Abstract
Background/Purpose
Pediatric obesity is an important public health concern, yet its effect on surgical outcomes is poorly understood. The purpose of this study was to determine if age and gender-specific body mass index (BMI) percentile influences complications and hospital resource utilization following pediatric gastrointestinal surgeries.
Methods
Patients aged age ≥2 to <18 years who underwent appendectomy or other gastrointestinal operations were identified in the 2012 - 2013 Pediatric National Surgical Quality Improvement Program datasets. Age- and gender-specific pediatric BMI percentiles were calculated. Patients who underwent appendectomy (n=9,606) and those undergoing all other intestinal operations (n=2,664) were evaluated as separate cohorts.
Results
In the appendectomy cohort, frequency of any complication increased with BMI category (normal-weight 4.5%, overweight 5.3%, obese 5.7%, morbidly obese 7.3%, overall 5.0%, p = 0.014). In multivariable analysis, there was a quadratic association between BMI percentile and increased frequency of superficial incisional infection, unplanned tracheal intubation, and longer operative duration. In the intestinal surgery cohort, BMI percentile was not a predictor of any individual complication or any measure of hospital utilization.
Conclusions
Age- and gender-specific BMI percentile was associated with increased risk of complications and longer operative duration in patients undergoing appendectomy but not other intestinal operations.
Keywords: Obesity, Pediatric, Appendicitis, Gastrointestinal surgery
1.1 Background
Over one third of youth are obese, and obese children are known to be at increased risk for chronic medical problems including hypertension, dyslipidemia, insulin resistance and diabetes, nonalcoholic fatty liver disease, obstructive sleep apnea, asthma, musculoskeletal complaints and psychological problems[1-4].
In adults, obesity is a well-recognized risk factor associated with chronic diseases and certain perioperative complications. From an anesthesia perspective, the obese habitus is associated with difficult airways, and difficulty visualizing anatomic landmarks makes line placements and regional anesthetics challenging[5]. Obese adults are at higher risk for aspiration due to elevated gastric residual volumes, and drug distributions may be more difficult to predict[5]. From a surgical perspective, studies have consistently shown an increase in wound complications including infections in multiple types of non-bariatric abdominal surgeries [5-14]. Data regarding other complications are more controversial: some studies have shown obesity to be associated with wound dehiscence[15, 16] and other nosocomial infections[5, 17], while others have not shown obesity to be a risk factor for other major perioperative complications[7, 9, 10]. In fact, moderate obesity was even protective against mortality in some studies[10, 13].
The literature regarding obesity in pediatric abdominal surgery is sparse in comparison to the adult literature. A single-institution study of 282 children requiring appendectomy found that obese children required longer operative times, longer hospital stays, and those with perforated appendicitis had increased risk of postoperative infections[18]. A small meta-analysis of 3 studies analyzed 220 pediatric patients undergoing laparoscopic appendectomy for perforated appendicitis, and identified that obese patients had longer operative times and increased abscess rate[19]. A study of 312 children requiring laparoscopic cholecystectomy, however, did not find any significant differences in outcomes with obesity[20]. In pediatric urologic surgery patients undergoing either genital or abdominal procedures, obese children had higher rates of overall and wound complications[21]. Recently, Michailidou studied complications following urgent or emergent laparoscopic appendectomy in 2,812 pediatric patients in the Pediatric National Surgical Quality Improvement Program dataset[22]. When comparing obese to non-obese patients, they demonstrated no difference in complications albeit longer operative duration for obese patients.
The existing pediatric literature dichotomizes obesity, which may overlook important differences between moderately obese and morbidly obese patients. Additionally, since overall complication rates in children are low, larger studies are needed to detect any potential differences. Given that the existing literature includes mostly small studies, assesses a narrow range of operations, and has inconsistent results, further investigation is warranted. Understanding risk factors for complications is important for quality assessment and benchmarking from a health systems perspective, and is also critical for informed consent and patient counseling. Many providers anecdotally associate obesity with higher perioperative risk, but at present there is not solid quantitative data to support this. Identifying patients at high risk for specific complications allows providers to be more vigilant about other mitigating efforts, such as ensuring appropriate antibiotic prophylaxis for a patient at high risk for surgical site infections. These behaviors are important for patient care, and are also becoming increasingly relevant in the context of the shift toward value-based purchasing for health care services.
In the present study, we examined the impact of age- and gender-specific body mass index (BMI) percentile on outcomes and hospital resource utilization following pediatric gastrointestinal surgeries involving the small bowel, colon and rectum. We hypothesized that increasing age- and gender-specific BMI percentile would confer a higher rate of perioperative complications, and that care of these patients may necessitate more hospital resources.
1.2 Methods
1.2.1 Patient selection and body mass index assessment
After the Seattle Children's Hospital Institutional Review Board approved this study as exempt, we obtained and queried the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) Pediatric Participant Use Data Files from 2012 and 2013. This database includes patients under18 years of age who underwent major inpatient or outpatient surgical procedures. Trauma and transplant cases are excluded. For high-volume contributing hospitals, the first 35 consecutive cases meeting inclusion criteria within 8-day cycles were included. Regular audits are performed to ensure data quality. The 2012 dataset contains 51,008 cases submitted from 50 sites, and the 2013 dataset contains 63,387 cases submitted from 56 sites. Hospital types eligible for inclusion in NSQIP-Pediatric include freestanding general and specialty children's hospitals, children's hospitals within larger hospitals, and general hospitals with pediatric wings.
Current Procedural Terminology (CPT) codes were chosen to include only patients undergoing operations on the small bowel, colon or rectum. Bariatric and feeding tube operations were excluded, as well as other cases such as adhesiolysis not involving resection, entrectomy, or anastomosis. Laparoscopic operations were determined based on procedure codes. For patients in the intestinal surgery cohort with multiple concurrent procedures, cases were coded as laparoscopic if at least one of the procedures was a laparoscopic abdominal procedure.
NSQIP-Pediatric includes binary variables for complications occurring within 30 days of surgery, which were assessed individually and in composite. Table 3 shows key complications assessed (the complete list is found in the tables in the supplemental material); the term “any complication” refers to the presence of at least one of these identified complications. The dataset also includes 30-day measures of hospital resource utilization including anesthesia time, operative duration, ventilator days, length of stay, readmission and reoperative data, and work Relative Value Units (RVUs), which were also assessed.
Table 3.
Complications and hospital utilization after appendectomy.
| Overall (n = 9,606) | Normal (n = 5,839) | Overweight (n = 1,727) | Obese (n = 1,572) | Morbidly Obese (n = 468) | P value | |
|---|---|---|---|---|---|---|
| Any complication | 4.96 % | 4.47 % | 5.27 % | 5.73 % | 7.26 % | 0.01a |
| Death within 30 days | 0.01 % | 0.02 % | 0.00 % | 0.00 % | 0.00 % | 1.00b |
| Specific complications: | ||||||
| Superficial incisional infection | 1.24 % | 1.01 % | 1.39 % | 1.59 % | 2.35 % | 0.03a |
| Deep incisional infection | 0.23 % | 0.24 % | 0.17 % | 0.19 % | 0.43 % | 0.67b |
| Organ space infection | 2.68 % | 2.43 % | 2.95 % | 3.05 % | 3.42 % | 0.30a |
| Wound disruption/dehiscence | 0.18 % | 0.17 % | 0.12 % | 0.25 % | 0.21 % | 0.70b |
| Pneumonia | 0.32 % | 0.29 % | 0.35 % | 0.25 % | 0.85 % | 0.22b |
| Unplanned intubation | 0.08 % | 0.03 % | 0.06 % | 0.32 % | 0.00 % | 0.02b |
| Acute renal failure | 0.03 % | 0.00 % | 0.12 % | 0.06 % | 0.00 % | 0.07b |
| Urinary tract infection | 0.15 % | 0.17 % | 0.06 % | 0.19 % | 0.00 % | 0.70b |
| Seizure | 0.03 % | 0.00 % | 0.12 % | 0.00 % | 0.00 % | 0.03b |
| Thromboembolic event requiring treatment | 0.02 % | 0.02 % | 0.06 % | 0.00 % | 0.00 % | 0.63b |
| Central line associated bloodstream infection | 0.01 % | 0.00 % | 0.00 % | 0.06 % | 0.00 % | 0.21b |
| Measures of hospital utilization | ||||||
| Operation time, minutes (SD) | 46.60 (26.95) | 45.56 (27.01) | 46.84 (27.54) | 49.00 (26.34) | 50.32 (25.25) | <0.001c |
| Mean length of stay, days (SD) | 2.61 (4.03) | 2.49 (3.69) | 2.73 (4.81) | 2.87 (4.48) | 2.82 (3.17) | 0.002c |
| Readmissions | 4.30 % | 4.52 % | 3.76 % | 3.69 % | 5.56 % | 0.16a |
| Mean work RVU (SD) | 9.78 (1.16) | 9.78 (1.15) | 9.76 (1.14) | 9.76 (1.17) | 9.88 (1.35) | 0.28c |
Footnotes: Statistical tests are indicated in the column after the p value
represents chi2
represents Fisher exact
represents ANOVA.
We included patients aged ≥2 to <18 years in this study. This range was chosen because the Center for Disease Control's (CDC) age and gender-specific BMIs begin at age 2 years. Other norms such as length-for-age and weight-for-age are available for younger children, but these are less appropriate for assessing obesity. The CDC's 2000 gender-specific growth chart tables and publically-available SAS program[23] were used to calculate age- and gender-specific pediatric BMI percentiles. We excluded cases with missing height and weight values rather than imputing them, given that there were limited variables available for imputation calculations and that these parameters were of primary interest. Weight data was missing for <0.5% of patients and height data was missing for 27% of patients; however, analysis comparing patients with full BMI data to those with weight data only demonstrated minimal, <5% differences. The CDC algorithm flags biologically implausible BMI percentiles; these patients were excluded from further analysis under the assumption that they were either very significant outliers or represented inaccuracies in the dataset. Given that our intent was to evaluate implications of obesity, we excluded patients <5th percentile for BMI.
12,270 patients met our inclusion criteria; of them, 9606 (78%) underwent either laparoscopic or open appendectomy and 2,664 underwent other intestinal operations. Given the large proportion of patients undergoing a single operation, we sought to determine whether the appendectomy and other intestinal surgery subsets should be pooled or separated for analysis of outcomes by comparing patient characteristics and pre-existing conditions (Tables 1 and 2). Given that the populations had different BMI distributions and extensive, statistically-significant differences in most parameters assessed (Tables 1 and 2), we therefore analyzed outcomes for appendectomy patients separately from other intestinal surgery patients.
Table 1.
Characteristics of the study populations
| Appendectomy (n = 9,606) | Intestinal operations (n = 2,264) | Combined population (n=12,270) | P value | |
|---|---|---|---|---|
| Mean Age (SD) | 11.21 (3.66) | 10.55 (4.79) | 11.07 (3.94) | <0.001a |
| % Female | 40.7% | 46.06 | 41.87% | <0.001b |
| % Hispanic | 22.5% | 8.63% | 19.50% | <0.001b |
| Race | <0.001b | |||
| White | 76.99% | 77.18% | 77.03% | |
| Black/African American | 9.10% | 11.64% | 9.65% | |
| Asian | 2.19% | 2.67% | 2.29% | |
| American Indian, Alaska Native, Native Hawaiian, Pacific Islander | 0.51% | 0.60% | 0.53% | |
| Discharged home | 99.67% | 98.24% | 99.36% | <0.001b |
| General anesthesia | 99.90 | 99.90% | 99.85% | 0.019b |
| Case type | <0.001b | |||
| Elective | 12.42% | 45.53% | 19.61% | |
| Emergent | 60.88% | 38.21% | 55.96% | |
| Urgent | 26.70% | 16.25% | 24.43% | |
| Laparoscopic (or combined) | 90.12% | 25.79% | 76.15% | <0.001b |
| ASA Class | <0.001 b | |||
| 1 | 50.69% | 37.73% | 47.87% | |
| 2 | 43.87% | 45.27% | 44.17% | |
| 3 | 5.09% | 14.79% | 7.20% | |
| 4 | 0.16% | 1.80%% | 0.51% | |
| 5 | 0% | 0.23 | 0.05% | |
| Wound classification | <0.001b | |||
| Clean | 2.18% | 14.94% | 4.95% | |
| Clean/contaminated | 27.85% | 44.89% | 31.55% | |
| Contaminated | 45.74% | 25.56% | 41.36% | |
| Dirty/infected | 24.23% | 14.60% | 22.14% |
Footnotes: Statistical tests were performed to evaluate for differences between the appendectomy subgroup and the intestinal operation subgroup. The test used is indicated in the column after the p value
represents t-test
represents chi2.
Table 2.
Preoperative comorbidities in study populations
| Appendectomy, % of population (n = 9,606) | Intestinal operations, % of population (n = 2,270) | Combined population (n=12,270) | P value | |
|---|---|---|---|---|
| Mean age- and sex-specific BMI percentile (SD) | 68.11 (28.01) | 59.6 (30.21) | 66.26 (28.71) | <0.001 |
| Chronic conditions - Any | 20.10% | 45.01% | 25.51% | <0.001 |
| Diabetes | 0.54% | 0.60% | 0.55% | 0.72 |
| History of prematurity | 2.69% | 8.82% | 4.02% | <0.001 |
| Asthma | 6.04% | 4.54% | 5.71% | 0.003 |
| Esophageal/gastric/intestinal disease | 6.80% | 15.54% | 8.70% | <0.001 |
| Biliary/liver/pancreatic disease | 0.19% | 6.23% | 1.50% | <0.001 |
| Cardiac anomaly or cardiac surgery | 1.29% | 5.52% | 2.21% | <0.001 |
| Impaired cognitive status | 1.37% | 4.39% | 2.03% | <0.001 |
| Structural CNS abnormality | 0.39% | 3.08% | 0.97% | <0.001 |
| Chronic immunosuppression | 0.39% | 1.09% | 0.54% | <0.001 |
| Bleeding or hematologic disorder | 1.06% | 3.64% | 1.62% | <0.001 |
| Congenital malformation | 2.29% | 20.01% | 6.14% | <0.001 |
| Malignancy (past or current) | 0.20% | 3.34% | 1.25% | <0.001 |
| Acute conditions - Any | 17.52% | 17.30% | 17.47% | 0.80 |
| Ventilator dependence within 48 hours | 0.03% | 1.88% | 0.43% | <0.001 |
| Acute renal failure | 0.04% | 0.38% | 0.11% | <0.001 |
| Steroid use within 30 days | 0.77% | 1.69% | 0.97% | <0.001 |
| Nutritional support at time of surgery | 0.30% | 4.95% | 1.31% | <0.001 |
| Sepsis or septic shock within 48h | 16.61% | 9.31% | 15.03% | <0.001 |
Footnotes: Chi2 tests were performed to evaluate for differences between the appendectomy subgroup and the intestinal operation subgroup. Comorbidities occurring in <2% of both subgroups are not shown unless clinically relevant although significant differences were present for many (tracheostomy, structural pulmonary/airway abnormalities, stroke, central nervous system tumor, seizure disorder, cerebral palsy, neuromuscular disorder, intraventricular hemorrhage, solid organ transplant, failure to thrive, supplemental oxygen at the time of surgery, dialysis within 2 weeks, coma longer than 24 hours, inotropic support at the time of surgery, cardiopulmonary resuscitation within 7 days, prior operation within 30 days, and chemotherapy or radiation within 30 days).
1.2.4 Univariate analysis
Descriptive statistics were performed to assess demographic characteristics and comorbidities for the overall population as well as the appendectomy and other intestinal surgery subgroups. The NSQIP-Pediatric dataset includes binary data on presence of conditions present preoperatively. These were divided into acute and chronic conditions by our research team for conceptualization, although the specific time course of diagnosis for individual patients is not available. For appendectomy patients, a marker for severe appendicitis was created based on both diagnosis and procedure codes, and included patients with documented perforation or diagnosis of appendicitis with intraabdominal abscess.
For categorical analysis, the CDC's established age- and gender-specific pediatric categories were adapted: normal weight for BMI 5th to less than the 85th percentile, overweight if 85th to less than the 95th percentile, and obese if 95th percentile or greater. An additional category of morbid obesity was applied to patients with BMIs greater than the 99th percentile (the obese category was adjusted to include ≥95th to ≤99th percentiles). Rates of complications within each BMI category were calculated, and significance assessed using either Pearson's Chi Square tests or Fisher's Exact test depending on observation count. The association of BMI category with temporal measures such as operative time and hospital length of stay were assessed using ANOVA.
1.2.5 Multivariable analysis
Multivariable logistic and linear regression analyses were constructed individually for each cohort to account for the effect of demographic factors and comorbidities on the association between BMI percentile and outcomes. Only variables with more than 20 observations were considered in the models. Variables were included if they caused at least a 10% change in the models or if clinically important. BMI percentile was used as a continuous variable.
For the appendectomy cohort, a quadratic association between BMI percentile and resulting complications was most predictive of the true relationship after evaluating multiple models. The final model to predict complications included the square of age and gender-specific BMI percentile, age, sex, Hispanic ethnicity, race, ASA class, presence of complicated appendicitis, wound class, presence of diabetes, laparoscopy vs open, preoperative sepsis or septic shock, gastrointestinal disease, hematologic disorder, congenital malformation, preoperative nutritional support, impaired cognitive status, cardiac anomaly and history of malignancy.
For the intestinal surgery cohort, a linear relationship between BMI percentile and resulting complications was most predictive of the true relationship after evaluating multiple models. The final model to predict complications include BMI percentile, age, sex, Hispanic ethnicity, race, ASA class, wound class, presence of diabetes, presence of asthma, laparoscopy vs open, preoperative oxygen requirement, recent steroid use, history of prematurity, esophageal/gastric/intestinal disease, cardiac risk factors, preoperative nutritional support, history of congenital malformation and history of malignancy.
1.2.6 Statistical software
Statistical analysis was performed using Stata version 12 (StataCorp LP, College Station, TX). The CDC algorithm was applied using SAS (SAS Institute, Cary, NC). P values of <0.05 were considered statistically significant.
1.3 Results
1.3.1 Descriptive data
Data from 9,606 patients were analyzed in the appendectomy cohort, and 2,664 patients were analyzed in the intestinal operation cohort. Descriptive statistics were tabulated for each population, as shown in Table 1. The mean age for the appendectomy patients was 11.2 years (SD 3.7) and mean BMI percentile was 68.1 (SD 28.0). Mean age for intestinal surgery patients was 10.5 years (SD 4.8) and mean BMI percentile was 59.6 (SD 30.2). Ninety percent of appendectomies and 26% of the other intestinal operations were performed laparoscopically.
Comorbidities and pre-existing conditions for the appendectomy patients and intestinal surgery patients are listed in Table 2. One fifth of the appendectomy cohort had a chronic condition, most commonly esophageal, gastric or intestinal disease, followed by asthma. In contrast, 45% of the other cohort had chronic conditions, most commonly a congenital malformation. Acute conditions occurred in approximately 17% of each cohort, most commonly sepsis or septic shock.
1.3.2 Univariate analysis - appendectomy
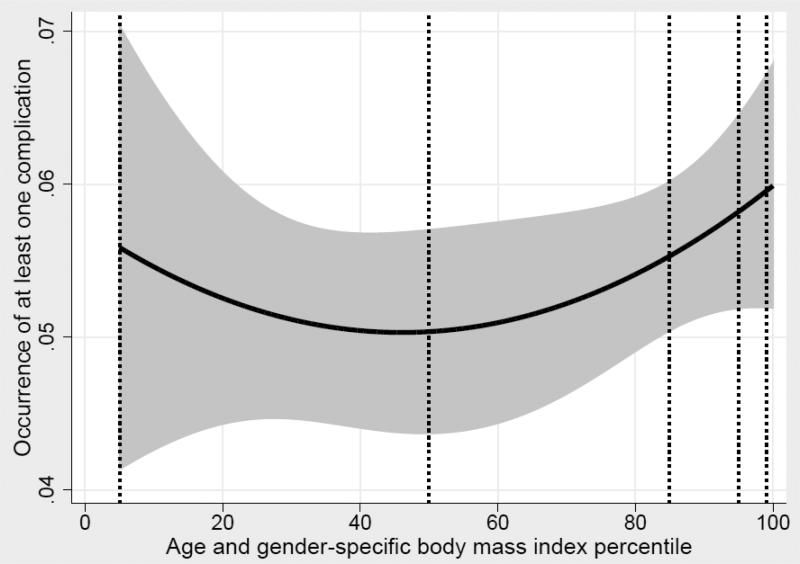
The overall frequency of any complication was 5.0%; however, this increased monotonically with BMI: 4.5% in normal-weight, 5.3% in overweight, 5.7% in obese, and 7.3% in morbidly obese patients (p = 0.01). This relationship was further explored with BMI percentile as a continuous variable using logistic regression. The quadratic line of best fit is shown in Figure 1, and the association between any complication and the square of BMI percentile was statistically significant with p = 0.03.
Figure 1. Association between BMI percentile as a continuous variable, and occurrence of any complication among appendectomy patients.
A quadratic line of best fit was applied and is demonstrated, with 95% confidence intervals denoted by the shaded gray region. The association between any complication and the square of BMI percentile is statistically significant, with a P value of 0.03. Vertical dashed lines denote the 50th percentile as well as the BMI category cutoff points used in this study of 5th percentile, 85th percentile, 95th percentile and 99th percentile.
Of the complications evaluated, three were individually significant in the univariate model: superficial incisional infection, unplanned intubation and postoperative seizure. The overall frequency of superficial incisional infection was 1.24% and increased with BMI category: 1.0% in normal weight, 1.4% in overweight, 1.6% in obese, and 2.4% in morbidly obese (p = 0.03). Unplanned intubation occurred in 0.1% overall; subdivided rates were 0.03% among patients with normal weight, 0.1% among overweight, 0.3 among obese, and 0% (no events) in morbidly obese patients (p = 0.02). There was also a statistically significant association between BMI category and postoperative seizure, albeit the overall rate of seizure was 0.03% and the only observations were for patients in the overweight category. There was no difference between BMI categories for 30-day mortality or other individual complications (Table 3 demonstrates key outcomes; full data is available in the supplemental material).
Age and sex-specific BMI category was associated with significantly longer hospital length of stay and greater operative duration, as also shown in Table 3 and the supplemental material. There was no difference between BMI categories for anesthesia duration, days of mechanical ventilation, readmission rate, reoperative rate or work RVUs.
1.3.3 Multivariable analysis – appendectomy
In the multivariable model described above, the square of age and sex-specific BMI percentile was a statistically significant predictor of complication (p = 0.04). The area under the Receiver Operating Characteristic (ROC) curve for the overall model was 0.76.
Using this multivariable model, a series of comparisons were created to assess the odds ratio for any complication as BMI percentile increased. Using the 50th percentile for BMI as a reference point, the odds ratio for occurrence of any complication increased with rising BMI percentile (p = 0.04). Patients in the 85th percentile for BMI were 1.15 times more likely to have any complication than patients in the 50th percentile for BMI (95% CI 1.01 - 1.32); likewise, the odds ratio for patients in the 95th percentile relative to the 50th percentile was 1.21 (95% CI 1.01 - 1.46), and the odds ratio for patients in the 99th percentile relative to the 50th percentile was 1.24 (95% CI 1.01 - 1.53).
We also analyzed individual complications using the same covariates in the multivariable model. The square of BMI percentile remained a statistically significant predictor of superficial surgical site infection (p = 0.01) and unplanned intubation (p = 0.04), as well as longer operative duration (Table 4). Increased BMI percentile was associated with increased work RVU in multivariable analysis (p = 0.02). The remaining complications and outcomes evaluated in the univariate analysis remained non-significant on multivariable analysis.
Table 4.
Multivariable analysis of complications and hospital utilization measures after appendectomy.
| BMI 85th percentile | BMI 95th percentile | BMI 99th percentile | P value | |
|---|---|---|---|---|
| Any complication | 1.15 (1.01 to 1.32) | 1.21 (1.01 to 1.46) | 1.24 (1.01 to 1.53) | 0.04 |
| Superficial incisional infection | 1.43 (1.09 to 1.89) | 1.64 (1.13 to 2.39) | 1.74 (1.15 to 2.65) | 0.01 |
| Unplanned intubation | 4.15 (1.06 to 16.18) | 7.13 (1.09 to 46.71) | 9.01 (1.10 to 73.79) | 0.04 |
| Operative duration | 1.63 (0.91 to 2.36) | 2.26 (1.26 to 3.25) | 2.52 (1.41 to 3.64) | <0.001 |
| Work RVU | 0.02 (0.003 to 0.03) | 0.02 (0.004 to 0.04) | 0.03 (0.004 to 0.05) | 0.02 |
Footnote: All variables were tested, but the table shows only those which reached statistical significance.
1.3.4 Univariate analysis – intestinal operations
For patients who underwent other intestinal operations, the overall frequency of any complication was 7.2%, without significant difference between BMI categories (normal weight 7.1%, overweight 7.9%, obese 7.6%, morbidly obese 5.5%, p = 0.82). Logistic regression analysis assessing the association between BMI percentile as a continuous variable and any complication was performed and similarly, did not show a significant association (p = 0.94). The only complication that had a statistically significant association with BMI category was wound dehiscence, with a frequency of 0.1% in normal weight, 1.3% in overweight, 0.4% in obese, and 0.0% in morbidly obese patients (p = 0.01). There were no significant differences in any other complication categories. For measures of hospital utilization, BMI category was associated with longer anesthesia duration and longer operative duration, but no difference in other parameters (Table 5 demonstrates key outcomes; full data is available in the supplemental material).
Table 5.
Complications and hospital utilization after intestinal operation.
| Overall (n = 2,664) | Normal (n = 1,873) | Overweight (n = 405) | Obese (n = 276) | Morbidly Obese (n = 110) | P value | |
|---|---|---|---|---|---|---|
| Any complication | 7.17% | 7.05% | 7.90% | 7.61% | 5.45% | 0.82a |
| Death within 30 days | 0.53% | 0.59% | 0.25% | 0.36% | 0.91% | 0.68b |
| Specific complications: | ||||||
| Superficial incisional infection | 1.09% | 1.28% | 0.25% | 1.45% | 0.00% | 0.19b |
| Deep incisional infection | 0.15% | 0.11% | 0.25% | 0.36% | 0.00% | 0.40b |
| Organ space infection | 1.46% | 1.44% | 1.73% | 1.45% | 0.91% | 0.97b |
| Wound disruption/dehiscence | 0.30% | 0.11% | 1.23% | 0.36% | 0.00% | 0.01b |
| Pneumonia | 0.15% | 0.21% | 0.00% | 0.00% | 0.00% | 1.00b |
| Unplanned intubation | 0.41% | 0.27% | 0.74% | 0.72% | 0.91% | 0.14b |
| Acute renal failure | 0.08% | 0.05% | 0.25% | 0.00% | 0.00% | 0.51b |
| Urinary tract infection | 0.90% | 0.91% | 0.49% | 1.45% | 0.91% | 0.56b |
| Thromboembolic event requiring treatment | 0.08% | 0.05% | 0.25% | 0.00% | 0.00% | 0.51b |
| Central line associated bloodstream infection | 0.15% | 0.16% | 0.25% | 0.00% | 0.00% | 0.76b |
| Measures of hospital utilization | ||||||
| Mean duration of anesthesia, minutes (SD) | 132.03 (97.98) | 127.70 (91.77) | 141.58 (114.94) | 144.58 (110.80) | 139.05 (94.19) | 0.01c |
| Operation time, minutes (SD) | 83.08 (80.05) | 79.27 (74.22) | 92.38 (95.65) | 92.34 (91.47) | 90.61 (78.03) | 0.002c |
| Mean mechanical ventilation days (SD) | 0.31 (2.27) | 0.32 (2.25) | 0.27 (2.33) | 0.42 (2.59) | 0.20 (1.24) | 0.80c |
| Mean length of stay, days (SD) | 4.45 (10.31) | 4.53 (10.84) | 4.80 (10.47) | 3.98 (7.58) | 3.15 (4.88) | 0.41c |
| Readmissions | 6.08% | 6.19% | 6.17% | 5.43% | 5.45% | 0.96a |
| Mean work RVU (SD) | 22.19 (8.15) | 22.26 (7.93) | 22.08 (9.05) | 22.02 (8.73) | 21.82 (6.73) | 0.91c |
Footnotes: Statistical tests are indicated in the column after the p value
represents chi2
represents Fisher exact
represents ANOVA.
1.3.5 Multivariable analysis – intestinal operations
In contrast to the appendectomy model, BMI percentile, not square of BMI percentile, represented best fit. BMI percentile was not a significant predictor of complication (OR 1.002; 95% CI 0.996 - 1.007). As in univariate analysis, BMI percentile was not a significant predictor of any individual complication or any measure of hospital utilization.
1.4 Discussion
We studied the impact of BMI percentile on complications and measures of hospital utilization in pediatric patients undergoing gastrointestinal surgeries. Patients were divided into children undergoing appendectomy and those undergoing other small bowel, colon or rectal operations given statistically-significant differences between the subgroups in demographic characteristics, comorbidities and BMI distributions. BMI percentile was predictive of complications, operative duration and work RVU in appendectomy patients, but was not predictive of any outcome measure in intestinal surgery patients.
In appendectomy patients, we observed that higher BMI percentile increased the odds of incurring any complication, superficial incisional infection, or unplanned intubation. In fact, the square of BMI percentile was the best predictor of complications, indicating that the risk of these complications increases in the setting of severe obesity. In multivariable analysis, appendectomy patients in the 99th percentile for BMI had a 1.24 times the likelihood of incurring any complication relative to the 50th percentile, and 1.75 times the likelihood of incurring superficial incisional infection, and 9 times the likelihood of unplanned intubation. Our data for deep incisional infections and for organ-space infections trended toward increased rates with higher BMI percentile; however, these were rare and differences were not significant. While complications are uncommon in this population, awareness of these risks may allow providers to mitigate them.
With respect to wound infections, our appendectomy data are consistent with two smaller prior studies showing increased infectious complications in obese children[18, 19], as well as with extensive data in adults[5-14]. More careful consideration of appropriate antibiotic prophylaxis is warranted, particularly given that dosing may be different in obese children. Subclinical insulin resistance may underlie the association between BMI percentile and infectious complications [24]; thus, testing of high-risk individuals may be warranted. Likewise, counseling of families regarding early evidence of infection may reduce the subsequent consequences of wound infections.
Unplanned tracheal intubations were rare, but there was a statistically significant association with high BMI percentile on univariate and multivariable regression analysis despite no events in the morbidly obese category. We examined this question because other studies have also demonstrated that obese patients have increased airway complications such as desaturation and laryngospasm following oropharyngeal or non-cardiac surgeries[25-28]. Our data supports these findings, despite the rarity of this event in our data. We also observed a significant increase in operative time, which is consistent with the existing literature[18, 19, 22], and may indicate technical challenges associated with abdominal wall depth and intra-abdominal adiposity.
We believe that there are two primary reasons why our finding that BMI percentile was associated with complications of any type differ from the results observed by Michailidou using the same NSQIP Pediatric dataset[22]. First, we included open appendectomy, elective cases, and two years of data rather than one (9,606 patients compared with 2,812) to increase our sample size and were, therefore, powered to detect different outcomes. Second, the Michailidou study categorized patients dichotomously as obese or not-obese, whereas our study utilized BMI both as a continuous variable and in finer classifications. The non-linear (quadratic) relationship between BMI and complications suggests that a single arbitrary cutoff is not appropriate to capture differences in risk of complications.
It is notable that the quadratic regression line between BMI percentile and occurrence of complication in appendectomy patients demonstrated in Figure 1 demonstrates an increased frequency of complication in lower BMI ranges. While our study excluded patients below the 5th percentile for BMI and the 95% confidence interval widens at low BMIs, this data is nonetheless consistent with existing literature suggesting that adults and children with low BMI are also at risk for complication.[10]. Malnutrition is of particular relevance to patients requiring intestinal surgeries; thus, our multivariable models did control for patients requiring preoperative nutritional support and we excluded operations for feeding tubes.
Among the patients who underwent intestinal surgeries, there was no significant difference in complication frequency as BMI percentile increased. In the multivariable model, significant predictors of complications included ASA class, wound class, preoperative oxygen requirement, preoperative steroid use, history of cardiac abnormalities, congenital malformations, and malignancy. The intestinal surgery cohort had a high rate of preexisting conditions, including congenital malformations in 20%; thus, it appears that these conditions had a much greater impact on outcomes than did BMI percentile. Indeed, complication frequency overall was low, which may also be related to the concentration of pediatric expertise in the hospitals within our study, as those contributing to the Pediatric NSQIP dataset are mostly large, free-standing hospitals and major pediatric centers.
Our study presents the largest evaluation of pediatric obesity in the context of appendectomy, and the only such evaluation for intestinal operations. We were limited by some missing anthropomorphic data in the dataset, with a low rate of missing weight and a moderate rate of missing height. Comparative analysis showed only minor differences in demographics and comorbidities between patients for whom this was missing or not; however, it is possible that this biased our results. Second, although this is the largest study in the literature at present, complications occur at low rates in children and so an even larger sample size would better capture any potential true differences. This is particularly relevant for the intestinal surgery cohort, who had very low rates of complications but relatively high rates of comorbidities which may impact analysis. An even larger sample size may also reduce the variability between subgroups that we observed and enable a pooled analysis of more surgery types that would expand the generalizability.
1.5 Conclusions
Increasing age- and gender-specific BMI percentile was associated with increased risk of any complication, superficial incisional infection, unplanned intubation and longer operative duration in patients undergoing appendectomy. BMI percentile was not associated with complications or measures of hospital utilization in patients undergoing other intestinal operations.
Supplementary Material
Acknowledgements
Funding support for this study was from the National Institute of Health, Institute of Child Health and Human Development (2T32HD057822-06; Drs. Frederick Rivara and Monica Vavilala).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CLCM, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daniels SR. Complications of obesity in children and adolescents. International journal of obesity. 2009;33(Suppl 1):S60–65. doi: 10.1038/ijo.2009.20. [DOI] [PubMed] [Google Scholar]
- 3.Reilly JJME, McDowell JC, Hacking B, Alexander D, Stewart L, Kelnar CJ. Health consequences of obesity. Arch Dis Child. 88:2003. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paulis WDSS, Koes BW, van Middelkoop M. Overweight and obesity are associated with musculoskeletal complaints as early as childhood: a systematic review. Obes Rev. 2014;15:52–67. doi: 10.1111/obr.12067. [DOI] [PubMed] [Google Scholar]
- 5.Choban PS, Flancbaum L. The impact of obesity on surgical outcomes: a review. Journal of the American College of Surgeons. 1997;185:593–603. doi: 10.1016/s1072-7515(97)00109-9. [DOI] [PubMed] [Google Scholar]
- 6.Chapman GW, Jr., Mailhes JB, Thompson HE. Morbidity in obese and nonobese patients following gynecologic surgery for cancer. Journal of the National Medical Association. 1988;80:417–420. [PMC free article] [PubMed] [Google Scholar]
- 7.Pemberton LB, Manax WG. Relationship of obesity to postoperative complications after cholecystectomy. American journal of surgery. 1971;121:87–90. doi: 10.1016/0002-9610(71)90081-x. [DOI] [PubMed] [Google Scholar]
- 8.Postlethwait RW, Johnson WD. Complications following surgery for duodenal ulcer in obese patients. Archives of surgery. 1972;105:438–440. doi: 10.1001/archsurg.1972.04180090043011. [DOI] [PubMed] [Google Scholar]
- 9.Dindo D, Muller MK, Weber M, et al. Obesity in general elective surgery. Lancet (London, England) 2003;361:2032–2035. doi: 10.1016/S0140-6736(03)13640-9. [DOI] [PubMed] [Google Scholar]
- 10.Mullen JT, Moorman DW, Davenport DL. The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Annals of surgery. 2009;250:166–172. doi: 10.1097/SLA.0b013e3181ad8935. [DOI] [PubMed] [Google Scholar]
- 11.Thelwall S, Harrington P, Sheridan E, et al. Impact of obesity on the risk of wound infection following surgery: results from a nationwide prospective multicentre cohort study in England. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2015;21:1008, e1001–1008. doi: 10.1016/j.cmi.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Frasson M, Granero-Castro P, Ramos Rodriguez JL, et al. Risk factors for anastomotic leak and postoperative morbidity and mortality after elective right colectomy for cancer: results from a prospective, multicentric study of 1102 patients. International journal of colorectal disease. 2015 doi: 10.1007/s00384-015-2376-6. [DOI] [PubMed] [Google Scholar]
- 13.Tjeertes EK, Hoeks SE, Beks SB, et al. Obesity--a risk factor for postoperative complications in general surgery? BMC anesthesiology. 2015;15:112. doi: 10.1186/s12871-015-0096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tuomi T, Pasanen A, Leminen A, et al. Incidence of and risk factors for surgical site infections in patients undergoing hysterectomy for endometrial carcinoma. Acta obstetricia et gynecologica Scandinavica. 2015 doi: 10.1111/aogs.12838. [DOI] [PubMed] [Google Scholar]
- 15.Foley K, Lee RB. Surgical complications of obese patients with endometrial carcinoma. Gynecologic oncology. 1990;39:171–174. doi: 10.1016/0090-8258(90)90427-m. [DOI] [PubMed] [Google Scholar]
- 16.Moghadamyeghaneh Z, Hanna MH, Carmichael JC, et al. Wound Disruption Following Colorectal Operations. World journal of surgery. 2015;39:2999–3007. doi: 10.1007/s00268-015-3208-0. [DOI] [PubMed] [Google Scholar]
- 17.Choban PS, Heckler R, Burge JC, et al. Increased incidence of nosocomial infections in obese surgical patients. The American surgeon. 1995;61:1001–1005. [PubMed] [Google Scholar]
- 18.Davies DA, Yanchar NL. Appendicitis in the obese child. Journal of pediatric surgery. 2007;42:857–861. doi: 10.1016/j.jpedsurg.2006.12.040. [DOI] [PubMed] [Google Scholar]
- 19.Garey CL, Laituri CA, Little DC, et al. Outcomes of perforated appendicitis in obese and nonobese children. Journal of pediatric surgery. 2011;46:2346–2348. doi: 10.1016/j.jpedsurg.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 20.Garey CL, Laituri CA, Keckler SJ, et al. Laparoscopic cholecystectomy in obese and non-obese children. The Journal of surgical research. 2010;163:299–302. doi: 10.1016/j.jss.2010.03.025. [DOI] [PubMed] [Google Scholar]
- 21.Kurtz MP, McNamara ER, Schaeffer AJ, et al. Association of BMI and pediatric urologic postoperative events: Results from pediatric NSQIP. Journal of pediatric urology. 2015 doi: 10.1016/j.jpurol.2015.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Michailidou M, Sacco Casamassima MG, Goldstein SD, et al. The impact of obesity on laparoscopic appendectomy: Results from the ACS National Surgical Quality Improvement Program pediatric database. Journal of pediatric surgery. 2015 doi: 10.1016/j.jpedsurg.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 23.Control CfD, editor. A SAS Program for the 2000 CDC Growth Charts (ages 0 to <20 years) Center for Disease Control, Center for Disease Control; 2015. [Google Scholar]
- 24.Ljungqvist O. Insulin resistance and outcomes in surgery. The Journal of clinical endocrinology and metabolism. 2010;95:4217–4219. doi: 10.1210/jc.2010-1525. [DOI] [PubMed] [Google Scholar]
- 25.Nafiu OO, Onyewuche V. Association of abdominal obesity in children with perioperative respiratory adverse events. Journal of perianesthesia nursing : official journal of the American Society of PeriAnesthesia Nurses / American Society of PeriAnesthesia Nurses. 2014;29:84–93. doi: 10.1016/j.jopan.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 26.Tait AR, Voepel-Lewis T, Burke C, et al. Incidence and risk factors for perioperative adverse respiratory events in children who are obese. Anesthesiology. 2008;108:375–380. doi: 10.1097/ALN.0b013e318164ca9b. [DOI] [PubMed] [Google Scholar]
- 27.Setzer N, Saade E. Childhood obesity and anesthetic morbidity. Paediatric anaesthesia. 2007;17:321–326. doi: 10.1111/j.1460-9592.2006.02128.x. [DOI] [PubMed] [Google Scholar]
- 28.Fung E, Cave D, Witmans M, et al. Postoperative respiratory complications and recovery in obese children following adenotonsillectomy for sleep-disordered breathing: a case-control study. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2010;142:898–905. doi: 10.1016/j.otohns.2010.02.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.