Abstract
Objectives:
Health research indicates that physician trust in the United States has declined over the last 50 years. Paralleling this trend is a decline in social capital, with researchers finding a negative relationship between immigration-based diversity and social capital. This article examines whether physician distrust is also tied to immigration-based diversity and declining social capital.
Methods:
Data come from the 2012 General Social Survey, one of the gold standards of US public opinion surveys, using a national probability sample of 1080 adult US respondents. Key measures included support for reducing levels of immigration to the United States and multiple measures of physician trust.
Results:
The results of ordinary least squares regressions, using survey weights, indicate that support for reducing immigration is positively linked to physician distrust, bringing physician distrust into the orbit of research on diversity and declining social capital. Models controlled for age, education, income, gender, race, nativity, conservatism, unemployed status, lack of health insurance, and self-rated health. Furthermore, analyses of a subset of respondents reveal that measures of general trust and some forms of institutional trust do not explain away the association between support for immigration reduction and physician distrust, though confidence in science as an institution appears relevant.
Conclusion:
Consistent with diversity and social capital research, this article finds that an immigration attitude predicts physician distrust. Physician distrust may not be linked just to physician–patient interactions, the structure of the health care system, or health policies, but could also be tied to declining social trust in general.
Keywords: Physician trust, health services, diversity, immigration
Introduction
Analyses of US public opinion for almost half a century indicate that physician distrust has increased sharply over time.1 Numerous studies have shown that physician trust is important for various health-related outcomes, including medication and other treatment adherence,2,3 self-rated health and additional health outcomes,2,4 and use of preventative services.5 Studies have found that physician trust varies across a number of different factors, including race,5–7 physician payment method,8 length of physician–patient relationship,9,10 patient health,9 physician wait times,9,10 physician communication, and 11 even interactions between race, gender, socioeconomic status (SES), and city of residence.7 Notably, a number of qualitative and quantitative studies have indicated lower physician trust for foreign physicians.9,10,12
Paralleling the decline in physician trust over time, social scientists studying social capital have observed a decline in social trust and civic engagement.13 Moreover, studies have found an inverse relationship between social capital and indicators of diversity, especially immigration-related diversity.14 Putnam proposed that social distance might account for this inverse relationship between social capital and diversity.14 Studies using attitudinal indicators of intergroup relations have confirmed that social distance–based attitudes toward Blacks moderate (increase) the negative relationship between population heterogeneity and both participation in voluntary organizations15 and trust.16 Furthermore, charitable giving decreases as perceptions of immigrant job competition increase, attitudes that also reflect social distancing from immigrants.17
Immigration for some is tied to both perceptions of out-group hostility and group competition.18 According to group position theory, a sociological social-psychological approach to analyzing intergroup relations,19,20 the construction of group boundaries and decisions about who is included in or excluded from such socially constructed categories is fundamental to understanding intergroup relations. Moreover, the perceived encroachment upon or violation of these group boundaries and their associated entitlements invites an emotional reaction. The construction and maintenance of group boundaries are also central to Putnam’s account of diversity, social distance, and social trust, particularly with Putnam’s reference to the social-psychological concept of social identity and his advocacy for “redraw[ing] more inclusive lines of social identity.” 21 These underlying dimensions of out-group hostility and emotionally charged perceptions of group competition20 are particularly relevant in light of research arguing that physician trust, in contrast to physician satisfaction, involves a strong affective dimension.22 It would not be a stretch to propose that out-group hostility and competition contribute to declining social trust in an increasingly diverse society. Finally, to the extent that some Americans bristle at immigration-related cultural changes and language differences,23 physician distrust might increase if linguistic/communication barriers become more prevalent in physician–patient interactions.12
While Putnam has stated that social trust is “different from trust in institutions and political authorities,” 24 some of his social trust examples lend themselves to a reconceptualization of physician trust as a partial reflection of social trust. Discussing “the social geography of social trust” in reference to survey data about honesty and trust, Putnam offered instances of reduced social trust in big cities versus small towns. These examples include “store clerks in small towns are more likely to return overpayment,” the small town lower likelihood of “cheating on … insurance claims,” and “[c]ar dealers in small towns perform far fewer unnecessary repairs than big-city dealerships.”25 Each of these generalizations might reasonably describe aspects of the health care system, for example, payment and insurance. Substituting physicians and medical procedures/tests for car dealers and repairs suggests an analogous example for physician trust. A linchpin underlying this reconceptualization of physician trust as a partial indicator of social trust is the centrality of honesty for both physician practice and generalized reciprocity, a key dimension of social capital. According to Putnam,26 “Trustworthiness, not simply trust, is the key ingredient.” The dense social networks at the center of most examinations of social capital facilitate the flow of information regarding reputations and honesty, factors relevant to physician practice. Finally, Putnam notes that the demand for lawyers has increased amid the decline in social trust and honesty, yet another factor not unfamiliar to physicians or the patients who distrust them. 27
Since social science research on immigration-based diversity and declining social capital indicates that immigration-related social distancing may be occurring, with deleterious effects on trust, this study brings together these two literatures (health/medical services and the social sciences) to pose the question “Is there a relationship between physician distrust and attitudes toward immigration?” Specifically, to the extent that support for immigration reduction captures in some part a social distancing away from immigrants, some of whom work as physicians and other health care professionals, the following hypothesis is tested: increasing support for immigration reduction is positively related to physician distrust.
Recent data reveal that close to one in four physicians in the United States was trained outside of the United States, though some international medical graduates are US-born.28 With a looming physician shortage projected over the next decade,29 some have argued that this shortage can be partially addressed with foreign-born and foreign-trained physicians and other health care providers.30 If this study’s data support the proposed hypothesis, foreign physician distrust may not only arise from physician–patient interaction itself. Instead, such distrust may be part of the immigration distancing already described by social capital and civic engagement researchers.14 Such social distrust is then reflected in patient encounters with foreign physicians, but not necessarily instigated by foreign physicians or by the structure of health care payments and other health policies.
This last point can also be understood in light of conceptual distinctions between personal and institutional objects of trust and individual and system levels of trust. As researchers have argued,31 a personal object of trust at the individual level may be a person’s personal doctor or care provider, while an institutional object of trust at the individual level may be a person’s particular hospital, clinic, or health plan. The latter institutional object at the system level would represent hospitals, clinics, or health plans in general.32 This study instead focuses on doctors or care providers in general, or the personal object of trust at the system level, rather than an individual’s own doctor or own experienced interactions with particular doctors. In line with the earlier discussion of group-level cognitive boundaries, this conceptual distinction between personal objects of trust at the individual and system levels is similar to the group position distinction between self-interest and perceived group interests, as captured in the following quote pertaining to school busing for racial desegregation:
People can form an opinion about an ongoing and controversial issue like busing simply by thinking in terms of the interests of “myself and people like me.” People need not be touched by busing directly … in order to form an opinion.33
Likewise, people can form an opinion about the trustworthiness of physicians in general by thinking in terms of group boundaries separating immigrants from the native-born. People need not interact with a foreign-born physician directly in order to form an opinion.
Methods
Sample
Data come from the 2012 General Social Survey (GSS), collected by the National Opinion Research Center, headquartered at the University of Chicago. The GSS has been collected since 1972 and is funded by the National Science Foundation’s sociology program. The 2012 GSS sampled both English and Spanish speakers, using a multi-stage area probability sample: standard metropolitan statistical area at the first stage, block groups and enumeration districts at the second stage, and blocks at the third stage. Quota sampling at the block level is used to select on sex, age, and employment status. Most interviews were face-to-face, though some were conducted by phone. The valid N for the study was 1080 respondents, omitting inapplicable respondents who were not asked the survey questions used in this study.
Measures
A physician distrust scale is constructed from responses to the following survey items:
How much do you agree or disagree with the following statements about doctors in general in the United States?
All things considered, doctors can be trusted;
Doctors discuss all treatment options with their patients;
The medical skills of doctors are not as good as they should be (reverse coded);
Doctors care more about their earnings than about their patients (reverse coded);
Doctors would tell their patients if they made a mistake during treatment.
Responses ranged on a 5-point scale from strongly agree to strongly disagree, with neither agree nor disagree at the midpoint. Don’t know and No answer responses were coded as missing and later imputed using multiple imputation methods. The constructed scale averaged standardized responses to these five items, with higher values of the scale representing stronger disagreement with doctor trust (alpha reliability = 0.69) and therefore higher levels of physician distrust. Construction of this scale required reverse coding of responses for the third and fourth items.
The predictor variable represents attitudes toward US immigration levels, captured with the following question: “Do you think the number of immigrants to America nowadays should be increased a lot, increased a little, remain the same as it is, reduced a little or reduced a lot?” Responses range on a 5-point scale, with support for immigration reduction at the high end. Can’t choose and No answer responses were coded as missing and later imputed. Although a single-item measure, prior research indicated that this immigration reduction attitude captures both perceptions of intergroup competition and affect-laden modern day prejudice, or racial resentment, among national samples of both White and Black respondents.18 Among White respondents, immigration reduction attitudes also reflected intergroup social distance, measured by disapproval of interracial/interethnic marriage.
The analyses controlled for a standard battery of demographic and social background variables: age (continuous), education (continuous, highest grade completed), family income (continuous, thousands of dollars), female (binary), race (binary variables for Black and other race), and foreign-born (binary).
This study also controlled for possible confounding variables. Given conservative advocacy for immigration control as well as conservative skepticism of physicians’ role in Affordable Care Act “death panels,” conservatism is controlled using a seven-response scale ranging from extremely liberal to extremely conservative, with moderate at the midpoint. The next three possible confounders (unemployed status, no health insurance, and poor health) reflect possible economic vulnerability that could be tied to both physician distrust and support for immigration reduction. Unemployed status (unemployed, laid off, looking for work) is a dummy variable, constructed from a work status variable with “other” coded as missing. Lack of health insurance is introduced as a dummy variable. Finally, self-reported poor health is based on a health status item that ranges from excellent to poor on a five-response scale. For conservatism, insurance status, and self-reported general health, Don’t know and No answer were coded as missing. Table 1 presents weighted sample means and distributions of the study variables.
Table 1.
Sample characteristics: General Social Survey (2012), N = 1080.
| Items for Physician Distrust Scale (multiple items) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Trusted | Discuss | Skills | Earnings | Mistake | ||||
| Support for immigration restriction | ||||||||
| Increased a lot | 4.4% | Strongly agree | 7.0% | 6.5% | 4.4% | 7.3% | 3.4% | |
| Increased a little | 9.2% | Agree | 51.3% | 36.2% | 28.6% | 21.7% | 21.6% | |
| Remain the same | 34.0% | Neither agree nor disagree | 23.1% | 17.9% | 25.5% | 28.3% | 19.7% | |
| Reduced a little | 27.3% | Disagree | 13.2% | 31.8% | 33.2% | 34.1% | 39.0% | |
| Reduced a lot | 22.8% | Strongly disagree | 3.2% | 4.4% | 3.6% | 5.7% | 12.3% | |
| Can’t choosea | 1.7% | Don’t knowa | 2.0% | 3.1% | 4.8% | 2.8% | 4.0% | |
| No answera | 0.5% | No answera | 0.2% | 0.2% | 0.04% | 0.04% | 0.04% | |
| Age (years) | 48.0 (SD = 17.1) | 1.3% missing | Physician distrust scale | −0.002 (SD = 0.67) | ||||
| Range: −1.9 to 2.0 | ||||||||
| Education (highest grade) | 13.7 (SD = 2.9) | 0.05% missing | ||||||
| Family income (thousands) | 38.7 (SD = 42.4) | 11% missing | ||||||
| Female | 55.1% | Foreign-born | 12.6% | |||||
| Race | Unemployed | 6.5% | 2.5% missing | |||||
| White | 74.3% | |||||||
| Black | 15.1% | No health insurance | 18.2% | 0.7% missing | ||||
| Other race | 10.6% | |||||||
| Conservatism | Health status | |||||||
| Extremely liberal | 3.4% | Excellent | 15.1% | |||||
| Liberal | 14.3% | Very good | 30.9% | |||||
| Slightly liberal | 10.1% | Good | 31.5% | |||||
| Moderate | 36.0% | Fair | 18.3% | |||||
| Slightly conservative | 14.8% | Poor | 4.0% | |||||
| Conservative | 14.0% | Don’t knowa | 0.2% | |||||
| Extremely conservative | 4.8% | No answera | 0.04% | |||||
| Don’t knowa | 1.9% | |||||||
| No answera | 0.6% | |||||||
Mean values (standard deviations (SD) in parentheses) for continuous measures.
Response coded as missing.
Analyses
Ordinary least squares (OLS) regression models with survey weights were used to estimate the dependent variable. Multicollinearity diagnostics on the unweighted model did not reveal any concerns. Multiple imputation methods were used to recover missing values on the variables used in this study.34 Missing data varied from 11% of cases on income to 0.1% of cases on education. Results did not differ between models estimated using a sample with no missing values imputed (complete cases only) and models estimated with cases recovered through multiple imputation of missing data. The results presented below utilize the sample that involved multiple imputations for missing data.
Results
Table 2 presents the results of the regression models. The unadjusted relationship between support for immigration reduction and physician distrust is positive and significant (Model 1, B = 0.104, p < 0.001, two-tailed), providing support for the hypothesis. The relationship remains significant even after adjusting for covariates (Models 2 and 3).
Table 2.
Survey-weighted models estimating physician distrust, by immigration restriction support and controls.
| Multiple item physician distrust |
Single item |
|||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Support for immigration restriction | 0.104*** (0.0226) | 0.101*** (0.0230) | 0.0948*** (0.0221) | 0.265*** (0.0723) |
| Age | 0.000143 (0.00143) | −0.000347 (0.00149) | −0.00882* (0.00446) | |
| Education (highest grade) | −0.00517 (0.00791) | 0.00111 (0.00766) | −0.0477 (0.0290) | |
| Family income (thousands) | −0.00144* (0.000582) | −0.000953 (0.000586) | −0.000349 (0.00220) | |
| Female | 0.0184 (0.0476) | 0.0237 (0.0467) | 0.264 (0.152) | |
| Racea | ||||
| Black | 0.0933 (0.0635) | 0.0838 (0.0620) | 0.622** (0.202) | |
| Other race | 0.154 (0.0894) | 0.127 (0.0870) | 0.450 (0.326) | |
| Foreign-born | −0.0840 (0.0835) | −0.0538 (0.0827) | −0.449 (0.317) | |
| Conservatism | 0.00707 (0.0171) | 0.0626 (0.0536) | ||
| Unemployed | 0.182 (0.111) | −0.0335 (0.391) | ||
| No health insurance | −0.00740 (0.0743) | 0.343 (0.208) | ||
| Poor health | 0.106*** (0.0236) | 0.257** (0.0782) | ||
| Constant | −0.344*** (0.0826) | −0.247 (0.168) | −0.626** (0.196) | (omitted) |
| F-statistic | 21.05*** | 4.48*** | 5.19*** | 5.22*** |
| Observations (N) | 1080 | 1080 | 1080 | 1080 |
Data: General Social Survey (2012).
Standard errors in parentheses.
Models (1)–(3) utilize an ordinary least squares (OLS) regression models estimating a physician distrust scale constructed from multiple items, and Model (4) utilizes an ordinal logistic regression model estimating a single-item physician distrust measure.
White (reference category).
p < 0.001; **p < 0.01; and *p < 0.05 (two-tailed).
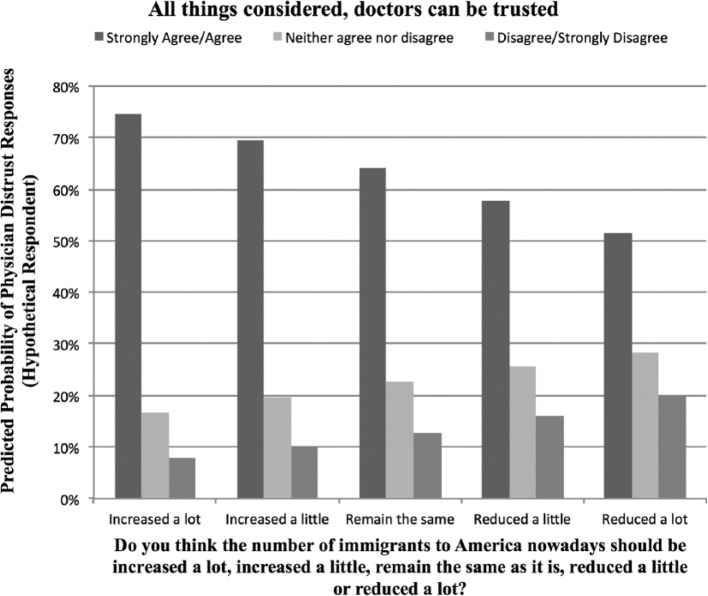
To more clearly show the relationship between immigration reduction attitudes and physician distrust, an ordinal logistic regression model, with survey weights, was estimated to obtain predicted probabilities of expressing physician distrust using the following single-item measure: “All things considered, doctors can be trusted.” For the purposes of estimating the model, responses to this item were collapsed into three categories: strongly agree/agree, neither agree nor disagree, and disagree/strongly disagree. Model 4 (Table 2) presents the results of the ordinal logistic regression for the single-item measure of physician distrust. The main hypothesized relationship between support for immigration reduction and physician distrust was confirmed, validating the aforementioned linear regression results. Ordinal logistic regression model diagnostics revealed that the immigration reduction independent variable did not violate the parallel slopes assumption in both the unweighted and weighted models (complete cases sample). In the unweighted model, poor health violated the proportional odds assumption, while in the survey-weighted model, age, female, other race, conservatism, and unemployment status violated the proportional odds assumption. In light of these model violations, partial proportional odds models were estimated, which also confirmed the hypothesized association between support for immigration reduction and physician distrust. The main effect of immigration reduction support estimated by the survey-weighted proportional odds model (N = 942) was 0.268 (p < 0.001), which approximates the comparable effect in Table 2, Model 4 (N = 1080) of 0.265 (p < 0.001).
Figure 1 presents the predicted probabilities calculated utilizing the coefficients estimated in Model 4. For the purpose of estimating the predicted probabilities, the covariates are set at their mean (continuous) or modal (categorical) values. Figure 1 illustrates that the probability of disagreeing or strongly disagreeing that doctors can be trusted increases as support for immigration reduction increases. For the hypothetical respondent who believes immigration numbers should be increased a lot, or does not appear to express social distance from immigrants, the predicted probability of physician distrust is 8%. By contrast, the comparable predicted probability of physician distrust is 20% for the hypothetical respondent who believes immigration numbers should be reduced a lot.
Figure 1.
Predicted probability of physician distrust, by support for US immigration reduction.
Supplementary analyses were conducted to examine the effects of controlling for various measures of trust. The GSS contained a handful of measures of institutional and general trust, the former in reference to providing correct information about causes of pollution (see Table 3 for question wording). The split ballot design did not allow analyses with these measures and this study’s full sample, so only subsamples are analyzed. Table 3 presents results from the sample subsets that included trust indicators (business trust, government trust, and general trust) as additional controls. As the supplementary results indicate, controlling for various trust measures, each of which is significant, does not explain away the significant relationship between support for immigration reduction and physician distrust.
Table 3.
Survey-weighted models estimating physician distrust (multiple item), by immigration restriction support, controls, and trust measures.
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Support for immigration restriction | 0.101** (0.0322) | 0.0897** (0.0318) | 0.104** (0.0319) | 0.0950** (0.0316) | 0.0889** (0.0299) | 0.0761* (0.0296) |
| Business trusta | 0.144*** (0.0386) | |||||
| Government trustb | 0.106** (0.0396) | |||||
| General trustc | 0.105** (0.0372) | |||||
| F-statistic | 3.10*** | 3.47*** | 3.08*** | 3.15*** | 4.10*** | 4.43*** |
| Observations (N) | 482 | 482 | 487 | 487 | 576 | 576 |
Data: General Social Survey (2012).
Standard errors in parentheses.
All models control for all covariates presented in Table 2.
Business trust: “How much trust do you have in each of the following groups to give you correct information about causes of pollution: business and industry?” (1) A great deal of trust, (2) Quite a lot of trust, (3) Some trust, (4) Not much trust, and (5) Hardly any trust.
Government trust: “How much trust do you have in each of the following groups to give you correct information about causes of pollution: government departments?” (1) A great deal of trust, (2) Quite a lot of trust, (3) Some trust, (4) Not much trust, and (5) Hardly any trust.
General trust: “Generally speaking, would you say that most people can be trusted or that you can’t be too careful in life?” (1) Most people can be trusted, (2) Depends, and (3) You can’t be too careful in life.
p < 0.001; **p < 0.01; and *p < 0.05 (two-tailed).
Additional supplementary analyses controlled for the possible effects of a respondent’s last doctor’s visit and confirmed the model’s relevance to other domains in which immigration may be salient (e.g. science). The GSS contained an item measuring satisfaction with treatment received during last doctor’s visit. Introducing this factor in the full model (Table 2, Model 3) did not explain away the association between immigration restriction support and physician distrust (see Table 4). Further models examined whether immigration restriction support was linked to science, technology, engineering, and mathematics (STEM)-related attitudes as professions with an increasing number of immigrants.35 Immigration restriction support was associated with a range of STEM-related attitudes, including declining confidence in the science community as a US institution and disagreement that scientific research advances the frontiers of knowledge and should be supported by the federal government (results available upon request). Confidence in the scientific community as an institution was considered as an additional control for the immigration restriction–physician distrust relationship, though with a smaller sample due to the split ballot design (N = 579). As Table 4 (Models 3–6) indicates, confidence in the scientific community accounts for much of the residual association between immigration restriction support and physician distrust, though there is still a marginally significant association (p = 0.07, two-tailed) after introducing this control. However, after also controlling for satisfaction from last doctor’s visit (Model 6), there is no longer an association between immigration restriction support and physician distrust. It therefore appears that (lack of) confidence in the US scientific community is a major factor associated with both immigration restriction support and physician distrust.
Table 4.
Ancillary analyses of physician distrust (multiple item), by immigration restriction support, controls, doctor satisfaction, and confidence in scientific community.
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Support for immigration restriction | 0.0925*** (0.0222) | 0.0828*** (0.0213) | 0.0747* (0.0292) | 0.0529+ (0.0293) | 0.0589* (0.0280) | 0.0364 (0.0279) |
| Doctor satisfactiona | 0.180*** (0.0171) | 0.184*** (0.0213) | 0.185*** (0.0201) | |||
| Confidence in scientific communityb | 0.211*** (0.0538) | 0.217*** (0.0464) | ||||
| F-statistic | 5.11*** | 14.50*** | 3.97*** | 10.54*** | 4.58*** | 12.25*** |
| Observations (N) | 1080 | 1080 | 579 | 579 | 579 | 579 |
Data: General Social Survey (2012).
Standard errors in parentheses.
All models control for all covariates presented in Table 2.
The Model 1 effect (0.0925) differs slightly from Table 2, Model 3 (0.0948) due to adding doctor satisfaction to the missing data imputation model.
Doctor satisfaction: “How satisfied or dissatisfied were you with the treatment you received: when you last visited a doctor?”(1) Completely satisfied, (2) Very satisfied, (3) Fairly satisfied, (4) Neither satisfied nor unsatisfied, (5) Fairly unsatisfied, (6) Very unsatisfied, and (7) Completely unsatisfied.
Confidence in scientific community: “I am going to name some institutions in this country. As far as the people running these institutions are concerned, would you say you have a great deal of confidence, only some confidence or hardly any confidence at all in them? Scientific community?” (1) A great deal, (2) Only some, and (3) Hardly any.
p < 0.001; **p < 0.01; *p < 0.05; and +p < 0.10 (two-tailed).
Discussion
The results of this study confirm the hypothesized relationship between immigration reduction attitudes and physician distrust. As such, this study ties physician trust to prior research focused on the reported negative effects of diversity, including immigration-based diversity.14–17 However, the supplementary analysis examining general trust as a possible mediator of this relationship raises some doubt as to whether social trust is a key dimension of the association between immigration reduction and physician distrust. Nevertheless, that general trust is itself independently associated with physician trust in the split ballot supplementary analysis does build on established social science research on social capital and physician trust,4,36 bringing physician distrust squarely into the orbit of social capital research using individual-level reports of general trust, though not necessarily as part of the immigration attitudes link to physician distrust.
Furthermore, the ancillary results from Table 4 reveal that these sentiments regarding immigration restriction are a key dimension of a more general lack of confidence in the US scientific community as an institution. Various explanations have been provided for either a lack of confidence in the US scientific community or anti-science attitudes, including difficulties with science education/schooling,37,38 religious faith,37,39 racial group skepticism toward past unethical scientific endeavors,37 and the perceived politicization of science, especially among conservatives.40
A further consideration of both the science education and group skepticism explanations invites consideration of an association specific to particular gender and racial groups. Recently, educators and researchers have focused their attention on improving STEM education among female38 and ethno-racial minority students.41 Some STEM classes are taught by foreign-born teachers, introducing potential language/communication challenges.42 In light of these studies, a final set of supplementary analyses was undertaken to explore group-specific associations (see Table 5). The most striking finding is that the association between immigration restriction support and physician distrust is significant among non-Hispanic White women (p < 0.05, two-tailed), even controlling for confidence in the scientific community and last doctor visit. There is no parallel association among White men. While the association between immigration restriction support and physician distrust among non-Whites is statistically non-significant in the smaller sample, the larger sample of non-Whites, prior to respondent omission due to the split ballot control for confidence in science, still revealed a significant association between immigration attitudes and physician distrust (p < 0.05, two-tailed, results available upon request).
Table 5.
Race/gender analyses of physician distrust (multiple item), by immigration restriction support, controls, doctor satisfaction, and confidence in scientific community.
| Pooled | Whites | Non-Whites | White males | White females | |
|---|---|---|---|---|---|
| Support for immigration restriction | 0.0364 (0.0279) | 0.049+ (0.029) | 0.043 (0.055) | −0.015 (0.044) | 0.101* (0.040) |
| Doctor satisfactiona | 0.185*** (0.0201) | 0.203*** (0.022) | 0.091* (0.044) | 0.211*** (0.029) | 0.194*** (0.032) |
| Confidence in scientific communityb | 0.217*** (0.0464) | 0.221*** (0.055) | 0.204* (0.090) | 0.289*** (0.062) | 0.161+ (0.088) |
| F-statistic | 12.25*** | 13.71*** | 3.53*** | 8.25*** | 8.64*** |
| Observations (N) | 579 | 446 | 133 | 189 | 257 |
Data: General Social Survey (2012).
Standard errors in parentheses.
All models control for all covariates presented in Table 2.
Doctor satisfaction: “How satisfied or dissatisfied were you with the treatment you received: when you last visited a doctor?” (1) Completely satisfied, (2) Very satisfied, (3) Fairly satisfied, (4) Neither satisfied nor unsatisfied, (5) Fairly unsatisfied, (6) Very unsatisfied, and (7) Completely unsatisfied.
Confidence in scientific community: “I am going to name some institutions in this country. As far as the people running these institutions are concerned, would you say you have a great deal of confidence, only some confidence or hardly any confidence at all in them? Scientific community?” (1) A great deal, (2) Only some, and (3) Hardly any.
p < 0.001; **p < 0.01; *p < 0.05; and +p < 0.10 (two-tailed).
Closer examination of the disaggregated multi-item-dependent variable provides clues regarding the individual items tied to immigration restriction support among particular types of respondents. White females were most concerned about doctors prioritizing earnings over patients in the smaller sample (N = 257), as well as doctors’ skills and nonspecific trust in doctors in the less constrained sample that does not control for scientific confidence (N = 476). Notably, this mirrors prior research that distinguishes between value and competence dimensions of trust toward the institution of health care as a whole, though not specifically physicians as an occupational subset of the health care system.43 Non-Whites’ immigration attitudes on the other hand were linked to nonspecific trust in doctors and doctors discussing all treatment options with their patients, but not doctors’ skills or doctors’ possible earnings incentives. Future research should re-examine these results with larger, multi-ethnic samples to minimize the loss of statistical power due to the GSS’ split ballot design.
The residual relationship between immigration reduction and physician distrust among non-Hispanic White women, after controlling for other (system level) trust measures, points in the direction of immigration-related interpersonal trust mediators tied to a social or group boundary involving nativity or immigration status. Because physician trust at the interpersonal level includes competence and interpersonal skills,31 social-psychological research on stereotype content, which maps group-based stereotypes along two dimensions, competence and warmth,44 may prove useful for future investigations of potential mediators of immigration-related attitudes and physician distrust. For instance, according to the stereotype content model, two US ethnic groups typically associated with immigration, Hispanics and Asians, fall short on either the competence and/or warmth dimension of stereotype content compared to Whites: Asians are stereotyped as more competent but less warm, while Hispanics are stereotyped as both less competent and less warm. Whether such stereotype dimensions mediate the link between immigration reduction and physician distrust, with warmth and competence seemingly important factors tied to physician trust, can be the subject of future research examining attitudes toward Asian and Hispanic immigrant doctors.
Also, because physician distrust involves an emotional component,22 future research may also want to consider whether perceptions of immigrant group competition may be a source of physician distrust. Among sociologists who study racial prejudice, group position theory proposes that negative out-group emotions are caused by perceived group competition; some part of the emotional component of physician distrust may be tied to such immigrant threat sentiments.19,20 Research has already shown that in some scientific occupations, such as computing and life sciences, the rising employment trends for US-born White women have either reversed and started to decline since the 1990s (computing) or plateaued (life sciences), while immigrant Asian men and immigrant women from various western countries (Europe, Canada, Australian, New Zealand, Canada, Germany, and Russia) have contemporaneously increased their share in these science occupations.45 There is also evidence that increases in the percent foreign-born in college decreases the likelihood that a US-born female college student selects a science and engineering major, possibly due to competition-related factors.46 The study’s additional analyses indicated that these US-born women were more likely to major in education and in psychology in response to the increasing percentages of immigrants in college.
Finally, the effects of some of the present study’s control variables, while not the central focus of this study, deserve some comment in light of previous research. For instance, researchers have found that education, health status, and insurance status are associated with negative attitudes toward physicians,47 though whether factors such as education and insurance status are significant can vary by ethno-racial group.7 Research has also discovered that the effect of foreign-born status differs based on the outcome, with no effect on trusting one’s own physician, though foreign-born respondents express less trust for physicians in general.48 Interestingly, a factor closely related to nativity, citizenship status has the opposite effect for Hispanics, with non-citizen Hispanics expressing greater trust for doctors than Hispanic US citizens.49 The apparent absence of these effects in this study appears to be tied in some part to differences in the items used to compose the multi-item dependent variable. For example, factors such as higher education and good health are both positively associated with the single-item measure of general trust in doctors, though the immigration attitude predictor explains away the effect of education in Table 2 (Model 4). Interestingly, those without health insurance are more likely to trust their doctor’s skills and trust that doctors will not prioritize their earnings, controlling for satisfaction with last doctor visit. This contradicts earlier research that identified a positive effect of having insurance.47 These last findings suggest, along with the absence of a foreign-born effect, that some associations may simply have changed with the present GSS data collected in 2012, compared to the GSS data collected in 1998.47,48 Research has already identified changes over time in factors associated with physician attitudes between the 1976 GSS data and the 1998 GSS data.47
Strength and limitations
A key strength of the study lies in data quality. The GSS is one of the three gold-standard public opinion surveys in the United States, in addition to the American National Election Studies and the Panel Study of Income Dynamics. The GSS is the second most frequently analyzed data source among social scientists, second only to the US Census.50
Despite relying on high-quality data, the study does have limitations. First, the data are cross-sectional. The causal arrow may be reversed; it may be the case that physician distrust, perhaps due to cultural or communication barriers with foreign physicians, leads respondents to want to reduce the number of immigrants to the US. Panel data that allows examination of whether a priori immigration attitudes predicts subsequent changes in physician trust would be useful. Second, the main predictor relies on a single-item measure of immigration concern; future research could draw on a wider range of immigration attitudes that also reflect intergroup social distance.18 Relatedly, future research can employ a variety of validated measures to examine physician trust/distrust,11 as well as generalized trust in doctors versus particular doctor trust.5,11 Future research might consider a number of additional omitted variables, such as attitudes toward English language proficiency and other physician communication variables. The GSS also lacked data on physician nativity or details about specific physician encounters, for example, patients’ perception of physicians’ scientific knowledge, technical skill, social skills, ethical conduct, compassion skills, and so on. Finally, given the widespread use of community-level social capital and diversity variables in research on social capital, future studies might employ community-level or even scientific occupation–level indices of ethnic or nativity heterogeneity to examine the role of contextual immigration-related diversity on physician distrust or confidence in science.
At a time when some consider turning to foreign-born and foreign-trained physicians to address the current and projected US physician shortage, this study reveals that Americans’ support for reducing immigration to the United States is linked to physician distrust. While prior studies have identified lower physician trust among patients interacting directly with a foreign physician,9,10 this study’s results suggest that physician–patient interactions may not solely be responsible for physician distrust even if the physician is foreign-born; rather physician distrust is linked to more oppositional attitudes toward immigration in general, which is also associated with a lack of confidence in the scientific community. Controlling for health insurance status indicated that this form of physician distrust was independent of healthy policy/health care payment structure. In light of social capital research that suggests social distance as the mechanism linking diversity to declining social capital,14 as well as health research indicating communication barriers with foreign doctors,12 future studies examining physician distrust through the lenses of both resistance to immigration-related diversity and lack of confidence in science as an institution, are needed.
Footnotes
Author’s note: Frank L Samson is currently affiliated to University of California, Los Angeles, CA, USA.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: Ethical approval was not sought for this study because survey data are de-identified, preserving respondent confidentiality. My previous institution’s institutional review board (University of Miami IRB) does not require ethics approval for de-identified secondary data analysis.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Informed consent was not sought for this study because the data are publicly available, de-identified survey data.
References
- 1. Blendon RJ, Benson JM, Hero JO. Public trust in physicians—US medicine in international perspective. N Engl J Med 2014; 371(17): 1570–1572. [DOI] [PubMed] [Google Scholar]
- 2. Lee Y-Y, Lin JL. The effects of trust in physician on self-efficacy, adherence and diabetes outcomes. Soc Sci Med 2009; 68(6): 1060–1068. [DOI] [PubMed] [Google Scholar]
- 3. Cuffee YL, Hargraves JL, Rosal M, et al. Reported racial discrimination, trust in physicians, and medication adherence among inner-city African Americans with hypertension. Am J Public Health 2013; 103(11): e55–e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mohseni M, Lindstrom M. Social capital, trust in the health-care system and self-rated health: the role of access to health care in a population-based study. Soc Sci Med 2007; 64(7): 1373–1383. [DOI] [PubMed] [Google Scholar]
- 5. Musa D, Schulz R, Harris R, et al. Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health 2009; 9(7): 1293–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Voils CI, Oddone EZ, Weinfurt KP, et al. Who trusts healthcare institutions? Results from a community-based sample. Ethn Dis 2005; 15(1): 97–103. [PubMed] [Google Scholar]
- 7. Armstrong K, Ravenell KL, McMurphy S, et al. Racial/ethnic differences in physician distrust in the United States. Am J Public Health 2007; 97(7): 1283–1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kao AC, Green DC, Zaslavsky AM, et al. The relationship between method of physician payment and patient trust. JAMA 1998; 280(19): 1708–1714. [DOI] [PubMed] [Google Scholar]
- 9. Shenolikar R, Balkrishnan R, Hall M. How patient-physician encounters in critical medical situations affect trust: results of a national survey. BMC Health Serv Res 2004; 4(1): 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Balkrishnan R, Dugan E, Camacho FT, et al. Trust and satisfaction with physicians, insurers, and the medical profession. Med Care 2003; 41(9): 1058–1064. [DOI] [PubMed] [Google Scholar]
- 11. Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. J Gen Intern Med 2000; 15(7): 509–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jacobs EA, Rolle I, Ferrans CE, et al. Understanding African Americans’ views of the trustworthiness of physicians. J Gen Intern Med 2006; 21(6): 642–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Putnam RD. Bowling alone: the collapse and revival of American democracy. New York: Simon & Schuster, 2000. [Google Scholar]
- 14. Putnam RD. E Pluribus Unum: diversity and community in the twenty-first century (The 2006 Johan Skytte prize lecture). Scand Polit Stud 2007; 30(2): 137–174. [Google Scholar]
- 15. Alesina A, La Ferrara E. Participation in heterogeneous communities. Q J Econ 2000; 115(3): 847–904. [Google Scholar]
- 16. Alesina A, La Ferrara E. Who trusts others? J Publ Econ 2002; 85(2): 207–234. [Google Scholar]
- 17. Samson FL. Perceived Group Competition and Charitable Giving: Racial Prejudice Affect as a Mediating Factor. Nonprof Volunt Sec Q . Epub ahead of print 10 December 2015. DOI: 10.1177/0899764015619702 [DOI] [Google Scholar]
- 18. Hutchings VL, Wong C. Racism, group position, and attitudes about immigration among blacks and whites. Du Bois Rev Soc Sci Res Race 2014; 11(2): 419–442. [Google Scholar]
- 19. Blumer H. Race prejudice as a sense of group position. Pac Socio Rev 1958; 1(1): 3–7. [Google Scholar]
- 20. Bobo LD. Prejudice as group position: microfoundations of a sociological approach to racism and race relations. J Soc Issues 1999; 55(3): 445–472. [Google Scholar]
- 21. Putnam RD. E Pluribus Unum: diversity and community in the twenty-first century (The 2006 Johan Skytte prize lecture). Scand Polit Stud 2007; 30: 165. [Google Scholar]
- 22. Thom DH, Hall MA, Pawlson LG. Measuring patients’ trust in physicians when assessing quality of care. Health Aff 2004; 23(4): 124–132. [DOI] [PubMed] [Google Scholar]
- 23. Huntington SP. The hispanic challenge. Foreign Pol 2004; 141: 30–45. [Google Scholar]
- 24. Putnam RD. Bowling alone: the collapse and revival of American democracy. New York: Simon & Schuster, 2000, p. 137. [Google Scholar]
- 25. Putnam RD. Bowling alone: the collapse and revival of American democracy. New York: Simon & Schuster, 2000, p. 138. [Google Scholar]
- 26. Putnam RD. Bowling alone: the collapse and revival of American democracy. New York: Simon & Schuster, 2000, p. 136. [Google Scholar]
- 27. Putnam RD. Bowling alone: the collapse and revival of American democracy. New York: Simon & Schuster, 2000, pp. 146–147. [Google Scholar]
- 28. Young A, Chaudhry HJ, Pei X, et al. A census of actively licensed physicians in the United States, 2014. J Med Regul 2015; 101(2): 8–23. [Google Scholar]
- 29. Dall T, West T, Chakrabarti R, et al. The complexities of physician supply and demand: projections from 2013 to 2025. Washington, DC: Association of American Medical Colleges, 2015. [Google Scholar]
- 30. Chen PG, Auerbach DI, Muench U, et al. Policy solutions to address the foreign-educated and foreign-born health care workforce in the United States. Health Aff 2013; 32(11): 1906–1913. [DOI] [PubMed] [Google Scholar]
- 31. Hall MA, Camacho F, Dugan E, et al. Trust in the medical profession: conceptual and measurement issues. Health Serv Res 2002; 37(5): 1419–1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Blendon RJ. Why Americans don’t trust the government and don’t trust healthcare. In: Shore DA. (ed.) The trust crisis in healthcare: causes, consequences, and cures. New York: Oxford University Press, 2007, pp. 21–31. [Google Scholar]
- 33. Bobo L. Whites’ opposition to busing: symbolic racism or realistic group conflict? J Pers Soc Psychol 1983; 45: 1196–1210. [Google Scholar]
- 34. Royston P. Multiple imputation of missing values. Stata J 2004; 4(3): 227–241. [Google Scholar]
- 35. Levin SG, Stephan PE. Are the foreign born a source of strength for US science? Science 1999; 285(5431): 1213–1214. [Google Scholar]
- 36. Ahern MM, Hendryx MS. Social capital and trust in providers. Soc Sci Med 57(7): 1195–1203. [DOI] [PubMed] [Google Scholar]
- 37. Plutzer E. The racial gap in confidence in science: explanations and implications. Bull Sci Tech Soc 2013; 33(5–6): 146–157. [Google Scholar]
- 38. Heaverlo CA, Cooper R, Lannan FS. STEM development: predictors for 6th–12th grade girls’ interest and confidence in science and math. J Women Minor Sci Eng 2013; 19(2): 121–142. [Google Scholar]
- 39. Gauchat GW. A test of three theories of anti-science attitudes. Socio Focus 2008; 41(4): 337–357. [Google Scholar]
- 40. Gauchat G. Politicization of science in the public sphere: a study of public trust in the United States, 1974 to 2010. Am Socio Rev 2012; 77(2): 167–187. [Google Scholar]
- 41. Hurtado S, Newman CB, Tran MC, et al. Improving the rate of success for underrepresented racial minorities in STEM fields: insights from a national project. New Dir Inst Res 2010; 2010(148): 5–15. [Google Scholar]
- 42. Nimoh P. Communication challenges faced by foreign-born faculty. Creat Nurs 2010; 16(2): 59–62. [DOI] [PubMed] [Google Scholar]
- 43. Yang T-C, Chen I-C, Noah AJ. Examining the complexity and variation of health care system distrust across neighborhoods: implications for preventive health care. Res Sociol Health Care 2015; 33: 43–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Fiske ST, Cuddy AJC, Glick P, et al. A model of (often mixed) stereotype content: competence and warmth respectively follow from perceived status and competition. J Pers Soc Psychol 2002; 82(5): 878–902. [PubMed] [Google Scholar]
- 45. Alegria SN, Branch EH. Causes and consequences of inequality in the STEM: diversity and its discontents. Int J Gend Sci Technol 2015; 7(3): 322–342. [Google Scholar]
- 46. Orrenius PM, Zavodny M. Does immigration affect whether US natives major in science and engineering? J Labor Econ 2015; 33(S1): S79–S108. [Google Scholar]
- 47. Pescosolido BA, Tuch SA, Martin JK. The profession of medicine and the public: examining Americans’ changing confidence in physician authority from the beginning of the “health care crisis” to the era of health care reform. J Health Soc Behav 2001; 42(1): 1–16. [PubMed] [Google Scholar]
- 48. Benjamins MR. Religious influences on trust in physicians and the health care system. Int J Psychiatry Med 2006; 36(1): 69–83. [DOI] [PubMed] [Google Scholar]
- 49. Boyas J, Valera PA. Determinants of trust in medical personnel. Hispanic Health Care Int 2011; 9(3): 144–152. [Google Scholar]
- 50. NORC. About GSS, n.d., http://www3.norc.org/GSS+Website/About+GSS/ (accessed 20 November 2015).