascular diseases were the leading cause of death among both men and women in the US. Due to a considerable decline in CVD mortality and a slower decrease in cancer mortality during 1969-2011, cancer overtook CVD as the leading cause of death among Americans aged 25-64 (Table 1). In 2011, the leading causes of death among men aged 25-64 were cardiovascular disease, cancer, unintentional injuries, suicide, and liver cirrhosis. For working-age women, the leading causes of death were cancer, cardiovascular disease, unintentional injuries, COPD, and diabetes. CVD remains the leading cause of death among US blacks aged 25-64 despite the steep decline in mortality over the past 4 decades.
Table 1.
Number of Deaths and Age-Adjusted Death Rates from Leading Causes of Death Among the Working-Age Population (25-64 years), United States, 1969 and 2011
| Deaths | Death rate | Deaths | Death rate | Deaths | Death rate | Percent | Percent | Percent | |
|---|---|---|---|---|---|---|---|---|---|
| Both sexes | Both sexes | Male | Male | Female | Female | Both sexes | Male | Female | |
| 1969 | |||||||||
| All causes of death | 587,562 | 606.7 | 379,442 | 815.8 | 208,120 | 414.7 | 100.0 | 100.0 | 100.0 |
| All cancers combined | 135,752 | 138.6 | 71,665 | 150.9 | 64,087 | 127.7 | 23.1 | 18.9 | 30.8 |
| HIV/AIDS | 0.0 | 0.0 | 0.0 | ||||||
| Diabetes mellitus | 11,655 | 11.8 | 5,561 | 12.0 | 6,094 | 11.7 | 2.0 | 1.5 | 2.9 |
| Major cardiovascular diseases (CVD) | 242,667 | 243.7 | 170,563 | 359.3 | 72,104 | 138.1 | 41.3 | 45.0 | 34.6 |
| Heart disease | 196,594 | 197.1 | 144,511 | 304.6 | 52,083 | 98.8 | 33.5 | 38.1 | 25.0 |
| Stroke | 35,835 | 36.3 | 19,393 | 40.8 | 16,442 | 32.2 | 6.1 | 5.1 | 7.9 |
| Pneumonia and influenza | 14,412 | 15.0 | 9,064 | 19.6 | 5,348 | 10.8 | 2.5 | 2.4 | 2.6 |
| COPD | 10,921 | 10.7 | 8,179 | 16.7 | 2,742 | 5.4 | 1.9 | 2.2 | 1.3 |
| Chronic liver disease and cirrhosis | 22,594 | 24.5 | 14,704 | 32.9 | 7,890 | 16.7 | 3.8 | 3.9 | 3.8 |
| Nephritis and kidney diseases | 5,025 | 5.3 | 2,899 | 6.4 | 2,126 | 4.3 | 0.9 | 0.8 | 1.0 |
| Accidents and adverse effects | 48,602 | 53.7 | 36,744 | 84.1 | 11,858 | 25.2 | 8.3 | 9.7 | 5.7 |
| Suicide and self-inflicted injury | 15,367 | 17.1 | 10,479 | 24.0 | 4,888 | 10.7 | 2.6 | 2.8 | 2.3 |
| Homicide and legal intervention | 10,205 | 11.7 | 8,156 | 19.2 | 2,049 | 4.6 | 1.7 | 2.1 | 1.0 |
| 2011 | |||||||||
| All causes of death | 620,203 | 326.6 | 381,650 | 411.6 | 238,553 | 244.9 | 100.0 | 100.0 | 100.0 |
| All cancers combined | 176,685 | 87.9 | 93,618 | 94.3 | 83,067 | 82.0 | 28.5 | 24.5 | 34.8 |
| HIV/AIDS | 6,862 | 4.1 | 4,900 | 5.8 | 1,962 | 2.4 | 1.1 | 1.3 | 0.8 |
| Diabetes mellitus | 21,228 | 10.8 | 12,875 | 13.4 | 8,353 | 8.3 | 3.4 | 3.4 | 3.5 |
| Major cardiovascular diseases (CVD) | 147,751 | 75.5 | 100,251 | 105.0 | 47,500 | 47.3 | 23.8 | 26.3 | 19.9 |
| Heart disease | 119,778 | 61.2 | 83,682 | 87.7 | 36,096 | 35.9 | 19.3 | 21.9 | 15.1 |
| Stroke | 19,158 | 9.8 | 10,796 | 11.3 | 8,362 | 8.4 | 3.1 | 2.8 | 3.5 |
| Pneumonia and influenza | 7,783 | 4.1 | 4,464 | 4.8 | 3,319 | 3.4 | 1.3 | 1.2 | 1.4 |
| COPD | 20,680 | 9.9 | 10,560 | 10.3 | 10,120 | 9.5 | 3.3 | 2.8 | 4.2 |
| Chronic liver disease and cirrhosis | 22,567 | 12.0 | 15,335 | 16.5 | 7,232 | 7.7 | 3.6 | 4.0 | 3.0 |
| Nephritis and kidney diseases | 7,618 | 3.8 | 4,369 | 4.5 | 3,249 | 3.2 | 1.2 | 1.1 | 1.4 |
| Accidents and adverse effects | 66,655 | 40.1 | 46,243 | 56.2 | 20,412 | 24.3 | 10.7 | 12.1 | 8.6 |
| Suicide and self-inflicted injury | 28,078 | 16.9 | 21,561 | 26.2 | 6,517 | 7.8 | 4.5 | 5.6 | 2.7 |
| Homicide and legal intervention | 10,214 | 6.5 | 8,091 | 10.3 | 2,123 | 2.7 | 1.6 | 2.1 | 0.9 |
Death rates are directly standardized to the 2000 US standard population. COPD=Chronic Obstructive Pulmonary Diseases
Area Socioeconomic Trends in CVD, Heart Disease, and Stroke Mortality
Area socioeconomic gradients (rate ratios) in CVD, heart disease, and stroke mortality increased substantially during 1969-2011 (Figure 1). Compared to those in the most-affluent group, individuals in the most-deprived area group had, respectively 35%, 29%, and 73% higher CVD, heart disease, and stroke mortality in 1969, but 120-121% higher mortality in 2007-2011 (Figures 1 and 2). Socioeconomic gradients in mortality were steeper for women than for men; in 2007-2011, women had 2.5, 2.6, and 2.2 times higher CVD, heart disease, and stroke mortality, respectively, in the most-deprived group than in the most-affluent group. During 1969-2011, even though CVD mortality rates decreased by at least 59% for all deprivation groups, more deprived groups had higher CVD mortality than less deprived groups in each year/time-period (Figure 3). Cause-specific mortality declined at a much faster pace among individuals in the most affluent group than those in more deprived groups. During 1969-2011, CVD mortality in the five most-to-least deprived groups decreased at average annual rates of 2.25%, 2.71%, 2.79%, 3.10%, and 3.55%, respectively. The corresponding annual rates of decline in heart disease mortality among 5 deprivation groups were: 2.18%, 2.71%, 2.78%, 3.12%, and 3.61% and in stroke mortality: 2.89%, 3.02%, 3.13%, 3.22%, and 3.51%. In the past 4 decades, absolute socioeconomic disparities in CVD and heart disease mortality, as measured by rate differences between the most and least deprived quintiles, have remained stable, while those in stroke mortality have decreased.
Figure 1.
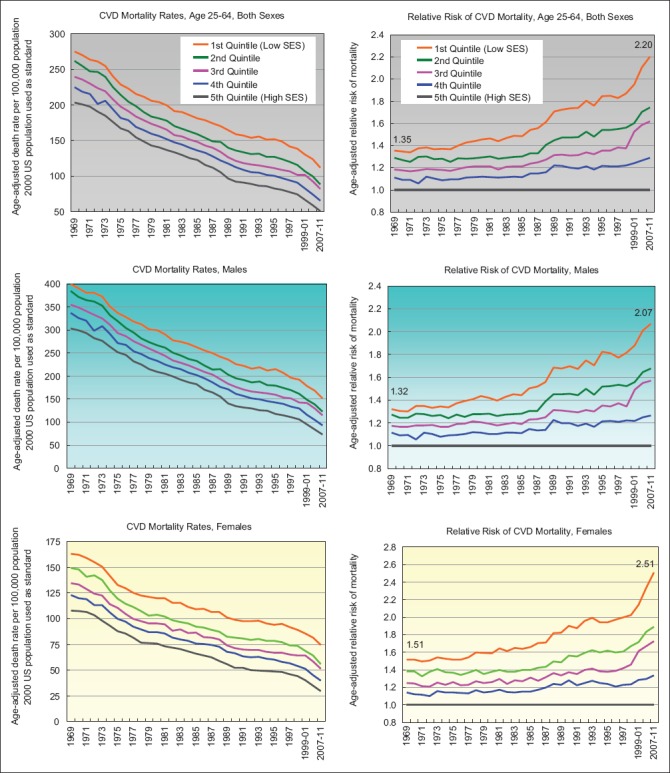
Cardiovascular Disease (CVD) Mortality Among US Population Aged 25-64 Years by Area Socioeconomic Deprivation Index, 1969-2011
Figure 2.
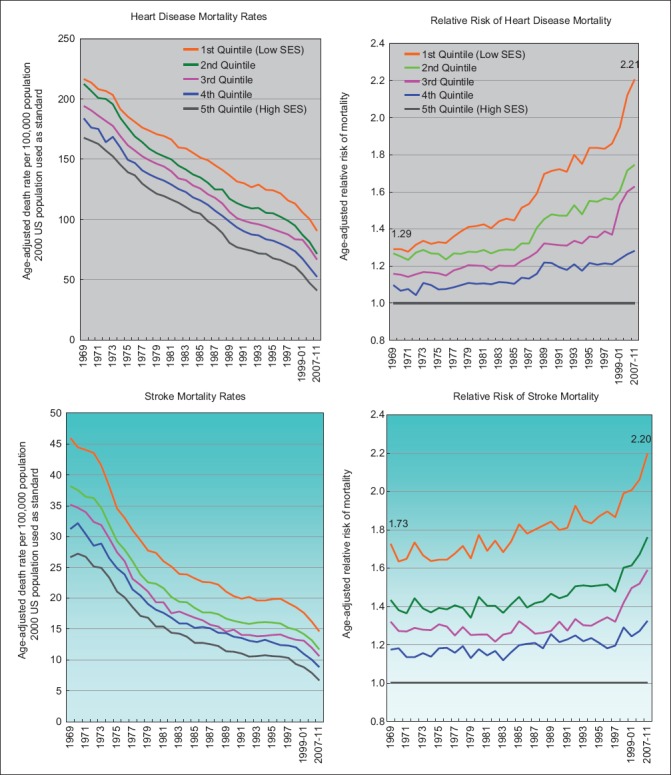
Heart Disease and Stroke Mortality Among US Population Aged 25-64 Years by Area Socioeconomic Deprivation Index, 1969-2011
Figure 3.
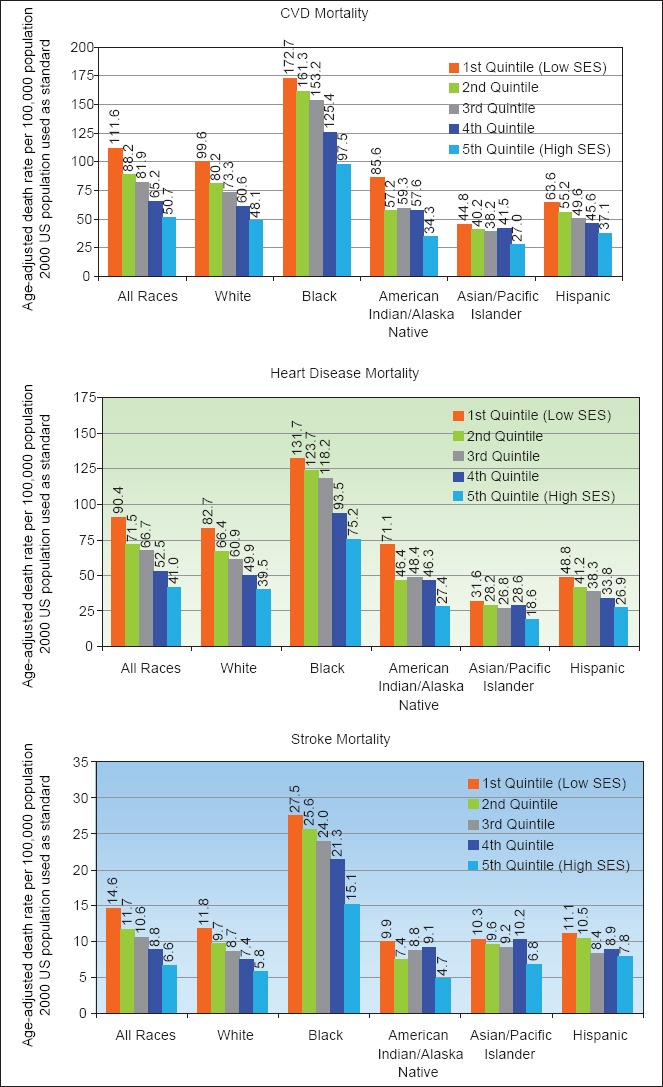
Cardiovascular Disease (CVD), Heart Disease, and Stroke Mortality by Race/Ethnicity and Socioeconomic Deprivation Level, United States, 2007-2011
CVD, heart disease, and stroke mortality rates decreased with decreasing levels of deprivation for both white and black populations aged 25-64, with socioeconomic gradients in CVD and heart disease mortality increasing consistently during 1969-2011 for both racial groups (data not shown for brevity). Ratio of CVD mortality between the most and least deprived quintiles increased from 1.20 in 1969 to 2.07 in 2007-2011 for whites and from 1.31 to 1.77 for blacks during 1969-2011. Similarly, the inequality ratio for stroke mortality during 1969-2011 increased from 1.26 to 2.05 for whites and from 1.55 to 1.82 for blacks. Absolute socioeconomic inequalities in CVD and heart disease mortality also widened over time for whites, but not for blacks.
Marked socioeconomic gradients in mortality existed not only for white and black Americans but also for the other major racial/ethnic groups: American Indians/Alaska Natives (AIANs), Asians/Pacific Islanders (APIs), and Hispanics (Figure 3). During 2007-2011, heart disease mortality rates varied from a low of 18.58 deaths per 100,000 population for APIs in the least-deprived group to a high of 131.74 for blacks in the most-deprived group. Stroke mortality rates ranged from 4.71 for the most-affluent AIANs to 27.47 for the most-deprived blacks. Whites, blacks, AIANs, APIs, and Hispanics had, respectively, 2.09, 1.75, 2.60, 1.70, and 1.82 times higher heart disease mortality in the most deprived group than in the least-deprived group. Ethnic-specific deprivation gradients were similar in stroke mortality (Figure 3).
Trends in Individual-Level Socioeconomic Disparities in CVD, Heart Disease and Stroke Mortality
Table 2 shows changes in cause-specific mortality risks according to individual-level baseline socioeconomic characteristics in the NLMS. Education, income, and occupation were inversely associated with mortality among those aged 25-64, with individual-level age-adjusted socioeconomic disparities being more marked during 1990-2002 than during 1979-1989. During 1990-2002, individuals with low education and incomes had 2.7 to 3.7 times higher age-adjusted CVD, heart disease, and stroke mortality risks than their counterparts with high education and income levels. Occupational inequalities were more pronounced for stroke than heart disease and somewhat greater in 1990-2002 than in 1979-1989. In 1990-2002, those in non-professional jobs had 81% higher age-adjusted risk of stroke and 47% higher risk of heart disease than those employed in professional and managerial jobs. Unemployed individuals were about twice as likely to die from heart disease and stroke as their employed counterparts. In covariate-adjusted models, education and income were independently related to CVD, heart disease, and stroke mortality although their effects were somewhat attenuated (Table 1). No occupational differentials were found after adjusting for covariates, although unemployed individuals maintained twice the mortality risk of CVD than their employed counterparts.
Table 2.
Age- and Covariate-Adjusted Relative Risks of Cardiovascular Disease (CVD), Heart Disease, and Stroke Mortality Among US Adults Aged 25-64 Years According to Baseline Socioeeconomic Characteristics: The US National Longitudinal Mortaliy Study, 1979-2002
| Baseline socioeconomic characteristics | 1979-1989 (N=513,991) | 1990-2002 (N=305,794) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age-adjusted1 | Covariate-adjusted2 | Age-adjusted1 | Covariate-adjusted2 | |||||||||
| Hazard ratio | 95% CI | Hazard ratio | 95% CI | Hazard ratio | 95% CI | Hazard ratio | 95% CI | |||||
| Cardiovascular diseases | ||||||||||||
| Education (years) | ||||||||||||
| <12 | 2.21 | 1.93 | 2.54 | 1.76 | 1.51 | 2.05 | 2.79 | 2.28 | 3.42 | 1.94 | 1.55 | 2.44 |
| 12 | 1.44 | 1.25 | 1.65 | 1.50 | 1.29 | 1.74 | 1.89 | 1.55 | 2.31 | 1.67 | 1.34 | 2.08 |
| 13-15 | 1.38 | 1.18 | 1.61 | 1.41 | 1.20 | 1.66 | 1.63 | 1.32 | 2.02 | 1.48 | 1.18 | 1.86 |
| 16 | 1.06 | 0.89 | 1.26 | 1.09 | 0.91 | 1.30 | 1.07 | 0.84 | 1.37 | 1.03 | 0.81 | 1.32 |
| 17+ | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | ||||
| Occupation | ||||||||||||
| Professional/managerial | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | ||||
| Non-professional | 1.24 | 1.14 | 1.35 | 0.96 | 0.87 | 1.06 | 1.51 | 1.32 | 1.72 | 1.05 | 0.90 | 1.21 |
| Unemployed/outside labor force | 1.87 | 1.72 | 2.04 | 1.89 | 1.70 | 2.09 | 2.62 | 2.29 | 3.00 | 1.97 | 1.68 | 2.30 |
| Poverty status (ratio of family income to poverty threshold) | ||||||||||||
| Below 100% | 2.81 | 2.54 | 3.12 | 1.76 | 1.56 | 1.98 | 2.93 | 2.53 | 3.40 | 1.67 | 1.41 | 1.98 |
| 100-149% | 2.14 | 1.90 | 2.40 | 1.52 | 1.34 | 1.72 | 2.59 | 2.19 | 3.05 | 1.62 | 1.35 | 1.94 |
| 150-199% | 2.02 | 1.81 | 2.27 | 1.54 | 1.37 | 1.74 | 2.26 | 1.91 | 2.66 | 1.55 | 1.30 | 1.86 |
| 200-299% | 1.65 | 1.49 | 1.83 | 1.36 | 1.22 | 1.51 | 1.71 | 1.48 | 1.99 | 1.28 | 1.09 | 1.49 |
| 300-399% | 1.52 | 1.37 | 1.70 | 1.31 | 1.17 | 1.46 | 1.61 | 1.38 | 1.87 | 1.27 | 1.09 | 1.49 |
| 400-599% | 1.30 | 1.17 | 1.45 | 1.17 | 1.05 | 1.31 | 1.20 | 1.03 | 1.39 | 1.04 | 0.89 | 1.21 |
| At or above 600% | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | ||||
| Heart disease | ||||||||||||
| Education (years) | ||||||||||||
| <12 | 2.09 | 1.80 | 2.42 | 1.72 | 1.46 | 2.03 | 2.69 | 2.16 | 3.35 | 1.92 | 1.51 | 2.46 |
| 12 | 1.38 | 1.19 | 1.60 | 1.47 | 1.25 | 1.73 | 1.87 | 1.51 | 2.32 | 1.70 | 1.34 | 2.15 |
| 13-15 | 1.30 | 1.11 | 1.54 | 1.36 | 1.14 | 1.62 | 1.63 | 1.29 | 2.05 | 1.52 | 1.19 | 1.94 |
| 16 | 1.01 | 0.84 | 1.22 | 1.05 | 0.87 | 1.27 | 1.04 | 0.79 | 1.35 | 1.01 | 0.77 | 1.32 |
| 17+ | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | ||||
| Occupation | ||||||||||||
| Professional/managerial | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | ||||
| Non-professional | 1.21 | 1.11 | 1.33 | 0.95 | 0.86 | 1.06 | 1.47 | 1.27 | 1.70 | 1.02 | 0.87 | 1.20 |
| Unemployed/outside labor force | 1.77 | 1.61 | 1.95 | 1.84 | 1.65 | 2.06 | 2.61 | 2.25 | 3.02 | 2.02 | 1.71 | 2.40 |
| Poverty status (ratio of family income to poverty threshold) | ||||||||||||
| Below 100% | 2.73 | 2.44 | 3.06 | 1.78 | 1.57 | 2.03 | 2.84 | 2.42 | 3.34 | 1.66 | 1.38 | 2.00 |
| 100-149% | 2.13 | 1.88 | 2.42 | 1.57 | 1.37 | 1.79 | 2.67 | 2.23 | 3.19 | 1.68 | 1.38 | 2.05 |
| 150-199% | 2.01 | 1.77 | 2.27 | 1.56 | 1.37 | 1.78 | 2.24 | 1.87 | 2.68 | 1.56 | 1.29 | 1.90 |
| 200-299% | 1.63 | 1.45 | 1.82 | 1.36 | 1.21 | 1.53 | 1.70 | 1.45 | 2.00 | 1.28 | 1.08 | 1.52 |
| 300-399% | 1.54 | 1.37 | 1.74 | 1.34 | 1.18 | 1.51 | 1.58 | 1.34 | 1.87 | 1.26 | 1.06 | 1.49 |
| 400-599% | 1.32 | 1.18 | 1.48 | 1.19 | 1.06 | 1.34 | 1.22 | 1.03 | 1.43 | 1.05 | 0.89 | 1.24 |
| At or above 600% | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | ||||
| Stroke | ||||||||||||
| Education (years) | ||||||||||||
| <12 | 3.17 | 1.99 | 5.05 | 2.12 | 1.27 | 3.54 | 3.17 | 1.69 | 5.95 | 1.72 | 0.86 | 3.47 |
| 12 | 1.91 | 1.20 | 3.05 | 1.71 | 1.03 | 2.84 | 2.22 | 1.19 | 4.13 | 1.52 | 0.77 | 2.99 |
| 13-15 | 1.98 | 1.20 | 3.28 | 1.81 | 1.07 | 3.06 | 1.81 | 0.94 | 3.50 | 1.34 | 0.67 | 2.69 |
| 16 | 1.13 | 0.63 | 2.03 | 1.10 | 0.61 | 2.00 | 1.44 | 0.70 | 2.98 | 1.27 | 0.61 | 2.65 |
| 17+ | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | ||||
| Occupation | ||||||||||||
| Professional/managerial | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | ||||
| Non-professional | 1.47 | 1.11 | 1.94 | 1.03 | 0.75 | 1.40 | 1.81 | 1.21 | 2.71 | 1.28 | 0.82 | 2.02 |
| Unemployed/outside labor force | 2.70 | 2.04 | 3.57 | 2.16 | 1.57 | 2.98 | 2.90 | 1.92 | 4.40 | 1.82 | 1.13 | 2.93 |
| Poverty status (ratio of family income to poverty threshold) | ||||||||||||
| Below 100% | 3.27 | 2.42 | 4.42 | 1.53 | 1.08 | 2.16 | 3.74 | 2.44 | 5.74 | 2.10 | 1.27 | 3.47 |
| 100-149% | 1.96 | 1.38 | 2.80 | 1.12 | 0.77 | 1.64 | 2.06 | 1.20 | 3.55 | 1.34 | 0.75 | 2.41 |
| 150-199% | 1.75 | 1.24 | 2.48 | 1.13 | 0.78 | 1.62 | 2.82 | 1.75 | 4.56 | 1.97 | 1.18 | 3.29 |
| 200-299% | 1.76 | 1.30 | 2.38 | 1.27 | 0.92 | 1.74 | 1.95 | 1.26 | 3.02 | 1.47 | 0.93 | 2.35 |
| 300-399% | 1.45 | 1.04 | 2.01 | 1.13 | 0.81 | 1.59 | 1.53 | 0.96 | 2.44 | 1.23 | 0.76 | 2.00 |
| 400-599% | 1.18 | 0.86 | 1.62 | 1.01 | 0.73 | 1.39 | 1.24 | 0.78 | 1.95 | 1.08 | 0.68 | 1.72 |
| At or above 600% | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | ||||
Notes: Relative risks (hazard ratios) were derived from multivariate Cox proportional hazards regression models.
Adjusted for age only.
Adjusted for age, sex, race/ethnicity, marital status, metropolitan/non-metropolitan residence educational attainment, occupation, and income/poverty level
Discussion
Cardiovascular disease, heart disease, and stroke mortality rates have decreased substantially for all socioeconomic groups in the US. Against this backdrop of impressive declines in overall mortality rates, our study shows substantial and increasing socioeconomic disparities in CVD, heart disease, and stroke mortality over time, as relative inequalities in mortality among those aged 25-64 widened consistently between 1969 and 2011. Between 1969 and 2011, those in more affluent groups experienced faster declines in mortality than those in more deprived groups, which contributed to the widening socioeconomic gap in CVD, heart disease, and stroke mortality. Absolute inequalities in CVD and heart disease mortality, however, remained stable in the past 4 decades.
Socioeconomic inequalities in CVD, heart disease, and stroke mortality among the working-age population shown here are substantially greater than those for the overall US population as reported in the companion paper.23 Such age-related patterns in socioeconomic inequalities in health and mortality have also been noted for other industrialized countries.[7,8,24] Several hypotheses have been proposed for these patterns. First, disparities in social conditions such as education, income, wealth, unemployment, and housing and in risk factors such as smoking, physical inactivity, obesity, unhealthy diet, alcohol consumption, and hypertension tend to be more pronounced among those aged 25-64 than in the general population or among the elderly.[3,8,24] Secondly, according to the differential selection hypothesis, individuals from the most deprived groups who survive into older ages (i.e., beyond age 65) represent an elite group who tend be healthier than their disadvantaged counterparts who perish earlier in life.[24] As a consequence, this tends to have a narrowing effect on social inequalities in mortality at older ages, all else being equal. The third hypothesis is that, the existence of social insurance programs in the industrialized world such as Medicare and Social Security programs for elderly and retired individuals reduces social inequalities in living conditions, material wealth, and access to high-quality medical care, leading to narrower health inequalities in older ages.[24] Whether a similar social patterning in cardiovascular-disease mortality among working-age adults and elderly exists in developing countries needs to be investigated. Individuals, especially those of retirement ages, in most low- and middle-income countries do not have access to universal health insurance or social security programs, but they might enjoy greater levels of social support and integration (a major positive determinant of health) than their counterparts in the industrialized world.
Increasing socioeconomic disparities in CVD mortality shown here are consistent with those observed previously for the United States and Europe.[8,11,25-29] In Britain, the gap in coronary heart disease mortality among those under age 65 between the most and least deprived deciles widened between 1981 and 1995.[27] Another study showed increasing social class inequalities in CVD mortality among men aged 15-64 in England and Wales and in Scotland during 1951-1981.[28] A recent UK government study showed a widening of the social-class gradient in stroke mortality among English men aged 35-64, with the ratio between the lowest and highest social classes increasing from 1.34 in 1986-1992 to 2.67 in 1997-1999 to 2.90 in 2001-2003.[29] Similarly, the relative inequality in ischemic heart disease mortality between the lowest and highest social classes for English men in working ages increased from 1.69 in 1986-1992 to 2.90 in 2001-2003.[29] Like the United States, the relative gap in heart disease and stroke mortality in England widened as mortality rates fell more rapidly in higher social classes.[29] However, for Canada, although mortality rates were higher in poorer neighborhoods, both absolute and relative socioeconomic inequalities in ischemic heart disease mortality diminished between 1971 and 1996, particularly among males.[30]
Socioeconomic disparities in CVD mortality may reflect differences in smoking prevalence, unhealthy diet, obesity, physical inactivity, and healthcare factors.[3,7-10,31] Higher smoking rates are more prevalent among US men and women in lower socioeconomic groups and in more deprived areas.[3,7,8,32] Smoking rates have fallen more rapidly for those in higher socioeconomic groups in the US, which largely explains temporal socioeconomic trends in CVD mortality rates.[3,8] Obesity prevalence is higher in lower socioeconomic groups, and social-class gradients in US obesity rates have persisted for the past 4 decades.[3,33] Higher consumption of lower-quality diets and energy-dense foods and lower intakes of fruits and vegetables have been reported among lower socioeconomic groups in the US.[3,33] Socioeconomic differences in these dietary factors have persisted or narrowed over time.[3,33]
Marked socioeconomic disparities in CVD mortality reported here are consistent with those reported in prevalence of heart disease, stroke, and hypertension in the US.[3,32] In 2012, those with less than a high school education had 88%, 150%, and 47% higher risk of coronary heart disease, stroke, and hypertension respectively than those with a college degree.[32] Similarly, substantially higher prevalence of heart disease, stroke, and hypertension is reported among unemployed and low-income Americans.[32]
Conclusions and Global Health Implications
With social inequalities and prevalence of smoking, obesity, physical inactivity, and westernization of diet on the rise, most segments of the working-age population in low- and middle-income countries will likely experience increased cardiovascular-disease burden in terms of higher morbidity and mortality rates. [31,34] Cardiovascular disease is the leading cause of death not only in the industrialized world, but also in low- and middle-income countries.[31,35,36] Over 14 million premature deaths from CVD and other non-communicable diseases (NCDs) such as cancer and diabetes occur globally between the ages of 30 and 70, of which 85% are in developing countries.[37] Most of these deaths are preventable through policy measures that are aimed at reducing behavioral risk factors such as smoking, physical inactivity, unhealthy diet, and heavy drinking that account for about 80% of cardiovascular diseases globally.[31]
Cardiovascular disease is projected to be an even bigger health concern in the developing world.[35] Cardiovascular-disease burden varies greatly across the world regions, with the largest number of deaths occurring in India and China, which together account for >30% of all CVD deaths in the world. The following countries have the highest disease burden (in terms of number of heart disease deaths): US and Germany among high-income countries; China and Indonesia in the East Asia and Pacific region; Russia and Ukraine in Europe and Central Asia; Brazil and Mexico in Latin America and the Caribbean; India and Pakistan in South Asia; and Nigeria and Ethiopia in Sub-Saharan Africa.[36] Economic and workforce implications of rising CVD morbidity and mortality risks in developing countries are profound. Many of the CVD deaths among people in low- and middle-income countries occur at younger ages, often in their most productive years in the labor force; the macro-economic effect of NCDs including CVD is a reduction of 6.8% in these countries’ GDPs.[31] Additionally, because of macro-societal forces, such as globalization and urbanization, people in developing countries are increasingly being exposed to such CVD risk factors as smoking, drinking, physical inactivity, and unhealthy diet. At the same time, they do not have similar access to public health education and prevention programs and access to primary care as their counterparts in the industrialized world.[31] In the absence of universal healthcare coverage, poorer people with CVDs in developing countries are disproportionately burdened with high out-of-pocket expenditure, which contributes to even greater economic hardship among them.[31]
In conclusion, we must state that much progress has been made to reduce CVD, heart disease, and stroke mortality among all socioeconomic groups in the US workforce. However, the growing socioeconomic disparities in CVD, heart disease, and stroke mortality must be seen as a major public health concern; these disparities in mortality may partly indicate that the benefits of CVD prevention and control have not reached all groups equally.[8,31] Heart disease and stroke continue to disproportionately affect those who are unemployed and socioeconomically disadvantaged in the US workforce. The underlying social determinants of these health inequalities must be addressed.[8,16,29,31] Tackling poverty, improving education, employment and labor market opportunities, reducing smoking prevalence and harmful use of alcohol, promoting and increasing opportunities for physical activity and access to a healthy diet, and improving access to and use of health services among those in lower socioeconomic groups and in poorer communities can reduce the risk of cardiovascular disease.[8,29,31] Social policies with greater welfare support, better work environment, and social protection for the disadvantaged can also help reduce behavioral and psychosocial risks, leading to reduced social inequalities in CVD mortality among working-age Americans.[8,16,29,31]
Key Messages.
Cardiovascular diseases, including heart disease and stroke, disproportionately affect those who live in poorer communities and who are unemployed and socioeconomically disadvantaged in the US workforce.
Socioeconomic disparities in cardiovascular disease, heart disease, and stroke mortality among working-age Americans rose markedly between 1969 and 2011.
Inequalities in cardiovascular disease, heart disease, and stroke mortality by area deprivation widened because higher socioeconomic groups experienced faster mortality declines during 1969-2011.
Increasing social inequalities in cardiovascular disease, heart disease, and stroke mortality among working-age Americans may be related to increasing temporal inequalities in living conditions and smoking, obesity, physical inactivity, and unhealthy diet.
With inequalities in living conditions and prevalence of smoking, obesity, physical inactivity, and westernization of diet on the rise, cardiovascular-disease burden among working-age populations in low- and middle-income countries will likely increase.
Acknowledgments
The views expressed are the authors’ and not necessarily those of their institutions.
Footnotes
Human Subjects Review: No IRB approval was required for this study, which is based on the secondary analysis of public-use databases.
Financial Disclosure: None.
Funding/Support: None.
Conflicts of Interest: None.
References
- 1.Hoyert DL. 75 years of mortality in the United States 2010. NCHS Data Brief. 2012;88:1–8. [PubMed] [Google Scholar]
- 2.Xu J, Kochanek KD, Murphy SL, Arias E. Mortality in the United States 2012. NCHS Data Brief. 2014;168:1–8. [PubMed] [Google Scholar]
- 3.National Center for Health Statistics. Health, United States, 2013 with Special Feature on Prescription Drugs. Hyattsville, MD: US Department of Health and Human Services; 2014. [PubMed] [Google Scholar]
- 4.World Health Organization. Monitoring Health Inequality: An Essential Step for Achieving Health Equity. Geneva, Switzerland: WHO; 2014. [Google Scholar]
- 5.US Department of Health and Human Services. Healthy People. 2020. [Accessed November 12 2014]. Available at: http://www.healthypeople.gov/2020/default.aspx .
- 6.Kitagawa EM, Hauser PM. Differential Mortality in the United States: A Study in Socioeconomic Epidemiology. Cambridge, MA: Harvard University Press; 1973. [Google Scholar]
- 7.Singh GK. Area deprivation and widening inequalities in US mortality 1969-1998. American Journal of Public Health. 2003;93(7):1137–1143. doi: 10.2105/ajph.93.7.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh GK, Siahpush M. Increasing inequalities in all-cause and cardiovascular mortality among US adults aged 25-64 years by area socioeconomic status 1969-1998. International Journal of Epidemiology. 2002;31(3):600–613. doi: 10.1093/ije/31.3.600. [DOI] [PubMed] [Google Scholar]
- 9.Davey Smith G, Neaton JD, Wentworth D, Stamler R, Stamler J. Socioeconomic differentials in mortality risk among men screened for the Multiple Risk Factor Intervention Trial: I-white men. American Journal of Public Health. 1996;86(4):486–496. doi: 10.2105/ajph.86.4.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davey Smith G, Wentworth D, Neaton JD, Stamler R, Stamler J. Socioeconomic differentials in mortality risk among men screened for the Multiple Risk Factor Intervention Trial: II-black men. American Journal of Public Health. 1996;86(4):497–504. doi: 10.2105/ajph.86.4.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh GK, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. American Journal of Public Health. 2001;91(3):392–399. doi: 10.2105/ajph.91.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rogot E, Sorlie PD, Johnson NJ, Schmitt C. A Mortality Study of 1.3 Million Persons by Demographic, Social, and Economic Factors, 1979-85 Follow-Up: U.S. National Longitudinal Mortality Study. Washington, DC: Public Health Service; 1992. NIH publication 92-3297. [Google Scholar]
- 13.Sorlie PD, Backlund E, Keller JB. US mortality by economic, demographic, and social characteristics: the National Longitudinal Mortality Study. American Journal of Public Health. 1995;85(7):949–956. doi: 10.2105/ajph.85.7.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Human Biology. 2002;74(1):83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- 15.Singh GK, Siahpush M, Altekruse SF. Time trends in liver cancer mortality, incidence, and risk factors by unemployment level and race/ethnicity, United States 1969-2011. Journal of Community Health. 2013;38(5):926–940. doi: 10.1007/s10900-013-9703-z. [DOI] [PubMed] [Google Scholar]
- 16.Marmot M, Bobak M, Davey-Smith G. Explanations for social inequalities in Health. In: Health and Society. Amick BC, Levine S, Tarlov AR, Walsh DC, editors. New York, NY: Oxford University Press; 1995. [Google Scholar]
- 17.National Center for Health Statistics. National Vital Statistics System, Mortality Multiple Cause-of-Death Public Use Data File Documentation. Hyattsville, MD: US Department of Health and Human Services; 2014. [Accessed November 5 2014]. http://www.cdc.gov/nchs/nvss/mortality_public_use_data.htm . [Google Scholar]
- 18.Singh GK, Azuine RE, Siahpush M, Kogan MD. All-cause and cause-specific mortality among US youth: socioeconomic and rural-urban disparities and international patterns. Journal of Urban Health. 2013;90(3):388–405. doi: 10.1007/s11524-012-9744-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.US Census Bureau. Census of Population and Housing 1990: Summary Tape File 3A on CD-ROM. Washington, DC: US Department of Commerce; 1992. [Google Scholar]
- 20.US Census Bureau. Summary File 3, Technical Documentation, 2000 Census of Population and Housing. Washington, DC: US Department of Commerce; 2005. [Google Scholar]
- 21.US Census Bureau. National Longitudinal Mortality Study, Reference Manual. Washington, DC: US Census Bureau; 2012. http://www.census.gov/did/www/nlms/publications/reference.html . [Google Scholar]
- 22.SAS Institute Inc. SAS/STAT User’s Guide, Version 9.1: The PHREG Procedure. Cary, NC: SAS Institute Inc; 2004. [Google Scholar]
- 23.Singh GK, Siahpush M, Azuine RE, Williams SD. Widening socioeconomic and racial disparities in cardiovascular disease mortality in the United States 1969-2013. International Journal of MCH and AIDS. 2015;3(2) [PMC free article] [PubMed] [Google Scholar]
- 24.Jefferys M. Social inequalities in health – do they diminish with age? American Journal of Public Health. 1996;86(4):474–475. doi: 10.2105/ajph.86.4.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mackenbach JP, Bos V, Anderson O, Cardano M, Costa G, Harding S, et al. Widening socioeconomic inequalities in mortality in six Western European countries. International Journal of Epidemiology. 2003;32(5):830–837. doi: 10.1093/ije/dyg209. [DOI] [PubMed] [Google Scholar]
- 26.Mackenbach JP, Cavellaars AEJM, Kunst AE, Groenhof F. Socioeconomic inequalities in cardiovascular disease mortality: an international study. European Heart Journal. 2000;21(14):1141–1151. doi: 10.1053/euhj.1999.1990. [DOI] [PubMed] [Google Scholar]
- 27.Shaw M, Dorling D, Gordon D, Davey-Smith G. The Widening Gap: Health Inequalities and Policy in Britain. Bristol: Policy Press; 1999. [Google Scholar]
- 28.Marang-van de Mheen PJ, Davey-Smith G, Hart CL, Gunning-Schepers LJ. Socioeconomic differentials in mortality among within Great Britain: time trends and contributory causes. Journal of Epidemiology and Community Health. 1998;52:214–218. doi: 10.1136/jech.52.4.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Department of Health. Tackling Health Inequalities: 10 Years On. London, UK: Health Inequalities Unit, Department of Health; 2009. [Google Scholar]
- 30.Wilkins R, Berthelot J, Ng E. Trends in mortality by neighbourhood income in urban Canada from 1971 to 1996. Health Reports. 2002;13(Suppl):1–27. doi: 10.1503/cmaj.1031528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization. Global Atlas on Cardiovascular Disease Prevention and Control. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 32.Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for US adults: National Health Interview Survey 2012. Vital and Health Statistics. 2014;10(260):1–161. [PubMed] [Google Scholar]
- 33.Singh GK, Siahpush M, Hiatt RA, Timsina LR. Dramatic Increases in Obesity and Overweight Prevalence and Body Mass Index among Ethnic-Immigrant and Social Class Groups in the United States 1976-2008. Journal of Community Health. 2011;36(1):94–110. doi: 10.1007/s10900-010-9287-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization. World Health Statistics Report 2014. Geneva, Switzerland: WHO; 2014. [Google Scholar]
- 35.Laslett LJ, Alagona P, Clark BA, Drozda JP, Saldivar F, Wilson SR, et al. The worldwide environment of cardiovascular disease: prevalence, diagnosis, therapy, and policy issues. Journal of the American College of Cardiology. 2012;60(25):S1–S49. doi: 10.1016/j.jacc.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 36.Finegold JA, Asaria P, Francis DP. Mortality from ischaemic heart disease by country, region, and age: statistics from World Health Organization and United Nations. International Journal of Cardiology. 2012;168(2013):934–945. doi: 10.1016/j.ijcard.2012.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization. Noncommunicable Diseases: Country Profiles 2014. Geneva, Switzerland: WHO; 2014. [Google Scholar]


