Abstract
We present an interesting case of congenital malrotation that was not discovered until adulthood. The patient presented with chronic, non-specific gastrointestinal symptoms which were subsequently alleviated with surgical correction of the congenital malrotation. Malrotation is less often considered in the adult patient and the associated presentation and imaging abnormalities of this case offer a valuable opportunity for thought and brief review.
Keywords: Congenital malrotation, Abdominal CT imaging, Intestinal malrotation
A 23-year-old woman presented with an 8-month history of intermittent epigastric abdominal pain with associated cramping, nausea, occasional vomiting and weight loss. Previous work-up was significant for helicobacter pylori antibody positivity, amidst replacement immunoglobulin therapy, resulting in two antibiotic treatment courses and chronic omeprazole. A previous abdominal upright anterior-posterior x-ray, obtained for the evaluation of scoliosis, demonstrated evidence of stool in the upper and lower left-sided abdominal quadrants not seen on the right (Fig. 1). Computer tomography (CT) of abdomen and pelvis with oral and intravenous (IV) contrast was performed due to symptom recurrence revealing anomalous left-sided colon, right-sided small bowel and oblique right-left inversion of the superior mesenteric artery (SMA) and the superior mesenteric vein (SMV) consistent with intestinal malrotation (Fig. 2). Our patient underwent surgical correction resulting in complete symptom cessation.
Figure 1.

Abdominal upright anterior-posterior x-ray demonstrating evidence of stool in the upper and lower left-sided abdominal quadrants not seen on the right.
Figure 2.
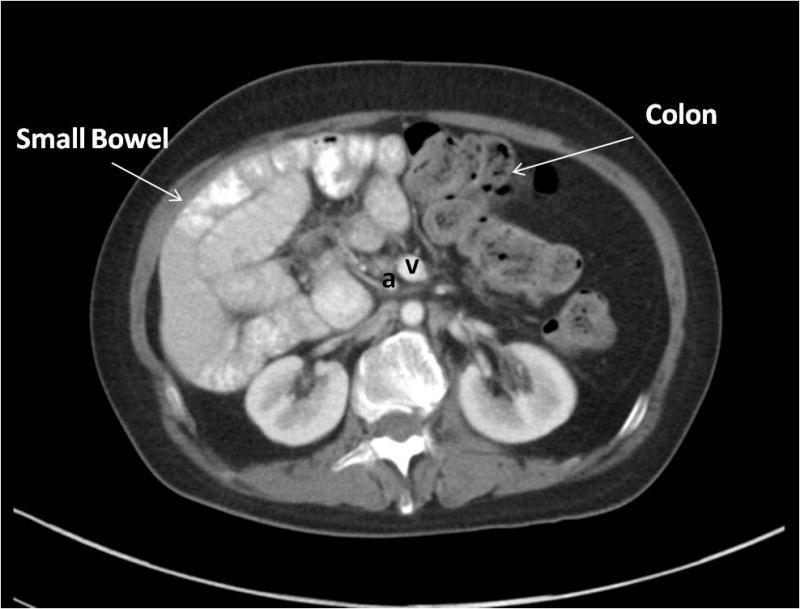
Abdominal axial CT with oral and IV contrast demonstrating right-sided small bowel and left-sided colon with oblique right-left inversion of the SMA (a) and SMV (v) consistent with congenital malrotation of the intestine.
Intestinal malrotation is any deviation from the normal embryonic 270° counter-clockwise rotation of the midgut resulting in the small bowel remaining on the right side of the abdomen and the large bowel on the left. Ladd’s bands, or congenital peritoneal fibrous bands, fix the duodenum and cecum to the abdominal wall leading to extrinsic obstruction or volvulus. Narrowing of the SMA increases the risk of ischemia and intestinal necrosis.1
Malrotation occurs in 1:500 live births with a majority of patients presenting before the age of one month, most commonly with vomiting.2 Diagnosis in adulthood is rare and most patients present with non-specific symptoms including chronic vomiting, intermittent, colicky abdominal pain, and diarrhea.3 Although less common, acute abdomen secondary to volvulus or internal herniation through Ladd’s bands remains possible.
The gold standard in diagnosing malrotation is cross sectional imaging with oral and IV contrast. Vertical positioning or right-left inversion of the SMA and SMV is indicative but not diagnostic of malrotation. Symptomatic malrotation requires curative surgical intervention, known as Ladd’s Procedure, which involves reduction of the volvulus if present, removal of Ladd’s bands and widening of the mesenteric base to prevent volvulus. Intestinal malrotation requires a high index of suspicion, especially in the adult patient, given the non-specific presentation and potentially catastrophic outcomes.
Acknowledgments
Study concept and design: JE, HS, CK, TH; Acquisition of data: CK, TH, AL; Analysis/interpretation: JE, CK, TH, AL; Drafting: JE; Critical revision: JE, HS, CK, TH, AL; Statistical analysis: N/A; Technical support: None; Supervision: CK.
Footnotes
Disclosures: The patient provided written consent to participate in a research protocol at the NIH. This submission was supported by the Intramural Research Programs of the NIDDK, NIAID, and CC NIH. None of the authors has any financial interest or conflict of interest related to this submission.
References
- 1.Dott N. Anomalies of intestinal rotation: their embryology and surgical aspects. Br J Surg. 1923;11:251–86. [Google Scholar]
- 2.Stewart DR, Colodny AL, Daggett WC. Malrotation of the bowel in infants and children: a 15 year review. Surgery. 1976;79(6):716–20. [PubMed] [Google Scholar]
- 3.Maxson RT, Franklin PA, Wagner CW. Malrotation in the older child: surgical management, treatment, and outcome. The American surgeon. 1995;61(2):135–8. [PubMed] [Google Scholar]


