Abstract
Background
A key barrier to preventing workplace violence injury is the lack of methodology for prioritizing the allocation of limited prevention resources. The hazard risk matrix was used to categorize the probability and severity of violence in hospitals to enable prioritization of units for safety intervention.
Methods
Probability of violence was based on violence incidence rates; severity was based on lost time management claims for violence-related injuries. Cells of the hazard risk matrix were populated with hospital units categorized as low, medium, or high probability and severity. Hospital stakeholders reviewed the matrix after categorization to address the possible confounding of underreporting.
Results
Forty-one hospital units were categorized as medium or high on both severity and probability and were prioritized for forthcoming interventions. Probability and severity were highest in psychiatric care units.
Conclusions
This risk analysis tool may be useful for hospital administrators in prioritizing units for violence injury prevention efforts.
Keywords: workplace violence, injury, risk assessment, hazard risk matrix, health care workers
INTRODUCTION
Despite established federal violence prevention guidelines for health care workers [OSHA, 2004], violence incidence and injury rates are not decreasing [BLS, 2010] in an industry employing over 5 million workers in general medical and surgical hospitals [BLS, 2012]. Hospital employees are at increased risk for workplace violence [Peek-Asa et al., 1997; Arnetz et al., 2011a] as well as violence-related injury/illness requiring time away from work: 11.7 incidents per 10,000 fulltime equivalents (FTEs) compared to the overall private sector rate of 3.8/10,000 FTEs [BLS, 2013a]. Additionally, one third of all fatal occupational injuries in hospitals result from violent acts [BLS, 2013b]. One key barrier to violence injury prevention is the lack of methodology for prioritizing allocation of limited resources [Bonauto et al., 2006]. This paper describes a method for categorizing the risk of violence across multiple units and prioritizing sites for intervention using the hazard risk matrix.
A Public Health Approach to Workplace Violence Injury Prevention
The past decade has seen a growing trend towards utilizing a public health approach to occupational injury prevention generally [Smith, 2001; Stout, 2008] and to workplace violence injury prevention specifically [Arnetz et al., 2011a]. This approach is population-based [Smith, 2001] and has five basic components: (1) Surveillance for identifying and prioritizing occupational hazards; (2) Risk factor identification through epidemiological analysis; (3) Intervention development based on strategy identification and development; (4) Implementation of interventions; and (5) Evaluation of the efficacy of intervention efforts [Smith, 2001; Stout, 2008].
Using this framework, a project based on participatory action research aimed at reducing workplace violence in hospitals is currently underway in a large U.S. hospital system. Participatory action research enables researchers to collaborate with those community or organization members who “own” the situation/problem [Lingard et al., 2008]. The goal with this approach is to transfer local solutions into knowledge, thus, helping to make research results more generally applicable [Lingard et al., 2008]. In the current project, researchers are collaborating with hospital system stakeholders who are responsible for workplace violence prevention, including representatives of quality and safety, nursing, human resources, security, occupational health services, and labor. [Arnetz et al., in press]. Ongoing collaboration between researchers and hospital system stakeholders has resulted in fulfillment of the first-two components of the public health approach to injury prevention: (1) a standardized surveillance system of workplace violence events and (2) population-based epidemiological assessment of risk factors for workplace violence [Arnetz et al., 2011a,b]. Researchers and hospital system stakeholders are also implementing the third component in the public health approach, a standardized intervention for workplace violence reduction. The intervention study was designed and funded to encompass approximately 40 hospital units. The current study addresses the identification of these high-risk units.
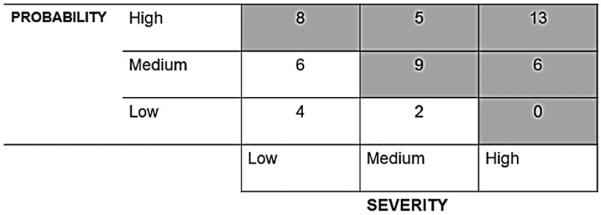
A critical first step in intervention implementation is the identification of units at increased risk for violence across the hospital system. Hospital system administrators need to know: (a) where prevention efforts are most needed in an organization with over 15,000 employees and 1300 units; and (b) how units can be prioritized in order for the violence intervention to be most cost-effective. For this purpose, we utilized an adapted version of the hazard risk matrix [CDC/NIOSH, 2003] to identify units at highest risk of workplace violence that would benefit most from the intervention (Fig. 1).
FIGURE1.
Hazard Risk Matrix [CDC/NIOSH, 2003].
Risk assessment matrices have more traditionally been used by the U.S. Military [DOD, 2000], NASA [NASA, 2008] and in industries with high-risk for occupational hazards [Clemens & Pfitzer, 2006], such as mining [CDC/NIOSH, 2003]. Their primary use is to categorize risks and set priorities for implementation of safety measures, not least because resource limitations do not often permit organizations to address multiple risks simultaneously [Donoghue, 2001]. Establishing priorities allows for the allocation of resources where they are most needed [CDC/NIOSH, 2003]. Common to these matrices is assessment of risk probability, i.e., the likelihood that a potential hazard will result in damage at a particular site, and risk consequence, i.e., how severe the outcome of the hazard can be in terms of harm to people/property [CDC/NIOSH, 2003]. Industries use these matrices to categorize and rank multiple occupational health risks [Donoghue, 2001; CDC/NIOSH, 2003]. In this study, the hazard risk matrix was used explicitly to examine the risk of a single occupational hazard — workplace violence — across a multi-site hospital system. Rather than ranking the probability and severity of multiple hazards within cells of the matrix, researchers ranked individual hospital units by risk and severity of workplace violence. Cells of the hazard risk matrix were populated by hospital units categorized as low, medium, or high probability and severity. Categorization of hospital units was based on previously-collected data regarding unit rates and severity of workplace violence. This study thus minimizes limitations in previous research which used qualitative appraisals of prospective potential hazards [Donoghue, 2001; CDC/NIOSH, 2003] by using systematically collected data on previously reported violent incidents to formulate the hazard assessments. The aim of this paper is to describe the application and implementation of the hazard risk matrix as a guide to prioritizing hospital units for violence prevention efforts.
MATERIALS AND METHODS
Setting and Participants
The violence reduction project is being carried out within a large American hospital system comprised of seven hospitals and approximately 15,000 employees. Since 2003, the hospital system has systematically collected employee-reported data on adverse events, including occupational exposures such as needle stick injuries, slips and falls, and violent events. Reports are documented electronically using a standardized form and submitted by employees from any hospital-system computer to a single, centralized database. In recent years, the research team has collaborated with the hospital system to create a subset of the database that includes only workplace violence data. Establishing a linkage between the violence database and the human resources database enabled the calculation of standardized rates of violence per 100 full-time equivalents (FTEs) per year. Detailed accounts of the reporting system and calculation of rates of workplace violence have been previously reported [Arnetz et al., 2011a,b]. The current study encompassed only hospital system employees and did not include contract or temporary workers. There were no eligibility criteria with regard to type of hospital. The only eligibility criteria were that all units should be hospital-based, since the focus of this study was violence in hospital environments. Thus, only units (n = 1159) within the system’s seven hospitals were included. Other types of units, such as convalescent centers, were excluded. In working with the hazard risk matrix, the aim was to identify approximately 40 units at high-risk for workplace violence. These units would be included in the intervention phase of the larger research project. Ethical approval for this study was granted by the Institutional Review Board at Wayne State University and the Research Review Council of the hospital system.
Workplace Violence
Using a broad definition similar to that provided by the Occupational Safety and Health Administration, OSHA [OSHA, 2002], the hospital system defines workplace violence as physical assault, harassment, intimidation, threats, and verbal aggression that occurs during the course of an employee’s work-related activities [Arnetz et al., 2011b]. Hospital system policy requires employees to report both physical and non-physical incidents of workplace violence within 72 hr of occurrence. Policy also ensures no retaliation or reprisal for employees reporting in good faith [Arnetz et al., 2011b]. Employees report demographic information along with the incident date, time, work shift, location, events preceding the incident, any injuries that occurred, and witnesses to the incident. A more detailed description of the incident may also be provided in free text. The majority of incident reports are complete, providing all incident details. Furthermore, rates of violence, both across and within hospitals, have been consistent over time. While underreporting of workplace violence is a common phenomenon among health care workers, especially among those for whom violence is commonplace [McPhaul & Lipscomb, 2004; Arnetz et al., 2011a], the stability of reporting trends in this hospital system over the past 10 years indicates consistent patterns of reporting.
All documented incidents of workplace violence are reviewed by hospital system data analysts and categorized according to the standard typology utilized in workplace violence research [IPRC, 2001]. Type I denotes incidents of criminal intent (e.g. robbery), where the perpetrator has no legitimate relationship with the workplace. In Type II incidents, the perpetrator is a customer, client or, in the case of hospitals, a patient receiving services. Type III are worker-to-worker incidents where the perpetrator is a current or former employee. In Type IV incidents, the perpetrator has no direct relationship with the workplace but does have a personal relationship with an employee. Type IV incidents often denote spillover of intimate partner violence from the home to the workplace.
The Hazard Risk Matrix
A version of the hazard risk matrix designed by The Centers for Disease Control/National Institute for Occupational Safety and Health (CDC/NIOSH) for the mining industry [CDC/NIOSH, 2003] provided the framework for the current project (Fig. 1). This matrix defines “hazard” as “any situation that has potential to cause damage” [CDC/NIOSH, 2003, pg. 3]. For the purposes of the current study, “hazard” was any incident of workplace violence documented and entered by an employee into the central reporting system. The matrix provides a framework for categorizing the hazard, i.e., workplace violence, based on its probability and its potential severity. Both probability and severity may be categorized as High, Medium, or Low (Fig. 1). Entries in the upper right quadrant of the matrix represent a combination of highest hazard probability and severity.
In a first step towards identifying units at risk for violence, researchers and system data analysts worked together to define key terms. Probability was defined as the likelihood of violence occurrence and was based on population-based workplace violence incidence rates. Rates were based on violent events reported into the hospital system’s incident database over the previous 30 months, between January 2010 and June 2012. Violence data was linked with the human resources’ database in order to identify employees’ assigned units. Using the number of violent events and paid productive hours (PPH), incidence rates were calculated for each work unit using the formula: [Number of incidents/Full-time equivalents (FTE)] × 100. FTEs were calculated as PPH/2080, which in the United States is the total number of hours worked by an FTE in one year, working 40 hr per week. Since PPH were only available by employee, and employees were identified in the human resource database via their assigned work units, rates of workplace violence were generated for work units. Categorization of violence probability was determined by reviewing the distribution for the hospital system units with at least one violent event. Probability rates ranged from 0.45 to 83.12 incidents/100 FTEs/year. Based on this distribution, the cutoffs for matrix categorization were set as follows: Low: <5 incidents per 100 FTEs per year (range 0.45–4.99); Medium: 5–10 incidents per 100 FTEs per year (range 5.03–9.79); High: ≥10 incidents per 100 FTEs per year (range 10.23–83.12 incidents/100 FTEs/year). With this categorization, approximately 46% of the units (n = 100) were categorized as Low; 25% (n = 56) were categorized as Medium; and 29% (n = 63) were categorized as High probability.
Severity was defined as injury due to violence resulting in time away from work and was measured in lost time costs. Injury was defined as any physical or psychological result of a workplace violence event that resulted in a lost time claim. All injuries occurring throughout the hospital system, including Workers’ Compensation cases, are processed centrally through the Loss Time Management department. Workers’ Compensation is the system designed to insure workers who are injured while performing a work-related task, covering their medical and rehabilitation expenses as well as lost wages [OWCP, 2013]. Other potential sources of severity measures were yes/no items in the incident report database regarding (1) whether medical treatment had been provided and (2) whether the employee had missed work as a result of the incident. The two latter measures were not always filled in; approximately 25% (n = 206) and 23% (n = 191) of the incidents were missing responses to the missed work and treatment provided questions, respectively. Employees may not always be aware of the extent of their injury or whether they would lose work time, at the time that the incident report is filed. Thus, lost time costs were considered a more reliable measure of incident severity. Events identified as workplace violence were linked to the lost time management data, which includes direct costs for claims related to violence-related injuries. These include the injured worker’s medical care and expense payments, any indemnity (wage replacement expense), plus a reserve of estimated future costs for those cases not yet closed. Miscellaneous expenses such as legal fees, mileage and parking reimbursements to the employee are also included. Rates were calculated for each unit using the formula [(Total amount paid + future reserves/full-time equivalents (FTEs)] × 100. Categorization of unit severity rates was determined by reviewing the distribution for the units with at least one workplace violence incident. Severity rates ranged from $0 to $215,175 per 100 FTEs/year. The majority of the units (73%, n = 160) had a lost time management rate of $0/100 FTEs per year and were assigned into the Low category. The remaining 27% (n = 59) were split evenly between Medium and High. Thus, the categories were as follows: Low: $0 per 100 FTEs per year; Medium: between $1 and $999 per 100 FTEs per year (range $16–$867); High: ≥$1,000 per 100 FTE’s per year (range$1518–$215174).
Identification of High-Risk Work Units
Based on these definitions, the data from the previous 30-month period was examined and used to populate the hazard risk matrix. Since this project focused on violence in hospital environments, analyses were restricted to units within hospitals and excluded, for example, community convalescent centers. The initial criterion for inclusion in the hazard risk matrix was a minimum of one violent event in the 30-month period. Since the forthcoming intervention was designed to include approximately 40 units, the criterion was narrowed to include only units with a minimum of five violent events in the previous 30-months. The rationale for including only those hospital units with five or more incidents was two-fold. First, reporting rates for units with less than five incidents might impact the statistical reliability of the data. Second, five was also considered a minimum number of events for unit managers and employees to consider workplace violence an occupational hazard. Once high-risk units were identified, the matrix was then used to prioritize a subset of approximately 40 of those units for participation in the forthcoming randomized, controlled violence prevention intervention. In a final step, results were presented at a group meeting of hospital system stakeholders, representing quality and safety, nursing, human resources, security, occupational health services, and labor. Stakeholder feedback was sought on the matrix results, as well as regarding the practicality, feasibility, and usefulness of the hazard risk matrix for categorization and prioritization of violence risk by unit. Evaluations of these aspects of the hazard risk matrix were based on stakeholder comments expressed in the group meeting. In a final step, correlation analysis was used to examine the association between probability and severity rates in the units identified as high-risk by the populated matrix.
RESULTS
Probability
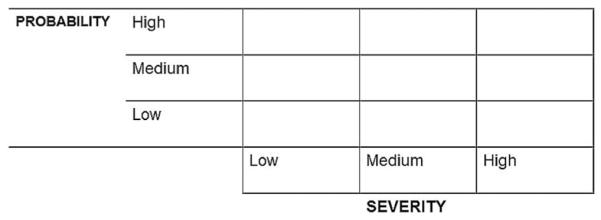
There were a total of 1159 units within the seven hospitals. A total of 838 incidents of workplace violence were documented at these units in the 30-month study period, which translated into an overall rate of 3.03 incidents/100 FTEs/year. The majority of incidents (n = 539, 64%) were perpetrated by patients or patient visitors (Type = II workplace violence), with 35% (n = 296) perpetrated by co-workers (Type III). One incident was Type I; no Type IV incidents were reported during the study period. Of the 1159 units, a total of 219 units had at least one incident of workplace violence during the study period, for an overall rate of 5.74 incidents/100 FTEs/year. Narrowing the criterion to those units with five or more incidents resulted in 53 units with an overall violence rate of 10.26 incidents/100 FTEs/year. A flowchart summarizing the data-driven process of identifying the 53 units with the highest probability of workplace violence is presented in Figure 2.
FIGURE 2.
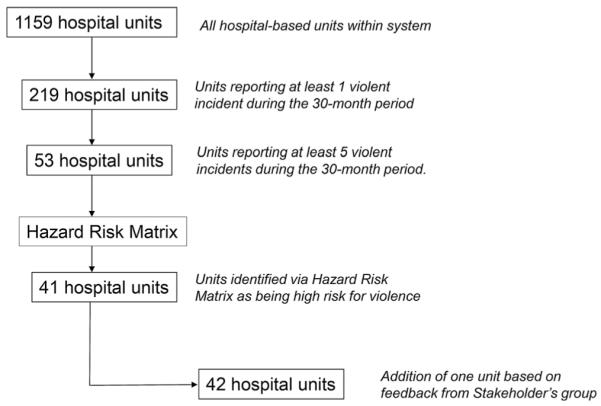
Flow chart describing identification of hospital units at risk for violence.
Rates for each of the 53 units were reviewed and categorized into the three probability categories (Low, Medium, High) in the matrix. Figure 3 summarizes the distribution of units based on this categorization of violence incidence rates. Nearly half the identified units (n = 26, 49%) were at high-risk for violence, i.e., with rates greater than 10 incidents/100 FTES/year.
FIGURE 3.
Populated Hazard Risk Matrix with number of units in each cell (n = 53 units).
Severity
The 53 units were also categorized as Low, Medium or High with regard to workplace violence severity based on lost time management rates (Fig. 3). Approximately 36% of work units (n = 19) had high rates of workplace violence severity. The majority (83%) of incidents in the high severity units were violent events in which the patient or patient visitor was the perpetrator (Type II workplace violence). Thus, units with higher rates of worker-to-worker (Type III) violence were more likely to fall into the Low or Medium severity category, as fewer of these incidents resulted in injuries with lost time claims.
Identification of Units for the Intervention Study
Probability and severity rates were combined to populate the hazard risk matrix for those units with five or more incidents (Fig. 3). Based on this categorization, researchers and data analysts selected units in the upper diagonal (shaded cells) which represented all units with either high or medium probability and high or medium severity. Using this method, 41 units were identified as potential targets of the intervention phase of the project. The overall rate of violence in the 41 units was 12.57 incidents/100 FTEs/year. For Type II incidents, the rate was 9.12/100 FTEs/year and for Type III, the rate was 3.41/100 FTEs/year. There was a moderate significant correlation between workplace violence rates and lost time claim rates (r = 0.32, P <.05).
Refinements Based on Stakeholder Perceptions
When presented with the populated hazard risk matrix in a group meeting, stakeholders questioned the exclusion of one unit, an emergency department that had been categorized in the low probability and medium severity cell. Stakeholders believed that violence there was more prevalent than the rates indicated, suggesting there was likely underreporting. Based on stakeholder input, the emergency department was included as a study site, resulting in a total of 42 units for the intervention project (Fig. 2).
The 42 units were further categorized according to type of patient care into the following blocks: Acute Care Nursing (i.e., all nursing units that were not intensive care), Intensive Care Unit (ICU) Nursing, Emergency Department, Psychiatry, Security, and Surgery. Distribution of the 42 identified units across the six blocks is presented in Table I. The number of incidents perpetrated by patients (Type II) exceeded those perpetrated by co-workers (Type III) in all blocks except Surgery, where Type III incidents dominated. Table I also provides the distribution of Type II and Type III incidents across units within blocks. The range of Type II incidents across all six blocks was 0–30, with zero incidents reported by one intensive care nursing unit and two surgery units. For Type III, the range was 0–13, with zero incidents reported by units in four of the six blocks. The number of Type II incidents was greater than the number of Type III incidents in most units with the exception of surgery units, where Type III incidents dominated in five out of six units. Nevertheless, 81% of the 42 identified units (n = 34) reported both types of incidents.
TABLE I.
Distribution of the 42 Units Across Blocks and Description and Range of Incidents Within Blocks
| Block | Number of units |
% | Number Type II incidents |
Range per unit Type II |
Number Type III incidents |
Range per unit Type III |
|---|---|---|---|---|---|---|
| Acute care nursing | 15 | 35.7 | 93 | 2–12 | 34 | 0–11 |
| Intensive care nursing | 8 | 19.0 | 29 | 0–11 | 24 | 0–7 |
| Emergency department | 5 | 11.9 | 61 | 4–19 | 20 | 1–10 |
| Psychiatry | 4 | 9.5 | 81 | 14–30 | 2 | 0–1 |
| Security | 4 | 9.5 | 53 | 4–24 | 1 | 0–1 |
| Surgery | 6 | 14.3 | 10 | 0–4 | 38 | 3–13 |
| Total | 42 | 100 | 327 | 0–30 | 119 | 0–13 |
Table II summarizes the categorization of the 42 units by violence probability, severity, and type of patient care. Both probability and severity were rated as high on all psychiatric care units. Acute care nursing and Surgery were the only patient care units with low severity ratings.
TABLE II.
Categorization of Hospital Units According to Workplace Violence Probability, Severity, and Unit Type (n = 42 Worksites Identified by the Hazard Risk Matrix)
| Probabilitya |
Severityb |
||||||
|---|---|---|---|---|---|---|---|
| Low |
Medium |
High |
Low |
Medium |
High |
||
| Nr. of Units | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Acute care nursing | 15 | 7 (46.7) | 8 (53.3) | 2 (13.3) | 6 (40.0) | 7 (46.7) | |
| Intensive care nursing | 8 | 4 (50.0) | 4 (50.0) | 3 (37.5) | 5 (62.5) | ||
| Emergency Dept. | 5 | 1 (20.0)c | 2 (40.0) | 2 (40.0) | 2 (40.0) | 3 (60.0) | |
| Psychiatry | 4 | 4 (100.0) | 4 (100.0) | ||||
| Security | 4 | 1 (25.0) | 3 (75.0) | 4 (100.0) | |||
| Surgery | 6 | 1 (16.7) | 5 (83.3) | 3 (50.0) | 2 (33.3) | 1 (16.7) | |
| Total | 42 | 1 (2.4) | 15 (35.7) | 26 (61.9) | 8 (19.0) | 15 (35.7) | 19 (45.3) |
Based on distribution of incidence rates.
Based on distribution of lost time management rates.
This emergency department was judged by hospital stakeholders to have a higher probability of violence and was added as the 42nd unit to the study.
Stakeholders were also asked to review and share their perceptions of the hazard risk matrix as a tool for examining the hospital system’s workplace violence data. All members of the group (n = 7) found the matrix “easy to understand” and stated that it provided an “excellent summary” of the violence data on a unit level. They perceived the categorization into Low, Medium, and High probability and severity as especially useful for distinguishing units at which workplace violence was most prevalent, most harmful to employees, and most costly to the organization.
DISCUSSION
Results of this study showed that the hazard risk matrix was a useful tool for identifying hospital units at high-risk for workplace violence within a large healthcare organization. By simultaneously examining both probability and severity data, units at greatest risk of workplace violence injury were identified. Out of a total of 1159 hospital-based units within the hospital system, 53 units (5%) reported a minimum of five violent events in a 30-month period. Of these, 41 (77%) were categorized both as high or medium probability and high or medium severity. With the additional unit added by the stakeholders, a total of 42 units were identified and are now included in an ongoing randomized, controlled study evaluating the impact of a standardized intervention on workplace violence prevalence and severity. Importantly, a broad definition that includes both physical and non-physical violence resulted in the inclusion of units that may have a high probability of violent events that are a combination of Type II (more likely to result in physical injury) and of Type III (less likely to result in injury) events. Hospital stakeholders appreciated this risk analysis, reporting that it provided an excellent summary of the workplace violence incidence and injury data.
Definition of terms is critical to using the hazard risk matrix. Typically, the matrix is used to examine the probability and severity of multiple risks within an industry, which are thereafter ranked in order of priority [Donoghue, 2001; Clemens & Pfitzer, 2006]. This requires occupational health and safety professionals to have in-depth knowledge of each individual risk, and how to measure its prevalence and consequences. In the current study, the matrix was used to categorize units at risk for a single hazard, workplace violence. This required a good working knowledge of the individual units, which was provided by the hospital system stakeholders. Upon review of the matrix, they immediately recognized the omission of one unit, an inner-city emergency department (ED), from the group of units identified by the hazard risk matrix. The stakeholders suspected that workplace violence was underreported at that ED, where violent incidents were known to be common. The database data from the ED suggest that it was primarily the more severe incidents (those resulting in injury) that were reported, since probability was categorized as low but severity was medium. A questionnaire study of emergency room workers [Gates et al., 2006] reported that only 35% reported assaults by patients that did not result in injury. This is in keeping with previous research that indicates that hospital workers in units with violent patient clientele do not report every violent event [Arnetz, 1998; Lanza et al., 2011; Iennaco et al., 2013]. Such underreporting is a major hindrance to the identification of hazardous worksites [Arnetz et al., 2011a; Iennaco et al., 2013]. Thus, while the hazard risk matrix provides a data-driven approach to identification of high-risk units, the “inside” information provided by stakeholders provides an important and necessary complement to the hazard assessment of workplace violence. This underlies the importance of a multi-disciplinary approach to violence and violence injury prevention within large healthcare organizations [Lipscomb et al., 2006; Gates et al., 2011].
Population-based rates of violence prevalence and violence-related injury were used to measure probability and severity, respectively. This resulted in a clear summary of units at greatest risk for violence, greatest risk for injury, and those sites at greatest risk of both. These units were easily categorized into one of six blocks, offering evidence that workplace violence in this healthcare organization is largely limited to certain types of patient care environments. Results clearly identified psychiatric, security, emergency, and nursing units at increased risk, especially for Type II violence and related injury. This supports previous literature on workplace violence in healthcare settings based on self-report [Gerberich et al., 2004] as well as on documented incidents [Kling et al., 2009; Arnetz et al., 2011a]. However, over 80% (n = 34) of the 42 identified units also reported Type III incidents. The surgical units reported primarily Type III incidents, resulting in relatively low severity ratings but high enough probability ratings to be identified as being at high-risk for violence. This may explain why probability and severity rates were only moderately correlated.
In measuring severity, we focused on the costs associated with violence-related injuries, measured by the total direct costs, i.e., total amount paid plus future reserves. This data was acquired from the hospital system’s central Loss Time Management Department and was selected because of its reliability due to the lack of missing data. Using costs as a measure of severity can be problematic, however, for example, violence-related injuries requiring time away from work were almost exclusively the result of incidents perpetrated by patients; these tended to be physical, more costly injuries than incidents perpetrated by co-workers. Future work with the hazard risk matrix should strive to incorporate additional measures of the severity of worker-to-worker violence, which is often non-physical [Gerberich et al., 2005; Arnetz et al., 2011b]. Reliable measures of the indirect costs of workplace violence injuries, such as musculoskeletal pain [Stock & Tissot, 2012], distraction [Barling, 1996] and depression [Wieclaw et al., 2006] would also enhance analysis of event consequences, both physical and non-physical.
Strengths and Limitations
This study has several important strengths. It applies an adapted version of an existing, evidence-based tool for risk assessment in hazardous industries to use in a healthcare setting. The matrix was populated with data from a standardized, central reporting system that encompassed all 15,000 hospital system employees at all 1159 hospital-based units. This allowed for the calculation of prevalence and severity rates based on the population at risk. Thus, both probability and severity were defined in quantitative values, rather than qualitative terms that are often used in other industries where population-based data is not readily available [Donoghue, 2001; Clemens & Pfitzer, 2006]. Examining the data and establishing cut-points for categorization establishes a data-driven process of risk assessment. Furthermore, the inclusion of both physical and non-physical violence in the assessment of hazardous units provides managers, administrators, and safety professionals with knowledge of the spectrum of violence within the hospital system. Implementation of the matrix was carried out in close collaboration with hospital stakeholders, ensuring its acceptance among end-users. Stakeholders also served to verify the final matrix results based on their in-depth knowledge of the hospital system units. Based on their qualitative comments, the matrix was considered easy to understand, feasible, and usable in summarizing and categorizing large amounts of workplace violence data. This underlies the importance of having a methodology for identifying and prioritizing units.
There are also a number of limitations. A common problem in workplace violence research is the issue of underreporting [McPhaul & Lipscomb, 2004; Arnetz et al., 2011a]. This is especially prevalent among healthcare employees for whom violence and aggression from patients is relatively common, such as in psychiatric care units or emergency departments. Violence is perceived as being “part of the job,” [Jackson et al., 2002] and it’s often difficult to motivate workers to report violent incidents [Arnetz, 1998; Lanza et al., 2011; Iennaco et al., 2013]. An example of this was evident in the current study, where probability measures for one emergency department were lower than what stakeholders believed were the actual levels. With this one exception, stakeholders verified that the hazard risk matrix had succeeded quite well in identifying the units that they, themselves, perceived as being at increased risk. However, the matrix serves to categorize the probability and severity of violence across multiple work units; it does not capture unit level risk or protective factors, as illustrated by the wide variation in the number of incidents of violence within blocks. For example, one intensive care nursing unit did not report any Type II incidents during the study period, while another reported 11. The matrix cannot ascertain whether that variation is due to actual increased risk in certain units; an increased tendency to report; or, conversely, a highly experienced work team that has developed methods to manage and prevent workplace violence. While no reporting system is perfect, some systematic method of incident reporting is a necessary prerequisite to hazard risk analysis and safety intervention [OSHA, 2004]. Second, rates of violence in this system are based on employee paid productive hours (PPH), and are therefore linked to employees’ respective work units, which may not always be where the violent event occurred. This is especially true of employees who work in different units within hospitals, such as security and patient transport staff. While incident location has important implications for intervention and prevention measures, it is not possible to generate accurate rates of occurrence or severity by incident location. However, location is most often included by employees in their incident reports, enabling database analysts to identify potential “hot spots” for workplace violence. Using injury data as a measure of severity also insured the inclusion of any Workers’ Compensation cases, which are most likely the violent events with the highest severity. Nevertheless, use of lost time management data as a measure of injury severity also has some limitations. This data was used since it was more reliable than other self-report data on medical treatment and missed work. However, these data do not encompass denied claims or claims without lost time, which is a similar issue when using workers’ compensation claims [Liss & McCaskell, 1994; McCall & Horwitz, 2004]. Using official lost time data also forced many of the violent events without physical injury into the low severity cells. Thus, Type III events (violence between workers), such as bullying, verbal abuse, and harassment, may be underrepresented with regard to severity since they most often have non-physical consequences [Gerberich et al., 2004; Arnetz et al., 2011b] that may not result in costly lost-time claims. Nevertheless, such events may have long-lasting psychological consequences, with negative implications for employee health and well-being [Barling, 1996; Wieclaw et al., 2006; Stock & Tissot, 2012]. In future work with the hazard risk matrix, alternate measures of severity for events with non-physical consequences should be developed.
CONCLUSION
The hazard risk matrix was used to identify hospital units at high-risk for workplace violence using previously collected data and hospital stakeholder input. This application of the matrix requires a system for incident reporting as well as hospital stakeholder knowledge of the work environments of specific units. Stakeholders agreed that the matrix can be helpful in prioritizing resources for violence injury prevention efforts on an ongoing basis. The hazard risk matrix may be useful in risk analysis of other occupational hazards in the healthcare environment.
ACKNOWLEDGMENTS
This study was funded by The Centers for Disease Control-National Institute for Occupational Safety and Health (CDC-NIOSH), grant number R01 OH009948. The content is solely the responsibility of the authors and does not necessarily represent the official views of CDC-NIOSH. The authors would like to thank all of the hospital system stakeholders who were involved in evaluating the hazard risk matrix as a tool for workplace violence injury prevention.
Footnotes
Disclosure Statement: The authors report no conflicts of interest.
REFERENCES
- Arnetz JE. The Violent Incident Form (VIF): A practical instrument for the registration of violent incidents in the health care workplace. Work Stress. 1998;12(1):17–28. [Google Scholar]
- Arnetz JE, Aranyos D, Ager J, Upfal MJ. Development and application of a population-based system for workplace violence surveillance in hospitals. Am J Ind Med. 2011a;54:925–934. doi: 10.1002/ajim.20984. [DOI] [PubMed] [Google Scholar]
- Arnetz JE, Aranyos D, Ager J, Upfal MJ. Worker-on-worker violence among hospital employees. Int J Occup Environ Health. 2011b;17:328–335. doi: 10.1179/107735211799041797. [DOI] [PubMed] [Google Scholar]
- Arnetz JE, Hamblin L, Ager J, Aranyos D, Essenmacher L, Upfal MJ, Luborsky M. Using database reports to reduce workplace violence: Perceptions of hospital stakeholders. Work. 2014 Jul 24; doi: 10.3233/WOR141887. In press. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barling J. The prediction, experience, and consequences of workplace violence. In: VandenBos GR, Bulatao EQ, editors. Workplace violence. American Psychological Association; Washington, DC: 1996. pp. 19–49. [Google Scholar]
- Bonauto D, Silverstein B, Adams D, Foley M. Prioritizing industries for occupational injury and illness prevention research, Washington state worker’s compensation claims, 1999–2003. J Occup Environ Med. 2006;48(8):840–851. doi: 10.1097/01.jom.0000225062.88285.b3. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics (BLS) Workplace safety and health in the health care and social assistance industry 2003–07. 2010 http://www.bls.gov/opub/cwc/print/sh20100825ar01p1.htm.
- Bureau of Labor Statistics (BLS) Occupational employment statistics: NAICS 622100–General medical and surgical hospitals (including private, state, and local government hospitals) 2012 http://www.bls.gov/oes/current/naics4_622100.htm.
- Bureau of Labor Statistics (BLS) Survey of Occupational Injuries and Illnesses, Resource Table R8, 2011. 2013a http://www.bls.gov/iif/oshwc/osh/case/ostb3210.pdf.
- Bureau of Labor Statistics (BLS) Census of Fatal Occupational Injuries, 2011. 2013b http://www.bls.gov/iif/oshwc/cfoi/cftb0259.pdf.
- Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health (CDC/NIOSH) Focus on prevention: conducting a hazard risk assessment 2003–139. CDC/NIOSH; Pittsburg, PA: 2003. http://www.cdc.gov/niosh/mining/UserFiles/works/pdfs/2003-139.pdf. [Google Scholar]
- Clemens P, Pfitzer T. Risk assessment and control: Is your system safety program wasting resources? Prof Saf January 2006. 2006:41–44. [Google Scholar]
- Department of Defense, (DOD) Standard practice for system safety MIL-STD-882D. DOD; Washington, DC: 2000. http://www.system-safety.org/Documents/MIL-STD-882D.pdf. [Google Scholar]
- Donoghue AM. The design of hazard risk assessment matrices for ranking occupational health risks and their application in mining and minerals processing. Occup Med. 2001;51(2):118–123. doi: 10.1093/occmed/51.2.118. [DOI] [PubMed] [Google Scholar]
- Gates D, Gillespie G, Smith C, Rode J, Kowalenko T, Smith B. Using action research to plan a violence prevention program for emergency departments. J Emerg Nurs. 2011;37(1):32–39. doi: 10.1016/j.jen.2009.09.013. [DOI] [PubMed] [Google Scholar]
- Gates DM, Ross CS, McQueen L. Violence against emergency department workers. J Emerg Med. 2006;31(3):331–337. doi: 10.1016/j.jemermed.2005.12.028. [DOI] [PubMed] [Google Scholar]
- Gerberich SG, Church TR, McGovern PM, Hansen NM, Geisser MS, Ryan AD, Mongin SJ, Watt GD. An epidemiological study of the magnitude and consequences of work related violence: The Minnesota Nurses’ Study. Occup Environ Med. 2004;61(6):495–503. doi: 10.1136/oem.2003.007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerberich SG, Church TR, McGovern PM, Hansen H, Nachreiner NM, Geisser MS, Ryan AD, Mongin SJ, Watt GD, Jurek A. Risk factors for work-related assaults on nurses. Epidemiology. 2005;16(5):704–709. doi: 10.1097/01.ede.0000164556.14509.a3. [DOI] [PubMed] [Google Scholar]
- Iennaco J, Dixon J, Whittemore R, Bowers L. Measurement and monitoring of health care worker aggression exposure. OJIN. 2013;18(1):1–19. [PubMed] [Google Scholar]
- Injury Prevention Research Center (IPRC) Workplace violence, a report to the nation. University of Iowa; Iowa City, IA: 2001. http://www.public-health.uiowa.edu/iprc/resources/workplace-violence-report.pdf. [Google Scholar]
- Jackson D, Clare J, Mannix J. Who would want to be a nurse? Violence in the workplace – a factor in recruitment and retention. J Nurs Manag. 2002;10:13–20. doi: 10.1046/j.0966-0429.2001.00262.x. [DOI] [PubMed] [Google Scholar]
- Kling RN, Yassi A, Smailes E, Lovato CY, Koehoorn M. Characterizing violence in health care in British Columbia. J Adv Nurs. 2009;65(8):1655–1663. doi: 10.1111/j.1365-2648.2009.05020.x. [DOI] [PubMed] [Google Scholar]
- Lanza ML, Schmidt S, McMillan F, Demaio J, Forester L. Support our staff–A unique program to help deal with patient assault. Perspect Psychiatr Care. 2011;47(3):131–137. doi: 10.1111/j.1744-6163.2010.00282.x. [DOI] [PubMed] [Google Scholar]
- Lingard L, Albert M, Levinson W. Grounded theory, mixed methods, and action research. BMJ. 2008;337:a567. doi: 10.1136/bmj.39602.690162.47. [DOI] [PubMed] [Google Scholar]
- Lipscomb J, McPhaul K, Rosen J, Brown JG, Choi M, Soeken K, Vignola V, Wagoner D, Foley J, Porter P. Violence prevention in the mental health setting: The New York state experience. Can J Nurs Res. 2006;38(4):96–117. [PubMed] [Google Scholar]
- Liss GM, McCaskell L. Injuries due to violence: Workers’ compensation claims among nurses in Ontario. AAOHN J. 1994;42(8):384–390. [PubMed] [Google Scholar]
- McCall BP, Horwitz IB. Workplace violence in Oregon: An analysis using workers’ compensation claims from 1990–1997. J Occup Environ Med. 2004;46:357–366. doi: 10.1097/01.jom.0000121131.34757.ed. [DOI] [PubMed] [Google Scholar]
- McPhaul KM, Lipscomb JA. Workplace violence in health care: Recognized but not regulated. Online J Issues Nurs. 2004;9(3) http://www.nursingworld.org/ojin/topic25/tpc25_6.htm. [PubMed] [Google Scholar]
- National Aeronautics and Space Administration (NASA) NASA safety manual NPR 8715.3C. NASA; Washington, DC: 2008. http://nodis3.gsfc.nasa.gov/displayDir.cfm?t=NPR&c=8715&s=3C. [Google Scholar]
- Occupational Safety and Health Administration (OSHA) OSHA Fact Sheet Workplace Violence. Washington, DC: 2002. https://www.osha.gov/OshDoc/data_General_Facts/factsheet-workplace-violence.pdf. [Google Scholar]
- Occupational Safety and Health Administration (OSHA) Guidelines for preventing workplace violence for health care and social service workers 3148-01R. Washington, DC: 2004. https://www.osha.gov/Publications/OSHA3148/osha3148.html. [Google Scholar]
- Office of Workers’ Compensation Programs (OWCP) About OWCP. 2013 http://www.dol.gov/owcp/owcpabot.htm.
- Peek-Asa C, Howard J, Vargas L, Kraus JF. Incidence of non-fatal workplace assault injuries determined from employer’s reports in California. J Occup Environ Med. 1997;39(1):44–50. doi: 10.1097/00043764-199701000-00009. [DOI] [PubMed] [Google Scholar]
- Smith GS. Public health approaches to occupational injury prevention: Do they work? Inj Prev. 2001;7(Suppl I):i3–10. doi: 10.1136/ip.7.suppl_1.i3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stock SR, Tissot F. Are there health effects of harassment in the workplace? A gender-sensitive study of the relationships between work and neck pain. Ergonomics. 2012;55(2):147–159. doi: 10.1080/00140139.2011.598243. [DOI] [PubMed] [Google Scholar]
- Stout NA. The public health approach to occupational injury research: From surveillance to prevention. Saf Sci. 2008;46(2):230–233. [Google Scholar]
- Wieclaw J, Agerbo E, Mortensen PB, Bonde JP. Risk of affective and stress related disorders among employees in human service professions. Occup Environ Med. 2006;63(5):314–319. doi: 10.1136/oem.2004.019398. [DOI] [PMC free article] [PubMed] [Google Scholar]