Abstract
Objective
Because hyperlipidemia is asymptomatic, many veterans affairs (VA) patients may not perceive it seriously. We assessed key Health Belief model concepts to describe patients’ cholesterol-related health beliefs and examine associations between patient-level factors and desire to improve cholesterol control.
Methods
We used baseline data from an ongoing randomized clinical trial. Eligible patients were receiving care at the Durham VA and had CVD risk-total cholesterol levels >130 mg/dL and/or <80% medication adherence in the previous 12 months. A survey assessed patients’ health beliefs about high cholesterol and self-reported medication adherence. Multivariable logistic regression examined whether there was an association between desire to control cholesterol and cholesterol status.
Results
Approximately 64% (n = 155) of patients perceived high cholesterol as ‘very serious’. In multivariable logistic regression analysis, patients who perceived high cholesterol as ‘very serious’ (OR 2. 26, p = 0.032) and/or with high self-efficacy (OR 4.70, p <0.001) had increased odds of desiring cholesterol control.
Conclusion
The factors most significantly associated with desire to improve cholesterol control were perceiving hyperlipidemia as ‘very serious and self-efficacy for cholesterol control.
Practice implication
Educating patients, with the goal of appropriately increasing their perceived risk of disease, is likely necessary to impact cholesterol control.
Keywords: Hyperlipidemia, United States Department of Veterans Affairs, Health behavior, Disease susceptibility, Medication adherence
1. Introduction
Elevated total cholesterol, or hyperlipidemia, is a modifiable risk factor for cardiovascular disease (CVD); CVD is a leading cause of death in the U.S. [1]. The American Heart Association purports that proper CVD risk reduction includes the management of high cholesterol through the modification of lifestyle factors, such as improving diet and exercise habits, as well as through the use of prescription medications including statins [2]. Although improvements in LDL-C have been associated with reduction in risk for major cardiovascular events [3], many veterans fail to take medications according to prescription instructions [4]. One possible cause is skepticism in the potential consequences of hyperlipidemia and related a lack knowledge regarding the impact of reducing cholesterol levels.
Potential reasons for not engaging in healthy behaviors and adhering to prescription medications are numerous. These factors include having low health literacy, being of lower socioeconomic status, and experiencing barriers such as forgetfulness [5–9]. While these are real and often tangible barriers, underlying these factors – and the ability to overcome them – are health beliefs. Health beliefs influence many avenues of health and well-being. Since hyperlipidemia is an asymptomatic disease, many patients may not perceive it to be serious, and subsequently may not have the desire or confidence to improve their total cholesterol levels. Understanding characteristics associated with a desire to improve cholesterol control may be an important first step in changing health beliefs associated with cholesterol management.
The Health Belief Model (HBM) is a prominent conceptual framework with broad applications for understanding health behaviors [10,11]. Underscoring HBM is the idea that patients will engage in positive health actions in a desire to avoid negative health consequences. The HBM has six key concepts. In the context of elevated hyperlipidemia, these concepts include: (1) perceived susceptibility—belief of the chances of developing complications of high cholesterol; (2) perceived severity—belief of seriousness of high cholesterol and its consequences; (3) perceived benefits—belief in the efficacy of taking medications and making lifestyle changes to reduce the risk or impact of having high cholesterol; (4) perceived barriers—belief in the costs, pill burden, and other obstacles of managing high cholesterol; (5) cues to action—strategies to indicate readiness to change; and (6) self-efficacy—confidence in the ability to take action to improve cholesterol levels [10,11]. This analysis addresses 4 of these 6 principles (i.e., perceived susceptibility, perceived severity, perceived barriers, self-efficacy).
Using baseline data from an ongoing randomized controlled trial, we assessed key concepts from the HBM to address two objectives. First, we sought to describe patients’ cholesterol-related health beliefs. Second, we aimed to examine the association between patients’ sociodemographic characteristics, health beliefs, and their desire to improve their cholesterol control. Understanding what motivates patients’ desires to improve cholesterol control may be an important foundation for future educational and interventional efforts.
2. Methods
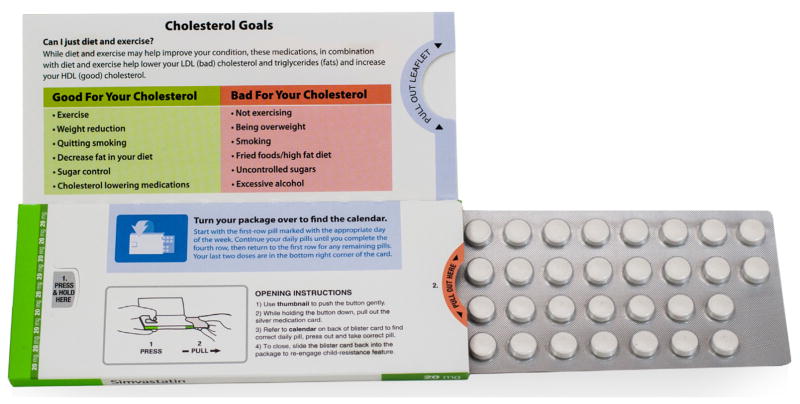
We used baseline data from an ongoing randomized clinical trial conducted at the Durham, North Carolina Veterans Affairs (VA) Medical Center. The trial design has been previously described in detail [12]. In brief, the trial is a two-arm trial with block randomization to ensure a rolling balance between the two arms (intervention vs. usual care). The objective of the trial is to evaluate the effect of a special child-resistant blister packaging that includes a reminder feature of daily labeled blisters and instructions for use (MeadWestvaco Corporations’ pre-filled Dosepak® Express with Optilock technology); the primary outcome of the overarching trial is medication adherence with prescribed statin drugs (Fig. 1). Eligible patients were receiving care at the Durham VA and were at risk for CVD; they had LDL-C levels greater than 130 mg/dL and/or they had less than 80% adherence to their statin medication in the previous 12 months. To determine medication adherence, the medication possession ratio (MPR) was calculated from electronic health record data. The sample for this analysis includes all patients enrolled in the trial that completed a baseline assessment (n = 242).
Fig. 1.
MeadWestvaco Corporations’ DosePak ® Express with Optilock Technology.
A survey assessing patients’ health beliefs about high cholesterol and self-reported medication adherence, among other factors, was administered at the time of trial enrollment. We used this baseline data to evaluate the association between sociodemographic characteristics, health beliefs, and desire to improve cholesterol control.
Patients could endorse up to 7 barriers for taking medications as prescribed, a key factor in cholesterol control, including issues such as, “I delay taking medications at an inconvenient time.” Responses ranged from ‘definitely true’ to ‘definitely false.’ For the purpose of descriptive analysis, ‘definitely’ and ‘probably’ true/false were collapsed into one category (e.g., ‘definitely or probably true’).
The primary outcome measure was patient-reported desire to improve cholesterol control. During the baseline in-person interview, patients were asked, “On a scale of 1–10, where 1 = definitely would not like to and 10 = definitely would like to, how much do you want to improve your cholesterol control?” The outcome measure was collapsed and dichotomized such that respondents with a value of 10 were classified as “Definitely would”, while all other non-missing values (1 through 9) were classified as “May or may not”.
Total cholesterol values were obtained from the laboratory reports in the electronic medical record. To be eligible for this study, all patients were required to have a total cholesterol level of ≥130 mg/dL. For the purpose of this analysis, we defined high cholesterol as a total cholesterol value equal to or above a threshold of 200 mg/dL.
To assess perceived susceptibility for negative health effects related to hyperlipidemia, patients were asked, “If over the next six months you don’t change any of your health behaviors related to high cholesterol, what do you think your chance of having a heart attack in the next year?” Responses ranged from ‘very likely’ to ‘not likely.’ Responses were collapsed and dichotomized as ‘very likely’ versus all other non-missing responses.
To assess patients’ perceived severity of hyperlipidemia, patients were asked, “How serious do you think it is to have high cholesterol?” with responses ranging from ‘very serious’ to ‘not at all serious.’ Responses were collapsed and dichotomized as ‘very serious’ versus all other non-missing responses.
Self-efficacy was assessed with a scale of 1–10: “How confident are you that you can control your cholesterol?” A score of 10 indicated the highest level of confidence. We dichotomized the variable as the highest level of self-efficacy (10) versus lower levels of self-efficacy.
There are gender differences in health beliefs and engagement in health behaviors, such as cholesterol screening [9]. Gender (male vs. female) was included in these analyses. There are also documented racial differences in cholesterol, adherence to medications, and health beliefs [13,14]. Racial information was based on patients’ self-reported race during the baseline survey. The majority of participants reported either white or African American races. Because of the relatively few participants reporting a non-African American minority race, the race measure included in multivariable regression is dichotomized (white vs. minority race).
Marital status is a common proxy measure for social support. Compared to those whom are unmarried, individuals who are married tend to engage in healthier behaviors [8]. This analysis included a binary measure of marital status (married or living with a partner vs. divorced, separated, widowed, or never married).
Having less than a high school education has been associated with lack of screening for hyperlipidemia [15]. Therefore, a dichotomized measure of patient-reported educational attainment was included in analysis (up to 12 years of school vs. more than 12 years of school). There is evidence that low health literacy suggests poor health behaviors; health literacy was assessed using the Rapid Estimate of Adult literacy in Medicine (REALM) test [6,7]. REALM is a 66-item word recognition evaluation to provide a rapid appraisal of health literacy. Low health literacy was a dichotomous variable defined as a REALM score of up to and including 8th grade (≤60 score) versus 9th grade or higher (≥61 score) [6,7]. We also included a binary measure of employment (employed part- or full-time vs. unemployed).
Difficulty paying for care, such as prescription medications, may be a barrier for patients [5]. Using a single-item measure, participants were asked to describe their household’s current financial situation [16]. Possible response options included: ‘after paying the bills, you still have enough money for special things that you want’, ‘you have enough money to pay the bills, but little spare money to buy extra or special things’, ‘you have money to pay the bills, but only because you have to cut back on things’, or ‘you are having difficulty paying the bills no matter what you do.’ A binary measure was created. Patients who reported the latter two categories (e.g., cutting back on things or difficulty paying bills) were coded as having inadequate financial status.
Medication adherence was assessed using a validated eight-item self-reported measure developed by Morisky [17]. Patients were presented with eight items about cholesterol medication taking behaviors and were asked to indicate whether each was true for them. The questions addressed forgetting to take medication, being careless about taking medication, feeling hassled about sticking to a cholesterol medication treatment plan, and stopping medication when feeling better or worse. Responses to these questions were on a 4-point Likert scale ranging from ‘strongly agree’ to ‘strongly disagree’. Patients were also asked how often they had difficulty remembering to take their medicine. Response items to that question were on a 5-point Likert scale ranging from ‘never/rarely’ to ‘all of the time.’ Items were initially summed and then patients were categorized as either adherent or non-adherent [18]. If any of the eight items were missing a response, then the non-adherence variable was also considered missing.
Baseline data were analyzed using Stata 12.1 (StataCorp, College Station, TX, USA) and SAS version 9.2 (SAS Institute, Cary, NC, USA). We used descriptive statistics to summarize patients’ baseline sociodemographic characteristics and patient-reported health beliefs (e.g., frequency (n) and percent (%) for categorical measures; mean and standard deviation (SD) for continuous measures). The primary outcome, desire to control their cholesterol, was evaluated both as an ordinal and binary outcome with multivariable logistic regression while adjusting for patient-level characteristics. Specifically, the models were adjusted a priori for high cholesterol, perceived susceptibility of having a heart attack, perceived seriousness of having high cholesterol, self-efficacy for controlling cholesterol, race, gender, marital status, health literacy, educational attainment, income, employment status, and medication adherence. Patients (n = 17) were excluded from multivariable regression analysis because of missing data. Statistical significance was considered a conventional 95% level. Model results are presented with odds ratios (OR), 95% confidence intervals (CI), and p-values (p).
3. Results
The baseline assessment was completed by 242 patients (Table 1). The mean age was 62.7 years (SD 8.7). Most patients were minority race (63%; n = 153), male (91%; n = 221), married (56%; n = 136), and had more than a high school education (66%; n = 160). Patients had high health literacy skills (66%) and, likely because they were of retirement age, many were not employed (68%; n = 165).
Table 1.
Baseline characteristics (n = 242).
| n | % | |
|---|---|---|
| Demographics | ||
| Age (years), mean (SD) | 62.7 | (8.7) |
| Racea | ||
| Caucasian | 89 | (36.8) |
| American | 153 | (63.2) |
| Gender | ||
| Female | 21 | (8.7) |
| Male | 221 | (91.3) |
| Marital status | ||
| Married/living together | 136 | (56.2) |
| Divorced/separated/widowed/never married | 105 | (43.4) |
| Missing | 1 | (0.4) |
| Education | ||
| Completed ≤12 years of school | 82 | (33.9) |
| Completed > 12 years of school | 160 | (66.1) |
| Low literacy level (REALM score ≦60) | ||
| Yes, low health literacy | 83 | (34.3) |
| No | 159 | (65.7) |
| Employment | ||
| Employed (full-time/part-time/self) | 77 | (31.8) |
| Not employed | 165 | (68.2) |
| Inadequate financial statusb | ||
| Yes | 52 | (21.5) |
| No | 189 | (78.1) |
| Missing | 1 | (0.4) |
| Lab measures | ||
| High cholesterol | ||
| Total cholesterol ≥200 mg/dL | 86 | (35.5) |
| Total cholesterol <200 mg/dL | 155 | (64.0) |
| Missing | 1 | (0.4) |
| Medication adherencec | ||
| Adherent | 75 | (31.0) |
| Not adherent | 167 | (69.0) |
Unless otherwise noted, number (%) with characteristic is shown.
Patients who reported ‘cutting back on things’ or having ‘difficulty paying bills’ were coded as having inadequate financial status.
Medication adherence was assessed using a validated eight-item self-reported measure developed by Morisky [17].
Although 64% (n = 155) of patients perceived high cholesterol to be ‘very serious’, patients were varied regarding their perceived likelihood of having a heart attack in the next year if they failed to change their health behaviors (Table 2). The most commonly endorsed barrier to taking medications was having too much medicine to take (32%, n = 77), followed by forgetting whether or not a particular medication dose has been taken (30%, n = 73). The majority of patients did not think that the instructions for how to take their medications were too complicated to understand (96%, n = 233). On average, patients were highly confident (mean 8.3; SD 2.0) in their ability to control their cholesterol and desired to do so (mean 9.3; SD 1.7) (Table 3).
Table 2.
Description of patient-reported health beliefs (n = 242).
| Identification of health beliefs | |||
|---|---|---|---|
| Perceived susceptibility | If over the next 6 months you don’t change any of your health behaviors related to high cholesterol, what do you think is your chance of having a heart attack in the next year?a | ||
| Very likely | 52 | (21.5) | |
| Likely | 86 | (35.5) | |
| Not likely | 96 | (39.7) | |
| Missing | 8 | (3.3) | |
| Perceived severity | How serious do you think it is to have high cholesterol? | ||
| Very serious | 155 | (64.0) | |
| Serious | 69 | (28.5) | |
| A little serious | 13 | (5.4) | |
| Not at all serious | 2 | (0.8) | |
| Missing | 3 | (1.2) | |
| Perceived barriers | I delay taking medications to avoid having side effects at an inconvenient time. | ||
| Definitely or probably true | 34 | (14.0) | |
| Definitely or probably false | 208 | (86.0) | |
| I get confused about how much medication of each kind to take. | |||
| Definitely or probably true | 21 | (8.7) | |
| Definitely or probably false | 221 | (91.3) | |
| I have too much medication to take | |||
| Definitely or probably true | 77 | (31.8) | |
| Definitely or probably false | 164 | (67.8) | |
| I have trouble remembering what my medications are for. | |||
| Definitely or probably true | 43 | (17.8) | |
| Definitely or probably false | 198 | (81.8) | |
| Missing | 1 | (0.4) | |
| There is no one to help me keep track of when to take my medication. | |||
| Definitely or probably true | 50 | (20.7) | |
| Definitely or probably false | 192 | (79.3) | |
| I forget whether or not I have taken my medication at a particular time. | |||
| Definitely or probably true | 73 | (30.2) | |
| Definitely or probably false | 168 | (69.4) | |
| Missing | 1 | (0.4) | |
| The instructions for how to take my medications are too complicated to understand. | |||
| Definitely or probably true | 9 | (3.7) | |
| Definitely or probably false | 233 | (96.3) | |
| Self-efficacy | On a scale of 1–10, where 1 = not at all confident and 10 = completely confident, how confident are you that you can control your cholesterol? mean (SD) | 8.3 | (2.0) |
| On a scale of 1–10, where 1 = definitely would not like to and 10 = definitely would like to, how much do you want to improve your cholesterol control? mean (SD) (n = 239) | 9.3 | (1.7) | |
Unless otherwise noted, number (%) with characteristic is shown.
Table 3.
Multivariable logistic regression results depicting the association between desire to improve cholesterol control and cholesterol status (n = 225).
| OR | 95% CI | p | |
|---|---|---|---|
| High cholesterol | 0.60 | 0.29–1.25 | 0.170 |
| Non-high cholesterol | Ref | – | – |
| Very likely to have heart attack (susceptibility) | 2.11 | 0.70–6.42 | 0.187 |
| Less than very likely to have heart attack | Ref | – | – |
| Very serious to have high cholesterol (severity) | 2.26 | 1.07–4.78 | 0.032 |
| Less than very serious to have high cholesterol | Ref | – | – |
| Self-efficacy | 4.70 | 2.06–10.74 | <0.001 |
| Minority race | 2.01 | 0.95–4.28 | 0.070 |
| White race | Ref | – | – |
| Male gender | 1.23 | 0.30–5.04 | 0.770 |
| Female gender | Ref | – | – |
| Married or living with partner | 1.64 | 0.77–3.51 | 0.203 |
| Not married or living with partner | Ref | – | – |
| Low health literacy | 1.21 | 0.50–2.91 | 0.671 |
| Average or high health literacy | Ref | – | – |
| Low education (≤12 years of school) | 1.14 | 0.51–2.57 | 0.747 |
| Higher education (>12 years of school) | Ref | – | – |
| Inadequate income | 0.78 | 0.31–1.96 | 0.598 |
| Adequate income | Ref | – | – |
| Employed | 0.77 | 0.36–1.66 | 0.501 |
| Not employed | Ref | – | – |
| Adherent with medications | 1.02 | 0.47–2.23 | 0.960 |
| Non-adherent with medications | Ref | – | – |
In multivariable logistic regression analysis, patients who perceive high cholesterol to be ‘very serious’ have a statistically significant greater odds (OR 2.26, p = 0.032) of desiring to control their total cholesterol. Self-efficacy for cholesterol control was positively associated with the odds of desiring to control cholesterol (OR 4.70, p <0.001). Being of minority race was marginally significantly associated with desire for cholesterol control (p ≤0.1). Having high cholesterol, perceived susceptibility of having a heart attack, gender, marital status, health literacy, educational attainment, income, employment status, and medication adherence were not associated with a desire to improve cholesterol control. Self-rated medication adherence was not associated with self-efficacy for cholesterol control (p = 0.960). Multivariable ordinal logistic regression provided similar results (results not presented).
4. Discussion and conclusions
4.1. Discussion
We found that one factor significantly associated with a desire to improve cholesterol control was a perception of hyperlipidemia as ‘very serious’; 64% of patients perceived high cholesterol to be ‘very serious.’ Since nearly half of patients did not perceive high cholesterol to be very serious, there may be opportunity to educate patients about the potential negative health outcomes associated with high cholesterol, such as heart attack and stroke, and the importance of adherence to medications as a mechanism to improve cholesterol control. We also found that having a high degree of self-efficacy is associated with a desire to improve cholesterol control. Skill- and confidence-building educational programs may also aid patients’ cholesterol control efforts. Strategies to build self-efficacy could include, but are not limited to, motivational interviewing, modeling, and behavioral rewards. These strategies can be employed to improve health behaviors, such as appropriate medication taking.
Moreover, hyperlipidemia is a serious health condition without symptoms, which may make it difficult for patients to recognize the severity of the problem or their susceptibility to it. The need for education is further evidenced by patients’ relatively low perceived susceptibility to negative health outcomes. When queried, 57% of patients reported that they were ‘very likely’ or ‘likely’ to have a heart attack in the next year unless they changed their health behaviors related to high cholesterol.
Additionally, patients identified common barriers to medication adherence. The most frequently cited barriers were having too much medicine to take and/or forgetting to take medication doses at a particular time. There are many existing interventions that may help patients manage their medications including medication synchronization, and reminder smartphone applications, among others. Effort should be made to screen patients for common medication adherence barriers and match patients with tools and strategies to meet their specific challenges. This will not only facilitate better medication adherence but may ultimately result in improved clinical outcomes, such as cholesterol control.
Interestingly, in multivariable regression, having the highest levels of cholesterol was not associated with the odds of desiring to improve control (p = 0.170). Because their levels are high, these patients may be most in need of lifestyle change and medication therapy. However, they may not have a desire to change their behavior. This lack of desire for change is a major barrier to behavior modification. Having a desire to change is an important step in the pre-contemplation and contemplation stages of behavior change. This presents an opportunity to intervene with those patients most at risk, educating them on the potential seriousness and severity of having high cholesterol, including the likelihood of experiencing a negative cardiovascular-related event. Also interesting is that medication adherence was not associated with any of the health beliefs in this study. Medication adherence is a multidimensional behavior with many influencing factors. Because adherence is important for cholesterol control, interventions to align patients’ health beliefs with adherence may be warranted. For example, if a patient reports a high perceived severity and seriousness of cholesterol, but low self-efficacy, this might present an opportunity to build self-efficacy for medication taking behaviors.
Medication management, largely through the use of statins, is a key component of cholesterol control [2]. In this study, patients commonly endorsed barriers to taking their medication as prescribed—feeling as though they have too much medicine to take and/or forgetting whether or not they have taken their medications. Since taking prescriptions is a primary method for reducing LDL-C, there may be opportunities to intervene and simplify medication taking. This could be through medication reconciliation or synchronization programs, providing education and counseling, and equipping patients with behavioral strategies to help them take medications as prescribed. These education and skills-based training opportunities could boost patients’ awareness of the seriousness and severity of high cholesterol, while simultaneously providing tangible skills and tools to overcome barriers and boost their confidence in the their ability to control their cholesterol.
This paper has several limitations. First, we examined baseline differences in sociodemographic characteristics and health beliefs. These factors are time varying and a future, longitudinal analysis might enable a more comprehensive understanding of predictors (rather than associations) with a desire to improve cholesterol control. Because the study sample is a cohort of VA healthcare system users with hyperlipidemia, the generalizability may be limited; the study sample may have lower educational attainment, lower health literacy, and otherwise different characteristics compared to the general U.S. population. Additionally, patients in this sample had voluntarily enrolled in a clinical trial related to cholesterol drug packaging [12]. It is possible that patients who self-select into a trial are different than those who do not. Social desirability bias is also possible. In other words, patients may have felt compelled to report “good behavior.” Lastly, we did not have information about patients’ treatment history (e.g., previous lipid-lowering therapies and/or adverse effects).
4.2. Conclusion
The factors most significantly associated with desire to improve cholesterol control were perceiving hyperlipidemia as ‘very serious’ and self-efficacy in ability to control cholesterol. Since many patients did not perceive elevated cholesterol as a serious health consideration, there may be opportunity to educate patients about potential negative health outcomes associated with hyperlipidemia.
4.3. Practice implications
Despite these limitations, this study has clinical value. It includes patient-reported measures of health beliefs and perceptions that cannot be obtained using administrative or electronic health record data alone. Our findings have important practical applications. Among this cohort of patients with high cholesterol, the relatively low perception of high cholesterol as being a serious health problem and lack of desire to improve cholesterol control provide opportunities ripe for patient engagement and tailored education. Providing an individual needs assessment, evaluating health beliefs related to high cholesterol and barriers to medication taking and lifestyle change might be an important first step in treatment planning for patients with high cholesterol. Primary care clinics may provide an appropriate setting for the evaluation of health beliefs and providing education about the importance of medication to control cholesterol. Similarly, community-based pharmacies may afford the opportunity to stress the importance of proper medication taking behaviors at a critical point in the adherence process.
Acknowledgments
This project was funded by WestRock/MeadWestvaco (MWV XNV 21-158). Dr. Zullig (CDA 13-025) was supported by VA Health Services Research and Development Career Development Award. Dr. Bosworth was supported by a research career scientist award from VA Health Service Research and Development (VA HSR&D 08-027). Statistical guidance was provided by Duke Translational Medical Institute Biostatistics Core, funded in part with the Duke CTSA grant (UL1TR001117).
Footnotes
Conflict of interest
The authors have no conflicts of interest to disclose. The content is solely the responsibility of the authors and does not necessarily reflect the position or policy of Duke University, the U.S. Department of Veterans Affairs, or the U.S. government.
References
- 1.Nelson RH. Hyperlipidemia as a risk factor for cardiovascular disease. Prim Care. 2013;40(1):195–211. doi: 10.1016/j.pop.2012.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stone NJ, Robinson J, Lichtenstein AH, Bairey Merz CN, Lloyd-Jones DM, Blum CB, McBride P, Eckel RH, Schwartz JS, Goldberg AC, et al. 2013 ACC/ AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American college of cardiology/ American heart association task force on practice guidelines. J Am Coll Cardiol. 2013 doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Schupf N, Costa R, Luchsinger J, Tang MX, Lee JH, Mayeux R. Relationship between plasma lipids and all-cause mortality in nondemented elderly. J Am Geriatr Soc. 2005;53(2):219–226. doi: 10.1111/j.1532-5415.2005.53106.x. [DOI] [PubMed] [Google Scholar]
- 4.Johnson ML, Pietz K, Battleman DS, Beyth RJ. Therapeutic goal attainment in patients with hypertension and dyslipidemia. Med Care. 2006;44(1):39–46. doi: 10.1097/01.mlr.0000188982.25397.37. [DOI] [PubMed] [Google Scholar]
- 5.Carr-Lopez SM, Shek A, Lastimosa J, Patel RA, Woelfel JA, Galal SM, Gundersen B. Medication adherence behaviors of medicare beneficiaries. Patient Prefer Adher. 2014;8:1277–1284. doi: 10.2147/PPA.S64825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19(12):1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DeWalt DA, Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124(Suppl 3):S265–S274. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- 8.Trivedi RB, Ayotte B, Edelman D, Bosworth HB. The association of emotional well-being and marital status with treatment adherence among patients with hypertension. J Behav Med. 2008;31(6):489–497. doi: 10.1007/s10865-008-9173-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vaidya V, Partha G, Karmakar M. Gender differences in utilization of preventive care services in the United States. J Womens Health (2002) 2012;21(2):140–145. doi: 10.1089/jwh.2011.2876. [DOI] [PubMed] [Google Scholar]
- 10.Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. John Wiley & Sons; 2008. [Google Scholar]
- 11.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 12.Zullig LL, Pathman J, Melnyk SD, Brown JN, Sanders LL, Koropchak C, Howard T, Danus S, McCant F, Bosworth HB. A protocol to evaluate the efficacy, perceptions, and cost of a cholesterol packaging approach to improve medication adherence. Contemp Clin Trials. 2014;39(1):106–112. doi: 10.1016/j.cct.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Ayanian JZ, Landon BE, Newhouse JP, Zaslavsky AM. Racial and ethnic disparities among enrollees in Medicare Advantage plans. N Engl J Med. 2014;371(24):2288–2297. doi: 10.1056/NEJMsa1407273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. 2010;140(2):226–235. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 15.Merkin SS, Karlamangla A, Crimmins E, Charette SL, Hayward M, Kim JK, Koretz B, Seeman T. Education differentials by race and ethnicity in the diagnosis and management of hypercholesterolemia: a national sample of U. S. adults (NHANES 1999–2002) Int J Public Health. 2009;54(3):166–174. doi: 10.1007/s00038-008-7030-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams RB, Barefoot JC, Califf RM, Haney TL, Saunders WB, Pryor DB, Hlatky MA, Siegler IC, Mark DB. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. J Am Med Assoc. 1992;267(4):520–524. [PubMed] [Google Scholar]
- 17.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Thorpe CT, Bryson CL, Maciejewski ML, Bosworth HB. Medication acquisition and self-reported adherence in veterans with hypertension. Med Care. 2009;47(4):474–481. doi: 10.1097/mlr.0b013e31818e7d4d. [DOI] [PubMed] [Google Scholar]