Abstract
BACKGROUND
The positive role of having a usual source of care (USOC) on the receipt of preventative services is known. However, associations between USOC and hypertension control and the differential association across age groups is unknown in the US population.
METHODS
We used data from the National Health and Nutrition Examination Survey (NHANES) from 2007 to 2012. Multivariable logistic regression was used to evaluate the association between having a USOC and hypertension control. The differential effect of USOC on hypertension control by age was assessed using predicted marginal effects across age groups in the multivariable logistic model.
RESULTS
In adjusted analyses, those with a USOC had higher odds of hypertension control (odds ratio = 3.89, 95% confidence interval (CI): 2.15–6.98). The marginal effect of having a USOC is associated with a 30 percentage point higher probability of controlled blood pressure compared to those without a USOC (marginal probability = 0.30, 95% CI: 0.19–0.41). The marginal effect of USOC on hypertension control varied by age groups, with a statistically significantly lower marginal effect of USOC on hypertension seen among those older than 74 years of age (marginal probability = 0.27, 95% CI: 0.18–0.36) and younger than 35 years of age (marginal probability = 0.23, 95% CI: 0.14–0.33).
CONCLUSION
Having a USOC is significantly associated with improved hypertension control in the US population. The variation in the association across age groups has important implications in targeting age-specific antihypertensive strategies to reduce the burden of hypertension in the US population.
Keywords: age, blood pressure, hypertension, usual source of care.
Approximately 80 million US adults have hypertension with just over half controlled.1 Because hypertension is a major risk factor for the development of heart failure, stroke, and coronary artery disease, controlling hypertension is critical for reducing morbidity, mortality, and costs.1–4
The burden of hypertension in older Americans is particularly striking. Nearly 3 out of 4 individuals aged >74 years have hypertension, and with each decade of life, the stroke mortality rate is significantly greater for those with hypertension than those with normal blood pressure.2,3,5,6
Elucidating the impact of having access to a usual source of care (USOC) on hypertension control has important policy implications in the organization of care and management of chronic disease. Observational studies have examined the association between having a USOC and the receipt of preventative care and found positive associations between regular sources of care and mammograms, flu vaccination, cholesterol checks, and blood pressure checks.7–10
Beyond blood pressure checks, there are few studies that have examined the relationship between structural access to care (i.e., insurance or a USOC) and treatment or control of blood pressure.11,12 An older study using National Health and Nutrition Examination Survey (NHANES) III data from the late 1980s and early 1990s found that having private health insurance and using the same facility or provider for healthcare was associated with higher odds of blood pressure control.11 In another study, having a USOC was associated with a higher prevalence of treatment for hypertension in adults, but hypertension control was not examined.12
Given major changes in the treatment landscape and population demographics over the past 25 years, it is important to re-examine the relationship between structural access to care and hypertension control. Thus, this study has 3 major objectives: (i) to evaluate whether having a USOC is associated with hypertension control in the US population, (ii) to assess if the effect of USOC on hypertension varies by age group, and (iii) to analyze age group behaviors and USOC type utilization. Assessing the link between USOC and hypertension control, and differences in the association by age, is an important step in understanding what effect increasing structural access to care may have on the US hypertensive population.
METHODS AND MEASURES
Data source
This cross-sectional study design uses health interview and medical exam data from the NHANES from 2007 to 2012. NHANES uses a complex, multistage sampling design to select a representative sample of the civilian noninstitutionalized population in the United States.13 The physical exam component contains data on blood pressure, height, and weight that is gathered at a mobile exam center. In addition, the NHANES questionnaires assess comorbidities, self-reported health status, dietary and health habits, and information on USOC.
The NHANES sample for this study is restricted to the hypertensive population (i.e., those who currently taking blood pressure medication or had systolic blood pressure 140 or diastolic 90 at the time of the mobile exam component). This restricted subsample is consistent with other studies assessing hypertension outcomes.11,12
Measures
Trained professionals measured blood pressure using sphygmomanometry and appropriately sized arm cuffs after 5 minutes seated rest. Blood pressure measurements were taken 3 consecutive times and averaged after discarding the first measurement.13
“Hypertension control” is defined as average systolic blood pressure less than 140mm Hg and diastolic less than 90mm Hg.2 Newer JNC8 criteria were not used because clinicians during the time period of this study would not have been using the new targets for the older population.3 Treatment for hypertension was defined by one’s response to: “Are you taking blood pressure medication?”
NHANES defines USOC as a place to go when one is ill and needs care; places are listed as hospital outpatient department, outpatient clinic or doctor’s office, emergency department, or none.14 If individuals report no USOC or use the emergency department, they are treated as “no USOC.” For some analyses, USOC type is broken down into “traditional” USOC (clinic, doctor’s office, or outpatient hospital department), emergency department USOC, and no USOC.
Other variables and their construction are as follows:
We include only adults 18 years of age and older and stratify by 10-year intervals to create 6 separate groups.
Race/ethnicity is defined as Hispanic, non-Hispanic White, non-Hispanic Black, and “other race” which includes multiracial.
We treat married individuals and those living with partner as “married” and all others as “not married.”
Insurance status is defined as either insured or uninsured.
Education is defined as the highest grade completed and is collapsed into 3 categories: (i) those who did not complete high school, (ii) high school graduates, and (iii) college graduates.
Income is defined as family income in relationship to federal poverty level (FPL). Specifically, we create 4 mutually exclusive categories: (i) “Poorest”/<150% FPL, (ii) 150–249% FPL, (iii) 250–349% FPL, and (iv) >350% FPL.
Self-reported health is defined as fair, poor, good, very good, or excellent health.
Self-reported activity is defined by whether individuals met the American College of Sports Medicine guidelines for aerobic physical activity.15
Smoking is defined as smoking at least 100 cigarettes in one’s lifetime.16
Comorbidities such as diabetes, heart failure, prior heart attack (myocardial infarction), prior stroke (cerebrovascular accident), and high cholesterol are all defined based on a patient’s answers to the following question: “Has a doctor ever told you that you have/had ‘X’?”
Kidney function was determined by laboratory assessment of creatinine (in mg/dl) and is treated as a continuous variable.
Body mass index (BMI) was calculated during the mobile exam center and is defined as a person’s weight (in kilogram) divided by their height (in meters) squared. We use the CDC definitions for underweight (BMI < 18.5), normal weight (BMI = 18.5–24.9), overweight (BMI = 25–29.9), and obese (BMI ≥ 30).
Study design and statistical methods
We use survey methods for all weighted bivariate analyses and regression models. Bivariate relationships between covariates and USOC and bivariate associations with hypertension control are assessed using the chi-square test. Unadjusted weighted proportions of those with controlled hypertension are presented by USOC type (e.g., “traditional” USOC, emergency department, and none) and unadjusted weighted proportions of age groups are presented by USOC type. We employed 2 logistic models to analyze the effects of USOC on hypertension control. The first adjusts for demographics and comorbidities and the second adjusts for demographics and comorbidities after imputation of variables with missing data (see below for missing data methods). We test the differential association between age and USOC by testing the equality of the marginal effects of USOC on the probability of hypertension control at each age group in the full multivariate logistic model.17 Predictions are generated using average probabilities among actual persons in the data and errors are weighted to account for population sampling. We made an a priori decision based on our conceptual models to explore the factors potentially responsible for the varying effect of USOC on hypertension control by examining bivariate relationships with age groups and antihypertensive medication use, follow-up, smoking status, and exercise.
Missing data
Variables with missing data were imputed using multiple imputation with chained equations using age, gender, race/ethnicity, diabetes status, smoking status, and USOC.18–20 We specified 5 multiply imputed datasets and variables were assumed to be missing at random.21
RESULTS
Missing data
Most of the variables had either no missing data or were missing <2%. Only 3 variables were missing approximately 10% (BMI category, income, and hyperlipidemia). All missing data were imputed as described above.
Bivariate analysis
In bivariate analysis, those without a USOC were more likely to be younger, of Hispanic ethnicity or non-Hispanic Black, and male. In addition, individuals without a USOC were less likely to be married, have insurance, have completed high school, and less likely to report having diabetes, heart failure, prior stroke, or high cholesterol. A higher proportion of antihypertensive medication use and control was seen in those with a USOC (see Table 1).
Table 1.
Characteristics of the NHANES 2007–2012 adult hypertension subsample by USOC
| USOC (n = 6,785)Weighted % = 90.7% | No USOC (n = 868)Weighted % = 9.3% | |
| Age strata, no. (weighted %) | ||
| 18–34 | 504 (7.5%) | 226 (28.5%)** |
| 35–44 | 625 (11.4%) | 145 (17.9%)** |
| 45–54 | 1,012 (19.3%) | 186 (26.6%)** |
| 55–64 | 1,540 (24.4%) | 167(15.5%)** |
| 65–74 | 1,523 (19.2%) | 89 (7.1%)** |
| >75 | 1,581 (18.2%) | 55 (4.3%)** |
| Race/ethnicity, no. (weighted %) | ||
| Hispanic | 1,359 (8.4%) | 327 (23.1%)** |
| Non-Hispanic White | 3,159 (71.9%) | 244 (48.9%)** |
| Non-Hispanic Black | 1,789 (14%) | 228 (19.6%)** |
| Other race | 478 (5.6%) | 69 (8.4%) |
| Gender | ||
| Male, no. (weighted %) | 3,158 (45.7%) | 539 (65%)** |
| Marital status | ||
| Married or partner, no. (weighted %) | 3,833 (63.7%) | 430 (51.9%)** |
| Insurance status | ||
| Insured, no. (weighted %) | 6,028 (90.9%) | 385 (47.5%)** |
| Education, no. (weighted %) | ||
| Less than high school | 2,110 (21.3%) | 387 (34.5%)** |
| High school graduate or some college | 3,415 (54.2%) | 390 (51.8%) |
| College graduate | 1,243 (24.5%) | 90 (13.7%)** |
| Physical activity, no. (weighted %) | ||
| Meeting physical activity guidelines | 2,262 (37.3%) | 418 (51.5%)** |
| Smoking status, no. (weighted %) | ||
| Nonsmoker | 3,589 (52.8%) | 441 (46.2%)* |
| Current smoker | 1,098 (15.4%) | 274 (35.8%)** |
| Former smoker | 2,098 (31.8%) | 153 (18%)** |
| Comorbidities, no. (weighted %) | ||
| Diabetes | 1,558 (19%) | 71 (6.3%)** |
| Heart failure | 452 (5.7%) | 18 (1.3%)** |
| Prior MI | 522 (6.5%) | 35 (3.2%)** |
| Prior stroke | 549 (6.6%) | 26 (2%)** |
| Hyperlipidemia | 3,218 (52.6%) | 169 (33.2%)** |
| COPD | 435 (6.6%) | 26 (3.2%)* |
| BMI category, no. (weighted %) | ||
| Obese | 2,848 (46.7%) | 295 (41.9%) |
| Overweight | 1,968 (32.8%) | 237 (30.7%) |
| Normal weight | 1,220 (19.2%) | 164 (24.7%)* |
| Underweight | 74 (1.3%) | 19 (2.7%)** |
| Hypertension treatment and control | ||
| Taking antihypertensive medication, no. (weighted %) | 4,746 (70.7%) | 182 (20.1%)** |
| Hypertension controlled, no. (weighted %) | 2,836 (54.8%) | 97 (17%)** |
Total sample size n = 7,653 representing 87,298,349 individuals. Abbreviations: BMI, body mass index; COPD, chronic obstructive pulmonary disease; MI, myocardial infarction; NHANES, National Health and Nutrition Examination Survey; USOC, usual source of care.
*Statistically significant at P <0.05.
**Statistically significant at P <0.01.
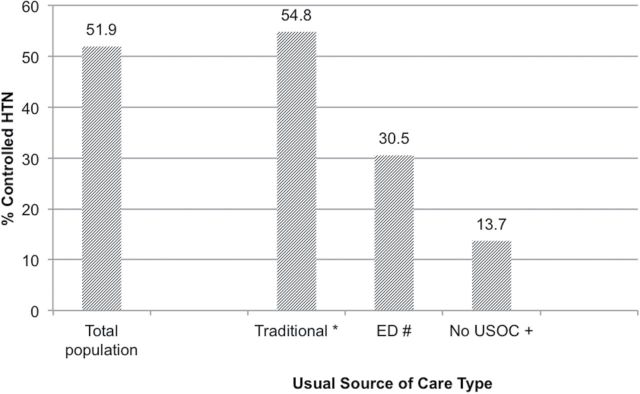
Figure 1 illustrates the proportion of controlled hypertension by USOC type. Fifty-two percent have controlled hypertension. Only 14% without a USOC have controlled hypertension, compared to 55% with a traditional USOC (P < 0.01). Those who use the emergency department as their USOC were less likely to have controlled hypertension than those with a “traditional” USOC (31% vs. 55%, P < 0.01).
Figure 1.
Proportion of controlled HTN by USOC type. *Traditional USOC includes office, clinic, and hospital outpatient department. #Proportion of population with controlled HTN and ED USOC significantly different from both no USOC (P = 0.002) and traditional USOC (P < 0.001). +No USOC excludes the ED. Abbreviations: ED, emergency department; HTN, hypertension; USOC, usual source of care.
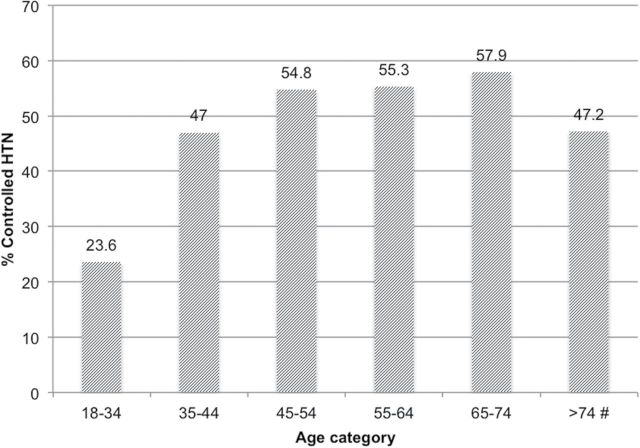
Figure 2 illustrates the proportion with controlled hypertension by age group. Hypertension control was statistically significantly lower in the youngest (18–34 and 35–44 year olds) and oldest (>74 years old) compared to other age groups. Only 24% of 18–34 year olds, 47% of 35–44 year olds, and 47% of those older than 74 had their blood pressure under control. The proportion with controlled hypertension in the other age groups was 55% (age 45–54), 55% (age 55–64), and 58% (age 65–74).
Figure 2.
Proportion of controlled HTN by age group. #Proportion of controlled HTN statistically significantly different between age >74 when compared to ages 65–74, 55–64, 45–54, and 18–34 (P < 0.001). No statistically significant difference in proportion of controlled HTN between age ≥75 and age 35–44 (P = 0.27). Abbreviation: HTN, hypertension.
Whites were more likely than non-Whites to have controlled hypertension (54% vs. 46%, P < 0.01). Women were more likely than men to have controlled hypertension (55% vs. 48%, P < 0.01). Those with insurance were also more likely to have controlled hypertension than the uninsured (54% vs. 32%, P < 0.01). Current smokers were less likely to have controlled hypertension than former and nonsmokers (46% vs. 53%, P < 0.01). Obese individuals were also more likely to have controlled hypertension than those with normal weight (57% vs. 39%, P < 0.05).
In our age group analyses—examining relationships between age groups and USOC type and behaviors—we found that younger individuals (<35 years old) are statistically significantly less likely to have a traditional USOC (72% vs. 92%, P < 0.01) and more likely to use the emergency department as their USOC (4% vs. 1%, P < 0.01) or have no USOC compared to older age groups (24% vs. 6%, P < 0.01). The youngest (<35 years old) are statistically significantly less likely to be taking blood pressure medication than older groups (15% vs. 71%, P < 0.01). The youngest (<35 years old) are also more likely to have no visits to their providers in the past year (20% vs. 8%, P < 0.01), meet physical activity guidelines (49% vs. 37%, P < 0.01), and be current smokers (27% vs. 16%, P < 0.01) than older groups. In contrast, the oldest individuals (>74 years old) were more likely to visit their providers 2 or more times in the past year (91% vs. 77%, P < 0.01) and more likely to be taking blood pressure medication (80% vs. 63%, P < 0.01) than all younger age groups. The oldest (>74 years old) were less likely to be smokers (5% vs. 20%, P < 0.01) and meet physical activity guidelines compared to all other age groups (23% vs. 42%, P < 0.01).
Multivariable models
Multivariable logistic regression models revealed a significant positive relationship between having a USOC and hypertension control (see Table 2). In the full model adjusting for demographics and comorbidities without imputation, those with a USOC had significantly higher odds of hypertension control than those without a USOC (odds ratio (OR) = 3.89, 95% confidence interval (CI): 2.15–6.98). The magnitude, direction, and significance of the relationship did not change in the imputation model (OR = 3.89, 95% CI: 2.6–5.83).
Table 2.
Odds ratios and 95% confidence intervals for hypertension control
| Covariate | Model 1a | Model 2b |
|---|---|---|
| Usual source of care | 3.89 (2.15–6.98) | 3.89 (2.60–5.83) |
| Age strata | ||
| >74 | 0.58 (0.45–0.76) | 0.66 (0.53–0.83) |
| 55–64 | 1.03 (0.79–1.36) | 1.01 (0.80–1.28) |
| 45–54 | 1.1 (0.84–1.45) | 1.14 (0.90–1.45) |
| 35–44 | 0.84 (0.59–1.22) | 0.89 (0.65–1.22) |
| 18–34 | 0.38 (0.25–0.58) | 0.42 (0.29–0.61) |
| Race/ethnicity | ||
| Hispanic | 0.72 (0.56–0.93) | 0.72 (0.59–0.87) |
| Non-Hispanic Black | 0.7 (0.59–0.84) | 0.75 (0.65–0.87) |
| Other race | 0.86 (0.60–1.23) | 0.81 (0.60–1.11) |
| Male | 0.76 (0.66–0.87) | 0.73 (0.65–0.83) |
| Married | 1.22 (1.01–1.47) | 1.2 (1.02–1.41) |
| Insured | 1.53 (1.09–2.16) | 1.67 (1.3–2.15) |
| Comorbid conditions | ||
| Heart failure | 1.3 (0.94–1.83) | 1.28 (0.97–1.69) |
| Diabetes | 1.02 (0.81–1.29) | 1.15 (0.94–1.40) |
| Hyperlipidemia | 1.55 (1.27–1.90) | 1.45 (1.22–1.74) |
| BMI category | ||
| Obese | 2.03 (1.58–2.61) | 1.94 (1.52–2.49) |
| Overweight | 1.61 (1.23–2.09) | 1.62 (1.26–2.10) |
| Underweight | 0.89 (0.28–2.76) | 0.87 (0.35–2.17) |
Reference categories for multiple category variables are as follows: age 65–74, White race, normal weight. Not all variables in model shown in table. Abbreviation: BMI, body mass index.
aLogistic model controlling for demographics and clinical characteristics.
bLogistic model after imputation.
Individuals older than 74 years of age had a 42% lower odds of hypertension control than 65–74 year olds (OR = 0.58, 95% CI: 0.45–0.76). Non-Hispanic Blacks had a 30% lower odds of hypertension control than Whites (OR = 0.70, 95% CI: 0.59–0.84); Hispanics had a 28% lower odds of hypertension control than Whites (OR = 0.72, 95% CI: 0.56–0.93).
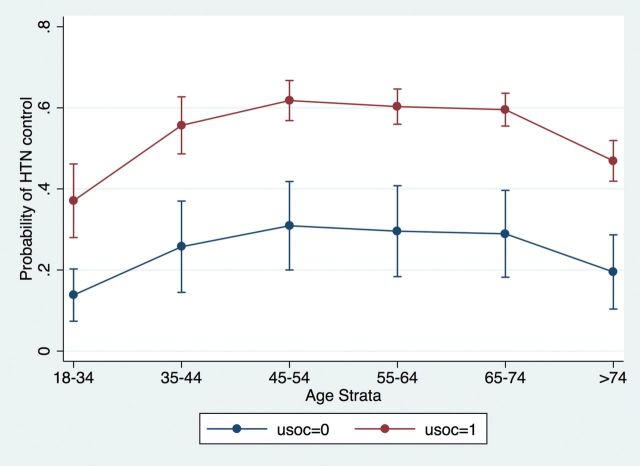
In probability terms, the marginal effect of having a USOC is associated with a 30 percentage point higher probability of controlled blood pressure compared to those without a USOC (marginal probability = 0.30, 95% CI: 0.19–0.41). This marginal effect amounts to an additional 300,000 individuals with controlled hypertension per million in the US hypertensive population. Figure 3 illustrates the marginal effect between USOC and hypertension at each age group. The marginal effect of USOC on the probability of hypertension control in the youngest age group (18–34 year olds) is 0.23 (95% CI: 0.14–0.33) and in the oldest group (>74 year olds), it is 0.27 (95% CI: 0.18–0.36). The marginal effect of USOC on hypertension control in 35–44 year olds is 0.30 (95% CI: 0.19–0.41); among 45–54 year olds, it is 0.31 (95% CI: 0.19–0.43); among 55–64 year olds, it is 0.31 (95% CI: 0.19–0.42); and among 65–74 year olds, it is 0.31 (95% CI: 0.19–0.42). The 7–8 percentage point difference in marginal effect of USOC on hypertension control in the youngest group (compared to all middle age groups) is statistically significantly lower. In terms of the US population, this difference amounts to 70,000–80,000 fewer young individuals with controlled hypertension per million individuals with hypertension. The 3–4 percentage point difference in marginal effect in the oldest age group (compared to all middle age groups) is statistically significantly lower. This difference amounts to 30,000–40,000 fewer older individuals with controlled hypertension per million in the US hypertension population.
Figure 3.
Marginal effect of USOC on HTN control by age group. The marginal effect of USOC on the probability of HTN control is statistically significantly lower in the oldest (>74 year olds) and youngest (18–34 year olds) age groups when compared to all other age groups (P < 0.05). Abbreviations: HTN, hypertension; USOC, usual source of care.
DISCUSSION
In this paper, we discovered several key relationships: (i) a significant positive association between having a USOC and hypertension control in the US population, (ii) a different marginal effect between USOC and controlled hypertension by age group, and (iii) different USOC types and behaviors by age group.
The association between USOC and hypertension control captures the totality of pathways through which structural access may impact hypertension control. There are several mediating pathways through which a USOC may operate to improve hypertension control. First, and likely most significant, having a USOC may lead to increased initiation of and adherence to antihypertensive medication use given that trust in one’s physician has been associated with improved medication compliance.22 Second, patients with a USOC may be more likely to follow up with their providers,23 allowing for titration of antihypertensive medications and discussion of healthy behaviors that lead to improved cardiovascular health. In addition, individuals with other chronic medical issues may be more likely to have a USOC, and management of other comorbidities may increase antihypertensive treatment.24,25
The reasons for a changing relationship between USOC and hypertension control by age group may be a result of differences in health habits, compliance with medication, or dynamic physiologic changes with aging. Some health and nutrition habits that are associated with good overall physical and mental health may been seen in aging, but there are also potential changes in mobility, cognition, and social support—in addition to changes in vascular physiology—that may negatively impact health and blood pressure control.26–29 In our age group analyses, older individuals were more likely to follow up, be taking blood pressure medication, and less likely to smoke. Assuming a mediating role for these factors between USOC and hypertension control, these data suggest that other physiologic factors may be playing a more prominent role in diminished marginal effect of USOC on hypertension control in the oldest individuals. This finding would be in alignment with basic science research demonstrating age-related changes in the blood vessels and chronic physiologic changes in the neural and biochemical systems responsible for regulating blood pressure.30–35 In contrast, the youngest age groups were more likely to use a different setting for their USOC (i.e., the emergency department) that may be less efficient in controlling hypertension long term. In addition, younger individuals were more likely to be current smokers and have no visits to their USOC in the past year and less likely to be taking blood pressure medication. These findings are in agreement with another study showing that infrequent healthcare may be a significant contributor to undiagnosed and/or untreated hypertension in the youngest individuals.36 Thus, in younger individuals, behavioral factors may play more of a role in the diminished marginal effect of USOC on hypertension control.
Limitations
There are several limitations to this study, given the cross-sectional design, measurement of hypertension, potential endogeneity of USOC, and subpopulation sizes. With a cross-sectional design, the causality underlying the observed relationship between USOC and hypertension control cannot be determined. Although blood pressure was measured by trained professionals, hypertension status and control are based on a single evaluation. Potential white coat hypertension that varies by USOC status could have overestimated or underestimated the effect of USOC on hypertension control. Moreover, if such white coat hypertension varied by age groups, that may have altered the differential marginal effect of USOC on hypertension control across the age groups. In terms of endogeneity, it is possible that those with controlled hypertension may be more likely to report a USOC or have other unmeasured factors that would overestimate the association between USOC and hypertension control in the US population. Finally, given the low sample size in the oldest age group without a USOC, statistical power is limited to draw more precise estimates.
Despite these limitations, the study remains robust given the control for major confounders and sensitivity analyses that give a range of potential effect of USOC on hypertension control. In addition, the relationship between USOC and hypertension—and the differential effect of USOC on hypertension across age groups—was consistent across multiple models. Finally, this is a nationally representative sample that has high external validity.
This study supports the positive effect of USOC on hypertension control in the US population and the changing dynamic of a USOC on hypertension control across age groups. The morbidity, mortality, and costs from hypertension in the general US population are enormous, with poor outcomes as people age. Thus, discovering the beneficial role that having a USOC plays in hypertension control across the entire population is key to assist with policy decisions to improve access to regular sources of care. In addition, the varying impact of USOC on hypertension control across age groups may reflect a need to change strategies to control blood pressure in different age groups. Specifically, a focus on improving health behaviors in younger individuals may involve focusing on antihypertensive medication initiation and compliance, regular follow-up, and cessation of smoking. Conversely, given that effect of having a USOC on blood pressure control is diminished in the oldest population, more information is needed to discover what strategies will most effectively improve health outcomes in the oldest and most vulnerable. Given shifting guidelines and newer data from the Systolic Blood Pressure Intervention Trial (SPRINT) suggesting lower blood pressure targets have improved cardiovascular morbidity and mortality outcomes in higher risk patients,37 it will be important to continue to monitor hypertension control and the cardiovascular sequelae in those most susceptible to poor outcomes.
DISCLOSURE
The authors declared no conflict of interest.
ACKNOWLEDGMENTS
Dr Dinkler receives grant funding from the National Institutes of Health (T32HL007895-16).
REFERENCES
- 1. Mozaffarian D, Benjamin EJ, Go A, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation 2015; 131:e29–e322. [DOI] [PubMed] [Google Scholar]
- 2. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green L, Izzo JL, Jones DW, Materson BJ, Oparil SW, Jackson TR, Edward J. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 3. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Jr., Svetkey LP, Taler SJ, Townsend RR, Wright JT, Jr., Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520. [DOI] [PubMed] [Google Scholar]
- 4. Peterson E. The burden of angina pectoris and its complications. Clin Cardiol 2007; 30:i10–i15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 6. Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D’Agostino RB, Levy D. Residual lifetime risk for developing hypertension in middle-aged women and men: the Framingham Heath Study. JAMA 2002; 287:1003–1010. [DOI] [PubMed] [Google Scholar]
- 7. Blewett LA, Johnson PJ, Lee B, Scal PB. When a usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med 2008; 23:1354–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Xu KT. Usual source of care in preventive service use: a regular doctor versus a regular site. Health Serv Res 2002; 37:1509–1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Devoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health 2003; 93:786–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ettner SL. The timing of preventive services for women and children: the effect of having a usual source of care. Am J Public Health 1996; 86:1748–1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. He J, Munter P, Chen J, Roccella EJ, Streiffer RH, Whelton PK. Factors associated with hypertension in the general population of the United States. Arch Intern Med 2002; 162:1051–1058. [DOI] [PubMed] [Google Scholar]
- 12. Spatz ES, Ross JS, Desai MM, Canavan ME, Krumholz HM. Beyond insurance coverage: usual source of care in the treatment of hypertension and hypercholesterolemia. Data from the 2003-2006 National Health and Nutrition Examination Survey. Am Heart J 2010; 160:115–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, Curtin LR. National Health and Nutrition Examination Survey: analytic guidelines, 1999–2010. National Center for Health Statistics. Vital Health Stat 2013; 2:1–24. [PubMed] [Google Scholar]
- 14. Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Questionnaire. US Department of Health and Human Services, Centers for Disease Control and Prevention: Hyattsville, MD, 2011. –2012. http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Accessed 10 January 2016. [Google Scholar]
- 15. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 2011; 43:1334–1359. [DOI] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention. State-specific secondhand smoke exposure and current cigarette smoking among adults―United States, 2008. MMWR Morb Mortal Wkly Rep 2009; 58:1232–1235. [PubMed] [Google Scholar]
- 17. Karaca-Mandic P, Norton EC, Dowd B. Interaction terms in nonlinear models. Health Serv Res 2012; 47:255–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Horton N, Kleinman K. Much ado about nothing: a comparison of missing data methods and software to fit incomplete data regression models. Am Stat 2007; 61:79–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Van Buuren S, Brand J, Groothius-Oudshoorn C, Rubin D. Fully conditional specification in multivariate imputation. J Stat Comput Simul 2006; 76:1049–1064. [Google Scholar]
- 20. Van Buuren S, Boshuizen H, Knook D. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med 1999; 18:681–694. [DOI] [PubMed] [Google Scholar]
- 21. White I, Daniel R, Royston P. Avoiding bias due to perfect prediction in multiple imputation of incomplete categorical variables. Comput Stat Data Anal 2010; 54:2267–2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kerse N, Buetow S, Mainous A, Young G, Arroll B. Physician patient relationship and medication compliance: a primary care investigation. Ann Fam Med 2004; 2:455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mainous AG, III, Baker R, Love M, Gray DP, Gill J. Continuity of care and trust in one’s physician: evidence from primary care in the United States and the United Kingdom. Fam Med 2001; 33:22–27. [PubMed] [Google Scholar]
- 24. Egan BM, Li J, Qanungo S, Wolfman TE. Blood pressure and cholesterol control in hypertensive hypercholesterolemic patients. A report from NHANES 1988–2010. Circulation 2013; 128:29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States, 1999 to 2012: progress toward Healthy People 2020 goals. Circulation 2014; 130:1692–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Samieri C, Sun Q, Townsend M, Chiuve SE, Okereke OI, Willett WC, Stampfer M, Grodstein F. The association between dietary patterns at midlife and health in aging: an observational study. Ann Intern Med 2013; 159:584–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moser C, Spagnoli J, Santos-Eggimann B. Self-perceptions of aging and vulnerability to adverse outcomes at the age of 65–70 years. J Gerontol B Psychol Sci Soc Sci 2011; 66B:675–680. [DOI] [PubMed] [Google Scholar]
- 28. Sodergren M, Wang WC, Salmon J, Ball K, Crawford D, McNaughton SA. Predicting healthy lifestyle patterns among retirement age older adults in the WELL study: a latent class analysis of sex differences. Maturitas 2014; 77:41–46. [DOI] [PubMed] [Google Scholar]
- 29. Pronk NP, Anderson LH, Crain AL, Martinson BC, O’Connor PJ, Sherwood NE, Whitebird RR. Meeting recommendations for multiple healthy lifestyle factors. Prevalence, clustering, and predictors among adolescent, adult, and senior health plan members. Am J Prev Med 2004; 27:25–33. [DOI] [PubMed] [Google Scholar]
- 30. Dohi Y, Thiel MA, Bühler FR, Lüscher TF. Activation of endothelial L-arginine pathway in resistance arteries. Effect of age and hypertension. Hypertension 1990; 16:170–179. [DOI] [PubMed] [Google Scholar]
- 31. Hamilton CA, Brosnan MJ, McIntyre M, Graham D, Dominiczak AF. Superoxide excess in hypertension and aging: a common cause of endothelial dysfunction. Hypertension 2001; 37:529–534. [DOI] [PubMed] [Google Scholar]
- 32. Higashi Y, Kihara Y, Noma K. Endothelial dysfunction and hypertension in aging. Hypertens Res 2012; 35:1039–1047. [DOI] [PubMed] [Google Scholar]
- 33. Kanasaki K, Kitada M, Koya D. Pathophysiology of the aging kidney and therapeutic interventions. Hypertens Res 2012; 35:1121–1128. [DOI] [PubMed] [Google Scholar]
- 34. Arnold AC, Gallagher PE, Diz DI. Brain renin-angiotensin system in the nexus of hypertension and aging. Hypertens Res 2013; 36:5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Virdis A, Bruno RM, Neves MF, Bernini G, Taddei S, Ghiadoni L. Hypertension in the elderly: an evidence-based review. Curr Pharm Design 2011; 17:3020–3031. [DOI] [PubMed] [Google Scholar]
- 36. Egan BM, Li J, Wolfman TE, Sinopoli A. Demographic differences in concurrent vascular risk factor control in patients with diabetes: NHANES 1988–2010. J Am Soc Hypertens 2014; 8:394–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. The SPRINT Study Research Group. The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT). Clin Trials 2014; 11:532–546. [DOI] [PMC free article] [PubMed] [Google Scholar]