Abstract
A 2011 randomized controlled trial compared the effectiveness of two brief motivation-enhancing therapy (MET) models among alcohol-positive adolescents in an urban emergency department: adolescent MET-only versus MET + Family Check-Up (FCU), a parent MET model. Results indicated that among the 97 adolescents completing the 3-month assessment, both conditions were associated with reduced drinking and MET+FCU was associated with lower rates of high volume drinking than adolescent MET-only. The goal of this study was to identify predictors and moderators of high volume drinking in the original trial. Seven candidate variables were evaluated as moderators across three domains: demographic characteristics, psychological factors, and socio-contextual factors. Analyses of covariance models identified one significant predictor and one significant moderator of outcome. Older adolescents had significantly worse drinking outcomes than younger adolescents regardless of MET condition. Adolescents whose parents screened positive for problematic alcohol use at baseline had significantly worse drinking outcomes in the MET+FCU condition than the MET-only condition. Results indicate that alcohol-positive adolescents presenting to the emergency department may respond better to MET models if they are under the age of 16. Involving parents who have problematic alcohol use in a parent-focused MET may have negative effects on adolescent high volume drinking.
Keywords: adolescent, motivation-enhancement therapy, moderator, emergency department
1. Introduction
Integrating alcohol and other drug use interventions for adolescents into traditional medical settings has been recognized as an area of public health importance (Addiction Technology Transfer Center Workgroup, 2015). The emergency department (ED) visit offers a unique opportunity to screen adolescents for alcohol problems and offer brief intervention, due to extremely high rates of alcohol-related problems in this setting (D’Onofrio et al., 2012; McDonald, Wang & Camargo, 2004).
Two recent systematic reviews by Tanner-Smith and Lipsey (2015) and Mitchell and colleagues (2013) identified a total of seven randomized controlled trials that have evaluated brief interventions incorporating motivational enhancement therapy (MET) principles among adolescents under the age of 18 in the ED (Bernstein et al., 2009; Bernstein et al., 2010; Cunningham et al., 2012; Johnston et al., 2002; Spirito et al., 2004; Spirito et al., 2011; Walton et al., 2010). Since these reviews were published, another randomized controlled trial by Cunningham and colleagues (2015) tested three conditions among adolescents age 14 to 20 presenting to the ED: MET delivered by a therapist, MET delivered by computer, and brief assessment.
Of the eight randomized clinical trials that included participants under the age of 18, seven focused specifically on alcohol use outcomes, five compared MET to brief assessment, and three compared MET to active comparison conditions. The pattern of results across these studies generally indicated that all of the conditions – MET, brief assessment, and active control - were associated with significant reductions in drinking frequency and drinking-related consequences. Only one of the five studies comparing MET and brief assessment (Spirito et al., 2004) found any evidence indicating that the MET condition was associated with superior drinking outcomes; over the 12 month follow-up period, MET was associated with lower rates of overall drinking days and high volume drinking days (i.e., days of 4 drinks for females and 5 drinks for males) than brief assessment, but only among the subgroup of adolescents who screened positive for problematic alcohol use at baseline.
In an attempt to enhance the performance of MET in the ED setting, Spirito and colleagues conducted a subsequent 2011 trial examining whether MET delivery could be improved by the addition of the Family Check-Up (FCU; Dishion & Kavanagh, 2003). The FCU is an assessment and feedback intervention, consistent with an MET approach, designed to enhance parental recognition of youth risk behaviors and increase parental motivation to reduce these behaviors and associated risk factors (Dishion et al., 2002). It consists of a family assessment task followed by a feedback session with the parent. The FCU was developed to target specific parent risk and protective factors linked to adolescent alcohol and drug use such as parental substance use, parental monitoring of peer substance involvement, and the nature of the parent-teen relationship (Dishion et al., 2002; Dishion, Nelson, & Kavanagh, 2003).
Using a two-group design with three follow-up points (3-, 6-, and 12-months), the Spirito et al. (2011) trial randomly assigned 125 adolescents aged 13 to 17 who presented to the ED for an alcohol-related event to either adolescent MET only or MET+FCU. Consistent with other trials testing two active conditions, results indicated that both conditions were associated with reductions in drinking across all three follow up points, with the strongest effects at the 3-month follow-up. At 3 months, there was a main effect favoring MET+FCU in the proportion of adolescents reporting any high-volume drinking days over the past 90 days, with rates of 14.6% in MET+FCU versus 32.1% in MET only (p < .05). At both 6 and 12 months, rates of adolescents reporting high volume drinking over the past 90 days were significantly lower than at baseline but there was no significant difference between the two conditions (6 months: 27.0% MET+FCU vs. 43.6% MET; 12-months: 48.6% MET+FCU vs. 58% MET). These findings provided preliminary indication of the acute benefits of adding a parent FCU to adolescent MET.
Detecting treatment differences at the group level represents only the first step in understanding the effects of the two MET models among adolescents presenting to the ED. A critically important remaining question is which treatment approach (adolescent MET only or MET+FCU) is optimal for which adolescent presenting to the ED. Addressing this question requires the identification of moderator variables, defined as variables that are present before treatment, are independent of treatment assignment, and have an interactive effect with treatment condition (see Kraemer et al, 2002; Wallace, Frank, & Kraemer, 2013). In contrast to predictor variables, which indicate which teens are most likely to respond to any treatment, moderator variables indicate which adolescents are most likely to benefit from a specific treatment approach and have prescriptive value (see Baron & Kenny, 1986). Identifying which ED patients are most likely to benefit from a specific intervention can support empirically informed triaging decisions, which in turn promotes more judicious allocation of services in this resource constrained environment.
1.1. Selection of Candidate Variables
The purpose of this article was to conduct analyses of predictors and moderators of 3-month treatment outcome among the 97 alcohol-abusing adolescents in the Spirito et al. (2011) study who received one of the two MET models and were included in the acute outcome analysis. We focus on predictors and moderators of outcome at the 3-month assessment because: a) both MET conditions had their maximum effects at 3-months; b) the 3-month outcome was the only timepoint at which treatment differences were found; and c) other randomized clinical trials in the ED have similarly found that brief MET interventions have their maximum effects at 3-months.
Identifying moderators of treatment outcome requires at least two treatment conditions and larger sample sizes than are often recruited for efficacy studies (see Kraemer et al., 2002). Consequently, prior research on moderators of adolescent substance use treatment outcome is relatively scant (see Strada, Donohue, Lefforge, 2006). A 2011 review by Becker, Curry, and Yang identified 14 variables that had been shown to significantly predict or moderate adolescent substance use post-treatment. These variables were organized into four broad categories: adolescent biological / demographic status, adolescent psychological factors, family factors, and social network factors. A more recent review by Hernandez and colleagues (2015) grouped potential moderators into three domains based on developmental theory: biological / demographic factors, psychological factors, and socio-contextual factors. The biological / demographic and psychological domains were identical to those discussed by Becker and colleagues (2011), whereas the socio-contextual domain encompassed both family and social network factors. We used the three domains identified in the more recent integrative review by Hernandez et al. (2015) to guide the current analysis of predictors and moderators.
To avoid spurious results that capitalize on chance, we limited our testing to one candidate variable per 10–15 subjects for a total of seven putative moderators (see Curry et al., 2006). We selected at least two candidate variables from each of the three categories, based on those measures that were available in the initial dataset. For the demographic category, we selected three variables: sex, age, and Hispanic ethnicity. Sex and age were selected because they have been found to differentially influence adolescents’ response to treatment in more than one trial (e.g., Henggeler, Pickrel, & Brondino, 1999; Kaminer, Burleson, & Goldberger, 2002). Hispanic ethnicity was also included because it is a frequently examined moderator that has mixed support. For instance, Clair and colleagues (2013) found that Hispanic adolescents responded better to an MET model than relaxation therapy, while other studies and literature reviews (e.g., Becker et al., 2012; Strada et al., 2006) have failed to find evidence that race/ethnicity moderated adolescent treatment outcome. For psychological factors, we focused on severity of alcohol use and depressed mood. Baseline alcohol use severity has consistently been found to be a significant predictor of treatment outcome (Coatsworth et al., 2001; Tamm et al., 2013), and was found to moderate treatment outcome in the Spirito et al. (2004) trial. Meanwhile, depressed mood is common among adolescent substance users (Grant et al., 2006; Kandel et al., 1999) and has demonstrated a mixed relationship with treatment outcome depending on the characteristics of the sample and the intervention (see Hersh, Curry, & Kaminer, 2014). Finally, for the socio-contextual domain, we included one measure of family factors and one measure of peer factors, as both have been independently associated with adolescent substance use outcomes (Kiesner, Poulin, & Dishion, 2010; Van Ryzin, Fosco, & Dishion, 2012). We selected problematic parent alcohol use as our indicator of family factors and peer substance involvement as our indicator of peer factors.
Although these analyses were designed to be exploratory, a few specific hypotheses were postulated. For predictors, we expected baseline alcohol use and depressed mood to be associated with poorer treatment response across both conditions. For moderators, we expected adolescents with higher levels of parental alcohol use and peer substance involvement to have better outcomes in the MET+FCU condition, due to the FCU’s emphasis on promoting parental awareness and monitoring (Dishion et al., 2002). We did not have specific hypotheses about the three demographic variables.
2. Method
The study participants, procedures, and treatment conditions have been described in detail previously (Spirito et al., 2011) and are briefly summarized below.
2.1 Participants
Adolescents were recruited in an urban level I trauma center in the Northeast United States. To be eligible, adolescents needed to self-report drinking of alcohol in the six hours before the ED visit or exhibit a positive blood alcohol concentration as tested using blood, breath, or saliva. Forty-two alcohol-positive adolescents were not approached to participate due to experiencing severe traumatic injury (n = 21), being actively suicidal (n = 17), or not speaking English or Spanish as the primary language (n = 4). Of 264 adolescents who were approached, 125 (47%) agreed to participate. Intoxication was the primary reason for admission in the majority (74%) of participants, with the remaining participants admitted for intoxication with injury or medical concern. The most common reason for non-participation was discharge from the ED prior to completion of recruitment. One hundred and thirteen adolescents (90% of randomized) received the allocated intervention and 97 (78% of randomized, 86% of treated) completed the 3 month assessment and were analyzed in the original trial.
2.2 Procedure
Study procedures were approved by the university and hospital institutional review boards. In both treatment conditions, master’s level clinicians with degrees in counseling or psychology were responsible for enrolling families in the study and conducting the consent, assessment, and MET protocols. Adolescents were not approached until their blood alcohol levels were below 0.1% and they were able to pass a mental status exam. The clinician then described the study and obtained written informed consent from parents and written assent from adolescents. The assessment battery was administered immediately prior to randomization, which was conducted using treatment assignments in sealed envelopes. Because participants in both conditions were often admitted very late in the night with high blood alcohol concentrations, most participants were scheduled to return to the ED to receive their intervention. Follow up interviews were conducted by research assistants blind to treatment assignment at 3, 6, and 12 months.
2.3 Intervention Conditions
MET
All adolescents received the MET, which was a 45-minute session that consisted of an empathetic and non-confrontational therapeutic style, paired with exploration of the teen’s motivation for drinking, review of potential negative consequences, personalized normative assessment feedback, development of goals regarding drinking, and anticipation of barriers to accomplishing goals. Independent raters evaluated each session for fidelity to the protocol and competency in treatment delivery. Fidelity ratings averaged 83% and competency ratings ranged from 83.0% to 97.0% (see Spirito et al., 2011).
MET+FCU
Families in the MET+FCU condition returned for a 1-hour videotaped family assessment task (FAsTask; Dishion & Kavanagh, 2003) that consisted of the parent(s) and teen discussing family beliefs regarding alcohol, marijuana and other drug use, as well as parent involvement in the teen’s life including parental monitoring and supervision of teens whereabouts, activities, and peers. Videos were coded by two independent raters in order to provide information about the parent and teen’s interaction patterns. A week after completion of the assessment task, parents received feedback derived from the FAsTask and from other self-report measures about family stress, parental substance use, parental supervision and monitoring, and parental beliefs about substance use. Parents were first guided through a self-assessment, then were given targeted feedback, and then were helped to develop of a plan for change. Fidelity ratings of the MET+FCU condition ranged from 79% to 100% and competence ratings ranged from 75% to 100% (see Spirito et al., 2011).
2.4 Potential Predictor and Moderator variables
Demographic Factors: Sex, Age, and Ethnicity
The adolescent’s sex, age in years, and ethnicity (i.e., Hispanic vs. non-Hispanic) were measured on a standard self-report demographic questionnaire.
Psychological Factors: Depressed Mood and Substance Use Severity
The Center for Epidemiologic Studies-Depression Scale (Radloff, 1977) was administered to the adolescent to assess self-reported depressed mood. It contains 20 depressive symptoms that are each rated on a four-point scale from 0 (rarely or none of the time) to 3 (most or all of the time) and summed for a total score. The CES-D has demonstrated high test-retest reliability and internal consistency with both adults and adolescents (Radloff, 1977; 1991). Cronbach’s alpha in this sample was .91. The measure has a well-established cutoff score (e.g., 16 or greater) to aid in identifying individuals with depressed mood, which has demonstrated good sensitivity and specificity (Cuijpers, Boluijt, & Van Straten, 2008; Field, Miguel, & Sanders, 2001). We used this cutoff score to dichotomize the variable in the analysis.
Severity of alcohol use was evaluated using the Adolescent Drinking Index (Harrell & Wirtz, 1989), a 24 item scale that assesses four dimensions of drinking problem symptoms (i.e., loss of control of drinking, social indicators, psychological indicators, and physical indicators). The ADI has demonstrated strong internal consistency, test-retest reliability, and discriminant validity in predicting diagnoses of substance use disorders (Harrell & Writz, 1989). The alpha value was .91. The ADI also has a well-established cutoff score of 16, which was used to make the variable categorical in the analysis.
Socio-Contextual Factors: Parent and Peer Substance Use
Problematic parent alcohol use was a categorical variable created from a series of questions about the parent’s drinking behaviors. The variable was intended to capture problematic alcohol use that did not rise to the level of an alcohol use disorder. Parents were classified (yes/no) as having problematic alcohol use if they reported: a) having stopped using alcohol because of problems with it in the past, b) occasionally becoming argumentative or irritable when drinking; or c) reporting having 3 or more drinks per drinking occasion “more than half the time,” i.e., indicating potential misuse that did not meet the criteria for binge drinking (National Institute of Alcohol Abuse and Alcoholism, 2004).
Peer substance involvement was measured using seven items about peer substance use and seven items about peer tolerance of adolescent substance use, adapted by Chassin and colleagues (1993) from the Monitoring the Future study (Johnston, O’Malley, & Bachman, 1988). On a 6-point scale, adolescents reported how many of their friends (1 = none to 6 = all) engaged in both occasional and regular use of alcohol, marijuana, and other drugs. Adolescents also rated on a 5-point scale whether their close friends would strongly disapprove (1) to strongly approve (6) of their engaging in these same forms of substance use. Alpha values of the peer substance use and peer tolerance of substance use items were .87 and .91, respectively. Consistent with initial report by Chassin et al. (1993), the two sets of items were highly correlated in this sample (r = .60, p < .001), and were therefore standardized and averaged to form an overall peer substance involvement score.
2.5 Dependent Variable
In the original trial, three outcome variables were collected using the Adolescent Drinking Questionnaire (ADQ; Jessor, Donovan, & Costa, 1989). The ADQ is scored on an 8-point scale and separately assesses: drinking frequency (days per month), quantity (drinks per occasion), and frequency of high-volume drinking (> 4 or 5 drinks per occasion for females and males, respectively) over the prior 3 months. We focused on frequency of high-volume drinking, since the original trial found a significant effect favoring MET+FCU over MET only on this variable.
2.6 Statistical Analyses
Prior to hypothesis testing, we conducted two preliminary analyses. First, we tested for pre-randomization differences across treatment conditions on the candidate variables. No group differences were found on any of these variables. We also conducted analyses of missing data across groups and did not find any patterns. We considered this as evidence to support the assumption that data that were missing were missing at random.
The primary outcome for all predictor/moderator analyses was frequency of high volume drinking at 3 months, which was measured on an 8-point ordinal scale. We used an analysis of covariance (ANCOVA) approach (i.e., follow-up variable regressed on baseline and other predictors) with an ordinal logistic model to accommodate the ordinal scale of the dependent variable. Separate ANCOVA models regressed high volume drinking at 3 months on baseline values of high volume drinking, treatment condition, each candidate variable, and the interactive effects of these variables. A candidate variable was considered a moderator if it demonstrated a significant (candidate × treatment) interaction on the 3-month outcome. Candidate variables that demonstrated a significant main effect on outcome without a significant (candidate × treatment) interaction were considered predictors. All variables were centered (Kraemer & Blasey, 2004) and continuous predictors were standardized to two standard deviations (Gelman, 2008) to put coefficients on the same scale as the dichotomous variables. Significant interactions between potential moderators and treatment condition were probed using simple intercepts and simple slopes (Preacher et al, 2006), estimated for treatment and control groups and sub-groups with and without the given moderator.
Given the sample size and associated power, our analyses were exploratory in nature and did not adjust for multiple comparisons. We use a standard statistical significance criterion of p < .05 and note p-values between .05 and .10 as statistical trends. Effect sizes are reported using Cohen’s (1988) f2 statistic, a measure of the proportion of unexplained variability in the outcome that is attributable to the moderator by treatment assignment interaction effect; values of .02 are considered small, .15 are considered medium, and .35 are considered large.
3. Results
3.1 Sample Characteristics
The final sample of 97 adolescents was almost evenly split between male (46%) and female (54%) and was predominantly Non-Hispanic White (67%). Hispanics comprised 26% of the sample. Sixty percent of the sample were older adolescents aged 16–17 years and 40% were younger adolescents aged 13–15 years. At baseline, 40% of the adolescents screened positive for an alcohol use problem on the ADI and 30% were in the clinical range for depressed mood on the CES-D. Adolescent self-reported rates of high volume drinking over the prior 90 days covered the full range: 14% reported never engaging in high volume drinking, 60% reported engaging in high volume drinking less than once a month, and 26% reported engaging in high volume drinking at least monthly. Based on parent self-report, 23% of the parents had problematic alcohol use.
3.2 Replication of Original Trial Results
Before testing predictors and moderators of outcome, we attempted to replicate the primary outcome analyses from the original comparative trial (Spirito et al., 2011), which used. the generalized estimating equation (GEE) procedure. ANCOVA modeling found that those in the MET+FCU condition had significantly lower levels of high volume drinking than those in the MET only condition at the 3 month assessment, but not at the 6 or 12 month assessment. This pattern of results was identical to those reported in the original trial.
3.3 Predictors
Table 1 presents the p-value results of the omnibus tests of each of the seven candidate variables. Of the seven variables, there was one significant predictor, one significant moderator, and one statistical trend for moderation.
Table 1.
Variables Examined as Potential Predictors and Moderators of Acute High Volume Drinking
| Potential Moderator | Main Effect P-Value | Main Effect ES | Interaction P-Value | Interaction ES | Status |
|---|---|---|---|---|---|
| Demographics | |||||
| Gender | .48 | .05 | .99 | .03 | |
| Age | .04* | .07 | .99 | .01 | Predictor |
| Hispanic ethnicity | .28 | .03 | .99 | .01 | |
| Psychological Factors | |||||
| Baseline alcohol use | .17 | .08 | .40 | .01 | |
| Depression | .37 | .02 | .38 | <.01 | |
| Social/Contextual | |||||
| Parent problematic use | .37 | .01 | .04* | .03 | Moderator |
| Peer substance involvement | .44 | .03 | .07+ | .02 | Moderator (trend) |
Note. ES = effect size. Effect sizes are computed using Cohen’s f2 statistic, which summarizes differences in model R2, and where values of.02, .15, and .35 indicate small, medium, and large effects, respectively.
p < .05,
p = 0.07.
The only significant predictor of outcome was the adolescent’s age. Across both treatment conditions, older adolescents had higher levels of high volume drinking at 3 months than younger adolescents, even when controlling for baseline status, b = 1.48, z = 2.03, p < .05, 95% CI [.05 to 2.91]. This effect was small to medium in size. These data suggest that older adolescents had worse acute treatment outcomes, regardless of treatment condition.
3.4 Moderators
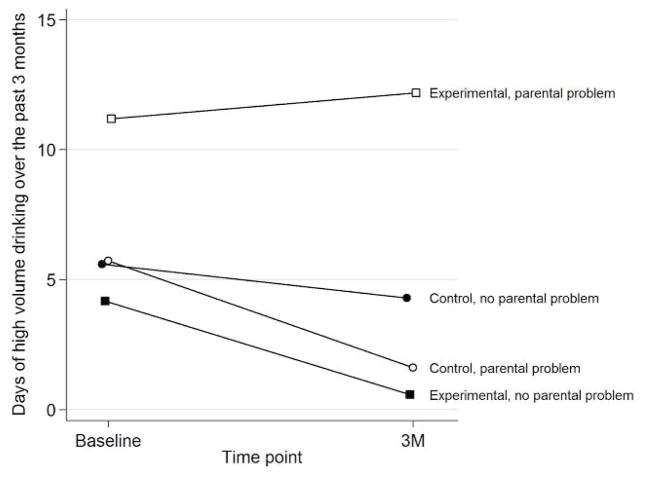
As shown in Table 1, problematic parent alcohol use significantly moderated the effect of treatment condition at 3 months, b = 2.97, z = 2.03, p < .05, 95% CI [.10, 5.83]. The moderation effect was small in size (f2 = 0.03).
Figure 1 depicts the problematic parent alcohol use × treatment interaction by plotting the level of high volume drinking at each timepoint. To facilitate visual depiction of the interaction, we converted the 8-point high volume drinking scale into a weighted estimate of raw drinking days over the past 90 days. Counter to hypotheses, among those parents with problematic alcohol use, MET+FCU had a negative effect on outcome relative to MET only. These results suggest that the superiority of MET+FCU over MET found in the original trial was driven by those whose parents did not have problematic alcohol use at baseline.
Figure 1.
There was also a statistical trend with a small effect size for peer substance involvement to moderate the effect of treatment condition at 3 months, b = 2.51, z = 1.76, p = .08, 95% CI [−.29, 5.31]. Examination of this interaction indicated that adolescents with higher levels of peer substance involvement at baseline appeared to respond better to MET+FCU than the MET only intervention.
4. Discussion
This study explored possible predictors and moderators of outcome across two brief, MET models in the ED setting: adolescent MET-only and MET+FCU. Older adolescents had worse treatment outcomes regardless of treatment assignment. Parent problematic alcohol use was associated with significantly less favorable response to MET+FCU than MET only, and there was also a trend for higher levels of peer substance use to be associated with better response to MET+FCU.
The identification of age as a significant predictor was consistent with prior literature indicating that younger and older adolescents respond better to different types of treatment. Kaminer and colleagues (2002) found that older adolescents did not respond as well as younger adolescents to cognitive behavioral therapy, while Henggeler and colleagues (1999) found that younger adolescents responded better than older adolescents to multisystemic therapy (a family-focused approach). Some researchers have argued that brief interventions are appropriate for adolescents with less entrenched substance use behaviors, whereas longer interventions are needed for adolescents with more serious problems (see Goti et al., 2010). Of note, in this sample, baseline severity of alcohol use was not a predictor of outcome. Thus, one possible interpretation of our finding that younger adolescents were more susceptible to the two brief MET models is that they had less entrenched patterns of alcohol use, but that these patterns were not detectable on a simple measure of alcohol-related problems.
Our finding that parent alcohol use was associated with less favorable response to FCU plus MET was unexpected and counter to our hypotheses. By providing individualized feedback within a motivational interviewing style, the FCU aims to enhance parental recognition of specific risk behaviors (including parents’ own substance use) and engender motivation for reducing these problem behaviors. The current results indicate that adolescents of parents who demonstrated problematic alcohol use at baseline, one of the specific risk factors that the FCU is designed to address, had the poorest response to the intervention. A possible interpretation of these findings is that the FCU’s attempt to increase parents’ awareness of how their drinking affected their teen’s alcohol use was either insufficient or actually sparked resistance among those parents with problematic alcohol use. While the adolescent MET was designed to accommodate adolescents across all levels of readiness to change, the FCU did not take into account the parent’s readiness for change. Future work should explore if the outcomes of the FCU can be improved by taking into account the family’s readiness to support all aspects of the planned intervention. Another consideration is that the joint family assessment task discussing beliefs about alcohol use may have had deleterious effects if the parent had problematic use. A second interesting direction for future research would be to examine if the FCU’s effectiveness could be enhanced by having parents and adolescents conduct parts of the assessment task separately before coming together.
The small effect size statistical trend for peer substance involvement to moderate treatment outcome also bears mention. Consistent with our hypotheses, adolescents with higher levels of peer substance involvement appeared to respond better to MET+FCU than adolescent MET only. It appears that the FCU’s focus on parental monitoring and supervision may have conferred incremental benefit over the MET’s generic focus on peer alcohol use norms and on change planning in terms of countering the effects of peer substance involvement. These results are consistent with previous literature demonstrating that interventions are most efficacious for adolescents who demonstrate the specific risk factors interventions were designed to target (Tien, Sandler, MacKinnon, & Wolchik, 2004; Prado et al., 2013). Replication of these findings in a larger sample is needed to bolster confidence.
4.1 Limitations
Results must be interpreted in the context of several limitations. First, the study was adequately powered to compare the two treatment conditions, but was not powered to test multiple moderators across the two conditions. As noted by Garcia and colleagues (2010), the “absence of findings should not be interpreted as findings of absence”. This work should be viewed as exploratory and hypothesis generating. Second, results should not be generalized beyond the current sample, which was predominantly comprised of relatively infrequent high volume drinkers (i.e., 76% reported engaging in high volume drinking less than monthly) that sought care in an ED. Future research is needed to determine the extent to which the current results extend to adolescents with different demographic and clinical characteristics. Third, most of the significant effects in this study were small in size, which may reflect the relatively low levels of high volume drinking at baseline. These results suggest that replication among more frequent high volume drinkers is warranted. Finally, we only examined the effects of Hispanic ethnicity on treatment outcomes and did not test treatment differences between racial groups. Given that race and ethnicity do not capture the within group heterogeneity that exists among racial and ethnic groups, future studies should consider examining variables that capture this within- group variability as well as help explain the inconsistent findings previous studies have demonstrated (Clair et al., 2013; Liddle, Rowe, Dakof, Henderson & Greenbaum, 2009; Robbins et al., 2008; Waldron & Turner, 2008). Relevant variables may include levels of acculturation, language, perceived discrimination, and racial/ethnic identity salience and pride.
4.2 Clinical Implications
The current findings extend the conclusion of the primary trial that adolescents presenting to the ED due to an alcohol-related event who receive the MET+FCU have better acute outcomes than adolescents who receive MET only. The previous study’s findings are extended by specifically asking and answering a significant question: “which intervention approach has the best acute outcomes for whom?” Overall, the results indicate that MET interventions at both the adolescent and parent level may be less effective and require adaptation for older adolescents. Our results also suggest that adolescents whose parents have problematic alcohol use are less likely to benefit from the addition of the FCU, while adolescents with high levels of peer substance involvement may be more likely to benefit from the FCU. These results provide mixed evidence for the notion that adolescents may be more amenable to interventions that are tailored to or that address their specific risks. Taken together, these results provide information for tailoring MET interventions according to the adolescents’ demographic, psychological, and socio-contextual risk factors, including the parent’s level of alcohol use. Such information can be of value to researchers and key stakeholders responsible for implementing evidence based interventions by identifying subpopulations that may benefit most from specific intervention strategies.
Highlights.
A 2011 trial of alcohol-positive adolescents presenting to the emergency department (ED) found that adolescent + parent motivational enhancement therapy (MET) reduced high volume drinking better than adolescent MET only.
Seven variables were tested as potential predictors or moderators of high volume drinking at 3 months post-treatment.
Older adolescents (age 16–18) had worse drinking outcomes than younger adolescents (age 13–15) in both MET conditions.
Adolescents whose parents screened positive for problematic alcohol use had worse drinking outcomes with adolescent + parent MET than adolescent MET only.
Alcohol-positive adolescents presenting to the ED may respond better to MET if they are under the age of 16 and involving parents with problematic alcohol use in MET may have negative effects on adolescent high volume drinking.
Acknowledgments
Original data collection was supported by AA013385 (PI: Spirito) from the National Institute on Alcohol Abuse and Alcoholism. The lead author’s contribution to this manuscript was supported by K23DA031743 (PI: Becker) from the National Institute on Drug Abuse. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Addiction Technology Transfer Center (ATTC) Workgroup. ATTC white paper: Integrating substance use disorder and health care services in an era of healthcare reform. University of Missouri, Kansas City: ATTC Network Coordinating Office; 2015. [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Becker SJ, Curry JF, Yang C. Factors that influence trajectories of change in frequency of substance use and quality of life among adolescents receiving a brief intervention. Journal of Substance Abuse Treatment. 2011;41(3):294–304. doi: 10.1016/j.jsat.2011.04.004. [DOI] [PubMed] [Google Scholar]
- Becker SJ, Stein GL, Curry JF, Hersh J. Ethnic differences among substance- abusing adolescents in a treatment dissemination project. Journal of Substance Abuse Treatment. 2012;42(3):328–336. doi: 10.1016/j.jsat.2011.08.007. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Edwards E, Dorfman D, Heeren T, Bliss C, Bernstein J. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Academic Emergency Medicine. 2009;16(11):1174–1185. doi: 10.1111/j.1553-2712.2009.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein J, Heeren T, Edward E, Dorfman D, Bliss C, Winter M, Bernstein E. A brief motivational interview in a pediatric emergency department, plus 10-day telephone follow-up, increases attempts to quit drinking among youth and young adults who screen positive for problematic drinking. Academic Emergency Medicine. 2010;17(8):890–902. doi: 10.1111/j.1553-2712.2010.00818.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Pillow DR, Curran PJ, Molina BS, Barrera M., Jr Relation of parental alcoholism to early adolescent substance use: a test of three mediating mechanisms. Journal of Abnormal Psychology. 1993;102(1):3. doi: 10.1037//0021-843x.102.1.3. [DOI] [PubMed] [Google Scholar]
- Cohen JE. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1988. [Google Scholar]
- Clair M, Stein LA, Soenksen S, Martin RA, Lebeau R, Golembeske C. Ethnicity as a moderator of motivational interviewing for incarcerated adolescents after release. Journal of Substance Abuse Treatment. 2013;45:370–375. doi: 10.1016/j.jsat.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coatsworth JD, Santisteban DA, McBride CK, Szapocznik J. Brief strategic Family therapy versus community control: engagement, retention, and an exploration of the moderating role of adolescent symptom severity. Family Process. 2001;40(3):313–332. doi: 10.1111/j.1545-5300.2001.4030100313.x. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Boluijt P, Van Straten A. Screening of depression in adolescents through the Internet. European Child & Adolescent Psychiatry. 2008;17(1):32–38. doi: 10.1007/s00787-007-0631-2. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Chermack ST, Zimmerman MA, Shope JT, Bingham CR, Blow FC, Walton MA. Brief motivational interviewing intervention for peer violence and alcohol use in teens: one-year follow-up. Pediatrics. 2012;129(6):1083–1090. doi: 10.1542/peds.2011-3419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Chermack ST, Ehrlich PF, Carter PM, Booth BM, Blow FC, … Walton MA. Alcohol interventions among underage drinkers in the ED: a randomized controlled trial. Pediatrics. 2015;136(4):e783–e793. doi: 10.1542/peds.2015-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry J, Rohde P, Simons A, Silva S, Vitiello B, Kratochvil C, … Weller E. Predictors and moderators of acute outcome in the Treatment for Adolescents with Depression Study (TADS) Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(12):1427–1439. doi: 10.1097/01.chi.0000240838.78984.e2. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Kavanagh K. Intervening in adolescent problem behavior: A family- centered approach. New York, NY: Guilford Press; 2003. [Google Scholar]
- Dishion TJ, Nelson SE, Kavanagh K. The family check-up with high-risk young adolescents: Preventing early-onset substance use by parent monitoring. Behavior Therapy. 2003;34(4):553–571. [Google Scholar]
- Dishion TJ, Kavanagh K, Schneiger A, Nelson S, Kaufman NK. Preventing early adolescent substance use: A family-centered strategy for the public middle school. Prevention Science. 2002;3(3):191–201. doi: 10.1023/a:1019994500301. [DOI] [PubMed] [Google Scholar]
- D’Onofrio G, Fiellin DA, Pantalon MV, Chawarski MC, Owens PH, Degutis LC, … O’Connor PG. A brief intervention reduces hazardous and harmful drinking in emergency department patients. Annals of emergency medicine. 2012;60(2):181–192. doi: 10.1016/j.annemergmed.2012.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Miguel D, Sanders C. Adolescent depression and risk factors. Adolescence. 2001;36(143):491. [PubMed] [Google Scholar]
- Gelman A. Scaling regression inputs by dividing by two standard deviations. Statistics in Medicine. 2008;27(15):2865–2873. doi: 10.1002/sim.3107. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, … Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Alcohol Research & Health. 2006;29(2):107–120. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Harrell AV, Wirtz PW. Screening for adolescent problem drinking: Validation of a multidimensional instrument for case identification. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989;1(1):61. [Google Scholar]
- Henggeler SW, Pickrel SG, Brondino MJ. Multisystemic treatment of substance-abusing and-dependent delinquents: Outcomes, treatment fidelity, and transportability. Mental Health Services Research. 1999;1(3):171–184. doi: 10.1023/a:1022373813261. [DOI] [PubMed] [Google Scholar]
- Hernandez L, Lavingne A, Wood M, Weirs RW. Moderators and mediators of treatments for youth with substance use disorders. In: Maric M, Prins PJM, Ollendick TH, editors. Moderators and Mediators of Youth Treatment Outcomes. Oxford University Press; 2015. pp. 174–209. [Google Scholar]
- Hersh J, Curry JF, Kaminer Y. What is the impact of comorbid depression on Adolescent substance abuse treatment? Substance Abuse. 2014;35(4):364–375. doi: 10.1080/08897077.2014.956164. [DOI] [PubMed] [Google Scholar]
- Jessor R, Donovan JE, Costa FM. Health Behavior Questionnaire. Boulder, CO: University of Colorado; 1989. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG. Drug use among American college students and their non-college age peers. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 1988. (Monitoring the Future Occasional Paper No. 25.) [Google Scholar]
- Johnston BD, Rivara FP, Droesch RM, Dunn C, Copass MK. Behavior change counseling in the emergency department to reduce injury risk: a randomized, controlled trial. Pediatrics. 2002;110(2):267–274. doi: 10.1542/peds.110.2.267. [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Burleson JA, Goldberger R. Cognitive-behavioral coping skills and psychoeducation therapies for adolescent substance abuse. The Journal of Nervous and Mental Disease. 2002;190(11):737–745.2. doi: 10.1097/00005053-200211000-00003. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Johnson JG, Bird HR, Weissman MM, Goodman SH, Lahey BB, … Schwab-Stone ME. Psychiatric comorbidity among adolescents with substance use disorders: Findings from the MECA study. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(6):693–699. doi: 10.1097/00004583-199906000-00016. [DOI] [PubMed] [Google Scholar]
- Kiesner J, Poulin F, Dishion TJ. Adolescent substance use with friends: Moderating and mediating effects of parental monitoring and peer activity contexts. Merrill-Palmer quarterly (Wayne State University Press) 2010;56(4):529. doi: 10.1353/mpq.2010.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Blasey CM. Centring in regression analyses: a strategy to prevent errors in statistical inference. International Journal of Methods in Psychiatric Research. 2004;13:141–151. doi: 10.1002/mpr.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Liddle HA, Rowe CL, Dakof GA, Henderson C, Greenbaum P. Multidimensional Family Therapy for early adolescent substance abusers: Twelve month outcomes of a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2009;77(1):12–25. doi: 10.1037/a0014160. [DOI] [PubMed] [Google Scholar]
- McDonald AJ, Wang N, Camargo CA. US emergency department visits for alcohol-related diseases and injuries between 1992 and 2000. Archives of Internal Medicine. 2004;164(5):531–537. doi: 10.1001/archinte.164.5.531. [DOI] [PubMed] [Google Scholar]
- Mitchell SG, Gryczynski J, O’Grady KE, Schwartz RP. SBIRT for adolescent drug and alcohol use: Current status and future directions. Journal of Substance Abuse Treatment. 2013;44(5):463–472. doi: 10.1016/j.jsat.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) NIAAA council approves definition of binge drinking. NIAAA Newsletter. 2004;(3) Available at: http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf.
- Prado G, Huang S, Cordova D, Malcolm S, Estrada Y, Cano N, … Brown CH. Ecodevelopmental and intrapersonal moderators of a family based preventive intervention for Hispanic youth: A latent profile analysis. Prevention Science. 2013;14(3):290–299. doi: 10.1007/s11121-012-0326-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of educational and behavioral statistics. 2006;31(4):437–448. [Google Scholar]
- Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurements. 1977;1(3):385–401. [Google Scholar]
- Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. Journal of Youth and Adolescence. 1991;20(2):149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Robbins MS, Szapocznik J, Dillon FR, Turner CW, Mitrani VB, Feaster DJ. The efficacy of structural ecosystems therapy with drug abusing/dependent African American and Hispanic American adolescents. Journal of Family Psychology. 2008;22(1):51–61. doi: 10.1037/0893-3200.22.1.51. [DOI] [PubMed] [Google Scholar]
- Spirito A, Monti PM, Barnett NP, Colby SM, Sindelar H, Rohsenow DJ, … Myers M. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. The Journal of Pediatrics. 2004;145(3):396–402. doi: 10.1016/j.jpeds.2004.04.057. [DOI] [PubMed] [Google Scholar]
- Spirito A, Sindelar-Manning H, Colby SM, Barnett NP, Lewander W, Rohsenow DJ, Monti PM. Individual and family motivational interventions for alcohol-positive adolescents treated in an emergency department: results of a randomized clinical trial. Archives of Pediatrics & Adolescent Medicine. 2011;165(3):269–274. doi: 10.1001/archpediatrics.2010.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strada MJ, Donohue B, Lefforge N. Examination of Ethnicity in Controlled Treatment Outcome Studies Involving Adolescent Substance Abusers. Psychology of Addictive Behaviors. 2006;20:11–27. doi: 10.1037/0893-164X.20.1.11. [DOI] [PubMed] [Google Scholar]
- Tamm L, Trello-Rishel K, Riggs P, Nakonezny PA, Acosta M, Bailey G, Winhusen T. Predictors of treatment response in adolescents with comorbid substance use disorder and attention-deficit/hyperactivity disorder. Journal of Substance Abuse Treatment. 2013;44(2):224–230. doi: 10.1016/j.jsat.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner-Smith EE, Lipsey MW. Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment. 2015;51:1–18. doi: 10.1016/j.jsat.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tein JY, Sandler IN, MacKinnon DP, Wolchik SA. How did it work? Who did it work for? Mediation in the context of a moderated prevention effect for children of divorce. Journal of Consulting and Clinical Psychology. 2004;72:617–624. doi: 10.1037/0022-006X.72.4.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ryzin MJ, Fosco GM, Dishion TJ. Family and peer predictors of substance use from early adolescence to early adulthood: An 11-year prospective analysis. Addictive Behaviors. 2012;37(12):1314–1324. doi: 10.1016/j.addbeh.2012.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical Child & Adolescent Psychology. 2008;37(1):238–261. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- Wallace ML, Frank E, Kraemer HC. A novel approach for developing and interpreting treatment moderator profiles in randomized clinical trials. JAMA Psychiatry. 2013;70(11):1241–1247. doi: 10.1001/jamapsychiatry.2013.1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, Cunningham RM. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA. 2010;304(5):527–535. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]