Abstract
Purpose
To expand the clinical usefulness of the Expanded Prostate Cancer Index Composite for Clinical Practice (EPIC-CP) by evaluating its responsiveness to health related quality of life (HRQOL) changes, defining the minimally important differences (MID) for an individual patient's change in each domain, and applying it to a sexual outcome prediction model.
Methods
In 1,201 subjects from a previously described multi-center, longitudinal cohort, we modeled each treatment group's EPIC-CP domain scores at pre-treatment, short-term, and long-term follow-up. We considered post-treatment domain score changes from pre-treatment ≥ 0.5 standard deviations (SD) clinically significant and with a p-value ≤ 0.01 as statistically significant. We determined domain MIDs using the 0.5 pooled SD of the 2, 6, 12, and 24 month post-treatment changes from pre-treatment. We recalibrated an EPIC-CP-based nomogram model predicting 2-year post-prostatectomy functional erections from that developed using EPIC-26.
Results
For every HRQOL domain, EPIC-CP was sensitive to similar post-treatment HRQOL changes over time as had been observed using EPIC-26. The EPIC-CP MIDs for changes in the urinary incontinence, urinary irritation/obstruction, bowel, sexual, and vitality/hormonal domains are 1.0, 1.3, 1.2, 1.6, and 1.0, respectively. The EPIC-CP-based sexual prediction model performs well (AUC=0.76) and shows robust agreement with its EPIC-26-based counterpart, with predicted probability differences between models of ≤10% for 95% of individuals and a mean difference of 0.0 (SD=0.05) across all individuals.
Conclusions
EPIC-CP is responsive to HRQOL changes during convalescence, and can be used to predict 2-year post-prostatectomy sexual outcomes. Its use can facilitate shared medical decision-making and patient-centered care.
Keywords: Prostatic Neoplasms/therapy, Quality of Life, Outcome Assessment (Health Care), Questionnaires, Patient Centered Care
Introduction
Evaluation of health related quality of life (HRQOL) in prostate cancer (PCa) patients without using a patient reported outcome (PRO) questionnaire underestimates the severity of side effects.1 Practitioners should be capable of not only counseling patients about these effects prior to treatment, but also accurately recognizing and managing any post-therapy HRQOL deficits.
Several existing PCa PRO instruments such as the UCLA-Prostate Cancer Index (UCLA-PCI)2 and the Expanded Prostate Cancer Index Composite (EPIC)3,4 can accurately evaluate PCa-related HRQOL changes over time.5 Researchers have also developed multivariable models that can predict post-treatment outcome based on pre-treatment HRQOL.6 However, these instruments are used mostly in the research realm, as they are too lengthy and time consuming to be used in clinical practice, limiting the ability of PCa practitioners to accurately assess HRQOL and optimally individualize treatment-related decisions.
To bridge the research and clinical realms, we previously developed the Expanded Prostate Cancer Index Composite for Clinical Practice (EPIC-CP) – a 16-item PRO questionnaire designed specifically for clinical use at the point of care – and showed that it has good internal consistency, reliability and discriminative validity, correlates highly with previous EPIC versions,3,4 and is convenient to use in the flow of routine practice.7 However, we have yet to demonstrate the responsiveness of EPIC-CP to treatment-related HRQOL changes over time.
Most PCa HRQOL PRO questionnaires, including EPIC-CP, group questions together into health domains (e.g. bowel, sexual), and represent outcomes using numerical domain scores. This is useful for examining trends or average changes in HRQOL over time, but can present challenges in clinical interpretation. For example, if a patient's EPIC-CP sexual score improves by two points between 6 and 12 months after brachytherapy, does this represent a statistical phenomenon or a clinically relevant change for the patient?
In this study, we had three objectives: 1) to evaluate the responsiveness of EPIC-CP to post-treatment HRQOL changes over time; 2) to increase the clinical interpretability of EPIC-CP by defining for each domain what score changes are clinically meaningful, and 3) to apply EPIC-CP to a clinically useful tool that uses pre-treatment EPIC-26 sexual score to predict post-treatment outcome, and compare the performance of the new EPIC-CP-based tool with its EPIC-26-based counterpart.
Methods
Study Population
We evaluated subjects from the previously described PRostate Cancer Outcomes and Satisfaction with Treatment Quality Assessment (PROST-QA) Cohort 8, a multicenter IRB-approved prospective study of 1,201 men with early stage PCa who had elected radical prostatectomy +/- nerve sparing, external beam radiotherapy +/- neoadjuvant hormonal therapy, or brachytherapy +/- external beam radiotherapy and/or neoadjuvant hormonal therapy from 2003 to 2006 at 9 university-affiliated hospitals. The EPIC-26 item responses of these 1,201 men were used to calculate their respective EPIC-CP scores.
Analysis and Statistical Considerations
Responsiveness of EPIC-CP to average post-treatment HRQOL changes over time
To model each of the six treatment group's EPIC-CP domain scores at pre-treatment, short-term, and long-term follow-up, we used generalized estimating equations with a compound symmetry working covariance structure. We defined “short-term” as either 2 or 6 months post-treatment based upon which time point showed greater EPIC-26 domain difference from pre-treatment,8 and considered “long-term” to be 24 months post-treatment. Each treatment group's EPIC-CP domain scores differing from pre-treatment with a p-value ≤ 0.01 were considered statistically significant (Bonferroni adjustment for multiple comparisons), and analogous to the original PROST-QA study8, domain scores differing by at least one-half standard deviation (0.5 SD) of the pre-treatment score were considered clinically significant.
Clinically Meaningful HRQOL changes in EPIC-CP
A clinically meaningful HRQOL change, also known as a minimally important difference (MID), is defined as the domain-specific summary score change threshold (usually a narrow range) at and above which an individual patient perceives a clinically relevant HRQOL change. Using Cohen's generally accepted effect size standard of one-half standard deviation to represent a moderate-size clinically relevant intra-individual HRQOL change,9 we used a distribution-based method to calculate the MID that emphasizes intra-individual changes in score over time. For each domain and treatment group, we determined the 0.5 SD of the pre-treatment scores, calculated the 0.5 SDs of the intra-individual score changes from pre-treatment at 2, 6, 12, and 24 months post-treatment, and then found the 0.5 pooled SD of the change from pre-treatment score, which we considered the MID for each treatment group. We used the 0.5 pooled SD of the change from pre-treatment score across timepoints and across treatments to calculate the overall MID (independent of treatment group) for each domain.
EPIC-CP-based multivariable predictive nomogram
We previously developed and externally validated an EPIC-26-based multivariable nomogram that uses pre-treatment sexual domain score to predict the probability of functional erections (defined as having erections firm enough for intercourse) 2 years after treatment.5 To adapt this tool for point of care clinical use among men planning radical prostatectomy, we used the same covariates of age, planned nerve-sparing approach, and PSA≤ 10 ng/mL to recalibrate the multivariable logistic regression prediction model using pre-treatment EPIC-CP sexual score in the 493 (of 524 previously-analyzed5) prostatectomy patients that had answered all EPIC-CP sexual domain questions. After examining Pearson residuals to ensure the recalibrated model was well fit, we examined the predicted probabilities for each individual under both sexual prediction models (EPIC-CP and EPIC-26), estimated the mean and standard deviation difference between the two models, determined the 95% limits of agreement,10 and compared the area under the curve of the receiver operating characteristic for each model.
Results
EPIC-CP vs EPIC-26
The key characteristics of EPIC-CP, its differences from EPIC-26, and its clinical feasibility were previously described and validated7, and are summarized in Table 1. Derived and reduced from EPIC-26, EPIC-CP retains the five EPIC HRQOL domains (urinary incontinence, urinary irritation/obstruction, bowel, sexual, and vitality/hormonal), has a total of 16 questions that fit on one page, and takes less than five minutes to complete. It differs from EPIC-26 primarily in its scoring system: whereas EPIC-26 requires transformation of item answers to a 0-100 scale that is calculation-intensive in the clinical setting, EPIC-CP is scored analogously to the AUA symptom index11: item answers for each domain are summed to calculate the domain score (0-12 for each domain). This enables EPIC-CP to be used at the point of care; it also changes the scoring directionality: good HRQOL is represented by a high score (100) in EPIC-26 and a low score (0) in EPIC-CP.
Table 1. Comparing and contrasting EPIC-CP and EPIC-26.
| EPIC-CP | EPIC-26 | |
|---|---|---|
|
|
||
| Number of domains | 5 | 5 |
| Can be scored at point of care | Yes | No |
| Scoring system | Similar to AUA-SI/IPSS | Similar to EPIC-50 and UCLA-PCI |
| Score range in each domain | 0-12 | 0-100 |
| Better QOL | Lower score | Higher score |
| Time to complete | 2-5 minutes | 10-15 minutes |
| Length | 16 questions – 1 page | 26 questions – 3 pages |
Figure 1 summarizes the EPIC-CP and EPIC-26 sexual domain scores for the group of subjects who underwent prostatectomy, and demonstrates the differences in scoring scale and direction between EPIC-CP (0-12) and EPIC-26 (0-100). Despite there being high domain score correlations between the instruments (>0.93 for all domains7), there is not a 1-to-1 mapping between measures; that is, each EPIC-CP score may correspond to a range of EPIC-26 scores for a domain. For example, subjects with EPIC-CP scores of 0 had corresponding EPIC-26 scores ranging from 83 to 100.
Figure 1.
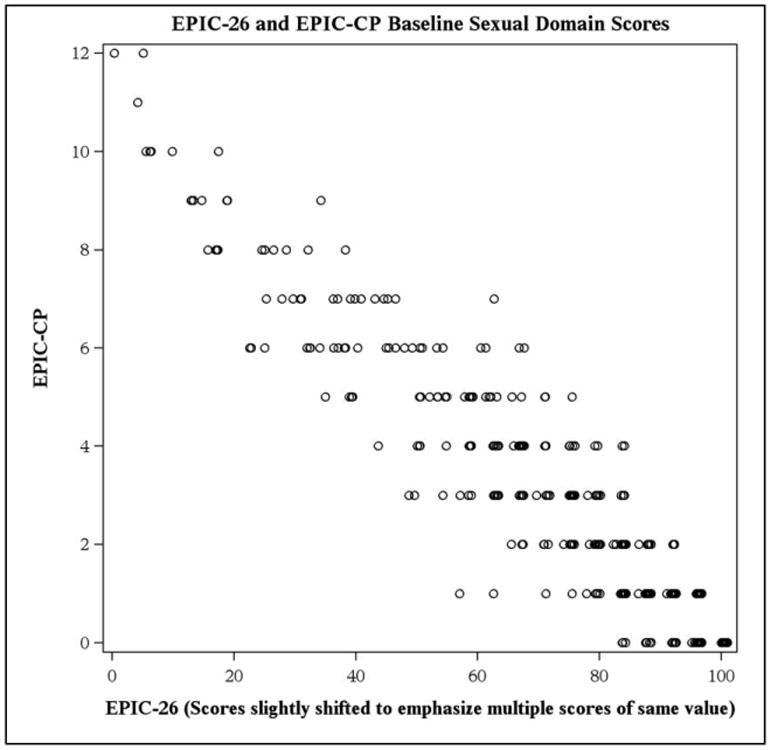
Relationship between EPIC-CP and EPIC-26 sexual domain scores in subjects who underwent radical prostatectomy and completed all EPIC-CP sexual domain questions (n=493).
EPIC-CP is responsive to average treatment-related HRQOL changes over time
The mean EPIC-CP domain summary scores by treatment group in the PROST-QA cohort at pre-treatment, short-term, and long-term post-treatment follow-up are shown in Table 2 for three of the six treatment groups. The treatment group XRT + NHT is displayed to demonstrate the sensitivity of the EPIC-CP vitality/hormonal domain to changes over time. For every HRQOL domain, treatment group, and post-treatment timepoint, EPIC-CP was able to detect almost identical statistically and clinically significant HRQOL differences between pre-treatment and short/long-term follow-up that were detected by EPIC-26 in the original PROST-QA study (Table 2).8
Table 2. Domain-specific short-term,a and long-termb changes in EPIC-CP scores from pre-treatment baseline by treatment group for 3 of 6 treatment groups analyzedc [Mean (SE)].
| Nerve-sparing Radical Prostatectomy | External Beam Radiotherapy with Neoadjuvant Hormonal Therapy | Brachytherapy Alone | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | Short term | Long term | Baseline | Short term | Long term | Baseline | Short term | Long term | |
|
|
|||||||||
| UI | 0.5 (0.0) | 4.2(0.1)* | 1.6(0.1)* | 0.6 (0.1) | 1.1 (0.2)† | 0.9 (0.2) | 0.5 (0.1) | 1.6 (0.1)* | 1.1 (0.1)* |
| UIO | 2.0 (0.1) | 2.6 (0.1)† | 1.2 (0.1)† | 1.8 (0.2) | 3.2 (0.3)* | 1.9 (0.3) | 1.6 (0.1) | 5.7 (0.2)* | 2.6 (0.2)† |
| B | 0.7 (0.1) | 1.2 (0.1)† | 0.8 (0.1) | 0.8 (0.2) | 2.8 (0.4)* | 2.2 (0.4)* | 0.7 (0.1) | 3.4 (0.2)* | 1.8 (0.2)* |
| S | 2.1 (0.1) | 8.0 (0.1)* | 5.8 (0.2)* | 4.4 (0.4) | 8.1 (0.4)* | 7.2 (0.4)* | 3.4 (0.2) | 5.3 (0.2)* | 5.3 (0.2)* |
| V/H | 1.4 (0.1) | 1.6 (0.1)† | 1.3 (0.1) | 1.2 (0.2) | 3.7 (0.3)* | 2.0 (0.3)† | 1.1 (0.1) | 1.9 (0.1)† | 1.3 (0.1) |
UI = urinary incontinence, UIO = urinary irritation/obstruction, B = bowel, S = sexual, V/H = vitality/hormonal
“Short-term” defined as either 2 or 6 months post-treatment depending upon which of the two time points showed greater EPIC-26 domain difference from pre-treatment baseline in Sanda et al8.
“Long-term” defined as 24 months post-treatment
The statistically and clinically significant changes observed above are identical to those observed with EPIC-26 in the PROST-QA study8 with the exception of the vitality/hormonal domain of XRT + NHT, and the sexual domain of BT + XRT and/or NHT (not shown above) at long-term follow-up, in which EPIC-26 found HRQOL changes to be clinically significant and EPIC-CP did not.
HRQOL at timepoint statistically and clinically significantly different from pre-treatment baseline
HRQOL at timepoint statistically significantly different from pre-treatment baseline only
Clinically meaningful changes in EPIC-CP scores
Table 3 describes the treatment-independent MIDs for each EPIC-CP domain, with the accompanying MID ranges among the six treatment groups. Treatment group-specific MIDs for each domain are described in Supplemental Table 1. We report MIDs for EPIC-CP to the nearest tenth despite EPIC-CP scores always being integers in practice. Practitioners should consider a score change greater than or equal to the MID to definitely be clinically meaningful, and should interpret a change within the MID range to be of potential clinical significance and worth further investigation during the clinical visit.
Table 3. Minimally important differences in EPIC-CP.
| MID* (range across treatment groups)† | |
|---|---|
| Urinary Incontinence | 1.0 (0.7 – 1.5) |
| Urinary Irritation/Obstruction | 1.3 (1.1 – 1.4) |
| Bowel | 1.2 (0.9 – 1.5) |
| Sexual | 1.6 (1.4 – 1.9) |
| Vitality/Hormonal | 1.0 (0.9 – 1.3) |
MID represents 0.5 pooled SD of the change between pre-treatment and 2, 6, 12, and 24 months post-treatment for each domain across all treatment groups and timepoints.
Described in the parenthesis is the range of this value across treatment groups (RP + NS, RP + NNS, XRT alone, XRT + NHT, BT alone, BT + XRT and/or NHT)
EPIC-CP-based multivariable sexual predictive model is usable at the point of care
The EPIC-CP-based sexual prediction model fits well based upon examination of Pearson residuals and performs similarly to its EPIC-26-based counterpart; the model AUC is 0.76. The odds ratios of the EPIC-CP-based model for age, planned nerve-sparing, and pre-treatment PSA are modified by no more than 0.1 from the EPIC-26-based model, and all factors remain statistically significant (p < 0.05). Because of the differences in the EPIC-CP scoring system, the EPIC-CP-based estimates for the intercept and pre-treatment sexual domain score are expectedly quite different from those of the EPIC-26-based model (Supplemental Table 2). A one point higher EPIC-CP pre-treatment sexual domain score (worse HRQOL) is associated with a reduced odds of 2-year functional erections by 30% (OR = 0.7, 95% CI 0.6 – 0.8; p < 0.001). Reciprocally, a one point lower EPIC-CP pre-treatment sexual domain score (better HRQOL) is associated with increased odds of 2-year post-treatment functional erections by 40% (OR =1.4, 95% CI 1.3 – 1.6).
Table 4 presents the EPIC-CP- and EPIC-26-based model-predicted probabilities of men having functional erections two years after radical prostatectomy stratified by the above factors. The corresponding model-predicted probabilities of the two nomograms differ by no more than 4 percentage points for each of the 36 model strata (Figure 2a). There is robust agreement between the models across subjects (n=493; Figure 2b), wherein the mean predicted probability difference is 0.0 (SD=0.05), with a predicted probability difference of ≤10% for 95% of individuals between models. Using this tool, a practitioner could counsel a 60 year old PCa patient with a PSA of 6.7 that given his pre-treatment EPIC-CP sexual score of 2, his approximate chances of having functional erections after nerve-sparing radical prostatectomy is 36%.
Table 4. Multivariable nomogram predicting the probability of having functional erections two years after radical prostatectomy, based on pretreatment a) EPIC-CP sexual score and b) EPIC-26 sexual score.
| Planned surgical technique | Age | Pretreatment PSA | Predicted Probability of Having Functional Erections 2-years After Treatment (by Pretreatment Sexual Score)* | |||||
|---|---|---|---|---|---|---|---|---|
| a) EPIC-CP† | b) EPIC-26†† | |||||||
| 0 | 2 | 4 | 100 | 83 | 67 | |||
| Nerve sparing | 50 | ≤10 | 67 | 50 | 34 | 70 | 52 | 35 |
| >10 | 46 | 30 | 18 | 50 | 32 | 18 | ||
| 60 | ≤10 | 53 | 36 | 22 | 57 | 38 | 23 | |
| >10 | 32 | 19 | 11 | 36 | 21 | 11 | ||
| 70 | ≤10 | 39 | 24 | 14 | 43 | 26 | 15 | |
| >10 | 21 | 12 | 6 | 24 | 13 | 7 | ||
| Non-nerve sparing | 50 | ≤10 | 35 | 21 | 12 | 39 | 23 | 13 |
| >10 | 19 | 10 | 6 | 21 | 11 | 6 | ||
| 60 | ≤10 | 23 | 13 | 7 | 27 | 15 | 8 | |
| >10 | 11 | 6 | 3 | 13 | 7 | 3 | ||
| 70 | ≤10 | 15 | 8 | 4 | 17 | 9 | 5 | |
| >10 | 7 | 3 | 2 | 8 | 4 | 2 | ||
Despite the lack of a 1:1 numerical correspondence in EPIC-CP and EPIC-26 scores across subjects (Figure 1), we present sexual domain strata in the EPIC-CP model that are numerically similar to those previously used in the EPIC-26 model (0 vs. 100, 2 vs. 83, 4 vs. 67) for the sake of juxtaposition.
Log odds of having Functional Erections after Radical Prostatectomy: 1.46 – 0.35 (Pre-treatment EPIC-CP Sexual Score) – 0.59 (age per 10 years) + 1.31 (Nerve-sparing) + 0.86 (PSA ≤ 10)
Adapted from Alemozaffar et al6
Figure 2.
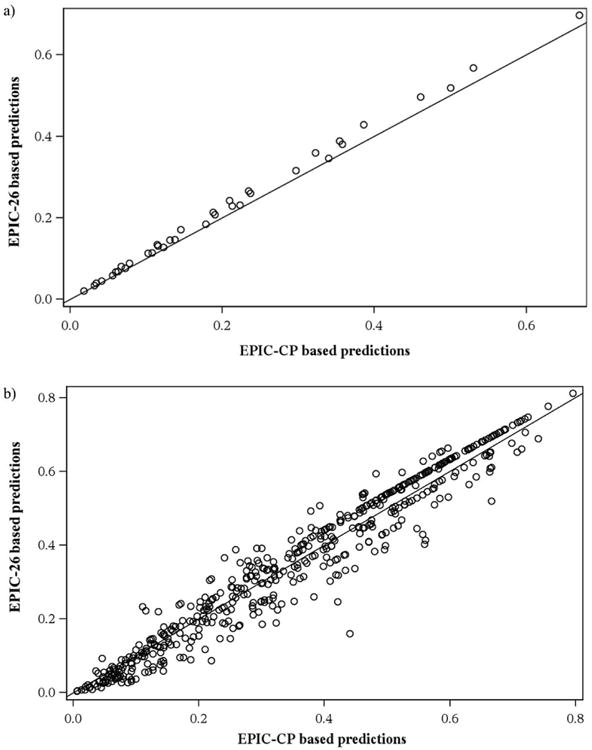
Comparing the predicted probability of having functional erections 2 years after treatment using pre-treatment EPIC-CP sexual score versus EPIC-26 sexual score a) at 36 different levels of the model factors (corresponding to the 36 strata in Table 4), and b) for all 493 subjects who underwent radical prostatectomy. The plotted line is the line of equality.
Discussion
This study aims to improve the clinical usefulness and interpretability of existing PCa instruments, thereby extending a path by which the fruits of cutting edge HRQOL research can be brought to every individual patient with prostate cancer. In its current state, PCa HRQOL research is equally as sophisticated in its depth and as it is challenging to apply to individuals in the clinical setting. Indeed, a recent CaPSURE study showed that despite the development of questionnaires such as the UCLA-PCI and EPIC, and the performance of several prospective long-term studies that have clarified the HRQOL consequences of PCa treatment, clinicians are no better at objectively assessing PCa patients' quality of life today than we were 20 years ago.1
The most obvious explanation is that the above mentioned instruments were developed for use in research, and are simply not being routinely used in clinical practice. We specifically designed EPIC-CP to bridge the research and clinical realms – it may lack the breadth and granularity of previous EPIC versions, but it is practical and convenient for use in busy routine practice.7 This study expands on our initial work and shows the responsiveness of EPIC-CP to PCa treatment effects over time, and therefore its appropriateness for use in every follow-up visit to assess patients' HRQOL after treatment.
This study also addresses another challenge inherent to all PRO instruments: clinical interpretability. By defining the minimally important difference (MID) of changes for EPIC-CP, practitioners now have a score threshold for each domain above which a change should be considered clinically meaningful. Other approaches to improving clinical interpretability of PRO instruments also deserve mention. The categorization of AUA Symptom Index11 scores into mild, moderate, and severe was derived in part by correlation of symptom scores with physiological and anatomic measures of benign prostatic hyperplasia, and has since been used in clinical guidelines12 and to predict the likelihood of clinical outcomes such as urinary retention.13 Others have used convergent validity to improve clinical interpretability. Ellison et al designated categories (mild, moderate, and severe) and score cutpoints (0-49, 50-69, 70-100, respectively) for the EPIC-26 urinary incontinence domain based on their correlation with established cutpoints for the Incontinence Severity Index (ISI).14,15 Several researchers have performed similar analyses correlating the EPIC-26 and Sexual Health Inventory for Men (SHIM) in attempts to define the score cutoff that dependably predicts “potency.”16-18 Analogous analyses correlating EPIC-CP with other established PROs or clinical outcomes deserve future investigation.
The importance of PRO administration becoming a routine part of clinical care in PCa extends beyond the act of objective and accurate HRQOL assessment. Routine PRO use in clinical practice opens the door to a much richer goal: improved patient-centered care – the ability to individualize patient management choices and expectations based on pre-treatment or post-treatment HRQOL.19 In this study, we developed an EPIC-CP-based prediction model for functional erections after radical prostatectomy and illustrated strong agreement between the EPIC-CP model and its EPIC-26-based counterpart. Similar approaches could be used to recapitulate other EPIC models on the EPIC-CP platform, potentially allowing a significant body of published literature to be more readily applied to patient counseling.
While this study further validates and bolsters the clinical interpretability and applicability of EPIC-CP, it does not address how to implement widespread dissemination of PRO use, a goal described recently by Cooperberg, in which (while citing the EPIC-CP validation article) he stated that “[i]f novel prediction models are to develop from research instruments into clinically useful tools, … the first prerequisite is that all men managed for prostate cancer complete validated quality-of-life questionnaires at regular intervals, regardless of their participation in research studies.”20 Strategies for implementation and dissemination of EPIC-CP and other PROs deserve future investigation, as does the identification of barriers to routine PRO administration, and the assessment of PRO use on patient outcome/satisfaction and physician workflow.
There are several limitations to this study. EPIC-CP scores were derived from EPIC-26 item answers; however, given a complete EPIC-26 questionnaire (not just numerical domain scores), this derivation can be performed without error, and should not have an impact on subsequent analyses. We did not use anchor-based methods to determine the domain MIDs; however, most studies have found distribution- and anchor-based methods to reveal comparable results21, and when we applied our MID strategy to EPIC-26 (data not shown), we found similar results to previous work that utilized both distribution and anchor-based methods for EPIC-26.22 External validation and other metrics of prediction accuracy would further strengthen our sexual prediction model; however, it shows convergent validity through its robust agreement with the externally validated analogous EPIC-26-based model.6 We acknowledge that other questionnaires such as the ISI, AUA-Symptom Index, and SHIM are also appropriate for clinical use; however, EPIC-CP is currently the only validated questionnaire specifically designed for point-of-care use that comprehensively assesses PCa-specific HRQOL domains.
Conclusions
Despite its limitations, this study demonstrates that EPIC-CP can be used in the follow-up setting to assess post-treatment HRQOL, improves the clinical interpretability of EPIC-CP by defining the MID for each domain, and shows how EPIC-CP can be successfully applied to existing EPIC-based prediction models, improving their ease of use in the clinical setting. It strengthens the bridge between the research and clinical realms, and takes another step towards the ultimate goal of implementing patient-centered care and improving care quality.
Supplementary Material
Supplemental Table 1: Minimally important differences in EPIC-CP by treatment group*
Supplemental Table 2: Model predicting of Functional Erections 2 years after Radical Prostatectomy using pre-treatment a) EPIC-CP Sexual Score and b) EPIC-26 Sexual Score*
Acknowledgments
The PROSTQA Consortium includes contributions in cohort design, patient accrual and follow-up from the following investigators: Meredith Regan (Dana Farber Cancer Institute, Boston, MA); Larry Hembroff (Michigan State University, East Lansing, MI); John T. Wei, Dan Hamstra, Rodney Dunn, Laurel Northouse and David Wood (University of Michigan, Ann Arbor, MI); Eric A Klein and Jay Ciezki (Cleveland Clinic, Cleveland, OH); Jeff Michalski and Gerald Andriole (Washington University, St. Louis, MI); Mark Litwin, Chris Saigal, and Jim Hu (University of California—Los Angeles Medical Center, Los Angeles, CA); Thomas Greenfield, PhD (Berkeley, CA), Louis Pisters and Deborah Kuban (MD Anderson Cancer Center, Houston, TX); Howard Sandler (Cedars Sinai Medical Center, Los Angeles, CA); Adam Kibel (Brigham and Women's Hospital, Boston, MA); Douglas Dahl and Anthony Zietman (Massachusetts General Hospital, Boston, MA); Peter Chang and Irving Kaplan (Beth Israel Deaconess Medical Center, Boston, MA) and Martin G. Sanda (Emory University, Atlanta, GA).
We acknowledge PROSTQA Data Coordinating Center Project Management by Jill Hardy, MS (Michigan State University, East Lansing, MI), Erin Najuch and Jonathan Chipman, MS (Dana Farber Cancer Institute, Boston, MA) and Catrina Crociani, MPH (Beth Israel Deaconess Medical Center, Boston, MA), grant administration by Beth Doiron, BA (Beth Israel Deaconess Medical Center, Boston, MA), and technical support from coordinators at each clinical site.
Funding: National Institutes of Health (R01 CA95662, RC1 CA146596). This work was supported in part by a grant from the UrologyCare Foundation Research Scholars Program and Dornier Medtech titled “Measuring Prostate Cancer Patient Reported Outcomes at the Point of Care”.
References
- 1.Sonn GA, Sadetsky N, Presti JC, et al. Differing perceptions of quality of life in patients with prostate cancer and their doctors. J Urol. 2013 Jan;189(1 Suppl):S59–65. doi: 10.1016/j.juro.2012.11.032. discussion S65. [DOI] [PubMed] [Google Scholar]
- 2.Litwin MS, Hays RD, Fink A, et al. The UCLA Prostate Cancer Index: development, reliability, and validity of a health-related quality of life measure. Med Care. 1998;36(7):1002–12. doi: 10.1097/00005650-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Wei JT, Dunn RL, Litwin MS, et al. Development and validation of the Expanded Prostate Cancer Index Composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56:899–905. doi: 10.1016/s0090-4295(00)00858-x. [DOI] [PubMed] [Google Scholar]
- 4.Szymanski KM, Wei JT, Dunn RL, et al. Development and validation of an abbreviated version of the Expanded Prostate Cancer Index Composite instrument for measuring health-related quality of life among prostate cancer survivors. Urology. 2010 Nov;76(5):1245–50. doi: 10.1016/j.urology.2010.01.027. Epub 2010 Mar 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rnic K, Linden W, Tudor I, et al. Measuring symptoms in localized prostate cancer: a systematic review of assessment instruments. Prostate Cancer Prostatic Dis. 2013 Jun;16(2):111–22. doi: 10.1038/pcan.2013.1. Epub 2013 Feb 5. [DOI] [PubMed] [Google Scholar]
- 6.Alemozaffar M, Regan MM, Cooperberg MR, et al. Personalized prediction of erection recovery after primary prostate cancer treatment: validation in the community-based CaPSURE cohort of a predictive model developed in PROST-QA. JAMA. 2011 Sep 21;306(11):1205–14. doi: 10.1001/jama.2011.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang P, Szymanski KM, Dunn RL, et al. Expanded prostate cancer index composite for clinical practice: development and validation of a practical health related quality of life instrument for use in the routine clinical care of patients with prostate cancer. J Urol. 2011 Sep;186(3):865–72. doi: 10.1016/j.juro.2011.04.085. Epub 2011 Jul 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanda MG, Dunn RL, Michalski J, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008;358(12):1250–61. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- 9.Cohen J. Statistical power analysis for the behavioral sciences. Academic Press; New York: 1977. [Google Scholar]
- 10.Bland MJ, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–10. [PubMed] [Google Scholar]
- 11.Barry MJ, Fowler FJ, Jr, O'Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committeee of the American Urological Association. J Urol. 1992;148(5):1549–57. doi: 10.1016/s0022-5347(17)36966-5. [DOI] [PubMed] [Google Scholar]
- 12.American Urological Association Education and Research, Inc. Guideline on the management of benign prostatic hyperplasia (BPH) Linthicum (MD): American Urological Association Education and Research, Inc.; 2010. p. 34. [Google Scholar]
- 13.Meigs JB, Barry MJ, Giovannucci E, et al. Incidence rates and risk factors for acute urinary retention: the health professionals follow-up study. J Urol. 1999 Aug;162(2):376–82. [PubMed] [Google Scholar]
- 14.Lewicky-Gaupp C, Wei JT, Delancey JO, et al. The association of Incontinence Symptom Index scores with urethral function and support. Am J Obstet Gynecol. 2008;199:680.e681–680.e685. doi: 10.1016/j.ajog.2008.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellison JS, He C, Wood DP. Stratification of postprostatectomy urinary function using expanded prostate cancer index composite. Urology. 2013 Jan;81(1):56–60. doi: 10.1016/j.urology.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 16.Schroeck FR, Donatucci CF, Smathers EC, et al. Defining potency: a comparison of the International Index of Erectile Function short version and the Expanded Prostate Cancer Index Composite. Cancer. 2008 Nov 15;113(10):2687–94. doi: 10.1002/cncr.23887. [DOI] [PubMed] [Google Scholar]
- 17.Hedgepeth RC, Labo J, Zhang L, et al. Expanded Prostate Cancer Index Composite versus Incontinence Symptom Index and Sexual Health Inventory for Men to measure functional outcomes after prostatectomy. J Urol. 2009 Jul;182(1):221–7. doi: 10.1016/j.juro.2009.02.155. discussion 227-8. Epub 2009 May 17. [DOI] [PubMed] [Google Scholar]
- 18.Wheat JC, Hedgepeth RC, He C, et al. Clinical interpretation of the Expanded Prostate Cancer Index Composite-Short Form sexual summary score. J Urol. 2009 Dec;182(6):2844–9. doi: 10.1016/j.juro.2009.08.088. Epub 2009 Oct 17. [DOI] [PubMed] [Google Scholar]
- 19.Abdollah F, Sun M, Suardi N, et al. Prediction of functional outcomes after nerve-sparing radical prostatectomy: results of conditional survival analyses. Eur Urol. 2012 Jul;62(1):42–52. doi: 10.1016/j.eururo.2012.02.057. Epub 2012 Mar 8. [DOI] [PubMed] [Google Scholar]
- 20.Cooperberg MR. To predict the future, consider the present as well as the past. Eur Urol. 2012 Jul;62(1):53–4. doi: 10.1016/j.eururo.2012.04.018. Epub 2012 Apr 14. [DOI] [PubMed] [Google Scholar]
- 21.Wyrwich KW, Wolinsky FD. Identifying meaningful intra-individual change standards for health-related quality of life measures. J Eval Clin Pract. 2000 Feb;6(1):39–49. doi: 10.1046/j.1365-2753.2000.00238.x. [DOI] [PubMed] [Google Scholar]
- 22.Dunn R, Sanda M, Wei J. Minimally Important Difference for the Expanded Prostate Cancer Index Composite (EPIC) International Society for Quality of Life; New Orleans, LA: 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1: Minimally important differences in EPIC-CP by treatment group*
Supplemental Table 2: Model predicting of Functional Erections 2 years after Radical Prostatectomy using pre-treatment a) EPIC-CP Sexual Score and b) EPIC-26 Sexual Score*


