Abstract
Background: One billion children live in war-affected regions of the world. We conducted the first cost-effectiveness analysis of an intervention for war-affected youth in sub-Saharan Africa, as well as a broader cost analysis.
Methods: The Youth Readiness Intervention (YRI) is a behavioural treatment for reducing functional impairment associated with psychological distress among war-affected young persons. A randomized controlled trial was conducted in Freetown, Sierra Leone, from July 2012 to July 2013. Participants (n = 436, aged 15–24) were randomized to YRI (n = 222) or care as usual (n = 214). Functional impairment was indexed by the World Health Organization Disability Assessment Scale; scores were converted to quality-adjusted life years (QALYs). An ‘ingredients approach’ estimated financial and economic costs, assuming a societal perspective. Incremental cost-effectiveness ratios (ICERs) were also expressed in terms of gains across dimensions of mental health and schooling. Secondary analyses explored whether intervention effects were largest among those worst-off (upper quartile) at baseline.
Results: Retention at 6-month follow-up was 85% (n = 371). The estimated economic cost of the intervention was $104 per participant. Functional impairment was lower among YRI recipients, compared with controls, following the intervention but not at 6-month follow-up, and yielded an ICER of $7260 per QALY gained. At 8-month follow-up, teachers’ interviews indicated that YRI recipients observed higher school enrolment [P < 0.001, odds ratio (OR) 8.9], denoting a cost of $431 per additional school year gained, as well as better school attendance (P = 0.007, OR 34.9) and performance (P = 0.03, effect size = −1.31). Secondary analyses indicated that the intervention was cost-effective among those worst-off at baseline, yielding an ICER of $3564 per QALY gained.
Conclusions: The YRI is not cost-effective at a willingness-to-pay threshold of three times average gross domestic product per capita. However, results indicate that the YRI translated into a range of benefits, such as improved school enrolment, not captured by cost-effectiveness analysis. We also outline areas for modification to improve cost-effectiveness in future trials.
Trial Registration: clinicaltrials.gov Identifier: RPCGA-YRI-21003
Keywords: Cost-effectiveness analysis, disability, mental health, school, sub-Saharan Africa, war
Key Messages
Over 1 billion children and adolescents live in war-affected regions of the world, representing a population at heightened risk of adverse health outcomes.
The Youth Readiness Intervention represents a novel group-based mental health intervention for war-affected young persons.
Based on the results of a randomized controlled trial conducted in Freetown, Sierra Leone, the Youth Readiness Intervention was estimated to cost $7260 per QALY gained and $431 per additional year of school retention.
Among those with the most salient mental health problems at baseline (upper quartile), the intervention was cost-effective—meaning that one QALY gained costs less than three times average GDP per capita.
Introduction
Mental disorders account for a larger burden of disease than HIV/AIDS and malaria combined (Murray et al. 2012). Half of all mental disorders develop by adolescence or early adulthood (Belfer 2008), and if left untreated these disorders persist throughout one’s adult life, resulting in severe disability and depreciated economic productivity (Lund et al. 2011). A recent report from the World Economic Forum estimated the cost of mental disorders to reach US $16 trillion dollars by 2030 (Bloom et al. 2011).
The consequences of mental disorders are exacerbated in the settings affected by war, particularly among young people. Worldwide, over 1 billion children and adolescents live in countries affected by armed conflict (UNICEF 2008). For these individuals, the effects of war are catastrophic, as a direct result of witnessing and participating in acts of violence (Machel 1996), and as an indirect effect of war on social, community and family structures (Patel et al. 2007b; Betancourt and Khan, 2008). High rates of depression, anxiety and post-traumatic stress reactions have been reported by war-affected youth around the globe, including in sub-Saharan Africa (Betancourt et al. 2010b), Asia (Kohrt et al. 2008) and the Middle East (Razokhi et al. 2006). Longitudinal studies in these settings have documented that the symptoms markedly improve over time for some individuals, while persisting for others (Betancourt et al. 2013a).
Although treatment levels for young persons affected by war are remarkably low, there is evidence that effective interventions do exist. Behavioural interventions in these settings have been successfully implemented to treat post-traumatic stress reactions (Onyut et al. 2005; Tol et al. 2008) and have shown modest benefits in reducing depression symptomatology (Bolton et al. 2007; Jordans et al. 2010). For example, a recent randomized controlled trial at internally displaced person camps in northern Uganda found that interpersonal therapy was significantly more effective than a group-based recreation program (and no treatment) for reducing depression symptoms in adolescents (Bolton et al. 2007). However, on further inspection, it was found that this effect was significant for girls but not for boys. Additionally, differences between groups on all secondary measures—including post-traumatic stress reaction and functional impairment—were non-significant. Studies like these indicate the potential inherent in psychotherapies for war-affected young persons while, at the same time, underscoring the need to further the clinical impact.
Despite a growing literature focused on measuring the effectiveness of interventions for war-affected youth, there is a dearth of research studying intervention costs and cost-effectiveness. The ratio of costs to benefits of an intervention plays a central role in the policymaking decision to scale up care (Chisholm 2005). In the context of today’s global health agenda, any investment in mental health must compete alongside myriad other health problems, including the leading causes of death in poor countries—lower respiratory infections, ischemic heart disease and diarrhoeal diseases—each of which has identified cost-effective interventions (Edejer et al. 2005; Gaziano 2005; Simoes et al. 2006). To date, only one cost analysis (Jordans et al. 2011) and no cost-effectiveness analyses have been published on behavioural treatments for war-affected youth in post-conflict settings. The cost analysis, by Jordans et al., found that a community-based mental health care package costs 3.46€ to 17.32€ per person while delivering reductions in symptom severity. However, because health outcomes were not converted to a standardized health metric like quality-adjusted life years (QALYs), the intervention’s efficiency could not be compared with investments in other areas of health care.
In this study, we evaluate the costs and cost-effectiveness of a behavioural intervention for war-affected Sierra Leonean youth (ages 15 to 24). Participants were randomly assigned to receive the intervention (n = 222) or care as usual (n = 214), after which they were randomized to receive an education subsidy beginning immediately (n = 220) or 1 year later (n = 216). We hypothesized that the intervention would be cost-effective, meaning that each QALY gained would cost less than three times the country’s average per capita gross domestic product (GDP) at purchasing power parity, following suggested benchmarks for good value for money (VfM) in global health interventions (World Health Organization 2012a). Additionally, we expected that the intervention would be particularly cost-effective for those with the highest levels of symptoms at baseline (in the upper quartile), and that additional improvements not captured by cost-effectiveness analysis would be observed on mental health and schooling outcomes.
Methods
Intervention
The Youth Readiness Intervention (YRI) is a multi-pronged group-based therapy which focuses on reducing functional impairment produced as a result of psychological problems such as depression, anxiety and hostility, as well as poor emotion regulation and interpersonal skills. Functional impairments relate to aspects of everyday living including mobility, self-care, communication with others and involvement in the community. The YRI’s development was grounded in the findings of an on-going prospective cohort study carried out in the region, beginning a year after the Sierra Leonean civil war ended (2002) (Betancourt et al. 2008, 2010b). To address the co-occurring problems documented by this longitudinal study, the YRI synthesizes empirically supported practice elements shown to have efficacy across disorders ranging from major depressive disorders to conduct disorders (Cloitre et al. 2002; Chorpita et al. 2005). Each session represented one module, in which facilitators taught specific components derivative from cognitive behavioural therapy: e.g., emotion regulation skills, cognitive restructuring, problem solving and interpersonal skills. This session content was developed in consultation with a team of clinical psychologists.
Components of the YRI were adapted to the Sierra Leonean context by integrating feedback from a series of key informant interviews with war-affected youth (n = 21), caregivers (n = 19) and youth-serving organizations (n = 8). For example, the application of local proverbs was suggested as a way to summarize the content of each session and serve as a mnemonic device for helping youth retain information. A Community Advisory Board (CAB) was established in communities where the intervention was implemented. Meetings were held on a monthly basis over the course of the study. Three CAB meetings reviewed intervention content and advised the team on adaptation of content. A comprehensive training and supervision system was established with a senior local mental health worker providing daily supervision to all interventionists, along with weekly group supervisions held with an international team which included a clinical psychologist originally from Sierra Leone.
Participants
Young persons were recruited via referrals from village chiefs, youth outreach centres and local churches and mosques. Individuals were eligible for participation if they (1) were between the ages of 15 and 24 years (in accordance with the UN definition of ‘youth’; United Nations 2011), (2) scored at least half a standard deviation above mean symptom levels previously documented among war-affected youth from the region, based on the Oxford Measure of Psychosocial Adjustment (OMPA; a level associated with substantial functional impairments) (Betancourt et al. 2010a,b), (3) reported impairment in day-to-day functioning as a result of emotional or behavioural problems and (4) were not currently attending school. Individuals were excluded and referred for one-on-one psychological counselling if they reported suicidal ideation or psychotic symptoms. Two such cases were reported over the duration of the trial.
Approval for the trial was provided by an ethics committee at the Harvard School of Public Health as well as by a local ethics committee administered by Sierra Leone’s Ministry of Health. All participants over 18 years provided oral consent; those younger than 18 years provided oral assent and a primary caregiver provided oral consent.
Randomization and masking
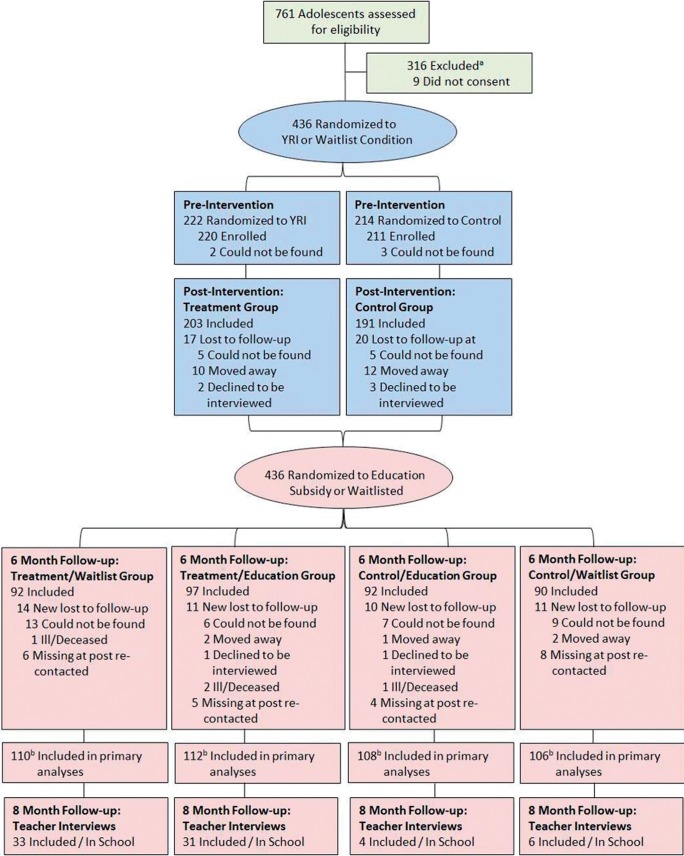
A randomization sequence was used to assign participants to the control condition or YRI, stratified by sex and age group (younger: 15–17 years, older: 18–24 years). Trained research staff members who obtained outcome measures following the intervention were blind to assignment. After completing the YRI, this procedure was repeated to assign youth to an educational opportunity in either the fall of 2012 or 2013, stratifying by intervention condition (Figure 1).
Figure 1.
Flowchart of study participants. aDid not meet inclusion criteria (described in study eligibility criteria). bPrimary analyses include all youth randomized, via an intention-to-treat approach using multiple imputation analysis.
Procedures
In order to facilitate capacity building and to test the possibility of task shifting at a health systems level (Petersen et al. 2012), eight local community health workers (4 male, 4 female) were trained to deliver the intervention in teams of two. Based on cultural norms, intervention groups were divided by sex and age group, with same-sex facilitators. All facilitators completed an intensive 2-week training conducted by clinicians who previously implemented the intervention in a pilot phase.
Prior to the intervention, 2-h baseline assessments were conducted by locally trained research staff in the local language, Krio. To ensure accuracy of materials, all instruments were forward and backward translated using a standardized protocol (World Health Organization 2012b). The intervention occurred over a 10-week period from the middle of August to the end of October 2012. Group sessions lasted for 2 h and were held once a week at one of the six sites throughout Freetown, the capital of Sierra Leone. Sessions were audio recorded to allow a locally trained clinical supervisor to review fidelity to session content. Youth were provided with a hot meal at each session they attended, and transportation was subsidized for a limited number of participants who lived farthest from intervention sites and would have been unable to attend sessions without support for transportation.
After completion of the YRI, at post-assessment (‘post’), all study youth were re-interviewed and then randomized to be offered a subsidized educational experience starting in 2012 (n = 220) or 2013 (n = 216). In total, 112 YRI recipients and 108 controls were offered subsidized education at a specialized school for impoverished youth, which covered school meals, textbooks and tuition. Youth were re-interviewed at 6-month follow-up, partway through the school year. Additionally, at the end of the school year (June 2013), teachers were interviewed about youths’ school enrolment, attendance and academic performance (Figure 1). Institutional Review Board approval was obtained from the Harvard School of Public Health and the Sierra Leonean Ministry of Health ethics committee.
Care as usual
Those in the control group received care as usual, comprising youth outreach programs provided by local non-governmental organization (NGOs) and religious organizations serving troubled youth in Freetown. In general, formal mental health care options in Sierra Leone are extremely limited, as indicated by the existence of only one mental hospital and no outpatient facilities (World Health Organization 2011). Based on this, we anticipated that control subjects would most likely have sought care through informal means such as family and community supports; but we did not directly ask about treatment-seeking behaviour. To the extent that formalized care was sought by wait-listed participants, this would only serve to (conservatively) reduce the apparent effect of the YRI.
Outcome measures
The primary outcome measure of intervention effectiveness was the 12-item version of the World Health Organization Disability Adjustment Scale II (WHODAS II) (World Health Organization 2001). The WHODAS II measures daily functioning across six domains: understanding and communicating, getting around, self-care, getting along with people, life activities and participation in society. Participants are asked to state the level of difficulty in accomplishing tasks and activities over the past 30 days, based on a 5-point ordinal scale. The instrument has undergone validity and reliability testing in 16 centres across 14 countries (World Health Organization 2001). Within our sample, the measure showed good reliability (Cronbach’s α = 0.91).
Given our a priori hypothesis that functional impairment would decline as a result of improved psychosocial well-being, several measures of mental health were incorporated. We used the OMPA (MacMullin and Loughry 2004)—an instrument previously adapted and validated for implementation in Sierra Leone and northern Uganda—to quantify internalizing (depression and anxiety; 16 items, α = 0.77) and externalizing problems (aggression and hostility; 12 items, α = 0.85), as well as adaptive behaviour (18 items, α = 0.82). Adaptive behaviour encompasses behaviour used to appropriately adjust to social contexts and challenging situations, e.g., recalibrating an unsuccessful coping strategy to a constructive one (Eisenberg et al. 2007). Additionally, a measure of emotion regulation, adapted from the Difficulties in Emotion Regulation Scale (Gratz and Roemer 2004), was administered to assess improvements in individuals’ ability to monitor and manage their experience and expression of emotions (23 items, α = 0.65).
At the end of the 2012 to 2013 academic year (July 2013), the number and percentage of participants enrolled in school were evaluated. A 20-item teacher survey, the Classroom Performance Scale (CPS; α = 0.95) (Children and Adults with Attention Deficit Disorder 1996), measured dimensions of academic performance including completion of coursework, classroom behaviour and classroom participation, and teachers were also asked to rate students’ attendance over the past month as poor, average or good.
Costing methodology
An ingredients approach was utilized for costing: activities were first identified to be costed, and then the financial and economic costs of carrying out these activities were quantified (Drummond et al. 2005). Activities encompassed trainings for staff and interventionists, recruitment of participants, delivery of treatment sessions with youth, community sensitization activities and routine review of work with the clinical team based in Boston. Although financial costs accounted for actual expenditures only, economic costs captured all resources used—including those volunteered and donated—and assumed a societal perspective by incorporating opportunity costs incurred by participants. The estimated time invested by each YRI participant totalled approximately 22 h; we assumed the value of this time to be $8.42 per hour, based on median hourly wage in Sierra Leone. We also made the conservative assumption that the incurred cost to participants under the care-as-usual framework was $US 0.
Cost estimates were obtained from various sources, including quotes, invoices and receipts. For example, the overhead cost of electricity was derived from monthly invoice statements at field headquarters, while costs of office supplies were compiled from receipts stored at the Harvard School of Public Health. Staff time was valued at full salary cost, including allowances for vacation. The cost of clinical space was estimated based on local rents. All costs were expressed in international dollars (int.$). A full overview of itemized capital and recurrent costs can be found in Table 3.
Table 3.
Financial and economic costs of the youth readiness intervention
| Cost category | Pre-implementation costs (Y0) total |
Implementation year costs (Y1) total |
Total implementation costs (Y0 and Y1) |
Percent of total average (Y0 and Y1) |
||||
|---|---|---|---|---|---|---|---|---|
| Financial cost | Economic cost | Financial cost | Economic cost | Financial cost | Economic cost | Financial cost | Economic cost | |
| Recurrent costs | ||||||||
| Clinician salaries (n = 8) | 3932.1 | 3932.1 | 6703.5 | 6703.5 | 10 635.6 | 10 635.6 | 58.3 | 46.0 |
| Part-time HR manager salary | 133.1 | 133.1 | 199.6 | 199.6 | 332.7 | 332.7 | 1.8 | 1.4 |
| Clinical supervisor salary | 749.1 | 749.1 | 1123.6 | 1123.6 | 1872.7 | 1872.7 | 10.2 | 8.1 |
| Part-time finances staff salary | 69.8 | 69.8 | 104.7 | 104.7 | 174.5 | 174.5 | 0.9 | 0.8 |
| Transport for clinicians | 54.9 | 54.9 | 0.00 | 0.0 | 54.9 | 54.9 | 0.3 | 0.2 |
| Transport for participants | 0.0 | 0.0 | 369.5 | 369.5 | 369.5 | 369.5 | 2.0 | 1.6 |
| Rental for clinical space | 0.0 | 635.9 | 1620.0 | 3240.0 | 1620.0 | 3875.9 | 8.9 | 16.8 |
| Food for participants | 0.0 | 0.0 | 2778.8 | 2778.8 | 2778.8 | 2778.8 | 15.2 | 12.0 |
| Opportunity cost to participants | 0.0 | 0.0 | 0.00 | 1868.7 | 0.0 | 1868.7 | 0.0 | 8.1 |
| Capital costs | ||||||||
| Staff training | 119.2 | 119.2 | 0.0 | 0.0 | 119.2 | 119.2 | 0.6 | 0.5 |
| Materials for treatment groups | 0.00 | 0.0 | 144.5 | 394.4 | 144.5 | 394.4 | 0.8 | 1.7 |
| Computers and office supplies | 48.3 | 48.3 | 76.9 | 576.9 | 125.2 | 625.2 | 0.7 | 2.7 |
| Subtotal recurrent costs | 4939.0 | 5574.9 | 12899.7 | 16388.4 | 17838.7 | 21963.3 | 95.1 | 95.1 |
| Subtotal capital costs | 167.5 | 167.5 | 221.4 | 971.3 | 388.9 | 1138.8 | 4.9 | 4.9 |
| Total costs of program | 5106.5 | 5742.4 | 13121.1 | 17359.7 | 18227.6 | 23102.1 | 100.0 | 100.0 |
| Cost per person | 23.0 | 25.9 | 59.1 | 78.2 | 82.1 | 104.1 | ||
Analyses for effectiveness estimates
Based on a recent meta-analysis of evidence-based psychotherapies for youth (Weisz et al. 2006), we adopted a standardized effect size of 0.30 as achievable by the YRI and clinically meaningful to youth. Assuming a standard alpha level of 0.05 with a 0.5 correlation (r) across 2 time points, 436 participants were required to have 0.8 power to detect an effect size of 0.30, allowing for 20% attrition.
Mixed linear effects models were utilized to compare the health states of YRI recipients and controls at baseline, post-assessment, 6-month and 12-month follow-up. This approach is analogous to typical multiple linear regression, save for the fact that random effects account for clustering of youth within treatment groups and lack of independence of observations over time. Without the inclusion of random effects, standard errors would be underestimated, leading to increased probability of a Type I Error when examining treatment effects. We examined the effect of treatment as two-way interactions (time×ntervention), after which we tested three-way interactions to inspect the roles of symptom severity (time × intervention × symptom severity), sex (time × intervention × sex) and age (time × intervention × age group) in relation to the treatment effect. Moderator analyses inspecting the effect of symptom severity utilized the upper quartile of symptom levels at baseline to classify those as ‘high severity’ (Kahn et al. 2004; Kohler et al. 2011). Fixed effects accounted for the stratified study design by incorporating age group, sex, education assignment, as well as interactions among these. The inclusion of these measures subsequently allowed us to examine the effect of education on mental health outcomes at 6-month follow-up.
The primary mode of analysis was intention-to-treat, meaning that all randomized participants were included in analyses, even if the individual was assigned to treatment and attended no sessions. In total, 90% of the sample provided interviews at post-assessment and 85% at 6-month follow-up. Among those re-interviewed, missing values were imputed in cases where fewer than 25% of item responses were missing on an outcome scale, using a Markov chain Monte Carlo method with an added error term. For those with more than 25% missingness, including those who were lost to follow-up, scores were imputed using multiple imputation analysis. This approach characterizes the joint probability distribution of all variables in the model to create multiple simulated values for missing observations, thereby reducing bias in addition to accounting for sampling variability across imputations (Rubin 1987).
Cost-effectiveness analyses
Cost-effectiveness was estimated using a Markov cohort modelling approach in TreeAge Pro 2009 (TreeAge 2009). Analyses were conducted from a societal perspective, incorporating participant time costs. The main outcome measure of functional impairment, the WHODAS, was converted to QALYs using a standardized methodology, as outlined by Buttorf et al. (2012). In short, the WHODAS summary score was converted to a preference-weighted utility index using a population-based survey of health state preferences from the WHO Multi-Country Survey Study on Health and Health System Responsiveness (14 countries, n > 40,000) (Üstün et al. 2001).
Sensitivity analyses were incorporated to provide a range of estimates for incremental cost-effectiveness ratios (ICERs). First, discount rates varied from 0% to 5%; 0% was assumed under the base scenario. Second, the estimated costs of the trial varied from 80% to 120%, where 100% represented the documented cost of the trial. Third, different future health state trajectories were simulated for participants. Health states were projected based on age-specific healthy life expectancy in Sierra Leone (Salomon et al. 2012). Under the base scenario, we assumed that the standardized mean difference between treatment and control groups would depreciate linearly over time by 0.055 standard deviation (SD) per year. This figure (Δ effect size = 0.055) is based on a meta-analysis of over 300 longitudinal intervention trials with adolescents suffering various mental health conditions (JR Weisz, unpublished results). As a more conservative approach, we also report cost-effectiveness based strictly on differences observed within trial, implying that there would be no observed effect of the intervention after the cessation of data collection (Table 4).
Table 4.
Incremental cost-effectiveness ratios for the YRI
| Linear reduction | Within study | |
|---|---|---|
| Full sample | ||
| 0–5% discount rate | $7260 to $10 044/QALY | $8052 to $10 140/QALY |
| 80–120% estimated cost | $5808 to $9432/QALY | $6444 to $9672/QALY |
| Upper quartile | ||
| 0–5% discount rate | $3564a to $6276/QALY | $8088 to $11 820/QALY |
| 80–120% estimated cost | $2856a to $4272/QALY | $6480 to $9708/QALY |
ICERs for cost per QALY gained.
aScenarios in which the intervention would be considered cost-effective in that the ICER is less than three times average gross domestic product per capita at purchasing power parity.
To provide confidence intervals around point estimates, a probabilistic sensitivity analysis was performed that included uncertainty estimates for individual health states (100 000 Monte Carlo simulations). Standard deviations were derived from the output of mixed effects models using STATA’s margins command. Acceptability curves were also utilized to determine the percentage of simulations in which the ICER fell below the willingness-to-pay threshold of three times average GDP per capita (PPP) in Sierra Leone (US$ 1359).
Results
Baseline sample characteristics
Among the 436 participants at baseline, 46% (n = 199) were female. Mean age at baseline was 18.0 (SD = 2.4) years. Two hundred and twenty-two participants (51%) were randomly assigned to receive the YRI, resulting in 26 therapy groups with an average of nine participants per group (range: 5–11 participants). Eighty-two percent of the participants attended at least one session; the average number of sessions attended was 6.3 (SD = 3.8). Defining ‘drop-out’ as those who attended fewer than 25% of the sessions and none of the last 3 sessions, retention would be seen as 76%. Additional information on the study sample is provided in Table 1.
Table 1.
Study sample characteristics at baseline
| Sample characteristic | Treatment group (n = 222) | Control group (n = 214) |
|---|---|---|
| Demographics | ||
| Male | 123 (55.4%) | 114 (53.3%) |
| Age | 17.8 (2.3) | 18.1 (2.6) |
| Years of schooling | 8.5 (2.0) | 8.6 (2.1) |
| Currently employed | 87 (39.2%) | 84 (39.3%) |
| War exposures | ||
| Lost friend/family member | 114 (58.5%) | 105 (54.7%) |
| Witnessed armed conflict | 35 (18.9%) | 38 (20.5%) |
| Separated from caregiver | 70 (38.5%) | 62 (35.2%) |
Continuous measures reported as mean (standard deviation) and categorical measures reported as number (percent).
Symptom severity at post-assessment and 6-month follow-up
Effectiveness estimates of the YRI are provided in Table 2. At post-assessment, YRI participants reported lower levels of disability (higher functioning) in day-to-day living compared with controls [β = 3.457, 95% confidence interval (CI) 0.874–6.041]. On the original disability measure (WHODAS), this would reflect a two-unit improvement over and above that reported by controls, e.g., reporting ‘mild’ impairment, rather than ‘moderate’ impairment, for 2 of the 12 items at follow-up compared with baseline. Additionally, adaptive behaviour among YRI recipients was significantly higher than among controls (β = 0.149, 95% CI 0.057–0.240), as were emotion regulation skills (β = 0.109, 95% CI 0.026–0.191). In contrast, those in treatment and control conditions reported similar levels of internalizing (β = 0.005, 95% CI: − 0.089 to 0.100) and externalizing (β = −0.032, 95% CI −0.134 to 0.070) at post-assessment. At 6-month follow-up, no group differences were present on outcomes.
Table 2.
Effectiveness estimates from mixed linear effects models
| Outcome | Post intx, full sample | Post intx, upper quartile | 6 months, full sample | 6 months, upper quartile |
|---|---|---|---|---|
| Disability | β = 3.46 | β = 1.04 | β = 1.07 | β = 5.61 |
| 95% CI 0.87–6.04 | 95% CI −4.38 to 6.46 | 95% CI −1.92 to 4.07 | 95% CI −0.13 to 11.36 | |
| P = 0.01, δ = 0.31 | P = 0.71, δ = 0.09 | P = 0.48, δ = 0.10 | P = 0.06, δ = 0.51 | |
| Adaptive behaviour | β = 0.15 | β = 0.09 | β = 0.01 | β = −0.106 |
| 95% CI 0.06–0.24 | 95% CI −0.11 to 0.29 | 95% CI −0.12 to 0.13 | 95% CI −0.31 to 0.10 | |
| P < 0.01, δ = 0.38 | P = 0.40, δ = 0.22 | P = 0.92, δ = 0.02 | P = 0.32, δ = −0.27 | |
| Internalizing | β = 0.01 | β = −0.22 | β = 0.03 | β = −0.069 |
| 95% CI −0.09 to 0.10 | 95% CI −0.44 −0.01 | 95% CI −0.09 to 0.14 | 95% CI −0.29 to 0.15 | |
| P = 0.91, δ = 0.01 | P = 0.04, δ = −0.61 | P = 0.63, δ = 0.07 | P = 0.54, δ = −0.18 | |
| Externalizing | β = −0.03 | β = −0.18 | β = −0.01 | β = −0.28 |
| 95% CI −0.13 to 0.07 | 95% CI −0.42 to 0.07 | 95% CI −0.13 to 0.11 | 95% CI −0.53 to −0.03 | |
| P = 0.54, δ = −0.07 | P = 0.15, δ = −0.37 | P = 0.88, δ = −0.02 | P = 0.03, δ = −0.59 | |
| Emotion regulation | β = 0.11 | β = 0.20 | β = 0.02 | β = 0.27 |
| 95% CI 0.03–0.19 | 95% CI 0.01–0.39 | 95% CI −0.09 to 0.12 | 95% CI 0.07–0.46 | |
| P = 0.01, δ = 0.31 | P = 0.04, δ = 0.59 | P = 0.79, δ = 0.04 | P = 0.01, δ = 0.82 |
‘Post’ indicates interviews conducted at post-assessment, following completion of the YRI; ‘6 months’ indicates follow-up interviews conducted 6 months after post-assessments. For all outcomes, the treatment effect represents the per-item difference between treatment and control groups at post-assessment. Effect size for the treatment effect is reported as standardized mean difference (δ).
Moderator analyses inspecting the role of symptom severity at baseline found several instances in which those in the upper quartile who received the YRI improved more than those who did not receive treatment, over and above the effect observed in the bottom three quartiles. At post-assessment, YRI recipients reported greater improvements in emotion regulation (β = 0.200, 95% CI 0.006–0.394) and greater decreases in internalizing symptoms (β = −0.227, 95% CI −0.440 to −0.014). At 6-month follow-up, those who received treatment again reported higher emotion regulation (β = 0.269, 95% CI 0.073–0.464) as well as lower externalizing (β = −0.277, 95% CI −0.527 to −0.027) and marginally greater levels of functioning (β = 5.613, 95% CI −0.131 to 11.357). Examining covariates at this time point, we also observed no effect of YRI assignment on mental health outcomes.
Schooling outcomes at 8-month follow-up
At the end of the 2012–2013 academic school year, 74 youth were enrolled in school: 28.8% (n = 64) of YRI participants vs 4.7% (n = 10) of controls [z = 4.31, P < 0.001, odds ratio (OR) 8.88]. Similar numbers of youth were still in school at the end of the year, when comparing cohorts randomized to receive education starting in 2012 (15.9%, n = 35) vs 2013 (18.1%, n = 39): z = −0.67, P = 0.50. Of youth who were still in school at the end of the school year, teachers (blinded to YRI condition) reported that YRI youth demonstrated significantly better classroom performance (t = −2.19, P = 0.03, effect size = −1.31), based on the CPS, as well as attendance over the past month (z = 2.70, P = 0.007, OR 34.93).
Costs and cost-effectiveness
The cost of the intervention was estimated to be $104.06 per participant. Table 3 outlines all expenditures incurred over the course of the trial. Almost half of all costs (46%) were derived from salaries for the eight clinicians who delivered the intervention. This was followed by the cost of rental space for group sessions (17%), incentives for participants (14%) and salaries of three support staff members—a clinical supervisor, a part-time human resources manager and a part-time finances manager (10%).
The economic cost of the YRI was 27% larger than the financial cost. This difference can be ascribed to free rental space at community facilities for hosting youth sessions, as well as incorporating opportunity costs to youth for participating. Given a scenario in which the intervention is integrated into an existing structure such as a schooling or employment program, it is possible that financial costs could be halved through savings in transport, staffing and rental of clinical space. However, to remain as close as possible to the collected data, cost-effectiveness analyses were based on observed expenditures.
The average health state value (converted WHODAS score for deriving QALYs: scale 0–1) reported by YRI recipients was 0.831 at post-assessment and 0.831 at 6-month follow-up, compared with 0.801 and 0.825 among controls. Estimated QALY was 52.30 among controls and 52.31 among YRI recipients. Table 4 provides a breakdown of the ICER under a range of scenarios. Under the base case scenario, the ICER was $7260 per QALY (95% CI $1056 to Inf.) and was cost-effective at three times average GDP per capita (PPP) in 39.6% of simulations. A one-way sensitivity analysis on discounting varied estimates from $7260 per QALY (0%) to $10 044 per QALY (5%), while modification of estimated intervention costs varied the ICER from $5808 (80%) to $9432 (120%). Looking only at cost-effectiveness within the time frame of data collection (Table 4, column 2), cost-effectiveness estimates were higher (less attractive) by 1.0–11.0%.
When restricting the sample to those who were in the upper quartile of symptom severity at baseline, cost-effectiveness improved substantially. At pre, post and follow-up, the health state value of YRI recipients in this subgroup was 0.615, 0.765 and 0.822, as compared with 0.637, 0.750 and 0.795 among controls. Under the base case scenario, the ICER was $3564 per QALY gained (95% CI $601 to Inf.), or 2.6 times the average GDP per capita, and was cost-effective in 51.9% of the simulations (World Bank 2013).
Sensitivity analyses found that varying the discount rate from 0% to 5% changed the ICER from $3564 to $6276 per QALY, while varying the cost from 80% to 120% changed the ICER from $2856 to $4272 per QALY. Restricting the analysis to the time frame of data collection, cost-effectiveness estimates were much worse—as much as 130% higher. The reason for this is that, among those in the upper quartile, the between-groups difference at 6-month follow-up is much larger (effect size = 0.5) than that observed overall (effect size = 0.1), and therefore whether one incorporates expected intervention benefits after the end of the trial has a larger effect.
Expanding this cost-per-outcome framework beyond health to education, the cost per additional year of school enrolment was also estimated. Given that 28.8% of YRI participants and 4.7% of controls persisted in school (were still enrolled in school at the end of the school year), the YRI is estimated to cost $430.80 per additional year of enrolment. The cost per unit increase in school attendance, say from ‘poor’ to ‘average’ attendance as reported by teachers, was estimated at $86.76 per participant.
Discussion
Today, 76% of Sierra Leoneans are under the age of 35 (World Bank 2011), and over half of these individuals are unemployed or underemployed (IRIN News 2012), indicating a marked under-appreciation of human capital. As shown by longitudinal research, many war-affected young persons in the region suffer from mental health problems linked to prior war exposures, as well as daily stressors that represent indirect and continuing consequences of the Sierra Leonean civil war (Betancourt et al. 2010b, 2013b). Against this backdrop, the YRI was developed to address functional impairments and a range of emotional and behavioural problems that put youth at risk for poor life trajectories, including schooling and employment outcomes. As reported elsewhere (Betancourt et al. under review), our findings demonstrate that the YRI is effective in improving aspects of daily functioning and mental health over the short term, while over the longer term stabilizing outcomes for those who may be considered the ‘worst-off’ and improving schooling outcomes among the wider group.
This study affords a policy-relevant vantage point, measuring intervention efficiency in terms of dollars spent per health and schooling outcome. When viewed narrowly in terms of dollars per standardized health outcome, the YRI yields an overall ICER of $7260 per QALY gained, exceeding a typical willingness-to-pay threshold of three times GDP per capita. However, the intervention also ‘buys’ several other outcomes which are not internalized within the cost-effectiveness analysis (CEA) framework: short-term improvements in emotion regulation (effect size = 0.31) and adaptive behaviour (effect size = 0.38), and improved longer term retention and performance in schooling. Seen from this vantage point, the YRI can also be viewed as costing $431 per additional year of school attendance, an investment shown to yield considerable economic returns (Psacharopoulos and Patrinos 2004).
Among those in the upper quartile of symptom severity at baseline, the effect of the intervention ‘increased’ over time. Assuming a gradual decline in this effect after the recorded 6-month follow-up, cost-effectiveness in this subgroup would be estimated as $3564 per QALY gained, less than the three times the GDP per capita threshold. This ICER is roughly equivalent to that of cholera or rotavirus immunization to reduce diarrhoeal disease, or the use of statin drugs to reduce risk of ischaemic heart disease (Laxminarayan et al. 2006). Looking at the original WHODAS measure, this investment translates into an improvement of 2 ordinal units on the 12-item WHODAS, e.g., reporting mild rather than moderate symptomology for 2 additional items, as compared with those who were wait listed. The broader literature on mental health interventions in low- and middle-income countries (LAMICs) has found the cost of care to range from $400 per QALY (tricyclics for the treatment of panic disorder) to $12 000 per QALY (atypical antipsychotics and psychotherapy for patients with psychosis) (Patel et al. 2007a,b). It should also be noted that those in this subgroup exhibited sizable, sustained improvements over time in two additional areas of mental health that are not directly captured by cost-effectiveness analysis: namely, emotion regulation (effect size = 0.82) and externalizing behaviour (effect size = 0.59).
There are two key insights to be drawn from these findings. First, whether the YRI is considered to be an ‘efficient’ investment in its present form depends, at least in part, on a range of assumptions and how one interprets the data. Although the intervention is not cost-effective by the traditional metric of cost per QALY, interpreted at a threshold of three times average GDP per capita, cost-effectiveness analysis does not fully capture all mental health and schooling outcomes addressed by the intervention. The more holistic cost analysis finds that an additional array of benefits is afforded by the YRI, including improved school retention and performance.
Second, as opposed to many interventions for physical ailments—such as vaccines—the content and delivery of the YRI can be easily adjusted in future iterations to enhance cost-effectiveness. For example, targeting individuals based on a higher level of disability, the cost-effectiveness could be dramatically improved. Qualitative feedback provided by interventionists and participants, as well as booster sessions following the conclusion of the main program, would also strengthen content and delivery, although this would also result in additional costs. Threshold analyses indicate that intervention effectiveness would need to be improved only moderately—to a standardized mean group difference of effect size = 0.07 at 6-month follow-up—to achieve cost-effectiveness. Alternatively, costs could be reduced by eliminating the intervention’s stand-alone framework. For example, if the YRI was delivered as part of an existing school program, this would save on costs of staff, facilities and transportation.
Looking at the wider global health agenda and reflecting on paths forward, there are at least two areas where follow-on research would provide a great deal of insight. First, a growing evidence base has indicated a direct connection between mental health and cycles of poverty—including that those who have been treated for mental health problems have demonstrated economic improvements (Lund et al. 2011). Longer term follow-up with our cohort of patients would allow us to examine whether improved educational outcomes among those who received the YRI later translates into improved economic productivity. Second, examination of the totality of outcomes in this manuscript from the lens of cost-benefit analysis (CBA)—i.e., comparing economic inputs with economic outputs—would contribute to discussions about VfM within the domain of global mental health (World Health Organization 2006). However, as with the more narrow lens of cost-effectiveness analysis, CBA assumes a utilitarian lens oriented towards utility maximization—in this case, using economic outputs as a proxy—and as such is indifferent to any inequality in the distribution of outcomes that may ensue as a consequence (Gold et al. 2002).
Study limitations
Several limitations deserve mention. First, in converting participants’ functioning scores to QALYs, we utilized a weighting scheme derived from an international sample of health state valuations from 14 countries (n > 40 000). Ideally, we would have used a nationally representative sample from Sierra Leone; however, no such survey exists. Given this, we must rely on the assumption that relative health state valuations within Sierra Leone are adequately reflected by the international sample. Using secondary data likewise limited our ability to examine gains in health utility in association with secondary measures such as emotion regulation.
Second, there is substantial uncertainty as to how long differences between treatment and control groups will persist moving forward. As stated earlier, the simulated trajectory of treatment and control cohorts plays a substantial role in shaping the longer term cost-effectiveness of the intervention. The assumption in this study is that, following data collection, the treatment effect will depreciate gradually over time in a manner similar to that observed in other studies, but there is also considerable variability in this rate of decline across studies (Kendall et al. 2004; Tarrier et al. 2004).
Third, this analysis was based on US$ in 2012. Adjusting for purchasing power parity (PPP) using international dollars would, arguably, have more accurately reflected the cost of the intervention ‘within’ the Sierra Leonean context. However, PPP comparisons between different countries often rest on weak theoretical foundations, undercutting the utility of this adjustment (Deaton 2008).
Finally, the inclusion criteria for our sample limit the external validity of our results. For example, it is unclear what the effectiveness of our intervention would be in an East African country, or if it were utilized with older adults as opposed to young persons. A rigorous process was undertaken to adapt intervention content to the Sierra Leonean setting and enhance ecological validity. Similar efforts would be required to replicate intervention effectiveness in other contexts.
Conclusion
This study represents the first cost-effectiveness analysis of a behavioural intervention for war-affected youth. We find that the YRI is effective but not cost-effective in its current form, based on a typical willingness-to-pay threshold of three times GDP per capita. However, the YRI demonstrates promise in a range of areas not traditionally captured in cost-effectiveness analysis, and the content and delivery can be modified in future trials to reduce costs and strengthen effectiveness.
Acknowledgements
We are grateful for the support from the Office of the US Ambassador to Sierra Leone. We would additionally like to thank our colleagues and supporters at CARITAS and EducAid in Sierra Leone and those at the François-Xavier Bagnoud Center for Health and Human Rights. In particular, we would like to acknowledge the conceptual input provided by Daniel J Norton (Boston University) and Robert T Brennan (Harvard University). Above all, we owe a debt of gratitude to our local advisory board for their steadfast guidance and the advice, our excellent local facilitators and supervisors and the many youth and families who participated in the study.
Funding
This study was supported by the United States Institute of Peace (USIP-008-10F) and the United Bank of Switzerland (UBS-5253). Further support was provided by the National Institute for Mental Health (5K01MH077246-05; 1F31MH097333-01A1), the National Institute of Aging (5P30AG024409-08), the Julie Henry Junior Faculty Development Fund, as well as the Australian Psychological Society, and National Health and Medical Research Council of Australia. Funders had no role in study design, data collection and analysis or manuscript preparation.
Conflict of interest statement. None declared.
References
- Belfer ML. 2008. Child and adolescent mental disorders: the magnitude of the problem across the globe. Journal of Child Psychology and Psychiatry 49: 226–36. [DOI] [PubMed] [Google Scholar]
- Betancourt TS, Agnew-Blais J, Gilman SE, Williams DR, Ellis BH. 2010a. Past horrors, present struggles: the role of stigma in the association between war experiences and psychosocial adjustment among former child soldiers in Sierra Leone. Social Science & Medicine 70: 17–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Brennan RT, Rubin-Smith J, Fitzmaurice GM, Gilman SE. 2010b. Sierra Leone’s former child soldiers: a longitudinal study of risk, protective factors, and mental health. Journal of the American Academy of Child & Adolescent Psychiatry 49: 606–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Khan KT. 2008. The mental health of children affected by armed conflict: protective processes and pathways to resilience. International Review of Psychiatry 20: 317–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, McBain R, Newnham EA, Brennan RT. 2013a. Trajectories of internalizing problems in war-affected Sierra Leonean youth: examining conflict and postconflict factors. Child Development 84: 455–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, McBain R, Newnham EA, et al. under review. Addressing interpersonal deficits and functioning in war-affected youth: a randomized controlled trial of the Youth Readiness Intervention in Sierra Leone. JAMA. [Google Scholar]
- Betancourt TS, Newnham EA, McBain R, Brennan RT. 2013b. Post-traumatic stress symptoms among former child soldiers in Sierra Leone: follow-up study. British Journal of Psychiatry 203: 196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Simmons S, Borisova I, et al. 2008. High hopes, grim reality: reintegration and the education of former child soldiers in Sierra Leone. Comparative Education Review 52: 565–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom DE, Cafiero ET, Jané-Llopis E, et al. 2011. The Global Economic Burden of Noncommunicable Diseases. Geneva: World Economic Forum. [Google Scholar]
- Bolton P, Bass J, Betancourt TS, et al. 2007. Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. Journal of the American Medical Association 298: 519–27. [DOI] [PubMed] [Google Scholar]
- Buttorff C, Hock RS, Weiss HA, et al. 2012. Economic evaluation of a task-shifting intervention for common mental disorders in India. Bulletin of the World Health Organization 90: 813–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Children and Adults with Attention Deficit Disorder. 1996. ADD and Adolescence: Strategies for Success from CHADD. Plantation, FL: CHADD. [Google Scholar]
- Chisholm D. 2005. Choosing cost-effective interventions in psychiatry: results from the CHOICE programme of the World Health Organization. World Psychiatry 4: 37–44. [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, Weisz JR. 2005. Identifying and selecting the common elements of evidence based interventions: a distillation and matching model. Mental Health Services Research 7: 5–20. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Koenen KC, Cohen LR, Han H. 2002. Skills training in affective and interpersonal regulation followed by exposure: a phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology 70: 1067–74. [DOI] [PubMed] [Google Scholar]
- Deaton A, Heston A. 2008. Understanding PPPs and PPP-based national accounts. NBER Working Paper No. 14499. http://www.nber.org/papers/w14499. accessed 2 October 2012. [Google Scholar]
- Drummond MB, Schulpher MJ, Torrance GW, O'Brien B, Stoddard GL. 2005. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press. [Google Scholar]
- Edejer TT, Aikins M, Black R, et al. 2005. Cost effectiveness analysis of strategies for child health in developing countries. BMJ 331: 1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Spinrad TL. 2007. Prosocial Development. Handbook of Child Psychology. Hoboken, NJ: Wiley. [Google Scholar]
- Gaziano TA. 2005. Cardiovascular disease in the developing world and its cost-effective management. Circulation 112: 3547–53. [DOI] [PubMed] [Google Scholar]
- Gold M, Stevenson D, Fryback DG. 2002. HALYs and QALYs and DALYs, oh my: similarities and differences in summary measures of population health. Annual Review of Public Health 13: 115–34. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. 2004. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment 26: 41–54. [Google Scholar]
- IRIN News. 2012. Youth Unemployment—A Threat to Sierra Leone’s Security [Online]. UN Office for the Coordination of Humanitarian Affairs. http://www.irinnews.org/report/96711/SLIDESHOW-Youth-unemployment-a-threat-to-Sierra-Leone-s-security, 2013. [Google Scholar]
- Jordans MJ, Komproe IH, Tol WA, et al. 2010. Evaluation of a classroom-based psychosocial intervention in conflict-affected Nepal: a cluster randomized controlled trial. Journal of Child Psycholology and Psychiatry 51: 818–26. [DOI] [PubMed] [Google Scholar]
- Jordans MJ, Komproe IH, Tol WA, et al. 2011. Practice-driven evaluation of a multi-layered psychosocial care package for children in areas of armed conflict. Community of Mental Health Journal 47: 267–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn RS, Brandt D, Whitaker RC. 2004. Combined effect of mothers’ and fathers’ mental health symptoms on children’s behavioral and emotional well-being. Archives of Pediatrics and Adolescent Medicine Journal 158: 721–9. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Safford S, Flannery-Schroeder E, Webb A. 2004. Child anxiety treatment: outcomes in adolescence and impact on substance use and depression at 7.4-year follow-up. Journal of Consulting and Clinical Psychology 72: 276–87. [DOI] [PubMed] [Google Scholar]
- Kohler S, Van Boxtel M, Jolles J, Verhey F. 2011. Depressive symptoms and risk for dementia: a 9-year follow-up of the Maastricht Aging Study. The American Journal of Geriatric Psychiatry 19: 902–5. [DOI] [PubMed] [Google Scholar]
- Kohrt BA, Jordans MJ, Tol WA, et al. 2008. Comparison of mental health between former child soldiers and children never conscripted by armed groups in Nepal. JAMA 300: 691–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laxminarayan R, Chow J, Shahid-Salles SA. 2006. Intervention cost-effectiveness: overview of main messages. In: Jamison JT, Breman JG, Measham AR, et al. (eds). Disease Control Priorities in Developing Countries. New York: Oxford University; 35–86. [Google Scholar]
- Lund C, De Silva M, Plagerson S, et al. 2011. Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. The Lancet 378: 1502–14. [DOI] [PubMed] [Google Scholar]
- Machel G. 1996. Impact of armed conflict on children. Report of the expert of the Secretary-General, submitted pursuant to UN General Assembly resolution 48/157. New York: United Nations. [Google Scholar]
- MacMullin C, Loughry M. 2004. Investigating psychosocial adjustment of former child soldiers in Sierra Leone and Uganda. Journal of Refugee Studies 17: 460–72. [Google Scholar]
- Murray CJ, Vos T, Lozano R, et al. 2012. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet 380: 2197–223. [DOI] [PubMed] [Google Scholar]
- Onyut LP, Neuner F, Schauer E, et al. 2005. Narrative Exposure Therapy as a treatment for child war survivors with posttraumatic stress disorder: two case reports and a pilot study in an African refugee settlement. BMC Psychiatry 5: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Araya R, Chatterjee S, et al. 2007a. Treatment and prevention of mental disorders in low- and middle-income countries. The Lancet 370: 991–1005. [DOI] [PubMed] [Google Scholar]
- Patel V, Flisher AJ, Hetrick S, McGorry P. 2007b. Mental health of young people: a global public-health challenge. The Lancet 369: 1302–13. [DOI] [PubMed] [Google Scholar]
- Petersen I, Lund C, Bhana A, Flisher AJ, Mental Health and Poverty Research Programme Consortium. 2012. A task shifting approach to primary mental health care for adults in South Africa: human resource requirements and costs for rural settings. Health Policy and Planning 27: 42–51. [DOI] [PubMed] [Google Scholar]
- Psacharopoulos G, Patrinos A. 2004. Returns to investment in education: a further update. Education Economics 12: 111–34. [Google Scholar]
- Razokhi AH, Taha IK, Taib NI, Sadik S, Gasseer NA. 2006. Mental health of Iraqi children. The Lancet 368: 838–9. [DOI] [PubMed] [Google Scholar]
- Rubin DB. 1987. Multiple Imputation for Nonresponse in Surveys. New York: Wiley. [Google Scholar]
- Salomon JA, Wang H, Freeman MK, et al. 2012. Healthy life expectancy for 187 countries, 1990-2010: a systematic analysis for the Global Burden Disease Study 2010. The Lancet 380: 2144–62. [DOI] [PubMed] [Google Scholar]
- Simoes EA, Cherian T, Chow J, et al. 2006. Acute respiratory infections in children. In: Jamison DT, Breman JG, Measham AR. (eds). Disease Control Priorities in Developing Countries. Washington, DC: World Bank; 483–498. [Google Scholar]
- Tarrier N, Lewis S, Haddock G, et al. 2004. Cognitive-behavioural therapy in first-episode and early schizophrenia. 18-month follow-up of a randomised controlled trial. British Journal of Psychiatry 184: 231–9. [DOI] [PubMed] [Google Scholar]
- Tol WA, Komproe IH, Susanty D, et al. 2008. School-based mental health intervention for children affected by political violence in Indonesia: a cluster randomized trial. JAMA 300: 655–62. [DOI] [PubMed] [Google Scholar]
- TreeAge. 2009. TreeAge Pro 2009. Williamstown, MA: TreeAge Software Inc. [Google Scholar]
- United Nations International Children’s Emergency Fund (UNICEF). 2008. State of the World’s Children 2008. New York: UNICEF. [Google Scholar]
- United Nations. 2011. Social and Human Services—UNESCO: Acting with and for Youth [Online]. http://www.unesco.org/new/en/social-and-human-sciences/themes/social-transformations/youth/, accessed 2 October 2012. [Google Scholar]
- Üstün TB, Chatterji S, Villanueva M, et al. 2001. WHO Multi-country Survey Study on Health and Responsiveness 2000-2001. Geneva: World Health Organization. [Google Scholar]
- Weisz JR, Jensen-Doss A, Hawley KM. 2006. Evidence-based youth psychotherapies versus usual clinical care: a meta-analysis of direct comparisons. American Psychologist 61: 671–89. [DOI] [PubMed] [Google Scholar]
- World Bank. 2011. Education in Sierra Leone: Present Challenges, Future Opportunities. Africa Human Development Series. Washington, DC: The World Bank. [Google Scholar]
- World Bank. 2013. GDP per Capita, PPP (Current International $), 2012. Washington, DC: World Bank. [Google Scholar]
- World Health Organization. 2001. WHODAS II: Disability Assessment Schedule [Online]. http://www.who.int/icidh/whodas/FAQ.html#q4, 2013. [Google Scholar]
- World Health Organization. 2006. Disease Control Priorities Related to Mental, Neurological, Developmental and Substance Abuse Disorders. Geneva: World Health Organization. [Google Scholar]
- World Health Organization. 2011. Sierra Leone: Mental Health Atlas 2011. Geneva: World Health Organization. [Google Scholar]
- World Health Organization. 2012a. Cost-effectiveness Thresholds (WHO-CHOICE) [Online]. http://www.who.int/choice/costs/CER_thresholds/en/index.html, accessed 30 November 2012. [Google Scholar]
- World Health Organization. 2012b. Process of Translation and Adaptation of Instruments [Online]. http://www.who.int/substance_abuse/research_tools/translation/en/index.html, accessed 10 July 2012. [Google Scholar]