ABSTRACT
Purpose
Pupil size is critical for optimal performance of presbyopic contact lenses. Although the effect of luminance is well known, little information is available regarding other contributing factors such as aging and refractive status.
Methods
The cohort population comprised 304 patients (127 male, 177 female) aged 18 to 78 years. Pupils were photographed at three controlled luminance levels 250, 50, and 2.5 cd/m2 using an infra-red macro video camera. Measurements of pupil diameter were conducted after transforming pixel values to linear values in millimeters.
Results
Luminance was the most influential factor with pupil diameter increasing with decreased luminance (p < 0.001, all comparisons). Age was also found to be a significant factor with a smaller diameter in the older groups, but overall the difference was only significant between the pre-presbyopes and the established presbyopes (p = 0.017). Pupil diameter decreased significantly with increasing age, the effect being most marked at low luminance (<0.001). The smallest pupil diameters were measured for hyperopes and the largest for myopes and although refractive error was not a significant factor alone, there was a significant interaction between luminance and refractive error with the greatest differences in pupil diameter between myopes and emmetropes at low luminance (p < 0.001). Pupil diameter changes modeled by multilinear regression (p < 0.001) identified age, luminance, best sphere refraction, and refractive error as significant factors accounting for just over 70% of the average variation in pupil diameter.
Conclusions
Both age and refractive status were found to affect pupil size with larger pupils measured for younger patients and myopes. Designs for multifocal contact lens corrections should take both age and refractive status into consideration; a faster progression from distance to near corrections across the optical zone of the lens is expected to be required for established presbyopes and hyperopes than it is for early presbyopes, myopes, and emmetropes.
Key Words: pupil, size, diameter, multifocal, contact lens, refractive error, luminance, age, presbyopia
The efficacy of presbyopia correction with multifocal contact lenses is contingent on the optimization of optical designs to meet the specific refractive needs of the patients wearing the lenses. Pupil size is a key factor to consider in the development of optical designs, particularly for contact lenses to be worn by a presbyopic population, and a number of studies have been conducted to investigate the factors that may influence pupil size.
It is well established that pupil size decreases with increasing luminance.1–4 The strongest patient-related determinative factor for pupil size has been shown to be age.5–9 In an early study conducted by Birren et al., a nonlinear decrease in pupil size with age was reported5; however, this study did not control for variations in illumination level. In a later study, Winn et al. measured pupil size under several different conditions of luminance in a group of 91 subjects between 17 and 83 years of age6; for each luminance level, the pupil size was found to decrease linearly with age. Subsequently, a number of large studies have confirmed the inverse correlation between age and preoperative pupil size in this refractive surgery candidates under several luminance levels.7–9
Other factors that have been investigated for their possible relationship with pupil size are gender, iris color, and refractive error. The evidence in the literature is consistent in its reports that there are no significant differences in pupil size between males and females or any correlation with iris color6–10; however, the evidence relating to the influence of refractive status is equivocal. Hirsch and Weymouth conducted the first study investigating the relationship between refractive state and pupil size in 1949, and reported smaller pupils in hyperopes than myopes among the population of 266 male university students examined.11 It was not until 1990 that a further study to investigate the role of refractive status on pupil size was conducted,10 and in this study no difference in pupil size was found between the low myopes and emmetropes investigated; however, the study only involved 48 young subjects ranging in age from 18 to 26. Winn et al. also evaluated the role of refractive status in their study of pupil size in normal human subjects6 and reported no significant relationship between refractive error and pupil size in their study population of myopes, emmetropes, and hyperopes; however, the groups were not matched for age with the hyperopes being on average 10 years older than the myopes and emmetropes, and the difference in age may therefore have been a confounding factor. More recently, the role of refractive status on pupil size has been investigated in several refractive surgery studies. Although no relationship was found in one study with a relatively small sample size,7 two larger studies of refractive surgery candidates reported that the preoperative refractive status was found to be a determinative factor in pupil size when measured under mesopic conditions, with smaller pupil sizes reported for hyperopes than myopes.8,9
Pupil size is also an important design consideration for simultaneous image multifocal or bifocal contact lenses because for these lenses to be successfully fitted and worn, optimal visual performance must be achieved at all viewing distances under varying luminance conditions.12–15 To date, no large studies have been conducted in which pupil size has been measured in hyperopes, emmetropes, and myopes of varying ages under different illumination conditions. Therefore, the objective of this analysis was to determine the influence of refractive status and age on pupil size under three commonly encountered luminance levels and to make recommendations regarding multifocal contact lens design optical characteristics for specific population groups.
MATERIALS AND METHODS
Study Design
This study was a non-interventional, retrospective analysis of a database collected by OCULAR TECHNOLOGY GROUP—International (operating at the time as OTG Research & Consultancy) that was transferred to Johnson & Johnson Vision Care Inc. The data were collected when patients attended the OCULAR TECHNOLOGY GROUP—International research clinic for routine screening visits before enrollment into its database of prospective study participants. The tenets of the Declaration of Helsinki 1975 were adhered to. Ethics approval was obtained and all subjects provided informed consent before data collection; appropriate measures were taken to ensure subject anonymity and the subjects were advised that the results of the findings of the investigation may be used for medical and scientific publications. The subjects had normal eyes, other than the need for vision correction.
The population comprised 304 subjects (127 male, 177 female) with a mean age of 39.5 ± 14.2 years (range 18–78 years), a mean spherical equivalent refractive error of −2.11 ± 2.46D (range −8.10 to +5.00D), and a mean astigmatic error of −0.48 ± 0.46D (range 0.00 to −3.00D). The mean flat central corneal radius was 7.78 ± 0.26 mm (range 7.05–8.80 mm) and central corneal astigmatism 0.15 ± 0.09D (range 0.01–0.50D).
Measurement Procedures
Refraction
The starting point for the subjective refraction was the objective refraction obtained with the Nidek AF9000 autorefractor. The refraction was refined subjectively using the cross-cylinder method under monocular blurring conditions and balanced binocularly by the Humphriss technique.16
Pupil Measurements
Pupils were photographed using an infra-red macro video camera in conjunction with a head-mounted eye tracker (Applied Science Laboratory) and the measurements were carried out post hoc after calibration of the system to transform pixel values to linear values in millimeters. The macro system was positioned in front of the eye being photographed but did not obscure the fellow eye. To control the accommodation and convergence that could affect pupil measurements, the subjects wore their spectacle correction in front of the eye not being photographed while fixating straight ahead at a distance target. Three diffuse light settings were set to produce 250 cd/m2 (high luminance), 50 cd/m2 (medium luminance), and 2.5 cd/m2 (low luminance), respectively, on the subject’s face and an interval of approximately 5 minutes elapsed between measurements at each of the luminance levels. Luminance measurements were conducted in a room that allowed full control of the lighting settings using a series of spot lights with diffusers (similar to those used in photographic studios) for both the printed visual acuity chart target and the subject’s face. The luminance levels were selected to represent outdoor daylight, indoor evening lighting, and night time driving. The images were coded to allow randomization and the measurements were made by a masked investigator. The horizontal pupil diameter was taken as the measurement endpoint using Sigma Scan software.
Statistical Methods
The Mixed Linear Model and Regression Analysis were carried out with SPSS 22.0 (IBM UK Ltd). Chi-squared (χ2) Automated Interaction Detection (CHAID) analysis was carried out with Tree Analysis. Before the analysis, the continuous variables were checked for normality because this is an assumption for the Regression and the Mixed Model. Based on Kolmogorov-Smirnov and Shapiro-Wilk tests, and taking into consideration the histograms and the values of skewness and kurtosis, it was found that no transformations were needed.
The Mixed Linear Model (MLM) for the pupil used age (pre-presbyopes: 18–39 years; early presbyopes: 40–54 years; established presbyopes: 55 years or older), refractive error group (best sphere: myopes: ≤−0.50D; emmetropes: ≥−0.25 to ≤+0.50D; hyperopes ≥+0.75D), and luminance (high: 250 cd/m2; medium: 50 cd/m2; low: 2.5 cd/m2) as fixed factors. Because data were collected from both eyes, eye was used as a repeated factor to be able to use all the data collected and not inflate the sample size. Factorial analysis was used to determine the significance of all main effects and their interactions. The covariance structure of the repeated effect was selected as a compound symmetry model because this was determined by the MLM analysis information criteria to be the best fitting model. In addition, the Bonferroni adjustment was used for the post hoc multiple comparisons.
CHAID analysis is based upon selecting the factors in their order of significance, based on the level of χ2 significance. The process is repeated for each subgroup identified until none of the χ2 factors remaining are significant. This statistical approach has great clinical value because it does not force a universal model for the entire population (e.g. it is possible that the significant interacting factors may be different for different luminance levels). A further advantage of CHAID analysis is that it can incorporate fixed and continuous factors (e.g. age), and for these factors CHAID does not require definition of the subgroup in advance but automatically divides the population based upon the grouping that achieves the greatest differentiation.
RESULTS
Mixed Linear Model Comparative Analysis
The mean pupil diameter according to age and refractive error group (mean of all three luminance levels) are presented in Table 1 and according to luminance level, age, and refractive error in Table 2. The pupil Mixed Linear Model (MLM) comparative analysis results revealed that luminance (p < 0.001) and age (p = 0.001) were significant factors but not refractive error group (p = 0.117). Luminance was the most significant factor, with pupil diameter increasing with decreased luminance. The differences recorded were both statistically (p < 0.001) and highly clinically significant between each luminance level. Although age was significant overall, only the individual comparison between pre-presbyopes and established presbyopes was significant (p < 0.001). The differences between the pre-presbyopes and the early presbyopes and between the early presbyopes and the established presbyopes were of lower amplitudes and were not statistically significant (p = 0.086 and p = 0.309, respectively).
TABLE 1.
Pupil diameter by demographics (age and refractive error groups): mean of all luminance levels tested
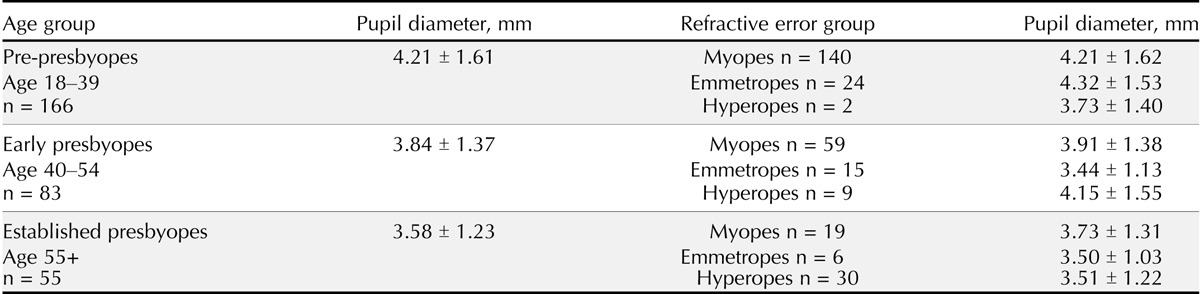
TABLE 2.
Pupil diameter by luminance, age group, and refractive error group
The two-way interactions of luminance by age (p < 0.001), luminance by refractive error group (p < 0.001), and the three-way interaction of luminance by age and by refractive error group (p < 0.001) were significant. These interactions clearly indicate that, in addition to being considered individually, the effects of the various factors need to be considered for different environmental situations.
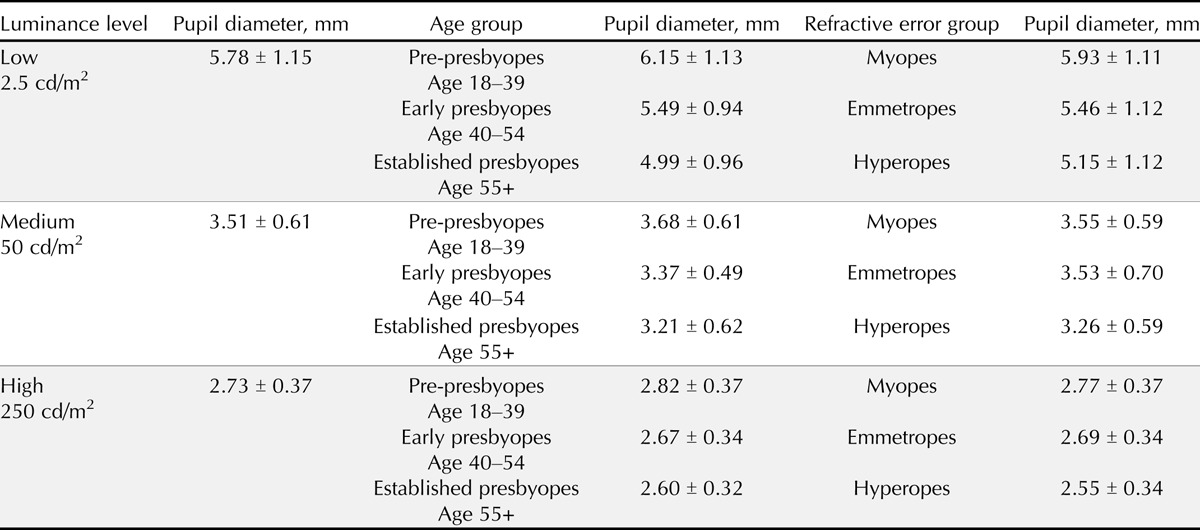
The interaction between luminance and age revealed that the magnitude of the differences recorded between the age groups decreased as the luminance increased (Fig. 1). At low luminance, the individual comparisons between pre-presbyopes and both early and established presbyopes were significant (p < 0.001–0.006) along with the difference between early and established presbyopes (p = 0.004). In contrast, at medium luminance, only the difference between pre-presbyopes and established presbyopes was significant (p = 0.017); although the same trend towards a decrease in pupil diameter with age was apparent, the changes were not significant between both pre-presbyopes and early presbyopes (p = 0.156) and early and established presbyopes (p = 1.000). At high luminance, the mean pupil diameters were not different between any of the age groups (p = 0.864–1.000).
FIGURE 1.
Pupil diameter in mm as a function of luminance for each age group evaluated.
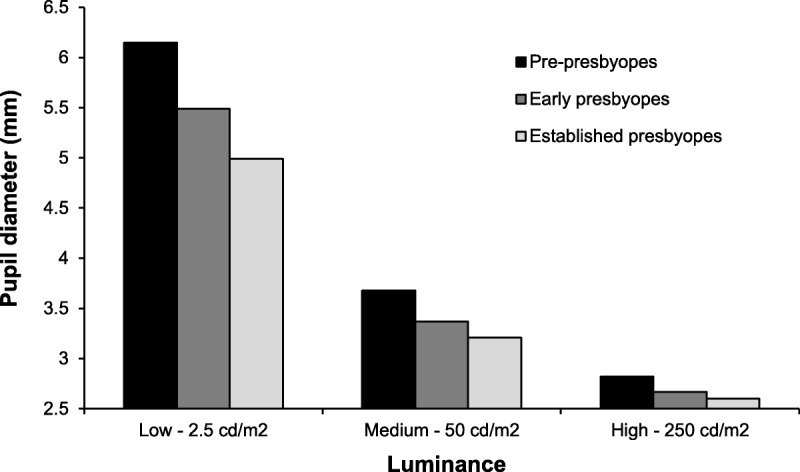
The interaction between luminance and refractive error group was less pronounced when comparing the pupil diameter of the three refractive error groups at each luminance (Fig. 2). The greatest difference was present at low luminance, where the individual comparisons between myopes and emmetropes was significant (p < 0.001) but not the differences between myopes and hyperopes or between emmetropes and hyperopes (p = 0.107 and p = 1.000, respectively). At medium and high luminance, the mean pupil diameters were not different between myopes, emmetropes, and hyperopes (p = 0.933–1.000 and p = 0.531–1.000, respectively).
FIGURE 2.
Pupil diameter (mm) as a function of luminance for each refractive error group evaluated.
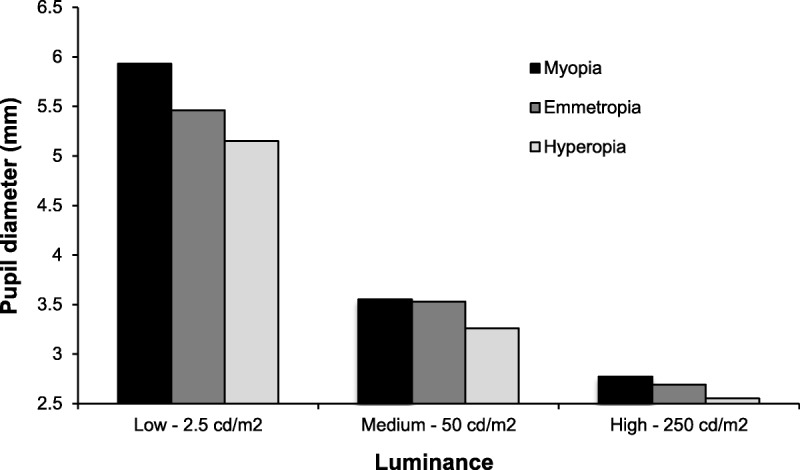
The three-way interaction between luminance, age, and refractive error group (Fig. 3) revealed a number of differences in pupil diameter between the three age groups with a trend toward the greatest differences being present at low luminance and among myopes. At low luminance, for myopes, the mean pupil diameter was significantly larger for pre-presbyopes than early presbyopes (p < 0.001) and established presbyopes (p < 0.001); further, the mean pupil diameter of early presbyopes was significantly larger than the mean pupil diameter of established presbyopes (p = 0.041). At low luminance, for emmetropes, once again the mean pupil diameter was significantly larger for pre-presbyopes (mean = 6.09 mm) than early presbyopes (p < 0.001) and established presbyopes (p < 0.001). At low luminance, for hyperopes, the only significant difference recorded was between early and established presbyopes, the latter having significantly (p < 0.001) larger pupil diameters. In Fig. 3A, it can be seen that the pre-presbyopic hyperopes had smaller pupil diameters than the early presbyopic hyperopes at low luminance; however, there were only two subjects in this pre-presbyopic group and nine in the early presbyopic group, and the difference was not statistically significant (p = 1.000). At medium luminance, for myopes, the mean pupil diameter of pre-presbyopes was significantly larger than the mean pupil diameter of early presbyopes (p = 0.048), and for emmetropes, the mean pupil diameter of pre-presbyopes was significantly larger than the mean pupil diameter of both early (p = 0.001) and established (p = 0.004) presbyopes. No differences were recorded among hyperopes. At high luminance, no significant differences were recorded.
FIGURE 3.
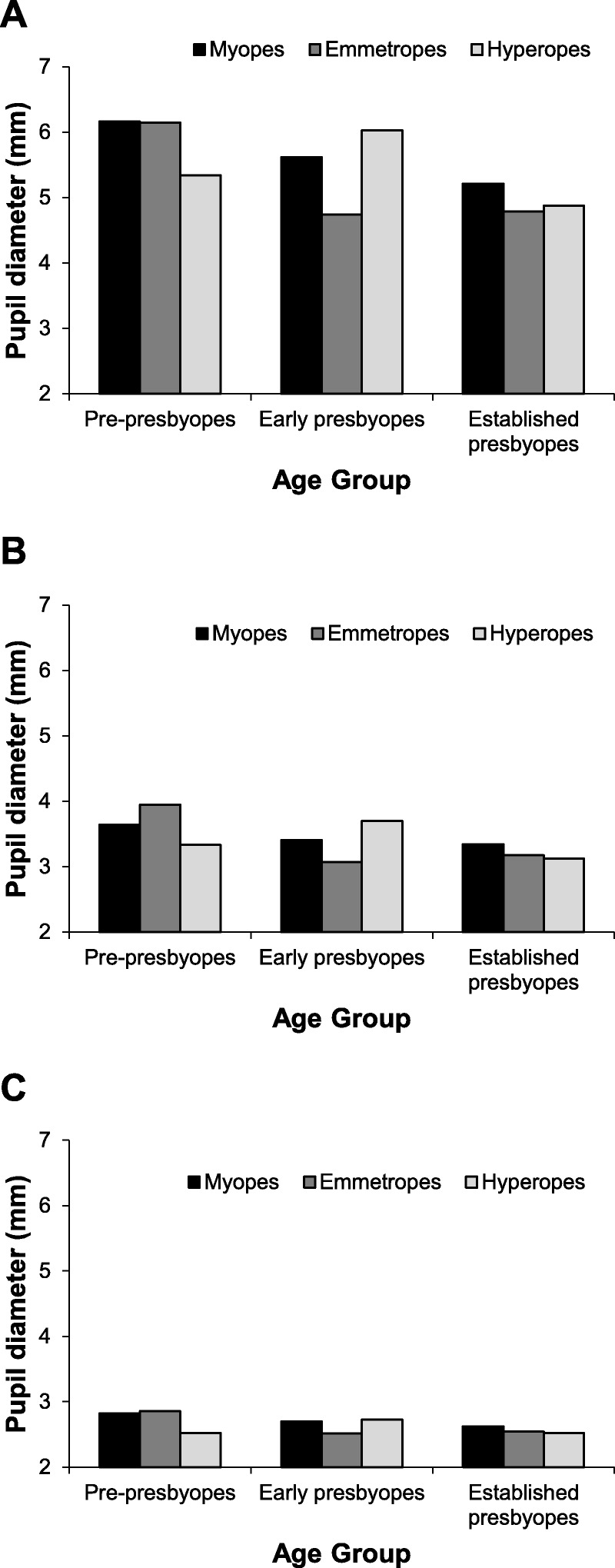
Pupil diameter (mm) as a function of age for each refractive error group at the three luminance levels evaluated: (A) low, 2.5 cd/m2; (B) medium, 50 cd/m2; (C) high, 250 cd/m2.
Multilinear Regression Analysis
To understand the influence of luminance, age, and refractive error and to ascertain the role of these parameters in predicting the characteristics of the population of interest, a multilinear regression (MLR) analysis was carried out. The stepwise MLR analysis revealed that all three factors had a significant influence and produced the following regression formula:
Pupil diameter (mm) = 7.748 − 1.514 Lighting Condition* − 0.020 Age (years) − 0.024 Best Sphere (D).
*Categorical values of 1 = 2.5 cd/mm2/2 = 50 cd.m2/3 = 250 cd/m2.
This regression predicted closed to three quarters of the variation in pupil diameter (r2 = 0.718).
CHAID Analysis
The CHAID analysis is summarized in Fig. 4. As expected, luminance was identified as the most influential factor (p < 0 .001), followed by age; however, the effect of age was variable depending upon the luminance condition which led to the identification of a different partitioning model for the various luminance levels.
FIGURE 4.
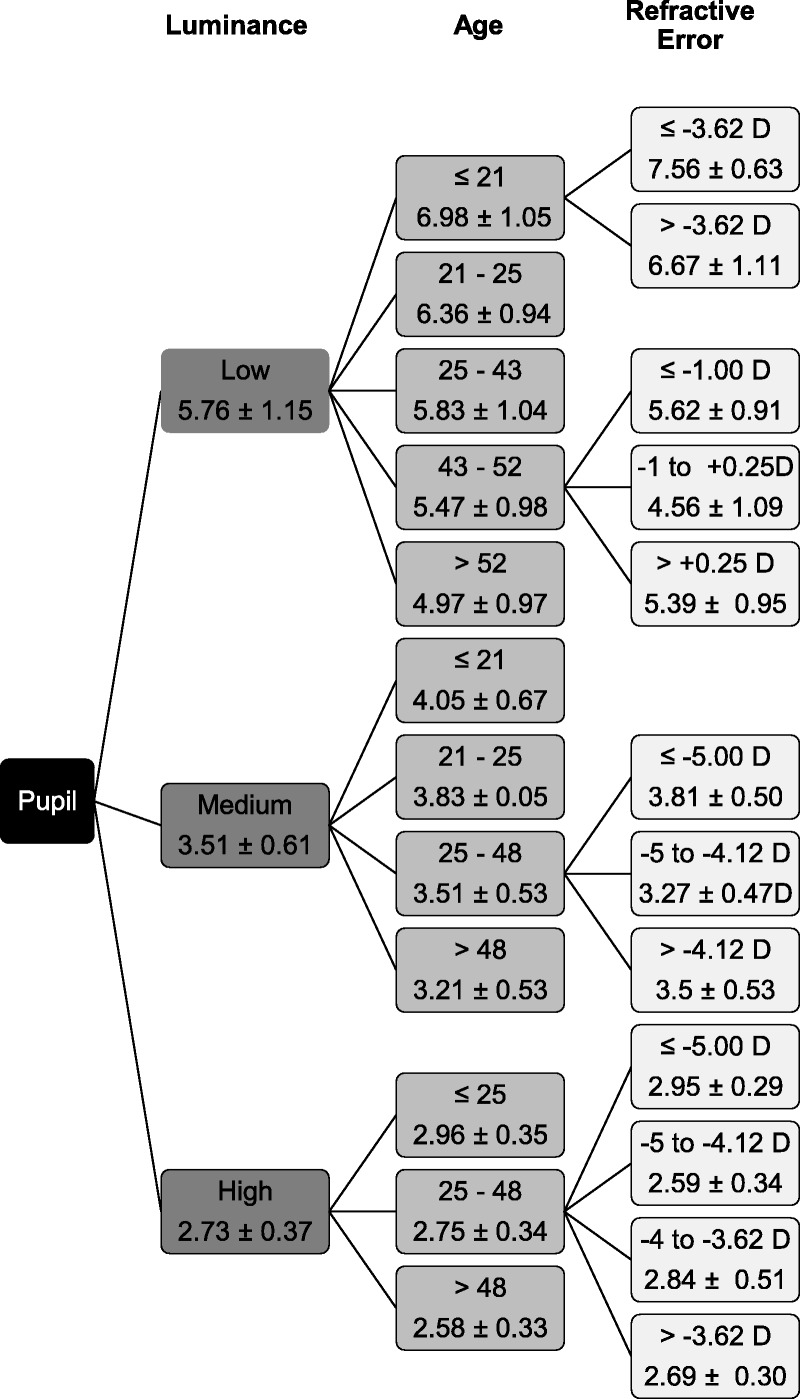
Pupil diameter (mm) CHAID analysis: factors selected in order, based on level of χ2 significance (all p ≤ 0.05). Selection individually re-tested for each subgroup identified producing group-specific models. Population division based upon factors achieving greatest differentiation: 1st level Luminance − 2nd level Age − 3rd level Refractive Error.
At low luminance (overall mean = 5.76 mm), five distinct groups of increasing age and decreasing mean pupil diameter were identified: (1) ≤21 years = 6.98 mm; (2) 21 to 25 years = 6.36 mm; (3) 25 to 43 years = 5.83 mm; (4) 43 to 52 years = 5.47 mm; (5) ≥52 years = 4.97 mm (p < 0.001). These data demonstrate that the decrease in pupil diameter is most marked in young adulthood, but still continues during presbyopia. Refractive error group was a further differentiating factor, but only within the youngest CHAID age group (≤21 years) and the CHAID early presbyopic population (43–52 years) (p = 0.017 and p = 0.048, respectively). In the youngest group, the higher myopes (>−3.63D) had larger pupil diameters than the low myopes (≤−3.63D), emmetropes, and hyperopes, and in the early presbyopic group, myopes (≤1.00D) and hyperopes (≥0.25D) had larger pupil diameters than emmetropes and near emmetropes (≤1.00 to +0.25D).
At medium luminance (overall mean = 3.51 mm), only four distinct groups of increasing age and decreasing mean pupil diameter were identified: (1) ≤21 years = 4.05 mm; (2) 21 to 25 years = 3.83 mm; (3) 25 to 48 years = 3.51 mm; (4) ≥48 years = 3.81 mm (p < 0.001). The data demonstrate that at medium luminance, the decrease in pupil diameter is minimal after the age of 48 years. Refractive error group was a further differentiating factor, but only in the pre-presbyopic/early presbyopic population (25–48 years, p = 0.001). The further breakdowns for the refractive groups in this age group are shown in Fig. 4.
At high luminance (overall mean = 2.73 mm), only three distinct groups of increasing age and decreasing mean pupil diameter were identified: (1) ≤25 years = 2.96 mm; (2) 25 to 48 years = 2.72 mm; (3) ≥48 years = 2.58 mm (p < 0.001). These data demonstrate that at high luminance, the decrease in pupil diameter is minimal after the age of 48 years. Refractive error group was a further differentiating factor, but only in the pre-presbyopic/early presbyopic population (25–48 years, p < 0.001). The further breakdowns for the refractive groups in this age group are shown in Fig. 4.
DISCUSSION
As expected, luminance was the most influential factor dictating pupil diameter, the mean night time driving pupil diameter at 2.5 cd/m2 (mean = 5.76 mm) being over twice the mean outdoor daylight pupil diameter at 250 cd/m2 (mean = 2.73 mm) and over one and half times the indoor evening lighting pupil diameter at 50 cd/m2 (mean = 3.51 mm). Predictably, age was also found to be a factor affecting pupil diameter with a smaller diameter in the older groups, but overall the difference was only significant between the pre-presbyopes and the established presbyopes. Of greater interest were the significant two- and three-way interactions between the environmental factor (luminance) and the subject biometrics (age and refractive error) which produced more specific categorical differences. When considering both age and refractive error individually, the common observations were that the largest differences in pupil diameter between age groups and between refractive conditions were recorded at low luminance and that when luminance was increased, the differences decreased in magnitude; however, there was an absence of differences between age groups and refractive conditions at high luminance.
A unique feature of our study was that the effects of the factors luminance, age, and refractive error, which were identified in the MLM analysis, were also identified in the less widely used CHAID analysis. The main differences between these two types of analyses are that, although the MLM analysis requires the subgroup thresholds to be set as part of the original design and force a single statistical model to explain variations for the whole study population, CHAID automatically identifies the threshold for the subgroups based upon the greatest statistical probability and also allows for different models for the various subgroups to be identified. In this study, the CHAID analysis showed that at low luminance, three groups were identified in which presbyopes were represented, with ages 43 and 52 years as the cutoff points between the three groups, whereas at medium and high luminance, only two groups were identified in which presbyopes were represented, with a younger cutoff point between the groups of 48 years. This analysis also showed differentiation between refractive groups which was most evident at low luminance but was also present at medium and high luminance, however with a lesser degree of differentiation.
The results from our study are in agreement with two earlier studies conducted on preoperative refractive surgery candidates.8,9 Cakmak et al. and Linke et al. reported significant differences in pupil size according to both age (smaller pupils with increasing age) and refractive error (smaller pupils in hyperopes than myopes); however, in their studies, measurements were only conducted under mesopic conditions, whereas our study was conducted at three luminance levels representing those commonly encountered during day-to-day activities. Contrary to these findings, Winn et al. and more recently Orr et al. failed to detect a refraction associated difference, and a possible reason for this may have been the relatively small sample sizes in each of these studies (91 and 60 subjects, respectively) and therefore insufficient power to detect differences.6,17 A further limitation of the study by Orr et al. is that all the measurements were made at photopic luminance levels, with five out of the six luminance levels used falling in the high photopic range that corresponds to outdoor luminance during the day,17 whereas we have confirmed that the lighting environments associated with the largest variations between individuals are encountered at mesopic level (<3 cd/m2) corresponding to visual tasks such as night driving.
One aspect that was not considered in the current study was the effect of accommodation as the measurements were taken while the subjects were fixating a distance target. Although it is known that accommodation plays a significant role in controlling pupil size,4 the influence of accommodation on pupil size in presbyopes is expected to be relatively small and is irrelevant when comparing the effect of luminance for the conditions of daytime outdoor vision and night time driving.
Simultaneous image multifocal or bifocal contact lenses are all pupil dependent, and as discussed earlier, the challenge with these designs is to achieve a balanced visual performance between distance and near vision under varying luminance conditions.12–15 The implications of the current study findings for multifocal contact lens designs are that they need to take into consideration the effects of aging and refractive error on the diameter of the pupil. A design with only one rate of progression from distance to near does not suffice; further, the effect of refractive error should also be considered. Typically, multifocal contact lenses are supplied in three near additions; hence, designs for advanced presbyopes not only require the incorporation of a higher addition than designs for early presbyopes but also the progression in power from the distance to the near correction regions must be faster, over a narrower diameter. Because the variation in pupil diameter is most marked at low luminance, the influence of the pupil is critical for medium and low luminance performance, and therefore the parameter that requires the most alteration to cope with the effect of pupil changes is the design within the mid- and peripheral optic zone regions. Because pupil size also changes with refractive error, to maintain constant visual performance for fixed luminance levels, the rate of progression in the optical designs must vary with refractive error.
Extensive modeling of factors influencing pupil size has been conducted by Watson and Yellott who derived a unified formula for light adapted pupil diameter including the effects of luminance, adapting field size, age of the observer, and whether one or both eyes were used.18 The authors did, however, provide a caveat that pupil size was subject to many influences and large individual differences are found. Our regression analysis demonstrated that luminance, age, and refraction accounted for just over 70% of the average variation in pupil diameter; however, the confidence interval of the regression and the pupil diameter distribution within both individual age and refractive groups point to large individual differences. This clearly indicates the potential benefits of customizing multifocal lens designs to achieve greater clinical acceptance by the use of an individualized visual performance optimization. The industry has previously demonstrated that lens customization was technically possible and suggested that this could be offered to wearers with high degrees of higher order aberrations, including distorted corneas. We contend that the presbyopic population represents a much greater potential contact lens wearing group, who are not currently fully satisfied with the limited designs available and who would benefit from a customized contact lens.
Although extremely precise, masked, and randomized measurements of pupil diameter under three different luminance conditions were made for this analysis, it must be recognized that this was a retrospective analysis, and therefore the distribution of subjects across age groups and refractive errors was not equal; however, the results clearly demonstrate that both age and refractive status affect pupil diameter with larger pupils measured for younger patients and myopes, with the most marked differences being measured at low luminance levels. By making adjustments to the optical design of multifocal contact lenses to account for changes in pupil diameter due to age and refractive status, optimal visual performance may be achieved under everyday luminance conditions.
CONCLUSION
As expected, the factor that was found to be most influential in dictating pupil diameter was luminance, and the largest pupils were measured under luminance levels that were representative of night driving conditions. Larger pupils were also measured for myopes and for younger individuals, and these differences were most pronounced at the lower luminance levels. Multifocal contact lenses are routinely fitted to myopes, emmetropes, and hyperopes and are required to provide good visual performance under a variety of luminance conditions. Because pupil size plays such a significant role in visual performance, the results of this study support the need for variations in the optical design of multifocal contact lenses according to patient’s age (and therefore requirement for near power addition) and refractive status. A faster progression from distance to near corrections across the optical zone of the lens is expected to be required for established presbyopes and hyperopes than it is for early presbyopes, myopes, and emmetropes.
Michel Guillon
OCULAR TECHNOLOGY GROUP—International
66 Buckingham Gate
London SW1E 6AU
United Kingdom
e-mail: mguillon@otg.co.uk
ACKNOWLEDGMENTS
This work was supported by Johnson & Johnson Vision Care Inc. CBW and KM are employees of Johnson & Johnson Vision Care Inc. The results from these analyses were presented at the Association for Research in Vision and Ophthalmology meeting in Denver in May 2015.
REFERENCES
- 1.De Groot SG, Gebhard JW. Pupil size as determined by adapting luminance. J Opt Soc Am (A) 1952;42:492–5. [DOI] [PubMed] [Google Scholar]
- 2.Wyatt HJ, Musselman JF. Pupillary light reflex in humans: evidence for an unbalanced pathway from nasal retina, and for signal cancellation in brainstem. Vision Res 1981;21:513–25. [DOI] [PubMed] [Google Scholar]
- 3.Ellis CJ. The pupillary light reflex in normal subjects. Br J Ophthalmol 1981;65:754–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mathur A, Gehrmann J, Atchison DA. Influences of luminance and accommodation stimuli on pupil size and pupil center location. Invest Ophthalmol Vis Sci 2014;55:2166–72. [DOI] [PubMed] [Google Scholar]
- 5.Birren JE, Casperson RC, Botwinick J. Age changes in pupil size. J Gerontol 1950;5:216–21. [DOI] [PubMed] [Google Scholar]
- 6.Winn B, Whitaker D, Elliott DB, Phillips NJ. Factors affecting light-adapted pupil size in normal human subjects. Invest Ophthalmol Vis Sci 1994;35:1132–7. [PubMed] [Google Scholar]
- 7.Netto MV, Ambrosio R, Jr., Wilson SE. Pupil size in refractive surgery candidates. J Refract Surg 2004;20:337–42. [DOI] [PubMed] [Google Scholar]
- 8.Cakmak HB, Cagil N, Simavli H, Duzen B, Simsek S. Refractive error may influence mesopic pupil size. Curr Eye Res 2010;35:130–6. [DOI] [PubMed] [Google Scholar]
- 9.Linke SJ, Baviera J, Munzer G, Fricke OH, Richard G, Katz T. Mesopic pupil size in a refractive surgery population (13,959 eyes). Optom Vis Sci 2012;89:1156–64. [DOI] [PubMed] [Google Scholar]
- 10.Jones R. Do women and myopes have larger pupils? Invest Ophthalmol Vis Sci 1990;31:1413–5. [PubMed] [Google Scholar]
- 11.Hirsch MJ, Weymouth FW. Pupil size in ametropia. J Appl Physiol 1949;1:646–8. [DOI] [PubMed] [Google Scholar]
- 12.Chateau N, De Brabander J, Bouchard F, Molenaar H. Infrared pupillometry in presbyopes fitted with soft contact lenses. Optom Vis Sci 1996;73:733–41. [DOI] [PubMed] [Google Scholar]
- 13.Bradley A, Nam J, Xu R, Harman L, Thibos L. Impact of contact lens zone geometry and ocular optics on bifocal retinal image quality. Ophthalmic Physiol Opt 2014;34:331–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chateau N, Baude D. Simulated in situ optical performance of bifocal contact lenses. Optom Vis Sci 1997;74:532–9. [DOI] [PubMed] [Google Scholar]
- 15.Guillon M, Maissa C, Cooper P, Girard-Claudon K, Poling TR. Visual performance of a multi-zone bifocal and a progressive multifocal contact lens. CLAO J 2002;28:88–93. [PubMed] [Google Scholar]
- 16.Humphriss D. Binocular refraction. In: Edwards K, Llewellyn R, ed. Optometry. London: Butterworths; 1988;140–9. [Google Scholar]
- 17.Orr JB, Seidel D, Day M, Gray LS. Is pupil diameter influenced by refractive error? Optom Vis Sci 2015;92:834–40. [DOI] [PubMed] [Google Scholar]
- 18.Watson AB, Yellott JI. A unified formula for light-adapted pupil size. J Vis 2012;12.1–12. [DOI] [PubMed] [Google Scholar]


