Supplemental Digital Content is available in the text.
Keywords: acute care, case management, frequent visitors, randomized-controlled trial, Sweden
Abstract
Background
A small group of frequent visitors to Emergency Departments accounts for a disproportionally large fraction of healthcare consumption including unplanned hospitalizations and overall healthcare costs. In response, several case and disease management programs aimed at reducing healthcare consumption in this group have been tested; however, results vary widely.
Objectives
To investigate whether a telephone-based, nurse-led case management intervention can reduce healthcare consumption for frequent Emergency Department visitors in a large-scale setup.
Methods
A total of 12 181 frequent Emergency Department users in three counties in Sweden were randomized using Zelen’s design or a traditional randomized design to receive either a nurse-led case management intervention or no intervention, and were followed for healthcare consumption for up to 2 years.
Results
The traditional design showed an overall 12% (95% confidence interval 4–19%) decreased rate of hospitalization, which was mostly driven by effects in the last year. Similar results were achieved in the Zelen studies, with a significant reduction in hospitalization in the last year, but mixed results in the early development of the project.
Conclusion
Our study provides evidence that a carefully designed telephone-based intervention with accurate and systematic patient selection and appropriate staff training in a centralized setup can lead to significant decreases in healthcare consumption and costs. Further, our results also show that the effects are sensitive to the delivery model chosen.
Introduction
Across most healthcare systems, a small group of patients account for a large proportion of total healthcare costs. One important factor behind the costs is a high frequency of Emergency Department visits 1–4. Although the concentration of resources to a small patient group is expected in most situations when few patients are affected by disease, patients with frequent Emergency Department visits often receive suboptimal care, leading to larger than expected costs and likely poor quality of care 5. This concentration of healthcare resources has been recognized both as an economic challenge and as an opportunity for targeted prevention. As such, several case and disease management programs aiming to improve the care of frequent Emergency Department visitors have been developed and implemented 6. However, the results have been highly variable, with some showing reductions in healthcare costs 7–11 and other investigations indicating no significant change, or even increased healthcare consumption 12,13.
The overall aim of this study was to evaluate a telephone-based case management intervention targeted at reducing healthcare expenditure for frequent Emergency Department visitors. Hence, the study presents a gradually modified intervention where a more basic model was used during the start of the study and later results reflect an improved, more experienced intervention.
Methods
We have previously reported results from the pilot phase of this intervention from 2010 14. On the basis of promising results, we expanded the original pilot to include five counties (three of which are included in this analysis) with longer follow-up. Throughout the study, both the patient selection process and the case management intervention were gradually developed in an iterative, adaptive manner.
Setting
The study was carried out within five counties in Sweden, where health services are almost exclusively financed through taxes and small patient fees. The first patients were included at the Karolinska University Hospital in Stockholm County in 2010 and subsequently expanded to include additional hospitals in Stockholm and in four additional counties of Sweden (Supplementary Table 1, Supplemental digital content 1, http://links.lww.com/EJEM/A91).
Study design and patient inclusion
Depending on local requirements and preferences, two different randomization methods were used (Fig. 1a and b). In Stockholm County, the study was based on Zelen’s design (ZD), where patients randomized to the intervention group are asked for informed consent after randomization 15. Because patients randomized to the control group are not contacted or informed about participation, ZD is both an effective study design and avoids the possibility of a Hawthorne effect, which may lead to modified behavior in patients who are not offered the intervention. In the Västra Götaland region and Uppsala County, it was decided, instead, to follow a traditional randomized-controlled trial (RCT) study design, where participants are asked for consent before randomization.
Fig. 1.
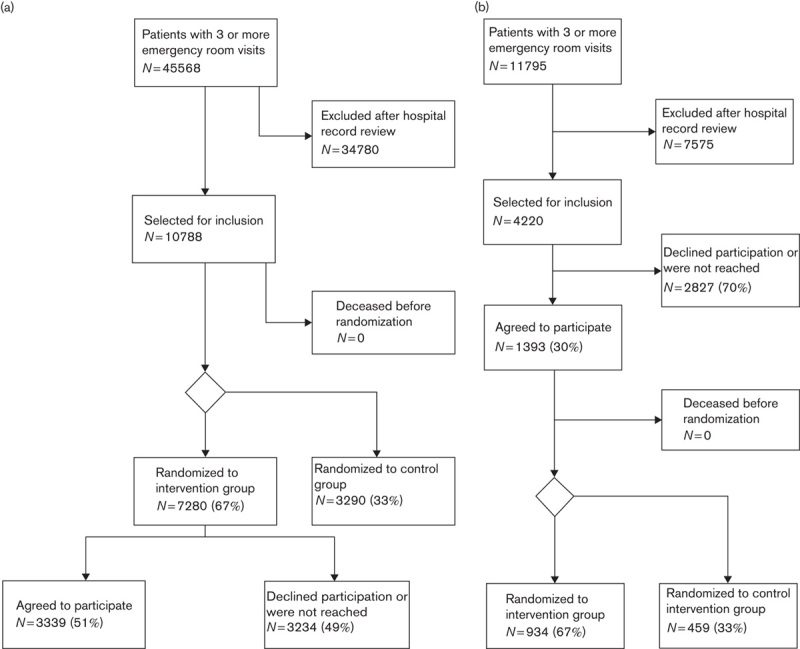
(a) Recruitment of patients under the Zelen design in Stockholm County from 2010 to 2014. (b) Recruitment of patients under the traditional RCT design, in Uppsala and Västra Götaland counties, from 2012 to 2014. RCT, randomized-controlled trial.
The patient inclusion followed the same three-step process at all participating sites. All patients with three or more Emergency Department visits during the previous 6 months were screened for inclusion. This threshold was used as it had previously been found to be predictive of a sustained high healthcare consumption and as it identified a meaningfully large population 14. A medical record review was then performed to exclude patients with dementia, severe hearing impairment, and/or a psychotic disorder, as well as terminally ill patients. Finally, qualitative manual screening was performed to identify patients deemed at risk of sustained high healthcare consumption as well as receptive to the intervention on the basis of criteria to determine the extent to which patients’ care consumption was avoidable. Typically, screening aimed to identify patients who seemed to be lacking in healthcare literacy, sought care at an improper level, or from too many providers. During the pilot phase, the screening was performed by one of two physicians, but in late 2010, when the rate of patient inclusion increased, this task was taken over by the case management nurses. In the county that followed ZD, all patients who fulfilled both the quantitative and the qualitative criteria were randomized weekly. In counties with a traditional RCT design, eligible patients were asked for consent before being directly randomized to control or intervention. Randomization was not blinded, but all randomization was performed using a central random number generator.
Study intervention
All patients who were randomized to the intervention arm were first invited to an introductory appointment with one of the study nurses, during which the patients underwent a structured interview to obtain information on the patients’ medical and social history. The information obtained during the interview was used to guide the intervention.
At the initial interview, a personalized support plan was designed on the basis of a standardized protocol. Telephone contact was made on a regular basis using the case and disease management concept developed by Reinius et al. 14. Importantly, nurses provided no medical advice, but rather facilitated contacts with healthcare providers, coached patients’ disease self-management, and supported interactions with social services. The participating nurses in all three counties were employed by a private entity, Health Navigator, which was contracted by the respective counties’ administration.
Frequent interim monitoring was performed throughout the study to provide each nurse with feedback on the results of their patients. The results of the monitoring were used to iteratively refine the screening process and the nurse intervention. This adaptive model, where both quantitative and qualitative results obtained during the study were used to modify the study, resulted in a gradually modified intervention, moving from a basic executed model during the early years (2010–2012) with noncentralized screening and recruitment, to a standardized model with partly automated and statistically driven patient selection, a controlled and electronically supported nurse-driven intervention and continuous follow-up and feedback. Major developments of the screening process and nurse intervention are outlined in Supplementary Table 2, Supplemental digital content 1 (http://links.lww.com/EJEM/A91).
Follow-up and statistical analyses
Patients were followed from the date of randomization until the date of death, end of follow-up (31 March 2014), or for a maximum of 2 years. Only patients randomized before 1 March 2014 were included in the analyses. A priori, we focused on two primary endpoints: the number of hospitalizations and the number of outpatient doctor appointments. We also included three secondary endpoints: total healthcare cost, defined as all-care consumption for days in hospital for inpatient care, and all primary and secondary care visit costs for outpatient care, as well as number of emergency visits and mortality, with the latter included mainly as a safety endpoint. Finally, we also considered the total number of days in hospital as an additional outcome. All outcome incidences were obtained through electronic medical record systems using individually unique national registration numbers that are assigned to all Swedish residents 16. The record linkages provided detailed information on all hospital admissions and outpatient visits, as well as costs of all healthcare services, thus ensuring almost no missing data.
We tested for baseline differences in age, sex distribution, prevalence of selected common diagnoses, and previous healthcare consumption using Wilcoxon tests for continuous variables and χ2-tests for categorical variables. Relative risks of healthcare consumption, expressed as incidence rate ratios (IRRs), comparing participants and control patients, were estimated using negative binomial regression. IRRs were used to allow patients to contribute several events for each outcome. To reduce overdispersion, we included time in study as the main time axis in the regression model using a restricted cubic spline with five knots. The regression model also included a categorical term for whether the individual was included as a participant or a control as well as the logarithm of time at risk as an offset. Differences in costs were analyzed using nonparametric bootstrap tests and number of days in hospital with Wilcoxon tests. All analyses were carried out on an intention-to-treat basis.
One set of analyses was carried out for the studies following ZD and one for those following a traditional RCT design. All costs were converted into Euros on the basis of current exchange rates. Because we made iterative changes to the intervention, we also stratified the analyses by calendar year of randomization. Tests for homogeneity were performed by fitting interactions between the study group variable and the variables for sex, age, and calendar year of randomization. P-values less than 0.05 were considered statistically significant. All statistical analyses were carried out using SAS Statistical Analysis Software, version 9.4 (Cary, North Carolina, USA). The study was registered at clinicaltrials.org (Nr: NCT01985074).
Ethical approval was obtained separately in all five counties where the intervention was implemented (Supplementary table 3, Supplemental digital content 1, http://links.lww.com/EJEM/A91). We also obtained separate ethical approval for the pooled analysis of all studies (Nr: 2013/2012-32).
Results
Study participants
The patient identification process is presented in Fig. 1a and b for the ZD and traditional RCT studies, respectively. Data from three counties were included in this analysis. In Stockholm County, which followed the ZD, 10 788 were randomized. Of these, 7280 (67%) were allocated to receive the study intervention (intervention group) and 3508 (32%) were allocated to the control group. Among patients randomized to receive the intervention, 3635 (50%) agreed to actively participate in the study (participants) and 3645 (50%) declined to participate or could not be reached by telephone or letter (nonparticipants). In the two counties following the traditional RCT design, 4220 patients were approached about participating in the study. Of these, 1393 (33%) agreed to participate, whereof 934 (67%) were randomized to receive the intervention (intervention group) and the remaining 459 (33%) were assigned to the control group.
Table 1 presents the baseline characteristics of the 12 181 randomized patients. Of these, 10 788 were randomized in the ZD study and 1393 were assigned to the traditional RCTs. There were no differences in age or sex distribution, or in previous healthcare consumption.
Table 1.
Characteristics of the two study populations stratified by study design

Overall results
The protocol changes that were made throughout the study period, both pertaining to patient selection and the intervention itself, are clearly reflected in tests for heterogeneity, which showed that the effect of the intervention differed significantly with year of randomization for both inpatient and outpatient care in both studies (P<0.001). We observed no overall significant differences in the risk of hospitalization in the ZD studies: IRR 0.99 [95% confidence interval (CI) 0.95–1.02]. In the traditional RCT centers, however, there was a significant overall decrease in the risk of hospitalization in the intervention group compared with controls with IRRs of 0.88 (95% CI 0.81–0.96). For outpatient doctors’ visits, we observed an increase in the frequency of outpatient visits for intervention patients for ZD with IRRs of 1.05 (95% CI 1.04–1.06) and a slight increase for traditional RCT with IRRs of 1.05 (95% CI 1.01–1.08). Irrespective of the randomization method, there were no significant differences in either total healthcare costs or the number of days in hospital (data not shown).
Results stratified by year of inclusion
In light of both the marked heterogeneity and of the continuous change in the patient inclusion process and the study intervention, the analyses were stratified by year of randomization, which we considered a more relevant presentation of the results. In Stockholm County, which followed ZD, we observed a significant decrease in outpatient care in patients included in 2010, with an IRR of 0.79 (95% CI 0.75–0.83), and the number of hospitalizations for those included in 2013, with an IRR of 0.85 (95% CI 0.79–0.90). At the same time, we also observed significantly increased rates of both outpatient and emergency outpatient visits for patients included in 2011 and in 2012 (Table 2). The analysis of cost and number of days in hospital is presented in Table 3, which showed sustained albeit nonsignificant decreases in the mean number of days in hospital and costs from 2010 to 2012. Only for patients included in 2013 did we observe a statistically significant decrease in both the number of days intervention patients spent in hospital compared with controls (14% reduction; P=0.007) and the average cost per patient per year, which decreased by 16% from €7343 per patient per year to €6183 (P=0.004).
Table 2.
Risk of hospitalization, emergency, and doctor visits for frequent visitors in both Zelen and RCT centers by year of randomization

Table 3.
Average number of hospital days and total costs presented by study design and stratified by calendar year of randomization

In the studies following the traditional RCT design, we observed no differences between the intervention and the control groups among patients included in 2012, but for patients included in 2013, there was again a significant reduction in hospitalization rates (IRR 0.77; 95% CI 0.69–0.86) (Table 2). There were no significant differences in the healthcare costs or number of days in hospital for patients included in 2012 or 2013 (Table 3).
We observed no significant differences in the risk of death between the intervention and the control groups in either study (data not shown).
Discussion
Here, we present the development, implementation, and results of a large adaptive multi-center study of a telephone-based case management intervention. The significant decrease in hospitalizations in the traditional RCT study centers and in the ZD center during the final year of data collection provides new support for the potential of such interventions in reducing avoidable healthcare consumption. At the same time, the variability in the results – even within this trial – provides insights into the difficulty of achieving positive health effects in this challenging patient group.
Although this study is, to our knowledge, the largest trial of a telephone-based case management intervention for frequent Emergency Department visitors in the literature to date, it is also unusual in that we have continuously modified both the patient inclusion process and the intervention that the included patients received. Hence, we emphasize that the variable results – with some periods of increased healthcare consumption in the patients receiving the intervention but ultimately a decreased healthcare consumption – are in line with expectations, given the gradual development of the intervention. In particular, the period 2011–2012, when increased healthcare consumption was noted among the intervention patients, coincided with a rapid operational expansion, hiring of many new study nurses, and a large influx of patients (Supplementary Figures 1, Supplemental digital content 1, http://links.lww.com/EJEM/A91 and 2, Supplemental digital content 1, http://links.lww.com/EJEM/A91). As such, and given that we are able to achieve positive results for both study designs in three somewhat different settings, we are cautiously optimistic about the intervention model.
This study is also the first RCT that we are aware of that has used both ZD and traditional recruitment designs. We started with ZD in Stockholm as we believed this to be an appropriate design where a ‘placebo’ intervention could not realistically be offered. However, on account of the unexpectedly high rate of nonparticipation, it was decided that additional counties joining the study after 2011 would use the traditional RCT method. Although the large nonparticipation rate significantly impaired the efficiency of the ZD study, in that only half of those randomized to the active arm chose to receive the intervention, it could be argued that this design more accurately mimics the effect that such an intervention would have if implemented in a real clinical setting, where nonparticipation is a reality. As such, we believe that the ability to present data from both study designs is informative.
In Stockholm County, we observed a significant decrease in outpatient care consumption among the few patients included in 2010. After a large scale-up and restructuring during 2011 and 2012, significant decreases in hospitalizations were achieved in 2013. This translated into a significant decrease in the number of days in hospital of 1 day per patient-year and a 15% decrease in the total healthcare cost per patient per year. In the other two counties, we observed an overall decrease in the rate of hospitalization as well as a more pronounced decrease in 2013. However, although both findings were significant, neither translated into significant cost benefits. The increased frequency of outpatient visits that we observed in the ZD study in patients included in the period 2011–2012 and in the traditional RCT centers in their first year (2012) is not readily explained. However, we speculate that it may have resulted from the case management nurses resorting to recommending the often very ill patients to seek emergency medical care upon telephone contact. As such, during the iteratively refined project, we made a number of changes in staffing, introduced a more focused patient selection scheme, and implemented an appropriate support and feedback system, whereby nurses were able to learn from their own and each other’s experiences. As the intervention process was refined and appropriate training was provided to nurses in the second half of 2012, the results gradually improved.
There are a number of limitations to this study. Of note, one limitation of the ZD design is the effect of nonparticipation, where those patients randomized to the intervention arm but refusing it are analyzed as part of the intervention group. As almost 50% of those randomized to the intervention chose not to participate, statistical power suffered markedly. In addition, approximately two-thirds of all patients with three or more Emergency Department visits were excluded on the basis of the predetermined criteria. Although this led to a sizable decrease in the number of available patients, and would limit the yield of an intervention such as this one in clinical practice, we believe that it was necessary to ensure that the intervention was not offered to patients who fulfilled the exclusion criteria agreed upon in the study. Also, because much of the patient selection relied on a qualitative assessment, it proved difficult to reliably identify patients with a high sustained healthcare consumption. Gradually, this led to concentration of the task of screening patients for inclusion to fewer nurses, but even so, we believe that it may be possible to improve further by using more quantitative methods such as prediction models. In its current format, the final stage of patient selection still involves a qualitative assessment and may therefore be difficult to apply directly in other settings without a certain degree of adaptation.
Previous studies involving nurse-led case management interventions to reduce healthcare consumption for frequent Emergency Department visitors have been mixed and relatively few compared with specific disease types such as heart failure 6. As the largest published intervention to date, our study lends further weight toward the possible success of such interventions, but the variable results also found within our study indicate the difficulty in achieving these results. Furthermore, our results are comparable with those of other successful interventions 7–9,11. Of the 11 studies noted in a review by Kumar and Klein 11, eight studies showed significant decreases in Emergency Department visits of up to 40%. In the largest study, which included 252 patients, the authors also noted a decrease in inpatient admissions, but no change in the number of days in hospital, outpatient care, or costs.
Conclusion
Our study provides evidence that a telephone-based intervention with accurate patient selection, appropriate staff training, and centralized intervention delivery can be implemented successfully on a large scale and lead to significant decreases in healthcare consumption. However, given the large variety of results noted both within our study and in different types of case management interventions, further research is clearly warranted to better identify success factors affecting risk for the accurate selection of patients for inclusion and for optimization of the delivery and management of the intervention.
Supplementary Material
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website (www.euro-emergencymed.com).
Acknowledgements
The authors would like to note the outstanding efforts of the nurses and other medical/nonmedical staff involved in the provision and development of this intervention who made this study possible. The study was jointly financed by the five participating county councils. The funding sources played no direct role in the planning, conduct, or analysis of the study.
Authorship statement: G.Ö., J.W., and G.E. conceived the study, designed the trial, and obtained funding from each county council; G.Ö., A.D., J.T., S.N., T.S., and B.C.F. supervised the conduct of the trial and data collection in their respective county; G.Ö., A.D., J.T., S.N., T.S., and B.C.F. undertook recruitment of participating centers and patients and managed the data, including quality control; G.E. and J.A. provided statistical advice on study design and analyzed the data; G.Ö. chaired the data oversight committee; G.E. and J.A. drafted the manuscript, and all authors contributed substantially to its revision and G.E. takes responsibility for the paper as a whole.
Conflicts of interest
Dr Gustaf Edgren has received consulting fees from Health Navigator AB for providing assistance with study design and research methodology. Joachim Werr is co-owner and managing director of Health Navigator AB. Jacqueline Anderson is an analyst with Health Navigator. Authors Anders Dolk, Jarl Torgerson, Svante Nyberg, Tommy Skau, Birger C Forsberg, and Gunnar Öhlen are county council representatives and therefore members of the funding bodies for this study.
References
- 1.Cook LJ, Knight S, Junkins EP, Jr, Mann NC, Dean JM, Olson LM. Repeat patients to the emergency department in a statewide database. Acad Emerg Med 2004; 11:256–263. [DOI] [PubMed] [Google Scholar]
- 2.Hansagi H, Olsson M, Sjöberg S, Tomson Y, Göransson S. Frequent use of the hospital emergency department is indicative of high use of other health care services. Ann Emerg Med 2001; 37:561–567. [DOI] [PubMed] [Google Scholar]
- 3.Hunt KA, Weber EJ, Showstack JA, Colby DC, Callaham ML. Characteristics of frequent users of emergency departments. Ann Emerg Med 2006; 48:1–8. [DOI] [PubMed] [Google Scholar]
- 4.LaCalle E, Rabin E. Frequent users of emergency departments: the myths, the data, and the policy implications. Ann Emerg Med 2010; 56:42–48. [DOI] [PubMed] [Google Scholar]
- 5.Marco CA, Moskop JC, Schears RM, Stankus JL, Bookman KJ, Padela AI, et al. The ethics of health care reform: impact on emergency medicine. Acad Emerg Med 2012; 19:461–468. [DOI] [PubMed] [Google Scholar]
- 6.Althaus F, Paroz S, Hugli O, Ghali WA, Daeppen JB, Peytremann-Bridevaux I, Bodenmann P. Effectiveness of interventions targeting frequent users of emergency departments: a systematic review. Ann Emerg Med 2011; 58:41–52.e42. [DOI] [PubMed] [Google Scholar]
- 7.Okin RL, Boccellari A, Azocar F, Shumway M, O’Brien K, Gelb A, et al. The effects of clinical case management on hospital service use among ED frequent users. Am J Emerg Med 2000; 18:603–608. [DOI] [PubMed] [Google Scholar]
- 8.Shumway M, Boccellari A, O’Brien K, Okin RL. Cost-effectiveness of clinical case management for ED frequent users: results of a randomized trial. Am J Emerg Med 2008; 26:155–164. [DOI] [PubMed] [Google Scholar]
- 9.Skinner J, Carter L, Haxton C. Case management of patients who frequently present to a Scottish emergency department. Emerg Med J 2009; 26:103–105. [DOI] [PubMed] [Google Scholar]
- 10.Wennberg DE, Marr A, Lang L, O’Malley S, Bennett G. A randomized trial of a telephone care-management strategy. N Engl J Med 2010; 363:1245–1255. [DOI] [PubMed] [Google Scholar]
- 11.Kumar GS, Klein R. Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: a systematic review. J Emerg Med 2013; 44:717–729. [DOI] [PubMed] [Google Scholar]
- 12.Motheral BR. Telephone-based disease management: why it does not save money. Am J Manag Care 2011; 17:e10–e16. [PubMed] [Google Scholar]
- 13.Steventon A, Tunkel S, Blunt I, Bardsley M. Effect of telephone health coaching (Birmingham OwnHealth) on hospital use and associated costs. BMJ 2013; 4585:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reinius P, Johansson M, Fjellner A, Werr J, Ohlrl G, Edgren G. A telephone-based case-management intervention reduces healthcare utilization for frequent emergency department visitors. Eur J Emerg Med 2013; 20:327–334. [DOI] [PubMed] [Google Scholar]
- 15.Zelen M. A new design for randomized clinical trials. N Engl J Med 1979; 300:1242–1245. [DOI] [PubMed] [Google Scholar]
- 16.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. European journal of epidemiology 2009; 24:659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website (www.euro-emergencymed.com).


