Abstract
There is a growing recognition of the importance of the commensal intestinal microbiota in the development and later function of the central nervous system. Research using germ-free mice (mice raised without any exposure to microorganisms) has provided some of the most persuasive evidence for a role of these bacteria in gut-brain signalling. Key findings show that the microbiota is necessary for normal stress responsivity, anxiety-like behaviors, sociability, and cognition. Furthermore, the microbiota maintains central nervous system homeostasis by regulating immune function and blood brain barrier integrity. Studies have also found that the gut microbiota influences neurotransmitter, synaptic, and neurotrophic signalling systems and neurogenesis. The principle advantage of the germ-free mouse model is in proof-of-principle studies and that a complete microbiota or defined consortiums of bacteria can be introduced at various developmental time points. However, a germ-free upbringing can induce permanent neurodevelopmental deficits that may deem the model unsuitable for specific scientific queries that do not involve early-life microbial deficiency. As such, alternatives and complementary strategies to the germ-free model are warranted and include antibiotic treatment to create microbiota-deficient animals at distinct time points across the lifespan. Increasing our understanding of the impact of the gut microbiota on brain and behavior has the potential to inform novel management strategies for stress-related gastrointestinal and neuropsychiatric disorders.
Keywords: microbiota-gut-brain axis, germ-free mouse, stress response, social development, cognitive dysfunction
Introduction
Medicine is magical and magical is art
Thinking of the Boy in the Bubble
“Boy in the Bubble” by Paul Simon, 1986
Humans and other animals share an inextricable and mutualistic relationship with a myriad of resident microorganisms, collectively known as the microbiota. These microbial species are present on all body surfaces, including the gastrointestinal (GI) tract, respiratory tract, skin, and urogenital tract (Costello et al., 2009). Research on the interactions between microorganisms and their host has largely and understandably been focused on those residing in the intestinal lumen, given that this is the most densely colonized and home to approximately 100 trillion bacteria (Frank and Pace, 2008). Over the last decade, numerous scientific discoveries have highlighted the role of the microbiota in critical processes, including digestion (Hooper and Gordon, 2001), immune responses (Bäckhed et al., 2005; Hooper and Macpherson, 2010), absorption of nutrients (Hooper and Gordon, 2001), growth (Nicholson et al., 2012), and metabolism (Tremaroli and Backhed, 2012). Until recently, little was known about the role of the microbiota in the regulation of the central nervous system (CNS); however, there is now a burgeoning body of evidence indicating that the gut microbiota also influences the brain and behavior (Rhee et al., 2009; Collins et al., 2012; Cryan and Dinan, 2012; Dinan and Cryan, 2012; Dinan et al., 2013; Foster and McVey Neufeld, 2013; Foster et al., 2015; Sampson and Mazmanian, 2015). These fascinating insights have largely been derived from the study of germ-free (GF) animals that effectively grow up in a sterile bubble and have provided conceptual impetus to the possibility of exploiting the gut microbiota as a therapeutic target.
The Microbiota-Gut-Brain Axis
The concept of the gut-brain axis has been recognized for some time and has been used as a framework to assess mechanisms by which bidirectional communication between these 2 systems occurs. More recently, this axis has been extended to include the contents of the intestinal lumen, and we now refer to the existence of a ‘microbiota-gut-brain axis’ (Rhee et al., 2009; Bercik, 2011; Cryan and O’Mahony, 2011; Cryan and Dinan, 2012; Burokas et al., 2015; Mayer et al., 2015), highlighting the increasingly appreciated importance of bacteria in this communication highway. While the necessity of commensal intestinal microbiota for the maintenance of optimal gut-brain function is no longer disputed, the exact mechanisms by which microbiota-gut-brain communication occurs are still largely unknown. It is probable that a number of systems are simultaneously involved in the transmission of information between microbiota and brain, and research has focused primarily on immune, neural, endocrine, and metabolic pathways as likely mediators in this bidirectional communication (Cryan and Dinan, 2012; Foster and McVey Neufeld, 2013; El Aidy et al., 2015; Janssen and Kersten, 2015; Mayer et al., 2015).
The human gut is extensively innervated, with approximately 50000 extrinsic and 100 million intrinsic sensory afferent neurons (Furness, 2006; Blackshaw et al., 2007), all of which function in proximity to the trillions of microorganisms housed in the intestinal lumen. It is thus unsurprising that neural pathways play a vital role in microbiota-gut-brain communication. The necessity of an intact vagal nerve for information regarding intestinal microbial status seems dependent upon the specific bacterial species in question, and while some studies have shown the vagus is vital for information transfer (Lyte et al., 2006; Bercik et al., 2011b; Bravo et al., 2011), others have found evidence of vagal independence (Bercik et al., 2010, 2011a). Intrinsic primary afferent neurons housed within the gut wall have also been shown to be responsive to changes in intestinal bacterial status (Kunze et al., 2009; Mcvey Neufeld et al., 2013).
Similarly, while rodent infection studies using subclinical doses of pathogenic bacteria have indicated that immune system activation is not always necessary to observe changes in brain neurochemistry and behavior (Lyte et al., 2006), there is clear evidence of the importance of an intact and functioning immune system in gut-brain communication (Macpherson and Harris, 2004; Bengmark, 2013; El Aidy et al., 2015).
The endocrine system too plays a role in the ability of bacteria to alter brain functioning (Lyte, 2013), and many studies have now demonstrated changes in endocrine signalling in models of intestinal dysbiosis (Sudo et al., 2004; Bercik and Collins, 2014) and also the ability to alter intestinal microbial contents following hypothalamic-pituitary-adrenal (HPA) axis activation (O’Mahony et al., 2009; De Palma et al., 2015; Golubeva et al., 2015).
The Microbiota in Health and Disease
Compelling clinical evidence exists supporting the view that a stable and diverse gut microbial composition is important for the maintenance of optimal health. Indeed, altered microbial profiles have been associated with numerous human illnesses, including cardiovascular disease (Koren et al., 2011; Howitt and Garrett, 2012; Karlsson et al., 2012; Tuohy et al., 2014; Hansen et al., 2015), irritable bowel syndrome (IBS) (Salonen et al., 2010; Tana et al., 2010; Jeffery et al., 2012; Wu, 2012), inflammatory bowel disease (Ananthakrishnan, 2015; Marchesi et al., 2015; Sheehan et al., 2015), obesity (Ley et al., 2006; Turnbaugh et al., 2009a; Tremaroli and Backhed, 2012), and type 2 diabetes (Qin et al., 2012; Vrieze et al., 2012; Karlsson et al., 2013). However, there is presently little data detailing a clear link between the gut microbiota and the clinical manifestation of CNS diseases, although mounting preclinical evidence highlights the necessity for such studies.
The impact of the microbiota on the CNS can be investigated by assessing behavior following various deliberate interventions. Infection with pathogenic bacteria heightens anxiety-like behavior and reduces cognitive abilities (Lyte et al., 1998, 2006; Goehler et al., 2008; Gareau et al., 2011). Similarly, antibiotic administration alters the gut microbial composition, which is accompanied by reduced anxiety-like behavior (Bercik et al., 2011a). Probiotics, live organisms that provide health benefits when consumed, improve cognition and attenuate heightened stress responsivity in both humans and rodents (Bravo et al., 2011; Messaoudi et al., 2011; Savignac et al., 2015). As such, we have recently coined the term “psychobiotic” to describe bacteria with beneficial effects on mental health (Dinan et al., 2013). Finally, behavioral traits such as anxiety can be transferred via fecal transplantation (Bercik et al., 2011a), although this field of research is still in its early stages.
Research using GF mice has arguably provided the most convincing evidence for a role of the microbiota in gut-brain signalling. GF studies have generated exciting data with the goal of directly answering the question: does the gut microbiota influence the nervous system? This review will summarize what the GF mouse model has revealed about the importance of the gut microbiota on the development and function of the CNS with a focus on neuropsychiatric disorders. Tables 1 and 2 detail what we currently know about how growing up in the absence of microorganisms alters behavior and brain function, respectively. In this review, we focus on the GF mouse, but it is worth noting that GF rats, pigs, flies, and fish have also been studied (Gordon and Wostmann, 1960; Gordon and Pesti, 1971; Luckey, 2012; Crumeyrolle-Arias et al., 2014; Wang and Donovan, 2015). GF mice are a powerful scientific tool allowing researchers to directly study the influence of the microbiota on CNS function and development. One of the main advantages to this model is that identified strains of bacteria, such as candidate psychobiotics, can be introduced into GF animals and their effects studied in isolation from other microbes. Furthermore, the gut microbiota of GF mice can be “humanized” by transplanting fecal microbiota from human patients or alternatively inoculated from animal models of disease (Turnbaugh et al., 2006, 2009b; Bercik et al., 2011a; Borody and Khoruts, 2012; Cryan and Dinan, 2012; Aroniadis and Brandt, 2013; Ridaura et al., 2013; Suez et al., 2014; Thaiss et al., 2014; Leone et al., 2015), thus enabling the study of the role of given combinations of bacteria on disease pathogenesis.
Table 1.
The Germ-Free Behavioral Profile
| Parameter | Phenotype | Strain and Sex | Test | Reversible? | Reference |
|---|---|---|---|---|---|
| Anxiety-like behavior | Decreased anxiety-like behavior | Swiss Webster (m) | OF | Arentsen et al., 2015 | |
| No change in anxiety-like behavior | Swiss Webster (m) BALB/c (m) |
SD | Bercik et al., 2011a | ||
| Decreased anxiety-like behavior | Swiss Webster (m) | LDB | Yes | Clarke et al., 2013 | |
| Increased anxiety like behavior | F344 rat (m) | OF | Crumeyrolle-Arias et al., 2014 | ||
| Altered anxiety-like behavior | C57BL/6N (m & f) | LD: decreased anxiety SD: increased anxiety |
De Palma et al., 2015 | ||
| No change in anxiety-like behavior | Swiss Webster (f) | LDB | Gareau et al., 2011 | ||
| Decreased anxiety-like behavior | NMRI (m) | OF, LDB, EPM | Yes: EPM No: LDB, OF |
Heijtz et al., 2011 | |
| Decreased anxiety-like behavior | Swiss Webster (f) | EPM | Neufeld et al., 2011 | ||
| Learning & memory | No change in olfactory memory | Swiss Webster (m) | STFP | Desbonnet et al., 2014 | |
| Impaired short-term recognition and working memory | Swiss Webster (f) | NOR, TM | Gareau et al., 2011 | ||
| Locomotor behavior | Increased locomotor and rearing behaviors | NMRI (m) | OF | Yes | Heijtz et al., 2011 |
| No change in locomotor activity | Swiss Webster (f) | – | Neufeld et al., 2011 | ||
| Self-grooming | Increased self-grooming time | Swiss Webster (m) | – | Desbonnet et al., 2014 | |
| Social cognition | No preference for novel vs familiar mouse | Swiss Webster (m>f) | TCS | Yes | Desbonnet et al., 2014 |
| Social preference | Increased social interaction with conspecific | Swiss Webster (m) | TCS | Arentsen et al., 2015 | |
| Social avoidance of conspecific | Swiss Webster (m>f) | TCS | No | Desbonnet et al., 2014 |
Abbreviations: EPM, elevated plus maze; f, female; LDB, light-dark box; m, male; m>f, phenotype expressed more strongly in males than females; NOR, novel object recognition test; OF, open field test; SD, step-down test; STFP, social transmission of food preference test; TM, T-maze; TCS, 3-chambered sociability test.
Summary of the behavioral profile of GF mice. Experiments which are reversible or irreversible with bacterial colonization are indicated with ‘Yes’ or ‘No,’ respectively.
Table 2.
The Germ-Free Physiological Profile
| Category | Parameter | Phenotype | Strain and Sex | Tissue/Brain Region | Reversible? | Reference |
|---|---|---|---|---|---|---|
| Neurological disease- related effects | Amyloid-β | Decreased amyloid-β pathology | APPPS1 transgenic on C57BL/6 background (m & f) | Brain | Yes, only if colonized with SPF APPPS1 mouse microbiota | Harach et al., 2015 |
| EAE | Fully protected against developing EAE | SJL/J | CNS and immune tissue | Yes | Berer et al., 2011 | |
| EAE | Highly resistant to EAE | C57BL6/J (f) | CNS and immune tissue | Yes | Lee et al., 2011 | |
| Neuronal activity, plasticity & survival | Neuronal Activity | Decreased c-Fos expression after 1 hour of stress | Swiss Webster (f) | CA1 of the hippocampus | Gareau et al., 2011 | |
| Neurogenesis | Increased cell and neuron survival | Swiss Webster | Subgranular zone of the hippocampus | No | Ogbonnaya et al., 2015 | |
| Synapse-related genes | Decreased synaptophysin and PSD- 95 expression | NMRI (m) | Striatum | Heijtz et al., 2011 | ||
| Transcriptome | Differential expression | NMRI (m) | Cerebellum > hippocampus > striatum > cortex | Heijtz et al., 2011 | ||
| Transcriptome | Upregulation of genes associated with neuronal activity | Swiss Webster (m) | Amygdala | No | Stilling et al., 2015 | |
| Neuroprotection | Blood brain barrier | Increased permeability | NMRI (m) | – | Braniste et al., 2014 | |
| Microglia | Impaired immune response and immature morphology | C57BL/6 (m, f) | Corpus callosum, cortex, hippocampus, olfactory bulb, cerebellum | Yes | Erny et al., 2015 | |
| Neurotransmission | Dopamine receptor | Increased Drd1a expression | NMRI (m) | Hippocampus | Heijtz et al., 2011 | |
| Glutamate receptor | Decreased Nr1 expression | BALB/c (m) | Cortex | Sudo et al., 2004 | ||
| Glutamate receptor | Decreased Nr2 expression | BALB/c (m) | Cortex, hippocampus | Sudo et al., 2004 | ||
| Glutamate receptor | Decreased Nr2 expression | Swiss Webster (f) | Central nucleus of the amygdala | Neufeld et al., 2011 | ||
| Kynurenine:tryptophan ratio | Decreased kynurenine:tryptophan ratio | Swiss Webster (m, f) | Blood: plasma | Yes | Clarke et al., 2013 | |
| Monoamine Turnover | Increased turnover of noradrenaline, dopamine, and serotonin | NMRI (m) | Striatum | Heijtz et al., 2011 | ||
| Serotonin | Increased CNS serotonin levels | Swiss Webster (m) | Hippocampus | No | Clarke et al., 2013 | |
| Serotonin | Decreased peripheral serotonin levels | C57BL/6 | Colon | Yes | Yano et al., 2015 | |
| Serotonin Receptor | Decreased Htr1a expression | Swiss Webster (f) | Dentate gyrus of the hippocampus | Neufeld et al., 2011 | ||
| Tryptophan | Increased levels of tryptophan | Swiss Webster (m) | Blood: plasma | Yes | Clarke et al., 2013 | |
| Neurotrophin expression | BDNF | Reduced Bdnf expression | Swiss Webster (m) | Amygdala | Arentsen et al., 2015 | |
| BDNF | Reduced Bdnf expression | Swiss Webster (m) | Hippocampus | Clarke et al., 2013 | ||
| BDNF | Reduced BDNF expression | Swiss Webster (f) | CA1 of the hippocampus | Gareau et al., 2011 | ||
| BDNF | Reduced Bdnf expression | NMRI (m) | Basolateral amygdala, CA1 of the hippocampus, cingulate cortex | Heijtz et al., 2011 | ||
| BDNF | Increased Bdnf expression | Swiss Webster (f) | Dentate gyrus of the hippocampus | Neufeld et al., 2011 | ||
| BDNF | Reduced BDNF expression | BALB/c (m) | Cortex, hippocampus | Sudo et al., 2004 | ||
| NGFI-A | Decreased Ngfi-a expression | NMRI (m) | Amygdala hippocampus, prefrontal cortex, striatum | Heijtz et al., 2011 | ||
| Stress hormone signalling | ACTH | Increased ACTH after 1 hour of restraint stress | BALB/c (m) | Blood: plasma | Yes | Sudo et al., 2004 |
| Corticosterone | Increased corticosterone after 30 minutes of stress | Swiss Webster (m, f) | Blood: plasma | Clarke et al., 2013 | ||
| Corticosterone | Increased corticosterone after open field stress | F344 rat (m) | Blood: serum | Crumeyrolle-Arias et al., 2014 | ||
| Corticosterone | Increased basal corticosterone | Swiss Webster (f) | Blood: plasma | Neufeld et al., 2011 | ||
| Corticosterone | Increased corticosterone after 1 hour of restraint stress | BALB/c (m) | Blood: plasma | Yes | Sudo et al., 2004 | |
| Glucocorticoid receptor | Decreased glucocorticoid mRNA expression | BALB/c (m) | Cortex | Sudo et al., 2004 |
Abbreviations: ACTH, adrenocorticotropic hormone; BDNF, brain-derived neurotrophic factor; EAE, experimental autoimmune encephalomyelitis; NGFI-A, nerve growth factor-inducible clone; PSD-95, post-synaptic density protein 95.
Summary of the molecular and cellular profile of GF mice. Experiments which are reversible or irreversible with bacterial colonization are indicated with ‘Yes’ or ‘No,’ respectively.
Germ-Free Life: Past and Present
A common approach used to gauge the key functions of an organ or brain structure involves abolishing its contribution either surgically or by other means. For example, the function of a brain region can be determined by studying the deficits that follow lesioning the area in question. It was therefore not surprising for biologists studying the effects of bacteria on health and disease to ask how the host would be affected by the absence of microbiota. To help answer this question, GF animals were generated.
Historically, the concept of gnotobiosis, where all forms of life present within an organism are known, can be attributed to Louis Pasteur. In 1885, he speculated that animals lacking bacteria would not be able to survive because of the close synergistic evolution of microbes and their hosts (Pasteur, 1885; Gordon and Pesti, 1971). After the Second World War, and following the advent of antibiotics, a life without microbes became a popular topic of discussion (Kirk, 2012). By the 1960s, GF life was prominently featured in medical, scientific, and popular press, often represented as the futuristic mixture of fact and fiction. In the early years of space exploration, scientists recognized that extraterrestrial ventures could introduce terrestrial microorganisms to space and, conversely, extraterrestrial microorganisms to earth with potentially devastating outcomes (Wolfe, 2002; Kirk, 2012). It was thus suggested that GF men may be necessary to explore space. This idea entered public awareness with Michael Crichton’s The Andromeda Strain, which narrated a fictional battle against a deadly extraterrestrial pathogen introduced to earth as a result of man’s travels in space (Crichton, 1993). Life without microbes has continued to garner interest in popular culture, perhaps most notably with David Vetter, a patient with severe combined immunodeficiency who was raised isolated in sterile conditions and became known as the Bubble Boy (Lawrence, 1985; Kirk, 2012).
The first GF animals, guinea pigs, were generated by aseptic caesarean section at the end of the nineteenth century and kept GF for 2 weeks (Nuttall and Thierfelder, 1897). GF research programs developed independently at 3 different institutions, definitively proving that life is possible, albeit not desirable, without microbes. In the mid-twentieth century, a group headed by James Reyniers at the University of Notre Dame was the first to rear successive generations of GF rodents (Reyniers et al., 1946; Reyniers, 1959). Around the same time, Bengt Gustafsson at the University of Lund in Sweden also generated GF animals with a novel rearing isolator system (Gustaffson et al., 1957; Gustafsson, 1959a). A third GF program later began at the University of Nagoya led by Masasumi Miyakawa (Miyakawa, 1959). GF technology was applied to various other fields. For example, GF techniques were utilized in the maternity ward, the general hospital, and the operating theater to prevent cross-infection (Reyniers, 1942, 1943; Kirk, 2012). In industrialized farming, GF animals were reared to create herds free of pathogens that slow livestock growth and to aid in veterinary practices (Betts and Trexler, 1969; Kirk, 2012). Perhaps most notoriously, GF technology was used to protect immunocompromised newborns, creating GF humans (Barnes et al., 1968, 1969a, 1969b; Lawrence, 1985; Kirk, 2012). However, despite GF technology’s numerous uses, it has failed to become widely implemented outside of the laboratory.
The current methodology underlying the generation of GF animals remains largely unchanged since it was first pioneered by Reyniers. To generate the initial GF colony, pups are carefully delivered via Caesarean section to avoid contamination with the microbes living on the mother’s vagina and skin (Gustafsson, 1959a; Reyniers, 1959; Macpherson and Harris, 2004; Smith et al., 2007; Faith et al., 2010; Bibiloni, 2012; Stilling et al., 2014b). Newly born animals are then hand-reared in an aseptic isolator. Subsequent generations of GF animals can be obtained through a much simpler process: GF mice are interbred and mothers can give birth naturally in the isolator without exposing the new litter to any microorganisms (Gustafsson, 1959a; Reyniers, 1959; Macpherson and Harris, 2004; Smith et al., 2007; Faith et al., 2010). Most commercially available GF animals generated in this way can be shipped in a sterile container for transfer to local GF facilities. An alternative method involves the transfer of an embryo at the 2-cell stage into a pseudo-pregnant GF mother (Smith et al., 2007; Faith et al., 2010; Bibiloni, 2012). Colonies are maintained in aseptic isolators in a GF unit where the food, water, and bedding are sterile. A technician swabs the cages and analyzes fecal samples using bacterial culture techniques weekly to confirm that the GF unit is indeed sterile (Bibiloni, 2012; Williams, 2014). These methods make certain that GF mice never come into contact with any bacteria, not only in their gut but also on any other body surface. It is worth noting the logistical difficulties that limit the study of GF mice: conduction of complex interventions and behavioral assessments must be performed in the isolator unit if these animals are to remain free of microbes. To avoid these limitations, most GF studies are often executed shortly after the animals are removed from isolation, before bacterial colonization can have an effect.
The Germ-Free Mouse and Health
The extent to which Pasteur was correct in his assertions of the importance of the microbiota for an organism’s health is now clear; GF animals are functionally and structurally abnormal across numerous body systems. GF research has revealed that the microbiota is necessary for normal aging and immune, metabolic, digestive, GI, and nervous system function (Grenham et al., 2011).
Aging
There is growing evidence indicating that the gut microbiota influences the aging process. Indeed, GF mice live longer than conventionally colonized control animals (Reyniers and Sacksteder, 1958; Gordon et al., 1966; Tazume et al., 1991). As GF mice are raised in sterile conditions, their longer life span is likely due to the absence of pathological infections. In humans, microbial diversity and stability decrease with age and are accompanied by cognitive decline (O’Toole and Claesson, 2010; Borre et al., 2014). These findings have prompted the idea that restoring microbial diversity in the elderly could improve general and mental health.
Figure 1.
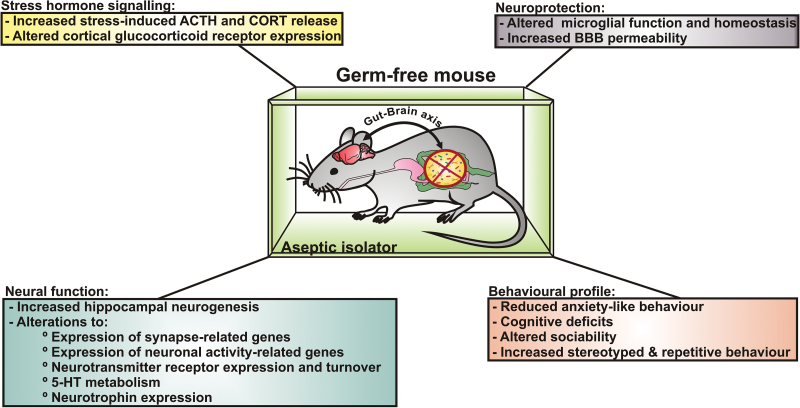
Germ-free (GF) mice as a tool to study the microbiota-gut-brain axis. GF mice are raised in isolation in a GF unit without any exposure to microorganisms. Gut-brain signalling is altered due to the lack of bacterial exposure throughout the lifetime. The microbiota is required for normal stress responsivity, anxiety-like behaviors, sociability, and cognition. Furthermore, the microbiota protects CNS homeostasis by regulating immune function and blood brain barrier (BBB) integrity.
Immune and Gastrointestinal Function
The gut microbiota is necessary for the normal function of the mucosal immune system. Toll-like receptors (TLRs) recognize pathogen-associated molecular patterns in the gut, differentiating pathogenic bacteria from harmless commensal microorganisms (Akira and Hemmi, 2003). GF animals have decreased or absent expression of certain TLRs, reduced IgA secretion, and fewer and smaller Peyer’s patches, which are the lymphoid follicles in the intestinal wall (Abrams et al., 1962; Wostmann et al., 1970; Shanahan, 2002; Grenham et al., 2011). The immune response of GF mice is blunted: animals produce less of the proinflammatory cytokine tumor necrosis factor α after splenocyte stimulation with lipopolysaccharide (Clarke et al., 2013). Intriguingly, colonization of GF animals rescues mucosal immune system function (Umesaki et al., 1995). Together, these findings indicate that exposure to bacteria is necessary to mount a normal immune response.
Studies in GF mice have demonstrated that the gut bacteria are required for the normal function and structure of the GI system. In GF mice, the cecum is enlarged, the intestinal surface area and number of villi are reduced, and Peyer’s patches are smaller and fewer (Wostmann and Bruckner-Kardoss, 1959; Gordon and Bruckner-Kardoss, 1961; Abrams et al., 1962; Shanahan, 2002). Moreover, enterochromaffin cells, the cells that produce serotonin in the GI tract (a key regulator of GI motility and secretion), are larger in GF animals (Shanahan, 2002) although not greater in abundance (Reigstad et al., 2015). Despite increases in cellular size, microbial metabolites dictate serotonin synthesis, and lower levels of this neurotransmitter have been noted in GF animals (Reigstad et al., 2015; Yano et al., 2015). GF mice have a decreased rate of epithelial cell turnover in the intestine (Rakoff-Nahoum et al., 2004). This likely results in reduced protection against GI insults, since epithelial cell turnover promotes healing (Grenham et al., 2011). The intestine secretes antimicrobial factors in response to TLR activation (Vaishnava et al., 2008); therefore, the reduction of certain TLRs in GF animals may also render them more susceptible to infection by pathogenic bacteria should they be exposed.
Metabolic and Digestive Function
The gut microbiota is involved in key metabolic processes. GF mice consume more food than control animals to maintain the same body weight (Wostmann et al., 1983). Moreover, GF mice remain resistant to diet-induced obesity even when they are fed a “Western” diet high in fat and sugar (Bäckhed et al., 2004, 2007; Ding et al., 2010; Rabot et al., 2010). This propensity for leanness in GF mice is accompanied by increased levels of fatty acid oxidation enzymes, indicating that the microbiota is involved in host metabolism and energy storage (Bäckhed et al., 2007). It is important to note, however, that not all studies support that GF mice are protected against diet-induced obesity. Using a different strain of mice, Fleissner and colleagues (2010) confirmed that GF mice were resistant to the obesigenic effects of a Western diet but not of a low-sucrose, lard-based, high-fat diet. These findings indicate that diet composition and possibly genetic strain could influence the protection against diet-induced obesity afforded by the GF state (Shen et al., 2013).
The gut microbiota releases nutrients from otherwise unavailable oligosaccharides, modulates absorption, and synthesizes essential nutrients (Sekirov et al., 2010; Grenham et al., 2011).Therefore, it is unsurprising that the absence of microbiota also affects digestion. GF rodents have reduced production of short chain fatty acids, which are beneficial to host metabolism and are produced when dietary fiber is fermented by bacteria (Høverstad and Midtvedt, 1986; den Besten et al., 2013). GF rats have deficient thiamine absorption: when these animals are fed radio-labeled thiamine, large quantities of the nutrient are found in the feces but little is found in the tissue (Wostmann et al., 1962). GF rats fed a diet without vitamin K rapidly become haemorrhagic and also require their diet to be supplemented with vitamin B to survive (Gustafsson, 1959b; Sumi et al., 1977). The gut microbiota is therefore required to synthesize vitamin K and B in the absence of these nutrients from the diet. To prevent nutritional deficiencies, the diet fed to GF mice is fortified with vitamins K and B (Grenham et al., 2011).
Enteric Nervous System Function
The changes that have been reported in CNS development and function in GF mice are reflected in the enteric nervous system (ENS), which is not surprising given that the cells found here are the first neural point of contact for commensal intestinal bacteria. Microbiota are necessary for the normal postnatal development of the enteric sensory and motor neurons, and at postnatal day 3, the structure, neurochemical composition, and function of enteric neurons in the jejunum and ileum of GF mice differ from controls (Collins et al., 2014). In the small intestine, GF mice have decreased overall nerve density, with fewer neuronal cell bodies in myenteric ganglia and less connective nerve fibers between ganglia (Collins et al., 2014). The ganglia of intrinsic sensory neurons of the ENS are embedded in the gut wall (Forsythe and Kunze, 2013), and it has been established that the electrophysiological properties of these myenteric sensory neurons, or afterhyperpolarization (AH) neurons, are altered in the absence of colonizing bacteria (Mcvey Neufeld et al., 2013; McVey Neufeld et al., 2015). Specifically, the AH period of the AH cells, during which the neuron is refractory to further firing, is elongated in GF mice when compared with both controls and adult conventionalized GF mice. In other words, the gut sensory neurons are less excitable under GF conditions. These same neurons are responsive to feeding of the probiotic Lactobacillus rhamonus (JB-1) in healthy rats, showing an increase in excitability after treatment (Kunze et al., 2009). Interestingly, GF rats have altered intestinal motility (Husebye et al., 1994, 2001), and these sensory neurons synapse on enteric motor neurons controlling gut motility, so this may provide a potential mechanistic explanation for the dysfunction. The AH sensory neurons also synapse, both anatomically and functionally, with vagal nerve endings in the gut (Powley et al., 2008; Perez-Burgos et al., 2014) and thus could represent a direct neural route whereby the intestinal bacterial status is transmitted to the brain. This hypothesis is consistent with the findings of alterations in extracellular recordings from mixed vagal and spinal nerve afferents in GF mice compared with both control and adult conventionalized GF animals (McVey Neufeld et al., 2015).
Stress Responsivity and Anxiety-Like Behavior
There is now a growing body of literature supporting the role of the gut microbiota in the regulation and development of the stress response system (Rhee et al., 2009; Collins et al., 2012; Dinan and Cryan, 2012; Foster and McVey Neufeld, 2013; Sampson and Mazmanian, 2015). Signals from the gut are well known to activate the HPA axis: both infection by pathogenic bacteria and stimulation of the vagus nerve elicit corticosterone release (Hosoi et al., 2000; Zimomra et al., 2011). Altered microbiota-brain-gut signalling is thought to play a role in the pathogenesis of GI disorders; patients with IBS have both an altered gut microbiota composition and irregular HPA axis activity (Jeffery et al., 2012; Kennedy et al., 2014a, 2014c). However, the evidence relating abnormal gut function to maladaptive responses to stressors is limited as of yet. Most of what is currently known about the regulation of stress responsivity by the gut microbiota has been discovered from preclinical rodent models.
Hypothalamic-Pituitary-Adrenal Axis Responsivity
Studies in GF mice have revealed that the microbiota influences the development of the HPA axis. The landmark study by Sudo et al. (2004) was the first to demonstrate that acute restraint stress induces an exaggerated release of corticosterone in GF mice compared with specific pathogen-free controls (SPF; mice guaranteed to not harbor certain pathogens). This HPA axis hyperactivity is completely normalized when GF mice are monocolonized with Bifidobacterium infantis in the neonate period (Sudo et al., 2004). However, monocolonization with the enteropathogenic bacteria Escherichia coli induces even higher stress hormone release in GF mice. These contrasting findings indicate that there are bacterial strain-specific effects on stress responsivity. Intriguingly, stress-induced corticosterone release is partially normalized by bacterial colonization occurring at 6 but not at 8 weeks (Sudo et al., 2004), demonstrating that there is a critical window prior to adolescence during which the brain is sensitive to signals from the gut required for the normal development of the HPA axis. Increased stress-induced corticosterone release has also been reported in GF rats (Crumeyrolle-Arias et al., 2014). There is conflicting evidence as to whether basal corticosterone levels are altered in GF mice: both increased (Neufeld et al., 2011) and normal (Sudo et al., 2004; Clarke et al., 2013) levels have been documented. These contrasting findings are likely due to fact that the strain, sex, mode of euthanasia, and acclimatization period differs between studies.
Stress Circuitry
Although it is now clear that microbiota-gut-brain signalling is involved in programming stress responsivity, little as of yet is known about the underlying neural circuitry. To determine if the normalization of HPA axis signalling occurs through an immunological or neural route, Sudo and colleagues (2004) colonized GF mice with B. infantis at 5 weeks of age and measured cytokine release and activation of the paraventricular nucleus (PVN) of the hypothalamus. Inoculation with B. infantis induces corticosterone release and activates the PVN, as quantified by a marker for neuronal activation (c-Fos). Inoculation also induced the release of the proinflammatory cytokine interleukin-6. However, this effect seems to be independent of stress hormone release, since pretreatment with an anti-interleukin-6 antibody fails to affect corticosterone levels or activate the PVN. Taken together, these results suggest that stress-relevant signals from the gut microbiota are relayed to the brain through a neuronal, humoral cytokine-independent pathway.
Anxiety-Like Behavior
The logical question arising from the discovery of HPA axis hyperactivity in GF mice was if stress-related behaviors were also under the influence of the microbiota. A number of independent laboratories have shown that GF mice exhibit a reduction in basal levels of anxiety-like behavior (Heijtz et al., 2011; Neufeld et al., 2011; Clarke et al., 2013; Arentsen et al., 2015). However, it is also worth noting that some studies report no change in anxiety-like behavior in GF mice (Bercik et al., 2011a; Gareau et al., 2011). The stress-related behavioral profile of GF mice appears to be amenable to microbial intervention: the colonization of GF mice normalizes anxiety-like behavior (Clarke et al., 2013). Curiously and perhaps more consistent with the exaggerated stress response, GF status in rats is anxiogenic, suggesting that growing up GF has a species-specific directional effect on anxiety levels (Crumeyrolle-Arias et al., 2014). Finally, the gut microbiota is required for the induction of the anxiogenic profile associated with early-life stress: unlike in conventionally colonized mice, anxiety-like behavior of GF mice is unaffected by maternal separation (De Palma et al., 2015).
One of the principle advantages of the GF model is that it allows the researcher to colonize mice with bacteria and study the effects on host physiology and behavior. The transfer of microbiota from the high anxiety-like Balb/C mouse strain to low anxiety-like GF NIH Swiss mice is anxiogenic in the recipient (Belzung and Griebel, 2001; O’Mahony et al., 2010; Bercik et al., 2011a). The same is true of the reverse transplantation: NIH Swiss bacteria transferred into GF Balb/C attenuate the recipients’ anxious phenotype (Bercik et al., 2011a). These results suggest that the composition of the gut microbiota may contribute to the behavioral and physiological aspects of GI disorders. For example, patients with IBS display exaggerated HPA axis responses to an acute stressor, an altered composition of gut microbiota, and a high psychiatric comorbidity most commonly with mood disorders (Fond et al., 2014; Kennedy et al., 2014b, 2014c). Targeting the microbiota with interventions such as probiotics could therefore improve both the GI and psychiatric symptoms of IBS and related psychosomatic illnesses (Clarke et al., 2012). Furthermore, given that microbial transfer can alter stress responsivity, fecal microbiota transplantation may be a viable therapy for disorders for the microbiota-brain-gut axis (Borody and Khoruts, 2012; Aroniadis and Brandt, 2013). This is currently an active area of research, but it remains to be seen if the high success rates for those with recurrent Clostridium difficile infection will also be reflected in more complex and heterogeneous GI disorders.
Sociability, Self-Grooming, and Locomotion
Living among groups affords an evolutionary advantage, providing mutual protection, sharing of food, and more opportunities to mate (Hamilton, 1964; Stilling et al., 2014a). It is therefore logical that the brain has evolved to foster social interaction. Microbes are contagious; they can spread to new hosts and environments through active or passive interactions. This trait has led scientists to hypothesize that natural selection has favored bacterial species that can maximize their own transmission, including during host social interaction (Troyer, 1984; Lombardo, 2008; Ezenwa et al., 2012; Montiel-Castro et al., 2013; Tung et al., 2015). The exchange of microbes between conspecifics is also advantageous for the host: symbiotic bacteria can protect against pathogenic infection and assist in digestion and nutrient absorption (Troyer, 1984; Lombardo, 2008; Stilling et al., 2014a). It can thus be hypothesized that both sociability and bacteria have had profound and convergent influences on the evolution of brain and behavior.
Sociability
Our group has investigated the interaction between the microbiota and social behavior (Desbonnet et al., 2014). Under normal conditions, mice will seek out social situations that are novel and stable. However, in the 3-chambered sociability test, GF mice spend more time exploring an empty chamber than a chamber containing a mouse (social preference). In addition, GF mice do not display the expected partiality for a novel over a familiar mouse (social cognition). Both social deficits are more pronounced in male GF mice. The postweaning colonization of GF mice successfully reverses the impairment in social preference but not social cognition; colonized GF mice prefer the chamber containing a mouse but display no preference for a novel compared with a familiar mouse. Taken together, this study demonstrates that microbes are required for normal sociability. Moreover, it shows that social cognition is permanently developed by the preweaning period; however, the critical window during which social preference is susceptible to microbial-based interventions appears to be longer.
In contrast to the results described above, a recent study by Arentsen and colleagues (2015) found that GF mice display increased social preference. The reason for these conflicting findings is unclear: the mouse strain, sex, and 3-chambered sociability test protocol were the same between studies. The authors propose that differences in the age of the GF mice and in the strain of novel mouse may account for the contrasting results. Moreover, the control SPF mice used by Arentsen et al. (2015) were housed in isolators, whereas the control mice used by Desbonnet et al. (2014) were not. The marked hyperactivity responses seen in the Arenston et al. (2015) study may also play a role. Regardless of the disparity between these results, the 2 studies are in agreement that a gut microbiota is required for normal social behavior in mice.
Self-Grooming and Locomotion
In addition to the observed deficits in sociability, male GF mice engage in more stereotyped, repetitive self-grooming behaviors compared with controls (Desbonnet et al., 2014). These animals also display increased locomotor activity and rearing (Heijtz et al., 2011). However, there are no locomotor changes in female GF mice (Neufeld et al., 2011). Where such changes have been noted, postweaning colonization normalizes abnormal self-grooming, locomotion, and rearing in GF mice (Heijtz et al., 2011; Desbonnet et al., 2014). These results indicate that the microbiota influences the neural networks controlling stereotyped, repetitive, and locomotor behaviors.
The Germ-Free Mouse: Parallels to Autism Spectrum Disorder
The observed alterations in sociability, locomotor activity, and repetitive, stereotyped behaviors in GF mice have particular significance for autism spectrum disorder (ASD). ASD is characterized by impaired sociability and communication and by frequent repetitive and stereotyped behaviors. Intriguingly, patients with ASD have an altered composition of the gut microbiota and commonly suffer from GI complications such as constipation and increased intestinal permeability (Howard et al., 2000; Kang et al., 2013; Mulle et al., 2013; Mayer et al., 2014; Rosenfeld, 2015; Sampson and Mazmanian, 2015). Furthermore, there is a higher prevalence of inflammatory bowel disease and GI illnesses in individuals with ASD (Kohane et al., 2012). Taken together, these findings implicate the microbiota in the pathogenesis of this neurodevelopmental disorder.
Interestingly, the behavioral and physiological profile of rodent models of ASD is comparable with that of GF mice. Maternal immune activation in mice reduces sociability and heightens both anxiety-like and stereotyped behaviors of the offspring (Hsiao et al., 2013). These animals also have deficient intestinal integrity and an altered composition of gut microbiota (Hsiao et al., 2013). Importantly, many of these behavioral and GI impairments in mice exposed to maternal immune activation can be ameliorated by administering B. fragilis (Hsiao et al., 2013). These behavioral and GI deficits have also been noted in another mouse model of autism: mice exposed to valproate in utero show both impaired sociability and an altered gut microbiome (de Theije et al., 2014). If the hypothesis that ASD has a microbial etiology proves correct, interventions targeting the gut microbiota such as diet and pro- and pre-biotics could provide safe and effective strategies for targeting neurodevelopmental disorders and their associated comorbidities (Gilbert et al., 2013; Mayer et al., 2014; Sampson and Mazmanian, 2015). ASD is of course too complex to be completely recapitulated in any one animal model (Mayer et al., 2014). These provocative results need to be integrated with the current genetic and environmental factors associated with the development of autistic behavior (Fakhoury, 2015). Interestingly, the early-life microbial disruption induced by Caesarean section delivery is associated with an only modestly increased ASD risk in epidemiological studies (Curran et al., 2015b) that may in fact be due to due to familial confounding (Curran et al., 2015a). Nevertheless, the preclinical data do suggest the potential of using microbial-based interventions to improve many of the prominent abnormal behaviors in ASD.
Learning and Memory
Given that the gut microbiota has pronounced effects on sociability and stress responsivity, it is perhaps unsurprising that it also regulates cognitive ability. Treatment of mice with a potential Lactobacillus probiotic improves memory (Savignac et al., 2015). This bacteria-induced memory enhancement may be due to changes in hippocampal activity: probiotic treatment prevents age-associated impairments in long-term potentiation in the rat hippocampus (Distrutti et al., 2014). In contrast, exposure to the enteric pathogen Citrobacter rodentium induces memory deficits in stressed mice (Gareau et al., 2011). To further explore the idea that the gut microbiota can influence cognition, Gareau and colleagues (2011) tested the learning and memory abilities of GF mice. To assess dorsal hippocampus-mediated memory, mice underwent a one-trial version of the novel object test that compares the frequency of exploration of a familiar vs a novel object between groups (Ennaceur and Delacour, 1988). In addition, the ability of mice to remember a familiar environment was tested using the T-maze test. In this test, memory is assessed by comparing left vs right arm entries, with an equal amount indicating the mice remember which arm they have previously explored. This study revealed that a gut microbiota is required for normal cognition, as GF mice spend less time exploring novel objects and environments compared with controls. However, olfactory memory in GF mice appears to be normal (Desbonnet et al., 2014). GF mice have less c-Fos-positive CA1 hippocampal cells after undergoing memory testing, indicating that these cognitive impairments may be due to a reduction in hippocampal activity. Together, this study indicates the absence of a gut microbiota impairs spatial and object, but not olfactory, memory abilities, possibly through altered hippocampal signalling tone. This is consistent with the molecular and neurochemical changes that have been noted in this important brain region in GF animals (see below).
Molecular and Neurochemical Changes in the Germ-Free Brain
Although studies of GF mice clearly demonstrate that the gut microbiota influences stress responsivity, sociability, and cognition, the molecular and neurochemical correlates of these effects remain largely unknown. Here, we summarize what is presently known about the microbial regulation of neurotransmission, neurotrophic factors, and synapse-related gene expression.
Serotonin
The neurotransmitter serotonin (5-hydroxytryptamine) regulates mood, appetite, sleep, and cognition (Wrase et al., 2006). Although it is principally known for its role in the CNS, approximately 95% of the body’s serotonin is found in the GI system, where it mediates pain perception and gut secretion and motility (Ridaura and Belkaid, 2015; Yano et al., 2015). Given the high comorbidity of GI and mood disorders, it makes sense that drugs targeting the serotonergic system effectively treat the symptoms of IBS and anxiety and depressive disorders (O’Mahony et al., 2015).
Tryptophan is an essential amino acid and a precursor for serotonin. Reduction in tryptophan levels results in deficient serotonin production and depressive-like symptoms (Myint et al., 2007). The gut microbiota is required for the normal breakdown and absorption of nutrients, which raises the possibility that both tryptophan levels and serotonergic signalling are altered in GF mice. Indeed, GF mice have elevated levels of plasma tryptophan compared with controls (Clarke et al., 2013). Increased hippocampal levels of serotonin are also found in male, but not female, GF mice. Importantly, colonization with bacteria postweaning normalizes tryptophan availability but not hippocampal serotonin levels (Clarke et al., 2013). Together, these findings indicate that the microbiota affects serotonergic signalling in the CNS, perhaps by altering peripheral tryptophan availability. Subsequent studies also suggest a degree of temporal specificity in this regulatory role (El Aidy et al., 2012). ENS serotonergic levels are also affected by microbial metabolites such as short-chain fatty acids (SCFAs) (Reigstad et al., 2015; Yano et al., 2015). Thus, serotonergic signalling in the “second brain” is also contingent on an intact gut microbiome (Ridaura and Belkaid, 2015). Since circulating serotonin levels are largely drawn from GI sources, this tallies with studies showing lower serum levels of serotonin in GF animals (Ridaura and Belkaid, 2015) and has implications beyond the gut given the expansive biology of serotonin (Berger et al., 2009).
Brain Derived Neurotrophic Factor
Brain derived neurotrophic factor (BDNF) promotes the growth and development of new neurons and the survival of existing neurons (Park and Poo, 2013). Altered levels of BDNF in the CNS are well known to be associated with affective disorders in humans (Autry and Monteggia, 2012). In GF mice, Bdnf expression is lower in the cortex and amygdala compared with controls (Heijtz et al., 2011). In the hippocampus, the changes in Bdnf levels documented are inconsistent: studies report both an increase (Neufeld et al., 2011) and a decrease in expression (Sudo et al., 2004; Gareau et al., 2011; Heijtz et al., 2011; Clarke et al., 2013). What is evident from these findings is that the microbiota influences BDNF expression in the CNS. How these microbiota-induced changes in neurotrophin factor expression affect the structure and function of the GF brain warrants further investigation.
Synapse-Related Transcriptome
Evidence that the microbiota acts on the brain at a synaptic level stems from differing expression of mRNA and proteins in GF vs control mice. In GF mice, the dopamine receptor subunit Drd1a is increased in the hippocampus (Heijtz et al., 2011). Moreover, the glutamate receptor subunit Nr1 is decreased in the cortex while Nr2 is reduced in the cortex, hippocampus, and central nucleus of the amygdala (Sudo et al., 2004; Neufeld et al., 2011). In the striatum, expression of the synaptic proteins synaptophysin and postsynaptic density protein-95 (PSD-95) is elevated (Heijtz et al., 2011). Our group has recently published data demonstrating that genes involved in neuronal activity are upregulated in GF mice, indicating potential amygdalar hyperactivity in these animals (Stilling et al., 2015). Although further experiments are required to fully understand how the microbiota regulates synaptic transmission and morphology, these results clearly indicate that brain regions important for sociability, stress responsivity, and cognition are altered on a synaptic level in GF mice.
Neurogenesis
Neurogenesis, the generation of new neurons, is a key process involved in memory formation, stress responsivity, and antidepressant treatment efficacy (Snyder et al., 2011; Marín-Burgin and Schinder, 2012; Miller and Hen, 2015). That anxiety-like behavior, HPA axis signalling, neurotrophic factor expression, and learning and memory differ in GF mice led us to hypothesize that adult hippocampal neurogenesis could also be influenced by the gut microbiota (Ogbonnaya et al., 2015). This study revealed that cell survival, but not proliferation, is increased in the subgranular zone of the hippocampus. Likewise, the survival of newly born neurons is increased in GF mice primarily in the dorsal hippocampus, a subregion preferentially involved in spatial memory (Moser et al., 1995; O’Leary and Cryan, 2014). This change in adult neurogenesis could therefore underlie the deficits in spatial learning and memory of GF mice. However, it is worth remarking that increased hippocampal neurogenesis is typically associated with improved cognitive ability (Deng et al., 2010). Postweaning colonization does not normalize any of the changes in cell and neuron survival, indicating that there may be a critical window prior to weaning during which neurogenesis is amenable to microbial intervention.
Blood Brain Barrier
The blood brain barrier (BBB) filters the passage of water-soluble molecules from the blood to the brain. The BBB is formed early in fetal life to protect the fetus against harmful toxins and bacteria during this sensitive period of brain development (Ballabh et al., 2004; Knudsen, 2004; Abbott et al., 2010). Disruption of the BBB can expose the CNS to damage and disease (Ballabh et al., 2004; Abbott et al., 2010). Understanding how the gut microbiota and its circulating metabolites affect the BBB may inform new strategies to prevent and treat BBB-associated neuropsychiatric disorders (Kelly et al., 2015).
To answer this question, Braniste et al. (2014) examined BBB development and function in GF mice. In fetal mice from SPF dams, the BBB prevents the penetration of labelled immunoglobulin; however, the BBB of fetal mice from GF dams allows the immunoglobulin to diffuse into the brain. As adults, the BBB of GF mice continues to be more permeable than that of their SPF counterparts. The authors propose that these changes in barrier function are due to tight junction abnormalities. Indeed, tight junction protein expression is reduced in both fetal and adult GF mice. Moreover, tight junctions in the brains of GF mice appear diffuse and disorganized. Colonization of adult GF mice with microbiota from SPF mice successfully reduces BBB permeability and increases tight junction protein expression. The effects of colonization on the BBB are likely mediated by SCFAs or metabolites produced by gut bacteria: monocolonization with a butyrate-producing bacterial strain or sodium butyrate administration alone decreases BBB permeability and increases tight junction expression. This study highlights the importance of the microbiota in BBB development: increased diffusion of molecules into the growing brain could affect neural connectivity and underlie the maladaptive behavioral and physiological profile of GF mice. More research is needed to determine if microbiota-directed interventions such as probiotics or dietary changes could effectively target BBB-related disorders and their associated comorbidities.
Microglia
Microglia are the resident macrophages of the CNS and act as the first line of immune protection for the brain and spinal cord. By scavenging infectious agents, damaged cells, and other potential toxins, these cells maintain CNS homeostasis (Ransohoff and Perry, 2009; Kettenmann et al., 2011; Prinz and Priller, 2014). Microglia are also involved in shaping neural circuits in the developing brain (Schafer and Stevens, 2013). A growing number of studies have associated microglia-related genes with neuropsychiatric disorders such as Alzheimer’s disease (AD) and dementia (Prinz and Priller, 2014), illnesses now termed microgliopathies.
Although the gut microbiota has long been known to impact the peripheral immune system, little was known until recently regarding its modulation of immune development and function in the CNS (Cryan and Dinan, 2015). To investigate the relationship between the microbiota and CNS immune function, Erny and colleagues (2015) studied the homeostasis and maturation of microglia in GF mice. Initial experiments revealed marked differences in mRNA expression profiles of microglial genes in GF mice. Further analyses confirmed that GF mice have more microglia throughout the entire brain compared with controls. The microglia of GF mice also have an abnormal morphology: processes are longer, more complex, and frequently overlap with other cells. In response to bacterial or viral challenge, proinflammatory gene expression is attenuated and microglia do not display an activated morphology in GF mice, indicating that a microbiota is required to mount an appropriate response to pathogenic infection in both the periphery and the CNS.
The above findings raise the possibility that microglia could require constant input from the host microbiota to maintain CNS homeostasis. To answer this question, Erny et al. (2015) investigated the effect of antibiotic-induced microbiota depletion on microglia of adult mice. Antibiotic-treated SPF mice exhibit an immature microglial profile similar to that of GF mice. Unlike GF mice, however, antibiotic treatment does not affect the number of microglia in the brain. Furthermore, it appears that a full repertoire of commensal microorganisms is necessary for normal microglial homeostasis: colonization with a complex composition of bacteria, but not a 3-strain Schaedler flora (select strains found in the normal mouse microbiota), normalizes microglial function and morphology in GF mice. Importantly, administration of SCFAs to GF mice almost completely restores microglia density, morphology, and maturity. This study elegantly demonstrates that SCFA signalling from a complex bacterial community is required for the normal structure and homeostatic function of the CNS immune system.
Neurological Disorders
To date, GF research has largely focused on the psychiatric disorders; however, there is now preliminary evidence that GF mice can also be useful tools in the study of neurological disorders. Recent studies have demonstrated that a GF state imparts a resistance to traits associated with multiple sclerosis (MS) and AD.
Multiple Sclerosis
MS is an autoimmune disease affecting myelin, the protective sheath that surrounds neurons of the CNS (Goverman, 2009; Mielcarz and Kasper, 2015). This damage can cause physical, cognitive, and sometimes psychiatric symptoms. The progression of MS likely involves both genetic and environmental factors (Becker et al., 1998; Willer et al., 2003; Dendrou et al., 2015). Recent studies have suggested that altered microbial stimulation of the immune system could be an environmental component of MS (Dendrou et al., 2015; Mielcarz and Kasper, 2015). Intriguingly, some microorganisms seem to potentiate MS in humans, while others have preventative effects (Ascherio, 2013).
The experimental autoimmune encephalomyelitis (EAE) animal model reproduces many of the characteristics of MS and is induced through immunization with CNS antigens in the presence of bacterial adjuvants (Stromnes and Goverman, 2006). When SPF mice are immunized with myelin oligodendrocyte glycoprotein peptides in complete Freund’s adjuvant, all animals develop signs of disease (Berer et al., 2011; Lee et al., 2011). Remarkably, GF are highly resistant to (Lee et al., 2011) or do not develop EAE at all (Berer et al., 2011). However, EAE responsivity is restored when GF mice are colonized with only segmented filamentous bacteria (Lee et al., 2011) or commensal microbiota from SPF mice (Berer et al., 2011). The absence of EAE in GF mice could be due to an altered balance in pro- and anti-inflammatory immune responses: GF mice produce lower levels of proinflammatory cytokines and anti-myelin oligodendrocyte glycoprotein autoantibodies, but higher levels of regulatory T cells (Berer et al., 2011; Lee et al., 2011). Taken together, these findings suggest that the modulation of the gut microbiota could represent novel therapeutic targets for inflammatory diseases such as MS.
Alzheimer’s Disease
AD is a chronic neurodegenerative illness and the most common cause of dementia in the Western world (Burns and Iliffe, 2009). The amyloid hypothesis posits that extracellular deposition of amyloid beta (Aβ) peptides triggers a cascade of pathological events, eventually leading to dementia (Hardy and Higgins, 1992; Ittner and Götz, 2011; Musiek and Holtzman, 2015). Although it is known that the composition of the gut microbiota changes as we age, the role of these microbes in the pathogenesis of age-related disorders such as AD remains to be explored (O’Toole and Claesson, 2010). To investigate a possible link with the gut microbiota, Harach and colleagues (2015) studied the amyloid deposition in transgenic AD mice raised GF. When raised with commensal microbiota, APPPS1 transgenic mice exhibit an age-dependent accumulation of Aβ plaques in the brain (Radde et al., 2006). In contrast, GF APPPS1 mice accumulate far less Aβ plaques in the CNS (Harach et al., 2015). This decrease in Aβ is accompanied by an increase in Aβ-degrading enzymes and a reduction in neuroinflammation, as measured by the microglial marker Iba-1 (Harach et al., 2015). Interestingly, the microbial composition of conventionally colonized APPPS1 mice differs from that of wild-type mice (Harach et al., 2015). Furthermore, only the transfer of microbiota from APPPS1 and not wild-type mice can effectively increase CNS Aβ levels in GF APPPS1 mice (Harach et al., 2015). These findings suggest that the gut microbiota may be involved in the development of AD pathology, and further experiments in this field are warranted.
Strengths, Limitations, and Alternatives to the Germ-Free Mouse Model
As humans are never in a truly GF state—even prenatally as previously hypothesized (Funkhouser and Bordenstein, 2013)—criticisms of the GF model usually revolve around its apparent lack of clinical relevance. It should be clear, however, that the use of GF animals in preclinical work is not to directly mimic the human condition. Arguably, we should instead focus on the strengths of the GF animals as models for understanding the role of bacteria on host development and function. Its artificially controlled state allows us to study the dysfunction arising in the absence of any microbial input on behavior, anatomy, and physiology. It also provides a clean background onto which we can add either a single strain of bacteria, such as in mono-colonization, or a predefined cocktail of commensal microbiota. Conventionalizing GF mice in this manner allows us to determine the impact of specific bacteria on any number of health-related issues. Vitally, bacteria can also be introduced to GF mice at various time points of host development, permitting us to examine the existence of critical windows of development that may require bacterial input. Indeed, this is currently an area of keen interest and the focus of many ongoing colonization experiments.
Given that GF animals have no bacterial exposure from conception onwards, they are perhaps of limited usefulness for experimental questions regarding the impact of altered microbiota composition that first occurs later in life. For these reasons, alternatives to the GF model must be explored that allow for alterations in bacterial exposure occurring throughout the lifespan. Some alternatives do currently exist and are being used to complement GF findings, including those using antibiotic treatment, probiotic feeding, fecal transplantation, and mouse humanization, among others. Antibiotic treatment of mice is regarded as a practical and potentially more relevant alternative to the use of GF mice, and, interestingly, many of the phenotypic features associated with the GF state (eg, reduced anxiety-like behaviors) are also evident after a sustained antibiotic-induced disruption of the gut microbiota. A recent study examining the long-term effects of antibiotic treatment and the resulting altered intestinal microbial composition focused on the critical developmental window of adolescence (Desbonnet et al., 2015). Here, treating mice with a combination of antibiotics resulted in reduced anxiety, reduced cognitive abilities, and social deficits. In addition, antibiotic-treated mice also displayed reduced levels of BDNF, oxytocin, and vasopressin in adult brain tissue (Desbonnet et al., 2015). Alterations to tryptophan metabolic pathways were also observed (Desbonnet et al., 2015). Earlier work involving administration of an antibiotic cocktail of bacitracin and neomycin as well as the anti-fungal primaricin to mice has demonstrated reduced anxiety-like behavior and increased hippocampal BDNF mRNA expression (Bercik et al., 2011a) as well as increased visceral sensitivity to colorectal distension tests that can be ameliorated after probiotic administration (Verdu et al., 2006). Researchers have also investigated the effects of introducing bacteria to mouse models of intestinal dysbiosis. Humanization studies can involve human fecal transfer to GF mice but have recently been broadened to include inoculating non-GF antibiotic-treated mice with human feces (Hintze et al., 2014). Mice treated in this fashion are not only useful in examining microbiota-gut-brain communication but provide a more clinically relevant model in which to ask questions regarding the effects of differing bacterial communities on the host. GF animals have been vital in helping us elucidate mechanisms of gut-brain communication, as well as the role of commensal microbiota in development and function of the organism. However, moving forward, alternatives to GF animals such as those elucidated above will provide us with a complementary understanding in a more obviously clinically relevant manner.
Conclusion
From the inception of studies using GF animals to today, we have garnered a significant body of knowledge with respect to bacterial-host communication in wellness and disease. Through the examination of GF animals both before and after introduction of bacteria, whether single-strain or as a bacterial community, we now know that host-bacterial communication is necessary for the optimal function of virtually all physiological processes in the organism. Bacteria are necessary for the healthy functioning of the immune, respiratory, GI, metabolic, endocrine, and nervous systems of the organism, and this has led many researchers to now consider humans (and most other organisms) as holistic functioning units working together with their bacterial counterparts. Moving forward, experiments using a variety of approaches to manipulate intestinal bacteria will be used to complement those carried out in the GF model and will provide us with a better understanding of the communication that occurs between the host and its bacterial residents, as well as how this communication works to improve overall health.
Statement of Interest
None.
Acknowledgments
The authors are funded by Science Foundation Ireland, through the Irish Government’s National Development Plan in the form of a centre grant (APC Microbiome Institute Grant Number SFI/12/RC/2273), by the Health Research Board through Health Research Awards (grant numbers HRA_POR/2012/32, J.F.C. and T.G.D.; and HRA_POR/2014/647, G.C. and T.G.D.), and through EU GRANT 613979 (MYNEWGUT FP7-KBBE-2013-7, J.F.C. and T.G.D.). The Centre has conducted studies in collaboration with several companies including GSK, Pfizer, Wyeth, and Mead Johnson. G.C. is supported by a NARSAD Young Investigator Grant from the Brain and Behavior Research Foundation (grant number 20771).The content of this paper was neither influenced nor constrained by the grant support received.
References
- Abbott NJ, Patabendige AAK, Dolman DEM, Yusof SR, Begley DJ. (2010) Structure and function of the blood–brain barrier. Neurobiol Dis 37:13–25. [DOI] [PubMed] [Google Scholar]
- Abrams GD, Bauer H, Sprinz H. (1962) Influence of the normal flora on mucosal morphology and cellular renewal in the ileum. A comparison of germ-free and conventional mice. DTIC Document. [PubMed] [Google Scholar]
- Akira S, Hemmi H. (2003) Recognition of pathogen-associated molecular patterns by TLR family. Immunol Lett 85:85–95. [DOI] [PubMed] [Google Scholar]
- Ananthakrishnan AN. (2015) Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol 12:205–217. [DOI] [PubMed] [Google Scholar]
- Arentsen T, Raith H, Qian Y, Forssberg H, Heijtz RD. (2015) Host microbiota modulates development of social preference in mice. Microb Ecol Health Dis 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aroniadis OC, Brandt LJ. (2013) Fecal microbiota transplantation: past, present and future. Curr Opin Gastroenterol 29:79–84. [DOI] [PubMed] [Google Scholar]
- Ascherio A. (2013) Environmental factors in multiple sclerosis. Expert Rev Neurother 13:3–9. [DOI] [PubMed] [Google Scholar]
- Autry AE, Monteggia LM. (2012) Brain-derived neurotrophic factor and neuropsychiatric disorders. Pharmacol Rev 64:238–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bäckhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, Semenkovich CF, Gordon JI. (2004) The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci U S A 101:15718–15723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bäckhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. (2005) Host-bacterial mutualism in the human intestine. Science 307:1915–1920. [DOI] [PubMed] [Google Scholar]
- Bäckhed F, Manchester JK, Semenkovich CF, Gordon JI. (2007) Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc Natl Acad Sci 104:979–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballabh P, Braun A, Nedergaard M. (2004) The blood–brain barrier: an overview: structure, regulation, and clinical implications. Neurobiol Dis 16:1–13. [DOI] [PubMed] [Google Scholar]
- Barnes RD, Tuffrey M, Cook R. (1968) A “germfree” human isolator. Lancet 291:622–623. [DOI] [PubMed] [Google Scholar]
- Barnes RD, Bentovim A, Hensman S, Piesowicz AT. (1969. a) Care and observation of a germ-free neonate. Arch Dis Child 44:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes RD, Fairweather DVI, Holliday J, Keane C, Piesowicz A, Soothill JF, Tuffrey M. (1969. b) A germfree infant. Lancet 293:168–171. [DOI] [PubMed] [Google Scholar]
- Becker KG, Simon RM, Bailey-Wilson JE, Freidlin B, Biddison WE, McFarland HF, Trent JM. (1998) Clustering of non-major histocompatibility complex susceptibility candidate loci in human autoimmune diseases. Proc Natl Acad Sci 95:9979–9984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belzung C, Griebel G. (2001) Measuring normal and pathological anxiety-like behavior in mice: a review. Behav Brain Res 125:141–149. [DOI] [PubMed] [Google Scholar]
- Bengmark S. (2013) Gut microbiota, immune development and function. Pharmacol Res 69:87–113. [DOI] [PubMed] [Google Scholar]
- Bercik P. (2011) The microbiota–gut–brain axis: learning from intestinal bacteria? Gut 60:288–289. [DOI] [PubMed] [Google Scholar]
- Bercik P, Collins SM. (2014) The effects of inflammation, infection and antibiotics on the microbiota-gut-brain axis. in: microbial endocrinology: the microbiota-gut-brain axis in health and disease, pp 279–289. Springer. [DOI] [PubMed] [Google Scholar]
- Bercik P, Denou E, Collins J, Jackson W, Lu J, Jury J, Deng Y, Blennerhassett P, Macri J, McCoy KD, Verdu EF, Collins SM. (2011. a) The intestinal microbiota affect central levels of brain-derived neurotropic factor and behavior in mice. Gastroenterology 141:599–609.e3. [DOI] [PubMed] [Google Scholar]
- Bercik P, Park AJ, Sinclair D, Khoshdel A, Lu J, Huang X, Deng Y, Blennerhassett PA, Fahnestock M, Moine D, Berger B, Huizinga JD, Kunze W, McLean PG, Bergonzelli GE, Collins SM, Verdu EF. (2011. b) The anxiolytic effect of Bifidobacterium longum NCC3001 involves vagal pathways for gut–brain communication. Neurogastroenterol Motil 23:1132–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bercik P, Verdu EF, Foster JA, Macri J, Potter M, Huang X, Malinowski P, Jackson W, Blennerhassett P, Neufeld KA. (2010) Chronic gastrointestinal inflammation induces anxiety-like behavior and alters central nervous system biochemistry in mice. Gastroenterology 139:2102–2112. [DOI] [PubMed] [Google Scholar]
- Berer K, Mues M, Koutrolos M, Al Rasbi Z, Boziki M, Johner C, Wekerle H, Krishnamoorthy G. (2011) Commensal microbiota and myelin autoantigen cooperate to trigger autoimmune demyelination. Nature 479:538–541. [DOI] [PubMed] [Google Scholar]
- Berger M, Gray JA, Roth BL. (2009) The expanded biology of serotonin. Annu Rev Med 60:355–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betts AO, Trexler PC. (1969) Development and possible uses for gnotobiotic farm animals. Vet Rec 84:630–632. [DOI] [PubMed] [Google Scholar]
- Bibiloni R. (2012) Rodent models to study the relationships between mammals and their bacterial inhabitants. Gut Microbes 3:536–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackshaw LA, Brookes SJH, Grundy D, Schemann M. (2007) Sensory transmission in the gastrointestinal tract. Neurogastroenterol Motil 19:1–19. [DOI] [PubMed] [Google Scholar]
- Borody TJ, Khoruts A. (2012) Fecal microbiota transplantation and emerging applications. Nat Rev Gastroenterol Hepatol 9:88–96. [DOI] [PubMed] [Google Scholar]
- Borre YE, O’Keeffe GW, Clarke G, Stanton C, Dinan TG, Cryan JF. (2014) Microbiota and neurodevelopmental windows: implications for brain disorders. Trends Mol Med 20:509–518. [DOI] [PubMed] [Google Scholar]
- Braniste V, Al-Asmakh M, Kowal C, Anuar F, Abbaspour A, Tóth M, Korecka A, Bakocevic N, Ng LG, Kundu P, Gulyás B, Halldin C, Hultenby K, Nilsson H, Hebert H, Volpe BT, Diamond B, Pettersson S. (2014) The gut microbiota influences blood-brain barrier permeability in mice. Sci Transl Med 6:263ra158–ra263ra158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo JA, Forsythe P, Chew M V, Escaravage E, Savignac HM, Dinan TG, Bienenstock J, Cryan JF. (2011) Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Natl Acad Sci 108:16050–16055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns A, Iliffe S. (2009) Alzheimer’s disease. BMJ 338. [DOI] [PubMed] [Google Scholar]
- Burokas A, Moloney RD, Dinan TG, Cryan JF. (2015) Chapter one-microbiota regulation of the mammalian gut–brain axis. Adv Appl Microbiol 91:1–62. [DOI] [PubMed] [Google Scholar]
- Clarke G, Cryan JF, Dinan TG, Quigley EM. (2012) Review article: probiotics for the treatment of irritable bowel syndrome–focus on lactic acid bacteria. Aliment Pharmacol Ther 35:403–413. [DOI] [PubMed] [Google Scholar]
- Clarke G, Grenham S, Scully P, Fitzgerald P, Moloney RD, Shanahan F, Dinan TG, Cryan JF. (2013) The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol Psychiatry 18:666–673. [DOI] [PubMed] [Google Scholar]
- Collins J, Borojevic R, Verdu EF, Huizinga JD, Ratcliffe EM. (2014) Intestinal microbiota influence the early postnatal development of the enteric nervous system. Neurogastroenterol Motil 26:98–107. [DOI] [PubMed] [Google Scholar]
- Collins SM, Surette M, Bercik P. (2012) The interplay between the intestinal microbiota and the brain. Nat Rev Micro 10:735–742. [DOI] [PubMed] [Google Scholar]
- Costello EK, Lauber CL, Hamady M, Fierer N, Gordon JI, Knight R. (2009) Bacterial community variation in human body habitats across space and time. Science 326:1694–1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crichton M. (1993) The andromeda strain. New York: Random House. [Google Scholar]
- Crumeyrolle-Arias M, Jaglin M, Bruneau A, Vancassel S, Cardona A, Daugé V, Naudon L, Rabot S. (2014) Absence of the gut microbiota enhances anxiety-like behavior and neuroendocrine response to acute stress in rats. Psychoneuroendocrinology 42:207–217. [DOI] [PubMed] [Google Scholar]
- Cryan JF, Dinan TG. (2012) Mind-altering microorganisms: the impact of the gut microbiota on brain and behavior. Nat Rev Neurosci 13:701–712. [DOI] [PubMed] [Google Scholar]
- Cryan JF, Dinan TG. (2015) Microbiota and neuroimmune signalling: Metchnikoff to microglia. Nat Rev Gastroenterol Hepatol. In press. [DOI] [PubMed] [Google Scholar]
- Cryan JF, O’Mahony SM. (2011) The microbiome-gut-brain axis: from bowel to behavior. Neurogastroenterol Motil 23:187–192. [DOI] [PubMed] [Google Scholar]
- Curran EA, Dalman C, Kearney PM, Kenny LC, Cryan JF, Dinan TG, Khashan AS. (2015. a) Association between obstetric mode of delivery and autism spectrum disorder: a population-based sibling design study. JAMA Psychiatry 72:935–942. [DOI] [PubMed] [Google Scholar]
- Curran EA, O’Neill SM, Cryan JF, Kenny LC, Dinan TG, Khashan AS, Kearney PM. (2015. b) Research review: birth by caesarean section and development of autism spectrum disorder and attention‐deficit/hyperactivity disorder: a systematic review and meta‐analysis. J Child Psychol Psychiatry 56:500–508. [DOI] [PubMed] [Google Scholar]
- De Palma G, Blennerhassett P, Lu J, Deng Y, Park AJ, Green W, Denou E, Silva MA, Santacruz A, Sanz Y. (2015) Microbiota and host determinants of behavioral phenotype in maternally separated mice. Nat Commun 6. [DOI] [PubMed] [Google Scholar]
- De Theije CGM, Wopereis H, Ramadan M, van Eijndthoven T, Lambert J, Knol J, Garssen J, Kraneveld AD, Oozeer R. (2014) Altered gut microbiota and activity in a murine model of autism spectrum disorders. Brain Behav Immun 37:197–206. [DOI] [PubMed] [Google Scholar]
- Den Besten G, van Eunen K, Groen AK, Venema K, Reijngoud D-J, Bakker BM. (2013) The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res 54:2325–2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dendrou CA, Fugger L, Friese MA. (2015) Immunopathology of multiple sclerosis. Nat Rev Immunol 15:545–558. [DOI] [PubMed] [Google Scholar]
- Deng W, Aimone JB, Gage FH. (2010) New neurons and new memories: how does adult hippocampal neurogenesis affect learning and memory? Nat Rev Neurosci 11:339–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desbonnet L, Clarke G, Shanahan F, Dinan TG, Cryan JF. (2014) Microbiota is essential for social development in the mouse. Mol Psychiatry 19:146–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desbonnet L, Clarke G, Traplin A, O’Sullivan O, Crispie F, Moloney RD, Cotter PD, Dinan TG, Cryan JF. (2015) Gut microbiota depletion from early adolescence in mice: Implications for brain and behavior. Brain Behav Immun 48:165–173. [DOI] [PubMed] [Google Scholar]
- Dinan TG, Cryan JF. (2012) Regulation of the stress response by the gut microbiota: implications for psychoneuroendocrinology. Psychoneuroendocrinology 37:1369–1378. [DOI] [PubMed] [Google Scholar]
- Dinan TG, Stanton C, Cryan JF. (2013) Psychobiotics: a novel class of psychotropic. Biol Psychiatry 74:720–726. [DOI] [PubMed] [Google Scholar]
- Ding S, Chi MM, Scull BP, Rigby R, Schwerbrock NMJ, Magness S, Jobin C, Lund PK. (2010) High-fat diet: bacteria interactions promote intestinal inflammation which precedes and correlates with obesity and insulin resistance in mouse. PLoS One 5:e12191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Distrutti E, O’Reilly J-A, McDonald C, Cipriani S, Renga B, Lynch MA, Fiorucci S. (2014) Modulation of intestinal microbiota by the probiotic VSL# 3 resets brain gene expression and ameliorates the age-related deficit in LTP. PLoS One 9:e106503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Aidy S, Dinan TG, Cryan JF. (2015) Gut microbiota: the conductor in the orchestra of immune–neuroendocrine communication. Clin Ther 37:954–967. [DOI] [PubMed] [Google Scholar]
- El Aidy S, Kunze W, Bienenstock J, Kleerebezem M. (2012) The microbiota and the gut-brain axis: insights from the temporal and spatial mucosal alterations during colonisation of the germfree mouse intestine. Benef Microbes 3:251–259. [DOI] [PubMed] [Google Scholar]
- Ennaceur A, Delacour J. (1988) A new one-trial test for neurobiological studies of memory in rats. 1: behavioral data. Behav Brain Res 31:47–59. [DOI] [PubMed] [Google Scholar]
- Erny D, Hrabě de Angelis AL, Jaitin D, Wieghofer P, Staszewski O, David E, Keren-Shaul H, Mahlakoiv T, Jakobshagen K, Buch T, Schwierzeck V, Utermöhlen O, Chun E, Garrett WS, McCoy KD, Diefenbach A, Staeheli P, Stecher B, Amit I, Prinz M. (2015) Host microbiota constantly control maturation and function of microglia in the CNS. Nat Neurosci 18:965–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezenwa VO, Gerardo NM, Inouye DW, Medina M, Xavier JB. (2012) Animal behavior and the microbiome. Science 338:198–199. [DOI] [PubMed] [Google Scholar]
- Faith JJ, Rey FE, O’Donnell D, Karlsson M, McNulty NP, Kallstrom G, Goodman AL, Gordon JI. (2010) Creating and characterizing communities of human gut microbes in gnotobiotic mice. ISME J 4:1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fakhoury M. (2015) Autistic spectrum disorders: a review of clinical features, theories and diagnosis. Int J Dev Neurosci 43:70–77. [DOI] [PubMed] [Google Scholar]
- Fleissner CK, Huebel N, El-Bary MMA, Loh G, Klaus S, Blaut M. (2010) Absence of intestinal microbiota does not protect mice from diet-induced obesity. Br J Nutr 104:919–929. [DOI] [PubMed] [Google Scholar]
- Fond G, Loundou A, Hamdani N, Boukouaci W, Dargel A, Oliveira J, Roger M, Tamouza R, Leboyer M, Boyer L. (2014) Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci 264:651–660. [DOI] [PubMed] [Google Scholar]
- Forsythe P, Kunze WA. (2013) Voices from within: gut microbes and the CNS. Cell Mol life Sci 70:55–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster JA, Lyte M, Meyer E, Cryan JF. (2015) Gut microbiota and brain function: an evolving field in neuroscience. Int J Neuropsychopharmacol doi: 10.1093/ijnp/pyv114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster JA, McVey Neufeld KA. (2013) Gut–brain axis: how the microbiome influences anxiety and depression. Trends Neurosci 36:305–312. [DOI] [PubMed] [Google Scholar]
- Frank DN, Pace NR. (2008) Gastrointestinal microbiology enters the metagenomics era. Curr Opin Gastroenterol 24:4–10. [DOI] [PubMed] [Google Scholar]
- Funkhouser LJ, Bordenstein SR. (2013) Mom knows best: the universality of maternal microbial transmission. PLoS Biol 11:e1001631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furness JB. (2006) The organisation of the autonomic nervous system: peripheral connections. Auton Neurosci 130:1–5. [DOI] [PubMed] [Google Scholar]
- Gareau MG, Wine E, Rodrigues DM, Cho JH, Whary MT, Philpott DJ, MacQueen G, Sherman PM. (2011) Bacterial infection causes stress-induced memory dysfunction in mice. Gut 60:307–317. [DOI] [PubMed] [Google Scholar]
- Gilbert JA, Krajmalnik-Brown R, Porazinska DL, Weiss SJ, Knight R. (2013) Toward effective probiotics for autism and other neurodevelopmental disorders. Cell 155:1446–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goehler LE, Park SM, Opitz N, Lyte M, Gaykema RPA. (2008) Campylobacter jejuni infection increases anxiety-like behavior in the holeboard: possible anatomical substrates for viscerosensory modulation of exploratory behavior. Brain Behav Immun 22:354–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golubeva A V, Crampton S, Desbonnet L, Edge D, O’Sullivan O, Lomasney KW, Zhdanov A V, Crispie F, Moloney RD, Borre YE. (2015) Prenatal stress-induced alterations in major physiological systems correlate with gut microbiota composition in adulthood. Psychoneuroendocrinology 60:58–74. [DOI] [PubMed] [Google Scholar]
- Gordon HA, Bruckner-Kardoss E. (1961) Effect of normal microbial flora on intestinal surface area. Am J Physiol Content 201:175–178. [Google Scholar]
- Gordon HA, Bruckner-kardoss E, Wostmann BS. (1966) Aging in germ-free mice: life tables and lesions observed at natural death. J Gerontol 21:380–387. [DOI] [PubMed] [Google Scholar]
- Gordon HA, Pesti L. (1971) The gnotobiotic animal as a tool in the study of host microbial relationships. Bact Rev 35:390–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon HA, Wostmann BS. (1960) Morphological studies on the germfreealbino rat. Anat Rec 137:65–70. [DOI] [PubMed] [Google Scholar]
- Goverman J. (2009) Autoimmune T cell responses in the central nervous system. Nat Rev Immunol 9:393–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grenham S, Clarke G, Cryan J, Dinan T. (2011) Brain–gut–microbe communication in health and disease. Front Physiol 2:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustaffson B, Kahlson G, Rosengren E. (1957) Biogenesis of histamine studied by its distribution and urinary excretion in germ free reared and not germ free rats fed a histamine free diet. Acta Physiol Scand 41:217–228. [DOI] [PubMed] [Google Scholar]
- Gustafsson BE. (1959. a) Lightweight stainless steel systems for rearing germfree animals. Ann N Y Acad Sci 78:17–28. [DOI] [PubMed] [Google Scholar]
- Gustafsson BE. (1959. b) Vitamin K deficiency in germfree rats. Ann N Y Acad Sci 78:166–174. [DOI] [PubMed] [Google Scholar]
- Hamilton W. (1964) The genetical evolution of social behavior. J Theortical Biol 7:1–52. [DOI] [PubMed] [Google Scholar]
- Hansen T, Gobel R, Hansen T, Pedersen O. (2015) The gut microbiome in cardio-metabolic health. Genome Med 7:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harach T, Marungruang N, Dutilleul N, Cheatham V, Mc Coy KD, Neher JJ, Jucker M, Fåk F, Bolmont T. (2015) Reduction of Alzheimer’s disease beta-amyloid pathology in the absence of gut microbiota. arXiv Prepr arXiv 150902273. [Google Scholar]
- Hardy JA, Higgins GA. (1992) Alzheimer’s disease: the amyloid cascade hypothesis. Science 256:184. [DOI] [PubMed] [Google Scholar]
- Heijtz RD, Wang S, Anuar F, Qian Y, Björkholm B, Samuelsson A, Hibberd ML, Forssberg H, Pettersson S. (2011) Normal gut microbiota modulates brain development and behavior. Proc Natl Acad Sci 108:3047–3052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hintze KJ, Cox JE, Rompato G, Benninghoff AD, Ward RE, Broadbent J, Lefevre M. (2014) Broad scope method for creating humanized animal models for animal health and disease research through antibiotic treatment and human fecal transfer. Gut Microbes 5:183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper L V, Gordon JI. (2001) Commensal host-bacterial relationships in the gut. Science 292:1115–1118. [DOI] [PubMed] [Google Scholar]
- Hooper L V, Macpherson AJ. (2010) Immune adaptations that maintain homeostasis with the intestinal microbiota. Nat Rev Immunol 10:159–169. [DOI] [PubMed] [Google Scholar]
- Hosoi T, Okuma Y, Nomura Y. (2000) Electrical stimulation of afferent vagus nerve induces IL-1β expression in the brain and activates HPA axis. Am J Physiol Integr Comp Physiol 279:R141–R147. [DOI] [PubMed] [Google Scholar]
- Høverstad T, Midtvedt T. (1986) Short-chain fatty acids in germfree mice and rats. J Nutr 116:1772–1776. [DOI] [PubMed] [Google Scholar]
- Howard MA, Cowell PE, Boucher J, Broks P, Mayes A, Farrant A, Roberts N. (2000) Convergent neuroanatomical and behavioral evidence of an amygdala hypothesis of autism. Neuroreport 11:2931–2935. [DOI] [PubMed] [Google Scholar]
- Howitt MR, Garrett WS. (2012) A complex microworld in the gut: gut microbiota and cardiovascular disease connectivity. Nat Med 18:1188–1189. [DOI] [PubMed] [Google Scholar]
- Hsiao EY, McBride SW, Hsien S, Sharon G, Hyde ER, McCue T, Codelli JA, Chow J, Reisman SE, Petrosino JF, Patterson PH, Mazmanian SK. (2013) Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell 155:1451–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husebye E, Hellström PM, Midtvedt T. (1994) Intestinal microflora stimulates myoelectric activity of rat small intestine by promoting cyclic initiation and aboral propagation of migrating myoelectric complex. Dig Dis Sci 39:946–956. [DOI] [PubMed] [Google Scholar]
- Husebye E, Hellström PM, Sundler F, Chen J, Midtvedt T. (2001) Influence of microbial species on small intestinal myoelectric activity and transit in germ-free rats. Am J Physiol Liver Physiol 280:G368–G380. [DOI] [PubMed] [Google Scholar]
- Ittner LM, Götz J. (2011) Amyloid-β and tau—a toxic pas de deux in Alzheimer’s disease. Nat Rev Neurosci 12:67–72. [DOI] [PubMed] [Google Scholar]
- Janssen AWF, Kersten S. (2015) The role of the gut microbiota in metabolic health. FASEB J 29:3111–3123. [DOI] [PubMed] [Google Scholar]
- Jeffery IB, O’Toole PW, Ohman L, Claesson MJ, Deane J, Quigley EMM, Simren M. (2012) An irritable bowel syndrome subtype defined by species-specific alterations in faecal microbiota. Gut 61:997–1006. [DOI] [PubMed] [Google Scholar]
- Kang D-W, Park JG, Ilhan ZE, Wallstrom G, LaBaer J, Adams JB, Krajmalnik-Brown R. (2013) Reduced incidence of Prevotella and other fermenters in intestinal microflora of autistic children. PLoS One 8:e68322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson FH, Fåk F, Nookaew I, Tremaroli V, Fagerberg B, Petranovic D, Bäckhed F, Nielsen J. (2012) Symptomatic atherosclerosis is associated with an altered gut metagenome. Nat Commun 3:1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson FH, Tremaroli V, Nookaew I, Bergström G, Behre CJ, Fagerberg B, Nielsen J, Bäckhed F. (2013) Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature 498:99–103. [DOI] [PubMed] [Google Scholar]
- Kelly JR, Kennedy PJ, Cryan JF, Dinan TG, Clarke G, Hyland NP. (2015) Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci 9:392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy PJ, Clarke G, O’Neill A, Groeger JA, Quigley EMM, Shanahan F, Cryan JF, Dinan TG. (2014. a) Cognitive performance in irritable bowel syndrome: evidence of a stress-related impairment in visuospatial memory. Psychol Med 44:1553–1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy PJ, Cryan JF, Dinan TG, Clarke G. (2014. b) Irritable bowel syndrome: a microbiome-gut-brain axis disorder? World J Gastroenterol WJG 20:14105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy PJ, Cryan JF, Quigley EMM, Dinan TG, Clarke G. (2014. c) A sustained hypothalamic–pituitary–adrenal axis response to acute psychosocial stress in irritable bowel syndrome. Psychol Med 44:3123–3134. [DOI] [PubMed] [Google Scholar]
- Kettenmann H, Hanisch U-K, Noda M, Verkhratsky A. (2011) Physiology of microglia. Physiol Rev 91:461–553. [DOI] [PubMed] [Google Scholar]
- Kirk RGW. (2012) “Life in a germ-free world”: isolating life from the laboratory animal to the bubble boy. Bull Hist Med 86:237–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen E. (2004) Sensitive periods in the development of the brain and behavior. Cogn Neurosci J 16:1412–1425. [DOI] [PubMed] [Google Scholar]
- Kohane IS, McMurry A, Weber G, MacFadden D, Rappaport L, Kunkel L, Bickel J, Wattanasin N, Spence S, Murphy S. (2012) The co-morbidity burden of children and young adults with autism spectrum disorders. PLoS One 7:e33224–e33224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koren O, Spor A, Felin J, Fåk F, Stombaugh J, Tremaroli V, Behre CJ, Knight R, Fagerberg B, Ley RE, Bäckhed F. (2011) Human oral, gut, and plaque microbiota in patients with atherosclerosis. Proc Natl Acad Sci 108:4592–4598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunze WA, Mao Y, Wang B, Huizinga JD, Ma X, Forsythe P, Bienenstock J. (2009) Lactobacillus reuteri enhances excitability of colonic AH neurons by inhibiting calcium-dependent potassium channel opening. J Cell Mol Med 13:2261–2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence RJ. (1985) David the “Bubble Boy” and the boundaries of the human. JAMA 253:74–76. [PubMed] [Google Scholar]
- Lee YK, Menezes JS, Umesaki Y, Mazmanian SK. (2011) Proinflammatory T-cell responses to gut microbiota promote experimental autoimmune encephalomyelitis. Proc Natl Acad Sci 108:4615–4622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leone V, Gibbons SM, Martinez K, Hutchison AL, Huang EY, Cham CM, Pierre JF, Heneghan AF, Nadimpalli A, Hubert N, Zale E, Wang Y, Huang Y, Theriault B, Dinner AR, Musch MW, Kudsk KA, Prendergast BJ, Gilbert JA, Chang EB. (2015) Effects of diurnal variation of gut microbes and high-fat feeding on host circadian clock function and metabolism. Cell Host Microbe 17:681–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ley RE, Turnbaugh PJ, Klein S, Gordon JI. (2006) Microbial ecology: human gut microbes associated with obesity. Nature 444:1022–1023. [DOI] [PubMed] [Google Scholar]
- Lombardo MP. (2008) Access to mutualistic endosymbiotic microbes: an underappreciated benefit of group living. Behav Ecol Sociobiol 62:479–497. [Google Scholar]
- Luckey T. (2012) Germfree life and gnotobiology. Elsevier. [Google Scholar]
- Lyte M. (2013) Microbial endocrinology in the microbiome-gut-brain axis: how bacterial production and utilization of neurochemicals influence behavior. [DOI] [PMC free article] [PubMed]
- Lyte M, Li W, Opitz N, Gaykema RPA, Goehler LE. (2006) Induction of anxiety-like behavior in mice during the initial stages of infection with the agent of murine colonic hyperplasia Citrobacter rodentium. Physiol Behav 89:350–357. [DOI] [PubMed] [Google Scholar]
- Lyte M, Varcoe JJ, Bailey MT. (1998) Anxiogenic effect of subclinical bacterial infection in mice in the absence of overt immune activation. Physiol Behav 65:63–68. [DOI] [PubMed] [Google Scholar]
- Macpherson AJ, Harris NL. (2004) Interactions between commensal intestinal bacteria and the immune system. Nat Rev Immunol 4:478–485. [DOI] [PubMed] [Google Scholar]
- Marchesi JR, Adams DH, Fava F, Hermes GDA, Hirschfield GM, Hold G, Quraishi MN, Kinross J, Smidt H, Tuohy KM, Thomas LV, Zoetendal EG, Hart A. (2015) The gut microbiota and host health: a new clinical frontier. Gut 65:330–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marín-Burgin A, Schinder AF. (2012) Requirement of adult-born neurons for hippocampus-dependent learning. Behav Brain Res 227:391–399. [DOI] [PubMed] [Google Scholar]
- Mayer EA, Padua D, Tillisch K. (2014) Altered brain-gut axis in autism: comorbidity or causative mechanisms? Bioessays 36:933–939. [DOI] [PubMed] [Google Scholar]
- Mayer EA, Tillisch K, Gupta A. (2015) Gut/brain axis and the microbiota. J Clin Invest 125:0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcvey Neufeld KA, Mao YK, Bienenstock J, Foster JA, Kunze WA. (2013) The microbiome is essential for normal gut intrinsic primary afferent neuron excitability in the mouse. Neurogastroenterol Motil 25:183–e88. [DOI] [PubMed] [Google Scholar]
- McVey Neufeld KA, Perez-Burgos A, Mao YK, Bienenstock J, Kunze WA. (2015) The gut microbiome restores intrinsic and extrinsic nerve function in germ-free mice accompanied by changes in calbindin. Neurogastroenterol Motil 27:627–636. [DOI] [PubMed] [Google Scholar]
- Messaoudi M, Lalonde R, Violle N, Javelot H, Desor D, Nejdi A, Bisson J-F, Rougeot C, Pichelin M, Cazaubiel M. (2011) Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br J Nutr 105:755–764. [DOI] [PubMed] [Google Scholar]
- Mielcarz DW, Kasper LH. (2015) The gut microbiome in multiple sclerosis. Curr Treat Options Neurol 17:1–10. [DOI] [PubMed] [Google Scholar]
- Miller BR, Hen R. (2015) The current state of the neurogenic theory of depression and anxiety. Curr Opin Neurobiol 30:51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyakawa M. (1959) The Miyakawa remote-control germfree rearing unit. Ann N Y Acad Sci 78:37–46. [DOI] [PubMed] [Google Scholar]
- Montiel-Castro AJ, González-Cervantes RM, Bravo-Ruiseco G, Pacheco-López G. (2013) The microbiota-gut-brain axis: neurobehavioral correlates, health and sociality. Front Integr Neurosci 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser M-B, Moser EI, Forrest E, Andersen P, Morris RG. (1995) Spatial learning with a minislab in the dorsal hippocampus. Proc Natl Acad Sci 92:9697–9701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulle JG, Sharp WG, Cubells JF. (2013) The gut microbiome: a new frontier in autism research. Curr Psychiatry Rep 15:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musiek ES, Holtzman DM. (2015) Three dimensions of the amyloid hypothesis: time, space and’wingmen’. Nat Neurosci:800–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myint A-M, Kim YK, Verkerk R, Scharpé S, Steinbusch H, Leonard B. (2007) Kynurenine pathway in major depression: evidence of impaired neuroprotection. J Affect Disord 98:143–151. [DOI] [PubMed] [Google Scholar]
- Neufeld KM, Kang N, Bienenstock J, Foster JA. (2011) Reduced anxiety-like behavior and central neurochemical change in germ-free mice. Neurogastroenterol Motil 23:255–265. [DOI] [PubMed] [Google Scholar]
- Nicholson J, Holmes E, Kinross J, Burcelin R, Gibson G, Jia W, Petttersen S. (2012) Host-gut microbiota metabolic interactions. Science 336:1262–1267. [DOI] [PubMed] [Google Scholar]
- Nuttall GHF, Thierfelder H. (1897) Thierisches Leben ohne Bakterien im Verdauungskanal.(II. Mittheilung). Hoppe Seylers Z Physiol Chem 22:62–73. [Google Scholar]
- O’Leary OF, Cryan JF. (2014) A ventral view on antidepressant action: roles for adult hippocampal neurogenesis along the dorsoventral axis. Trends Pharmacol Sci 35:675–687. [DOI] [PubMed] [Google Scholar]
- O’Mahony CM, Sweeney FF, Daly E, Dinan TG, Cryan JF. (2010) Restraint stress-induced brain activation patterns in two strains of mice differing in their anxiety behavior. Behav Brain Res 213:148–154. [DOI] [PubMed] [Google Scholar]
- O’Mahony SM, Marchesi JR, Scully P, Codling C, Ceolho A-M, Quigley EMM, Cryan JF, Dinan TG. (2009) Early life stress alters behavior, immunity, and microbiota in rats: implications for irritable bowel syndrome and psychiatric illnesses. Biol Psychiatry 65:263–267. [DOI] [PubMed] [Google Scholar]
- O’Mahony SM, Clarke G, Borre YE, Dinan TG, Cryan JF. (2015) Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behav Brain Res 277:32–48. [DOI] [PubMed] [Google Scholar]
- O’Toole PW, Claesson MJ. (2010) Gut microbiota: changes throughout the lifespan from infancy to elderly. Int Dairy J 20:281–291. [Google Scholar]
- Ogbonnaya ES, Clarke G, Shanahan F, Dinan TG, Cryan JF, O’Leary OF. (2015) Adult hippocampal neurogenesis is regulated by the microbiome. Biol Psychiatry 78:e7–9. [DOI] [PubMed] [Google Scholar]
- Park H, Poo M. (2013) Neurotrophin regulation of neural circuit development and function. Nat Rev Neurosci 14:7–23. [DOI] [PubMed] [Google Scholar]
- Pasteur L. (1885) Observations relatives à la note précédente de M. Duclaux. CR Acad Sci 100:68. [Google Scholar]
- Perez-Burgos A, Mao Y-K, Bienenstock J, Kunze WA. (2014) The gut-brain axis rewired: adding a functional vagal nicotinic “sensory synapse.” FASEB J 28:3064–3074. [DOI] [PubMed] [Google Scholar]
- Powley TL, Wang XY, Fox EA, Phillips RJ, Liu LWC, Huizinga JD. (2008) Ultrastructural evidence for communication between intramuscular vagal mechanoreceptors and interstitial cells of Cajal in the rat fundus. Neurogastroenterol Motil 20:69–79. [DOI] [PubMed] [Google Scholar]
- Prinz M, Priller J. (2014) Microglia and brain macrophages in the molecular age: from origin to neuropsychiatric disease. Nat Rev Neurosci 15:300–312. [DOI] [PubMed] [Google Scholar]
- Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, Liang S, Zhang W, Guan Y, Shen D. (2012) A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490:55–60. [DOI] [PubMed] [Google Scholar]
- Rabot S, Membrez M, Bruneau A, Gérard P, Harach T, Moser M, Raymond F, Mansourian R, Chou CJ. (2010) Germ-free C57BL/6J mice are resistant to high-fat-diet-induced insulin resistance and have altered cholesterol metabolism. FASEB J 24:4948–4959. [DOI] [PubMed] [Google Scholar]
- Radde R, Bolmont T, Kaeser SA, Coomaraswamy J, Lindau D, Stoltze L, Calhoun ME, Jäggi F, Wolburg H, Gengler S. (2006) Aβ42-driven cerebral amyloidosis in transgenic mice reveals early and robust pathology. EMBO Rep 7:940–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R. (2004) Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell 118:229–241. [DOI] [PubMed] [Google Scholar]
- Ransohoff RM, Perry VH. (2009) Microglial physiology: unique stimuli, specialized responses. Annu Rev Immunol 27:119–145. [DOI] [PubMed] [Google Scholar]
- Reigstad CS, Salmonson CE, Rainey JF, Szurszewski JH, Linden DR, Sonnenburg JL, Farrugia G, Kashyap PC. (2015) Gut microbes promote colonic serotonin production through an effect of short-chain fatty acids on enterochromaffin cells. FASEB J 29:1395–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyniers JA. (1942) Design characteristics of double cubicle system for protecting babies in nurseries. Am J Dis Child 63:934–944. [Google Scholar]
- Reyniers JA. (1943) The control of cross infection among limited populations. The use of mechanical barriers in preventing cross infection among hospitalized infant populations. Micrurgical Germ-Free Tech Their Appl to Exp Biol Med Balt MD Charles C Thomas Publ:205–232. [Google Scholar]
- Reyniers JA. (1959) The pure culture concept and gnotobiotics. Ann N Y Acad Sci 78:3–16. [Google Scholar]
- Reyniers JA, Sacksteder MR. (1958) Observations on the survival of germfree C3H mice and their resistance to a contaminated environment. In: Proc Anim Care Panel, pp 41–53. [Google Scholar]
- Reyniers JA, Trexler PC, Ervin RF. (1946) Rearing germ-free albino rats. Lobund Rep 1. [PubMed] [Google Scholar]
- Rhee SH, Pothoulakis C, Mayer EA. (2009) Principles and clinical implications of the brain-gut-enteric microbiota axis. Nat Rev Gastroenterol Hepatol 6:306–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridaura V, Belkaid Y. (2015) Gut microbiota: the link to your second brain. Cell 161:193–194. [DOI] [PubMed] [Google Scholar]
- Ridaura VK, Faith JJ, Rey FE, Cheng J, Duncan AE, Kau AL, Griffin NW, Lombard V, Henrissat B, Bain JR. (2013) Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science 341:1241214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfeld CS. (2015) Microbiome disturbances and autism spectrum disorders. Drug Metab Dispos 43:1557–1571. [DOI] [PubMed] [Google Scholar]
- Salonen A, de Vos WM, Palva A. (2010) Gastrointestinal microbiota in irritable bowel syndrome: present state and perspectives. Microbiology 156:3205–3215. [DOI] [PubMed] [Google Scholar]
- Sampson TR, Mazmanian SK. (2015) Control of brain development, function, and behavior by the microbiome. Cell Host Microbe 17:565–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savignac HM, Tramullas M, Kiely B, Dinan TG, Cryan JF. (2015) Bifidobacteria modulate cognitive processes in an anxious mouse strain. Behav Brain Res 287:59–72. [DOI] [PubMed] [Google Scholar]
- Schafer DP, Stevens B. (2013) Phagocytic glial cells: sculpting synaptic circuits in the developing nervous system. Curr Opin Neurobiol 23:1034–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekirov I, Russell SL, Antunes LCM, Finlay BB. (2010) Gut microbiota in health and disease. Physiol Rev 90:859–904. [DOI] [PubMed] [Google Scholar]
- Shanahan F. (2002) The host–microbe interface within the gut. Best Pract Res Clin Gastroenterol 16:915–931. [DOI] [PubMed] [Google Scholar]
- Sheehan D, Moran C, Shanahan F. (2015) The microbiota in inflammatory bowel disease. J Gastroenterol 50:495–507. [DOI] [PubMed] [Google Scholar]
- Shen J, Obin MS, Zhao L. (2013) The gut microbiota, obesity and insulin resistance. Mol Aspects Med 34:39–58. [DOI] [PubMed] [Google Scholar]
- Smith K, McCoy KD, Macpherson AJ. (2007) Use of axenic animals in studying the adaptation of mammals to their commensal intestinal microbiota. In: Seminars in immunology, pp 59–69. Elsevier. [DOI] [PubMed] [Google Scholar]
- Snyder JS, Soumier A, Brewer M, Pickel J, Cameron HA. (2011) Adult hippocampal neurogenesis buffers stress responses and depressive behavior. Nature 476:458–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stilling RM, Bordenstein SR, Dinan TG, Cryan JF. (2014. a) Friends with social benefits: host-microbe interactions as a driver of brain evolution and development? Front Cell Infect Microbiol 4:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stilling RM, Dinan TG, Cryan JF. (2014. b) Microbial genes, brain and behavior–epigenetic regulation of the gut–brain axis. Genes, Brain Behav 13:69–86. [DOI] [PubMed] [Google Scholar]
- Stilling RM, Ryan FJ, Hoban AE, Shanahan F, Clarke G, Claesson MJ, Dinan TG, Cryan JF. (2015) Microbes and neurodevelopment - absence of microbiota during early life increases activity-related transcriptional pathways in the amygdala. Brain Behav Immun 50:209–220. [DOI] [PubMed] [Google Scholar]
- Stromnes IM, Goverman JM. (2006) Active induction of experimental allergic encephalomyelitis. Nat Protoc 1:1810–1819. [DOI] [PubMed] [Google Scholar]
- Sudo N, Chida Y, Aiba Y, Sonoda J, Oyama N, Yu X-N, Kubo C, Koga Y. (2004) Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J Physiol 558:263–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suez J, Korem T, Zeevi D, Zilberman-schapira G, Thaiss CA, Maza O, Israeli D, Zmora N, Gilad S, Weinberger A, Kuperman Y, Harmelin A, Kolodkin-gal I, Shapiro H. (2014) Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 514:181–186. [DOI] [PubMed] [Google Scholar]
- Sumi Y, Miyakawa M, Kanzaki M, Kotake Y. (1977) Vitamin B-6 deficiency in germfree rats. J Nutr 107:1707–1714. [DOI] [PubMed] [Google Scholar]
- Tana C, Umesaki Y, Imaoka A, Handa T, Kanazawa M, Fukudo S. (2010) Altered profiles of intestinal microbiota and organic acids may be the origin of symptoms in irritable bowel syndrome. Neurogastroenterol Motil 22:512–e115. [DOI] [PubMed] [Google Scholar]
- Tazume S, Umehara K, Matsuzawa H, Aikawa H, Hashimoto K, Sasaki S. (1991) Effects of germfree status and food restriction on longevity and growth of mice. Jikken Dobutsu 40:517–522. [DOI] [PubMed] [Google Scholar]
- Thaiss CA, Zeevi D, Levy M, Zilberman-Schapira G, Suez J, Tengeler AC, Abramson L, Katz MN, Korem T, Zmora N, Kuperman Y, Biton I, Gilad S, Harmelin A, Shapiro H, Halpern Z, Segal E, Elinav E. (2014) transkingdom control of microbiota diurnal oscillations promotes metabolic homeostasis. Cell 159:514–529. [DOI] [PubMed] [Google Scholar]
- Tremaroli V, Backhed F. (2012) Functional interactions between the gut microbiota and host metabolism. Nature 489:242–249. [DOI] [PubMed] [Google Scholar]
- Troyer K. (1984) Microbes, herbivory and the evolution of social behavior. J Theor Biol 106:157–169. [Google Scholar]
- Tung J, Barreiro LB, Burns MB, Grenier J-C, Lynch J, Grieneisen LE, Altmann J, Alberts SC, Blekhman R, Archie EA. (2015) Social networks predict gut microbiome composition in wild baboons. Elife 4:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuohy KM, Fava F, Viola R. (2014) “The way to a man”s heart is through his gut microbiota’ – dietary pro- and prebiotics for the management of cardiovascular risk. Proc Nutr Soc 73:172–185. [DOI] [PubMed] [Google Scholar]
- Turnbaugh PJ, Hamady M, Yatsunenko T, Cantarel BL, Duncan A, Ley RE, Sogin ML, Jones WJ, Roe BA, Affourtit JP. (2009. a) A core gut microbiome in obese and lean twins. Nature 457:480–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. (2006) An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 444:1027–1031. [DOI] [PubMed] [Google Scholar]
- Turnbaugh PJ, Ridaura VK, Faith JJ, Rey FE, Knight R, Gordon JI. (2009. b) The effect of diet on the human gut microbiome: a metagenomic analysis in humanized gnotobiotic mice. Sci Transl Med 1:6ra14–ra16ra14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umesaki Y, Okada Y, Matsumoto S, Imaoka A, Setoyama H. (1995) Segmented filamentous bacteria are indigenous intestinal bacteria that activate intraepithelial lymphocytes and induce MHC class II molecules and fucosyl asialo GM1 glycolipids on the small intestinal epithelial cells in the ex-germ-free mouse. Microbiol Immunol 39:555–562. [DOI] [PubMed] [Google Scholar]
- Vaishnava S, Behrendt CL, Ismail AS, Eckmann L, Hooper L V. (2008) Paneth cells directly sense gut commensals and maintain homeostasis at the intestinal host-microbial interface. Proc Natl Acad Sci 105:20858–20863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdu EF, Bercik P, Verma-Gandhu M, Huang X-X, Blennerhassett P, Jackson W, Mao Y, Wang L, Rochat F, Collins SM. (2006) Specific probiotic therapy attenuates antibiotic induced visceral hypersensitivity in mice. Gut 55:182–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrieze A, Van Nood E, Holleman F, Salojärvi J, Kootte RS, Bartelsman JF, Dallinga-Thie GM, Ackermans MT, Serlie MJ, Oozeer R, Derrien M, Druesne A, Van Hylckama Vlieg JE, Bloks VW, Groen AK, Heilig HG, Zoetendal EG, Stroes ES, de Vos WM, Hoekstra JB, Nieuwdorp M. (2012) Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology 143:913–916.e7. [DOI] [PubMed] [Google Scholar]
- Wang M, Donovan SM. (2015) Human microbiota-associated swine: current progress and future opportunities. ILAR J 56:63–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willer CJ, Dyment DA, Risch NJ, Sadovnick AD, Ebers GC, Group CCS. (2003) Twin concordance and sibling recurrence rates in multiple sclerosis. Proc Natl Acad Sci 100:12877–12882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams SCP. (2014) Gnotobiotics. Proc Natl Acad Sci 111:1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe AJ. (2002) Germs in space. Isis 93:183–205. [DOI] [PubMed] [Google Scholar]
- Wostmann B, Bruckner-Kardoss E. (1959) Development of cecal distention in germ-free baby rats. Am J Physiol Content 197:1345–1346. [DOI] [PubMed] [Google Scholar]
- Wostmann BS, Knight PL, Keeley LL, Kan DF. (1962) Metabolism and function of thiamine and naphthoquinones in germfree and conventional rats. In: Federation proceedings, pp 120–124. [PubMed] [Google Scholar]
- Wostmann BS, Larkin C, Moriarty A, Bruckner-Kardoss E. (1983) Dietary intake, energy metabolism, and excretory losses of adult male germfree Wistar rats. Lab Anim Sci 33:46–50. [PubMed] [Google Scholar]
- Wostmann BS, Pleasants JR, Bealmear P, Kincade PW. (1970) Serum proteins and lymphoid tissues in germ-free mice fed a chemically defined, water soluble, low molecular weight diet. Immunology 19:443. [PMC free article] [PubMed] [Google Scholar]
- Wrase J, Reimold M, Puls I, Kienast T, Heinz A. (2006) Serotonergic dysfunction: brain imaging and behavioral correlates. Cogn Affect Behav Neurosci 6:53–61. [DOI] [PubMed] [Google Scholar]
- Wu JCY. (2012) Psychological co-morbidity in functional gastrointestinal disorders: epidemiology, mechanisms and management. J Neurogastroenterol Motil 18:13–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yano JM, Yu K, Donaldson GP, Shastri GG, Ann P, Ma L, Nagler CR, Ismagilov RF, Mazmanian SK, Hsiao EY. (2015) Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell 161:264–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimomra ZR, Porterfield VM, Camp RM, Johnson JD. (2011) Time-dependent mediators of HPA axis activation following live Escherichia coli. Am J Physiol Integr Comp Physiol 301:R1648–R1657. [DOI] [PMC free article] [PubMed] [Google Scholar]