Abstract
Background
Measurement of basal metabolic rate (BMR) is suggested as a tool to estimate energy requirements. Therefore, BMR prediction equations have been developed in multiple populations because indirect calorimetry is not always feasible. However, there is a paucity of data on BMR measured in overweight and obese adults living in Asia and equations developed for this group of interest. The aim of this study was to develop a new BMR prediction equation for Chinese adults applicable for a large BMI range and compare it with commonly used prediction equations.
Methods
Subjects were 121 men and 111 women (age: 21–67 years, BMI: 16–41 kg/m2). Height, weight, and BMR were measured. Continuous open-circuit indirect calorimetry using a ventilated hood system for 30 min was used to measure BMR. A regression equation was derived using stepwise regression and accuracy was compared to 6 existing equations (Harris-Benedict, Henry, Liu, Yang, Owen and Mifflin). Additionally, the newly derived equation was cross-validated in a separate group of 70 Chinese subjects (26 men and 44 women, age: 21–69 years, BMI: 17–39 kg/m2).
Results
The equation developed from our data was: BMR (kJ/d) = 52.6 x weight (kg) + 828 x gender + 1960 (women = 0, men = 1; R2 = 0.81). The accuracy rate (within 10 % accurate) was 78 % which compared well to Owen (70 %), Henry (67 %), Mifflin (67 %), Liu (58 %), Harris-Benedict (45 %) and Yang (37 %) for the whole range of BMI. For a BMI greater than 23, the Singapore equation reached an accuracy rate of 76 %. Cross-validation proved an accuracy rate of 80 %.
Conclusions
To date, the newly developed Singapore equation is the most accurate BMR prediction equation in Chinese and is applicable for use in a large BMI range including those overweight and obese.
Introduction
Since the classical experiments by Lavoisier and Laplace in 1783, energy metabolism remains the central tenant of human nutrition. Basal metabolic rate (BMR) was introduced to describe energy expended at rest in contrast to energy expended during physical activity and has been described as the “minimal rate of energy expenditure compatible with life” [1]. It represents the energy required for maintenance, necessary to sustain and maintain the integrity of vital functions and is mainly determined by the amount of lean tissue. Generally, BMR represents 60–80 % of total daily energy expenditure (TDEE) [2, 3].
In the 1985 FAO/WHO/UNU report on human energy and protein requirements, the use of energy expenditure rather than food intake was proposed to calculate energy requirements and additionally, it was proposed that TDEE can be expressed as multiples of BMR, defined as physical activity level (PAL) [3–7]. This approach to estimate energy requirements necessitates the accurate estimation of BMR in populations of different ethnicities and body weight and living under various environmental conditions.
Indirect calorimetry, which is based on the measurement of oxygen consumption and carbon dioxide production, is the preferred method to accurately assess BMR. It requires subjects to be at rest while being awake, fasted for at least 10 h, in a supine position, and under thermoneutral conditions [8]. Measurement equipment can be costly, is not widely available, requires trained personnel, and can be time consuming. Therefore, indirect calorimetry is not feasible in daily practice. Consequently, predictive equations to estimate energy requirements are the order of the day in dietetic practice and for most clinical and inpatient care. Commonly, the prediction equations are based on readily available physical measures such as age, sex, height and weight [9].
Among the first widely used prediction equations were the equations developed by Harris and Benedict (HB) in 1918 and the FAO/WHO/UNU recommended prediction equations based on the 1985 Schofield database [10, 11]. Over the years, several studies have shown that these equations overestimate BMR in tropical populations [12–17] because in tropical populations BMR is 15–20 % lower compared to Europeans and Americans [18–20]. This explains the overestimation by the Schofield and HB equations because respectively 87 % and 100 % of the data came from Caucasian men and women. Likewise, it has been shown that these equations overestimate BMR in overweight and obese populations [21–23].
Consequently, improved equations have been developed in an attempt to improve estimates of BMR and reflect racial variations [12, 14, 24–29]. Among these are the EU recommended Henry equations, and the equations of Liu et al. and Yang et al. [8, 25, 26], which have in common that they have been developed in predominantly healthy Asian subjects. Similarly, Mifflin et al. and Owen et al. have reported improved predictive equations for overweight and obese Caucasian subjects [30–32]. However, there is a paucity of data on BMR measured in overweight and obese adults living in Asia and equations developed for this group is of interest.
Since the prevalence of overweight and obesity has been rising globally since the 1980s with no exception in Asia, there is an increased need for accurate assessment of daily energy requirements to plan for healthy weight management or appropriate weight loss [33–35]. Current prediction equations for BMR to estimate energy requirements have not been developed specifically for the overweight and obese Chinese population.
Therefore, the first objective of this study was to develop BMR predictive equations in Chinese adults applicable for a large BMI range. The second aim was to compare the accuracy of the newly developed equations with a) commonly used prediction equation: Harris-Benedict equation, b) prediction equations suitable for a broader ethnic range: Henry equations, Liu equation and Yang equation and c) prediction equations advised for use in overweight and obese subjects: Mifflin and Owen equation. Thirdly, the newly derived prediction equation was cross-validated in a separate group of Chinese subjects to confirm the applicability.
Subjects and methods
Subjects
A total of 232 Singaporean Chinese subjects (121 men and 111 women, age: 21–67 years, BMI: 16–41 kg/m2) participated in the cross-sectional study. These were used to generate the regression equation. A separate set of 70 Singaporean Chinese subjects (26 men and 44 women, age: 21–69 years, BMI: 17–39 kg/m2) was used to cross-validate the new equation. They underwent a pre-participation screening that included the completion of a questionnaire on general health. Subjects were of Chinese descent, in good health, not using medication (except for contraception), were non-smokers and at most moderate alcohol consumers. They were weight stable as defined by a weight change <3 kg for at least 6 months prior to the study. The study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures were approved by the National Healthcare Group Domain-Specific Review Board (2013/00783). Written informed consent was obtained from all participants. This trial was registered at www.anzctr.org.au as ACTRN12614000643673.
Study design
Subjects were required to undergo a 12 h overnight fast and refrain from intensive physical activity for 24 h prior to the measurement. On the test day, subjects reported to the Clinical Nutrition Research Centre at 0830 h. They were instructed to travel by public transport or by car and use the elevator to avoid physical activity that would increase BMR. Subjects were then allowed to lie supine quietly and relax for 15 min before measurement of BMR via indirect calorimetry commenced. Subsequently, anthropometric measurements were performed. All measurements were performed by two researchers experienced in the field of nutrition and energetics.
Basal metabolic rate
BMR was measured (BMRm) continuously by open-circuit indirect calorimetry using a ventilated hood system (Quark CPET, COSMED, Rome, Italy) for 30 min. For this, a transparent Perspex ventilated hood was placed over the subjects head, through which outside air was drawn by a pump. The flow rate (20–40 L/min) was measured and adjusted to keep the difference in carbon dioxide readings between inspired and expired air within the range of 0.8–1.2 %. A small sample of air leaving the hood was analysed for oxygen (O2) and carbon dioxide (CO2) by a paramagnetic analyser and infrared analyser respectively. Calibration of flow and gas analysers were calibrated with dried standard gas mixture (16.01 % O2, 4.98 % CO2) and dried atmospheric air (20.93 % O2, 0.03 % CO2). The validity of the ventilated hood system was further tested by ethanol combustion tests conducted biweekly. All measurements were carried out in a quiet room with an ambient temperature between 23–25 degrees Celsius, barometric pressure of 750–770 mmHg and constant humidity of 60 %. During the measurements, subjects were lying in a semi-supine position, quiet, motionless and were kept awake. O2 and CO2 concentrations of the outflowing air and the airflow rate through the hood were measured every 5-s to obtain oxygen consumption and carbon dioxide production. To eliminate effects of subject habituation to the test procedure, the respiratory measurements during the first 5 min were discarded. Only steady-state periods of measurements of 10 min were used to calculate BMR. BMR was calculated from oxygen consumption and carbon dioxide production by the Weir formula [36]. In addition to measured values, BMR was predicted (BMRp) by the Harris-Benedict, Henry, Liu, Yang, Owen and Mifflin equations (Table 1) [8, 11, 25, 26, 30–32].
Table 1.
Prediction equations to calculate BMR (kJ/d)
| Equations | Age | Men | Women |
|---|---|---|---|
| Singapore | Adult | 52.6 W + 2788 | 52.6 W + 1960 |
| HB [11] | Adult | 278 + 57.5 W + 20.9H– 28.2A | 2783 + 40.0 W + 7.7H– 19.5A |
| Henry [8] | 18–30 | 60.0 W + 13.1H + 473 | 43.3 W + 25.7H – 1180 |
| 30–60 | 47.6 W + 22.6H – 574 | 34.2 W + 21.0H – 49 | |
| 60–70 | 47.8 W + 22.6H – 1070 | 35.6 W + 17.6H + 45 | |
| Liu [26] | Adult | 58.1 W + 17.4H – 14.4A + 227 | 58.1 W + 17.4H – 14.4A – 243 |
| Yang [25] | Adult | 89 W + 877 | 89 W + 277 |
| Mifflin [30] | Adult | 41.8 W + 26.2H -20.6A +21 | 41.8 W + 26.2H -20.6A – 674 |
| Owen [31, 32] | Adult | 42.7 W + 3678 | 30.0 W + 3326 |
W weight (kg), G gender (men = 1, women = 0), H height (cm), A age (years), HB Harris and Benedict
Anthropometric measurements and body composition
Height was measured to the nearest 0.1 cm using a calibrated electronic weighing and measuring station (Seca 763, Medical Scales and Measuring System, Hamburg, Germany) and weight to the nearest 0.001 kg using a calibrated scale (Life Measurement Corporation, Inc, Concord, CA, USA). Both height and weight measurements were taken twice, and the mean of the two measurements was recorded. BMI was calculated as weight (kg) divided by height (m) squared. The conventional cut-off point of BMI greater than 25.0 to describe overweight and obesity in Caucasians does not apply in Asians. Hence, in this study a BMI greater than 23.0 will be used to define overweight and greater than 27.5 to define obesity [37].
Statistical analysis
Statistical analysis was performed using Microsoft Excel 2010. Statistical significance was set at P < 0.05 (two-sided test). All results were expressed as mean ± standard deviation. Multiple stepwise regression analysis was used to derive the new prediction equation (Singapore equation) to estimate BMR based on weight, height, age and gender as independent variables. Pearson’s coefficient of determination (R2) and the residual standard deviation (RD) were calculated as measures of goodness of fit between the measured and predicted regression equations used. The degree of agreement between the predicted and measured BMR was evaluated by Bland-Altman limits of agreement analysis [38]. The limits of agreement were defined as the mean difference ±2 standard deviations. The estimated accuracy was defined as the percentage of the subjects whose BMRp was within ±10 % of BMRm. Overestimation and underestimation were defined as >10 % and <10 % of BMRm, respectively [21]. Estimated accuracy was used to cross-validate the newly derived equation in an independent group of 70 subjects. Pearson’s coefficient of determination was calculated as measure of goodness of fit between the BMRm and BMRp from the newly derived equation.
Results
Subject characteristics for the separate cross-sectional study and cross-validation study are summarised in Table 2a and b and BMI distribution is shown in Fig. 1. There were no significant differences between men and women for age and BMI.
Table 2.
Subject characteristics (mean ± SD)
| a. | |||
| cross-sectional study | Men (n = 121) | Women (n = 111) | Total (n = 232) (range) |
| Age (years) | 32.3 ± 9.9 | 33.4 ± 11.2 | 32.8 ± 10.5 (21.6–66.8) |
| Weight (kg) | 79.2 ± 14.9 | 66.1 ± 16.1 | 72.9 ± 16.8 (39.3–113.1) |
| Height (cm) | 171.7 ± 5.9 | 159.9 ± 6.2 | 166.1 ± 8.5 (147.4–189.3) |
| BMI (kg/m2) | 26.9 ± 4.9 | 25.8 ± 5.9 | 26.4 ± 5.4 (16.4–40.8) |
| BMR (kJ/d) | 6958 ± 1033 | 5439 ± 908 | 6230 ± 1234 (3615–10213) |
| b. | |||
| cross-validation study | Men (n = 26) | Women (n = 44) | Total (n = 70) (range) |
| Age (years) | 28.2 ± 6.3 | 28.8 ± 10.2 | 28.6 ± 10.45 (21.6–66.8) |
| Weight (kg) | 72.1 ± 13.3 | 59.7 ± 15.6 | 64.3 ± 15.8 (40.7–104.6) |
| Height (cm) | 173.4 ± 6.3 | 162.3 ± 5.3 | 166.4 ± 7.8 (151.9–185.5) |
| BMI (kg/m2) | 24.0 ± 3.9 | 22.7 ± 5.8 | 23.2 ± 5.2 (16.6–38.9) |
| BMR (kJ/d) | 6473 ± 941 | 5075 ± 870 | 5594 ± 1121 (3774–8301) |
BMI body mass index, BMR basal metabolic rate
Fig. 1.
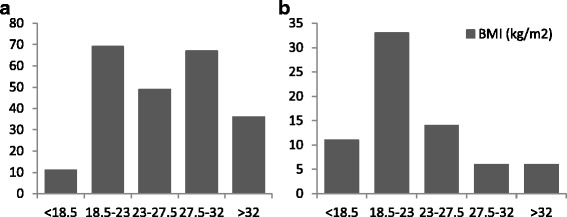
Subject distribution according to body mass index (BMI) of a cross-sectional study (n = 232) and b cross-validation study (n = 70)
Multiple stepwise regression analysis was used to determine which variables independently contributed to the prediction of BMR. Weight, height and gender were significantly correlated to BMR; however height was excluded following stepwise regression analysis resulting in the following BMR prediction equation: BMR (kJ/d) = 52.6 x weight (kg) + 828 x gender + 1960 (women = 0, men = 1) + 468.36 (R 2 = 0.81, P < 0.001) (Table 1). Inclusion of weight resulted in a RD of 656 (kJ/d) and inclusion of gender improved RD to 534 (kJ/d); inclusion of either or both height and age did not improve RD.
Predicted BMR values in the cross-sectional and cross-validation study by all prediction equations and the differences with measured BMR values are summarised in Table 3a and b. The second column shows the mean difference between BMRm and BMRp with a positive value being an overestimation by the prediction equation. Paired t-tests were used to compare the differences between BMRm in both studies and BMRp using the prediction equations. This was not applicable for the predicted BMR by the Singapore equation in the cross-sectional study as by design of the study. The validation study showed that only BMRp by the Singapore equation showed no significant difference from BMRm. Significant correlations were found between BMRm and BMRp for all equations. For the cross-validation study, the individual differences between measured and predicted BMR plotted against the average of the measured BMR and predicted BMR are shown in Fig. 2. The limits of agreement were wide for all equations while only the Singapore and Liu’s equations did not show directional bias.
Table 3.
Mean predicted BMR and difference with measured BMR
| Mean ± SD (kJ/d) | Bias ± SD (kJ/d) | P value in paired t-test | R2 | Limits of Agreement (kJ/d) | |
|---|---|---|---|---|---|
| a. | |||||
| Cross-sectional study (n = 232) | |||||
| Singapore | 6230 ± 1115 | -3 ± 534 | NA | 0.81* | -1070 to 1064 |
| HB [11] | 6777 ± 1124 | 545 ± 607 | <0.0001 | 0.76* | -669 to 1759 |
| Henry [8] | 6362 ± 1003 | 131 ± 655 | <0.005 | 0.72* | -1179 to1440 |
| Liu [26] | 6558 ± 1187 | 426 ± 745 | <0.0001 | 0.79* | -718 to 1570 |
| Mifflin [30] | 6397 ± 1080 | 165 ± 621 | <0.0001 | 0.74* | -1076 to 1406 |
| Owen [31, 32] | 6214 ± 1036 | -17 ± 604 | 0.66 | 0.79* | -1225 to 1190 |
| Yang [25] | 7028 ± 1638 | 850 ± 786 | <0.0001 | 0.79* | -721 to 2421 |
| b. | |||||
| Cross-validation study (n = 70) | |||||
| Singapore | 5651 ± 1055 | 56 ± 407 | 0.25 | 0.87* | -759 to 870 |
| HB [11] | 6356 ± 998 | 761 ± 413 | <0.0001 | 0.87* | -65 to 1586 |
| Henry [8] | 6029 ± 980 | 434 ± 469 | <0.0001 | 0.83* | -503 to 1371 |
| Liu [26] | 6154 ± 1107 | 559 ± 381 | <0.0001 | 0.89* | -204 to 1322 |
| Mifflin [30] | 6030 ± 1000 | 435 ± 429 | <0.0001 | 0.85* | -424 to 1293 |
| Owen [31, 32] | 5722 ± 934 | 126 ± 516 | 0.044 | 0.79* | -907 to 1159 |
| Yang [25] | 6225 ± 1545 | 630 ± 668 | <0.0001 | 0.85* | -707 to 1967 |
*P < 0.001
HB Harris and Benedict
Fig. 2.
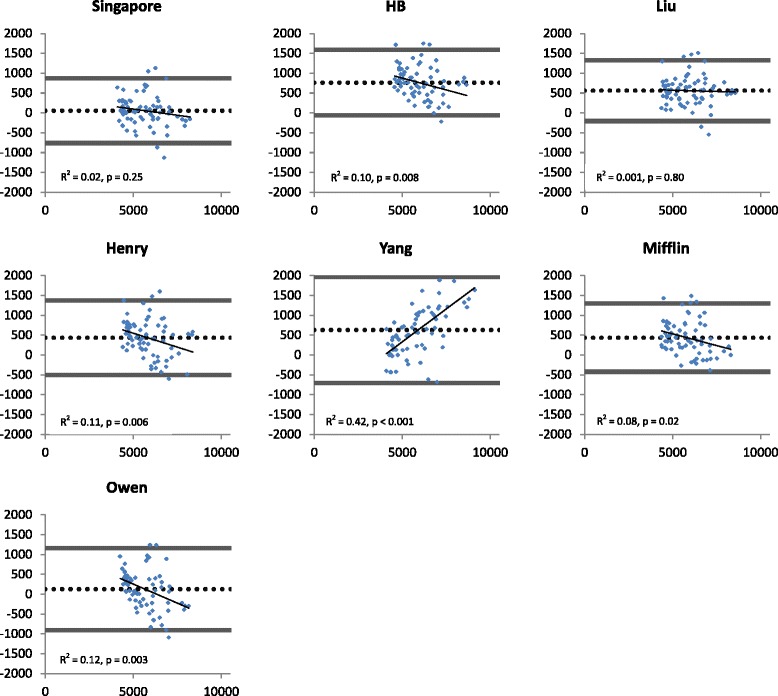
Bland-Altman plots describing agreement between measured BMR and predicted BMR from 7 equations in the cross-validation study (n = 70). Delta BMRp – BMRm (kJ/d) is plotted against the average of BMRm and BMRp (kJ/d). Reference lines represent the mean error (dotted line) of the prediction equation (bias) and the limits of agreement (±2 SD) (solid line). Regression lines, their coefficient of determination and p-value for the slope are provided. BMRp = predicted basal metabolic rate, BMRm = measured basal metabolic rate, HB = Harris and Benedict
Table 4 summarises percentages of accurate (accuracy rate), underestimated and overestimated BMR predictions by all equations for all subjects of the cross-sectional and cross-validation study and subcategorized for a BMI smaller and greater than 23 for the cross-sectional study. A value is considered accurate when the difference between BMRp and BMRm is not greater than ± 10 %. In the cross-validation part of the study, the accuracy rate for the newly derived prediction equation reached 80 %, while under- and overestimation were respectively 4 % and 16 %. Goodness of fit between BMRm and BMRp from the new equation was good (R 2 = 0.87).
Table 4.
The percentage of accurate, underestimated and overestimated BMR predictions for all subjects and subcategorized for a BMI smaller and greater than 23, BMR prediction equations are ranked according to overall accuracy for the cross-sectional study (n = 232) and underestimated and overestimated BMR predictions for all subjects of the cross-validation study (n = 70)
| Cross-sectional study | Cross-validation study | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| underestimation | accurate within ± 10 % | overestimation | under | accurate | over | |||||||
| All | ≤23 | >23 | All | ≤23 | >23 | All | ≤23 | >23 | All | All | All | |
| Singapore | 9 % | 6 % | 11 % | 78 % | 80 % | 76 % | 13 % | 14 % | 13 % | 4 % | 80 % | 16 % |
| Owen [31, 32] | 14 % | 2 % | 20 % | 70 % | 74 % | 68 % | 16 % | 24 % | 12 % | 9 % | 70 % | 21 % |
| Henry [8] | 9 % | 2 % | 13 % | 67 % | 59 % | 72 % | 24 % | 39 % | 16 % | 2 % | 59 % | 41 % |
| Mifflin [30] | 9 % | 1 % | 13 % | 67 % | 61 % | 70 % | 24 % | 38 % | 16 % | 1 % | 59 % | 41 % |
| Liu [26] | 3 % | 0 % | 5 % | 58 % | 63 % | 56 % | 38 % | 37 % | 39 % | 0 % | 49 % | 51 % |
| HB [11] | 4 % | 1 % | 6 % | 45 % | 33 % | 52 % | 50 % | 66 % | 42 % | 0 % | 37 % | 63 % |
| Yang [25] | 2 % | 4 % | 1 % | 37 % | 69 % | 20 % | 61 % | 27 % | 79 % | 4 % | 44 % | 56 % |
BMR basal metabolic rate, BMI body mass index (kg/m2), HB Harris and Benedict
Discussion
Measuring basal metabolic rate in a group of Chinese adults allowed us to develop an accurate BMR prediction equation (Singapore equation) applicable for a large BMI range including overweight and obese. The equation, based on weight and gender, proved to have a high rate of accurate BMR predictions which was confirmed in a cross-validation study.
Basal metabolic rate is defined as the energy required to sustain and maintain the integrity of vital functions or the minimal rate of energy expenditure compatible with life [1]. In literature, controversy exists whether measurement conditions meet BMR requirements or provide resting metabolic rate [39]. In our study BMR was measured using indirect calorimetry under the essential standard conditions requiring subjects to be at rest while being awake, fasted for at least 10 h, in a supine position, and under thermoneutral conditions [8]. An overnight stay at the research centre before the measurement is sometimes suggested but is often not practical. The newly developed Singapore equation based on these measurements estimated BMR accurately in almost 80 % of the subjects across the wide BMI range, which was confirmed in the cross-validation population. The Singapore equation can now be used to estimate daily energy requirements in Chinese overweight and obese adults to plan for healthy weight management or appropriate weight loss.
Previously, the equations of Henry, Liu and Yang were developed to improve estimates of BMR and reflect ethnic variations. Compared to the Schofield database, the Henry equations contained a larger number of people from the tropics and they excluded the Italian subjects from the Schofield database [8]. The European Food Safety Authority recommends the use of the Henry equations to predict BMR in all 27 countries of the European Union [40]. In our Chinese study population, the Henry equations showed a small overestimation which ranked 3rd lowest (131 kJ/d) and showed the 3rd highest accuracy rate (67 %) on BMR predictions in the cross-sectional study and similar in the validation study. Additionally, Henry’s equations showed an improvement in accuracy rate in subjects with a BMI above 23. The equation from Liu et al. was developed in 223 healthy Chinese adults within normal limits for body weight [26] and has been recommended to predict BMR in Chinese [14–16] while Yang’s equation was developed in 165 normal weight Chinese subjects [25]. Though, in our Chinese study population both equations overestimated BMR while they were accurate in 58 % (Liu) and only 37 % (yang) of the subjects, and performed equally in the validation study. The equation by Liu et al. showed an even accuracy rate across the BMI range in contrast to Yang’s equation which decreased to 20 % for overweight and obese subjects but improved to 69 % (3rd highest) in normal weight subjects; in line with their own conclusions [25]. In comparison, the Harris-Benedict equation showed an average overestimation of 545 kJ/d while the BMR prediction was accurate in 45 % of the subjects. Since, the Harris-Benedict equations is based on gender, height, weight and age and developed in only Caucasian subjects, the overestimation is to be expected [11, 22].
For overweight and obese populations Mifflin’s and Owen’s equations have been advised to be used in respectively American and Chinese [21, 22]. The Mifflin equation was developed in 498 normal and obese Americans while the Owen equation was developed from a group of Caucasian, Negro, and Oriental subjects [30–32]. Our results showed a 4th lowest overestimation for Mifflin’s equation (165 kJ/d) and an average underestimation of BMR by 17 kJ/d for Owen’s equation in our Chinese population while accuracy rates were ranked: 3rd highest for Mifflin’s and 2nd highest for Owen’s equation. Their accuracy rates stayed the same or increased slightly in overweight and obese compared to normal weight subjects which could be explained by the inclusion of such subjects in their studies. They performed correspondingly in the validation study, where Owen’s equation had the 2nd lowest overestimation and the 2nd highest accuracy rate. Previously, Song et al. found an accuracy of 73 % by Owen’s equation for Chinese with a BMI range of 18.5–30 which is similar to the 70 % we found. They concluded that the equation of Owen provided a valid estimation of BMR in Singaporean Chinese men at group level, though critically claimed that the Owen equation displayed wide limits of agreement and directional bias across the range of BMR [22].
In summary, the results showed that BMR predictions by the Singapore equation as well as the equations by Owen et al., Henry et al. and Mifflin et al. had a low bias towards the measured BMR and were accurate around 70 % or as high as 80 % (Singapore equation) of the time. Furthermore, the results confirm that population specific prediction equations with respect to ethnicity and body type are necessary [12–16, 21–23].
The Singapore equation is limited to their derivation from our study population and the clinical utility can only be assessed by testing in other Chinese populations. Though, a cross-validation confirmed the accuracy and applicability for a large BMI range in an independent subject group with a similar wide BMI and age range. The Singapore equation did not show a significant directional bias, however it is assumed that the use of body composition could improve BMR estimation. However, therefore the Singapore equation is simple to use as it is solely based on body weight and gender. In addition, the equation confirmed that BMR is highly correlated with body weight [3] while the addition of other routinely available values (height and age) did not contribute significantly to the accuracy of predicting BMR. The strength of the newly developed Singapore equation lies in the direct practical and clinical use in a large BMI range including overweight and Chinese adults. It is important to note that BMR is the major component of TDEE; however, accurately estimating physical activity plays a role in estimating total daily energy expenditure and thus daily energy requirements.
Conclusion
The newly developed Singapore equation reached the highest accuracy in predicting BMR in normal weight, overweight and obese Chinese Singaporeans when compared to other prediction equations, which was confirmed with a cross-validation in a separate study population.
The Singapore equation developed in the present study is the most appropriate for predicting BMR in Chinese and is applicable in a broad BMI range including overweight and obese. Their utility will be further enhanced if the equations are shown to be valid in Chinese living in other regions of Asia.
Acknowledgements
The authors would like to thank Xinyan Bi, Yi Ting Loo and Siang Wee Lim for their contributions.
Funding
The research was supported by the Agency for Science, Technology and Research (A*STAR), Singapore.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
NXW and WSK carried out the anthropometric and basal metabolic rate measurements. SGC performed the statistical analysis and drafted the manuscript. CJH conceived of the study, and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable
Ethics approval and consent to participate
The study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures were approved by the National Healthcare Group Domain-Specific Review Board (2013/00783). Written informed consent was obtained from all participants. This trial was registered at www.anzctr.org.au as ACTRN12614000643673.
Names for PubMed indexing
Camps SG, Wang NX, Tan WSK, Henry CJ
Abbreviations
- BMI
Body mass index
- BMR
Basal metabolic rate
- BMRm
Measured basal metabolic rate
- BMRp
Predicted basal metabolic rate
- PAL
Physical activity level
- TDEE
Total daily energy expenditure
- TEE
Total energy expenditure
Contributor Information
Stefan G. Camps, Email: Stefan_camps@sics.a-star.edu.sg
Nan Xin Wang, Email: wang_nan_xin@sics.a-star.edu.sg.
Wei Shuan Kimberly Tan, Email: kimberly_tan@sics.a-star.edu.sg.
C. Jeyakumar Henry, Phone: +65 6407 0793, Email: jeya_henry@sics.a-star.edu.sg.
References
- 1.Mitchell HH. Comparative Nutrition of Man and Domestic Animals. New York: Academic; 1962. pp. 3–90. [Google Scholar]
- 2.Black AE, Coward WA, Cole TJ, Prentice AM. Human energy expenditure in affluent societies: an analysis of 574 doubly-labelled water measurements. Eur J Clin Nutr. 1996;50:72–92. [PubMed] [Google Scholar]
- 3.Adriaens MP, Schoffelen PF, Westerterp KR. Intra-individual variation of basal metabolic rate and the influence of daily habitual physical activity before testing. Br J Nutr. 2003;90:419–423. doi: 10.1079/BJN2003895. [DOI] [PubMed] [Google Scholar]
- 4.Joint FAO/WHO/UNU Expert Consultation. Energy and protein requirements. Report of a joint FAO/WHO/UNU Expert Consultation. World Health Organ Tech Rep Ser. 1985;724:1–206. [PubMed]
- 5.Rising R, Harper IT, Fontvielle AM, Ferraro RT, Spraul M, Ravussin E. Determinants of total daily energy expenditure: variability in physical activity. Am J Clin Nutr. 1994;59:800–804. doi: 10.1093/ajcn/59.4.800. [DOI] [PubMed] [Google Scholar]
- 6.Westerterp KR. Impacts of vigorous and non-vigorous activity on daily energy expenditure. Proc Nutr Soc. 2003;62:645–650. doi: 10.1079/PNS2003279. [DOI] [PubMed] [Google Scholar]
- 7.Shetty P. Energy requirements of adults. Public Health Nutr. 2005;8:994–1009. doi: 10.1079/phn2005792. [DOI] [PubMed] [Google Scholar]
- 8.Henry CJ. Basal metabolic rate studies in humans: measurement and development of new equations. Public Health Nutr. 2005;8:1133–1152. doi: 10.1079/PHN2005801. [DOI] [PubMed] [Google Scholar]
- 9.da Rocha EE, Alves VG, da Fonseca RB. Indirect calorimetry: methodology, instruments and clinical application. Curr Opin Clin Nutr Metab Care. 2006;9:247–256. doi: 10.1097/01.mco.0000222107.15548.f5. [DOI] [PubMed] [Google Scholar]
- 10.Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985;39(Suppl 1):5–41. [PubMed] [Google Scholar]
- 11.Harris JA, Benedict FG. A Biometric Study of Human Basal Metabolism. Proc Natl Acad Sci U S A. 1918;4:370–373. doi: 10.1073/pnas.4.12.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henry CJ, Rees DG. New predictive equations for the estimation of basal metabolic rate in tropical peoples. Eur J Clin Nutr. 1991;45:177–185. [PubMed] [Google Scholar]
- 13.Tseng CK, Hsu HS, Ho CT, Huang HY, Liu CS, Lin CC, Lin WY. Predictive equation of resting energy expenditure in obese adult Taiwanese. Obes Res Clin Pract. 2011;5:e267–360. doi: 10.1016/j.orcp.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 14.Leung R, Woo J, Chan D, Tang N. Validation of prediction equations for basal metabolic rate in chinese subjects. Eur J Clin Nutr. 2000;54:551–554. doi: 10.1038/sj.ejcn.1601054. [DOI] [PubMed] [Google Scholar]
- 15.Case KO, Brahler CJ, Heiss C. Resting energy expenditures in Asian women measured by indirect calorimetry are lower than expenditures calculated from prediction equations. J Am Diet Assoc. 1997;97:1288–1292. doi: 10.1016/S0002-8223(97)00308-8. [DOI] [PubMed] [Google Scholar]
- 16.Rao ZY, Wu XT, Liang BM, Wang MY, Hu W. Comparison of five equations for estimating resting energy expenditure in Chinese young, normal weight healthy adults. Eur J Med Res. 2012;17:26. doi: 10.1186/2047-783X-17-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooper JA, Manini TM, Paton CM, Yamada Y, Everhart JE, Cummings S, Mackey DC, Newman AB, Glynn NW, Tylavsky F, et al. Longitudinal change in energy expenditure and effects on energy requirements of the elderly. Nutr J. 2013;12:73. doi: 10.1186/1475-2891-12-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Boer JO, van Es AJ, Voorrips LE, Blokstra F, Vogt JE. Energy metabolism and requirements in different ethnic groups. Eur J Clin Nutr. 1988;42:983–997. [PubMed] [Google Scholar]
- 19.Arciero PJ, Goran MI, Gardner AM, Ades PA, Tyzbir RS, Poehlman ET. A practical equation to predict resting metabolic rate in older females. J Am Geriatr Soc. 1993;41:389–395. doi: 10.1111/j.1532-5415.1993.tb06946.x. [DOI] [PubMed] [Google Scholar]
- 20.Piers LS, Shetty PS. Basal metabolic rates of Indian women. Eur J Clin Nutr. 1993;47:586–591. [PubMed] [Google Scholar]
- 21.Frankenfield D, Roth-Yousey L, Compher C. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: a systematic review. J Am Diet Assoc. 2005;105:775–789. doi: 10.1016/j.jada.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 22.Song T, Venkataraman K, Gluckman P, Seng CY, Meng KC, Khoo EY, Leow MK, Seng LY, Shyong TE. Validation of prediction equations for resting energy expenditure in Singaporean Chinese men. Obes Res Clin Pract. 2014;8:e201–298. doi: 10.1016/j.orcp.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 23.de Oliveira EP, Orsatti FL, Teixeira O, Maesta N, Burini RC. Comparison of predictive equations for resting energy expenditure in overweight and obese adults. J Obes. 2011;2011:534714. doi: 10.1155/2011/534714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muller MJ, Bosy-Westphal A, Klaus S, Kreymann G, Luhrmann PM, Neuhauser-Berthold M, Noack R, Pirke KM, Platte P, Selberg O, Steiniger J. World Health Organization equations have shortcomings for predicting resting energy expenditure in persons from a modern, affluent population: generation of a new reference standard from a retrospective analysis of a German database of resting energy expenditure. Am J Clin Nutr. 2004;80:1379–1390. doi: 10.1093/ajcn/80.5.1379. [DOI] [PubMed] [Google Scholar]
- 25.Yang X, Li M, Mao D, Zeng G, Zhuo Q, Hu W, Piao J, Huang C. Basal energy expenditure in southern Chinese healthy adults: measurement and development of a new equation. Br J Nutr. 2010;104:1817–1823. doi: 10.1017/S0007114510002795. [DOI] [PubMed] [Google Scholar]
- 26.Liu HY, Lu YF, Chen WJ. Predictive equations for basal metabolic rate in Chinese adults: a cross-validation study. J Am Diet Assoc. 1995;95:1403–1408. doi: 10.1016/S0002-8223(95)00369-X. [DOI] [PubMed] [Google Scholar]
- 27.Weijs PJ. Validity of predictive equations for resting energy expenditure in US and Dutch overweight and obese class I and II adults aged 18-65 y. Am J Clin Nutr. 2008;88:959–970. doi: 10.1093/ajcn/88.4.959. [DOI] [PubMed] [Google Scholar]
- 28.Vander Weg MW, Watson JM, Klesges RC, Eck Clemens LH, Slawson DL, McClanahan BS. Development and cross-validation of a prediction equation for estimating resting energy expenditure in healthy African-American and European-American women. Eur J Clin Nutr. 2004;58:474–480. doi: 10.1038/sj.ejcn.1601833. [DOI] [PubMed] [Google Scholar]
- 29.Soares MJ, Francis DG, Shetty PS. Predictive equations for basal metabolic rates of Indian males. Eur J Clin Nutr. 1993;47:389–394. [PubMed] [Google Scholar]
- 30.Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51:241–247. doi: 10.1093/ajcn/51.2.241. [DOI] [PubMed] [Google Scholar]
- 31.Owen OE, Holup JL, D’Alessio DA, Craig ES, Polansky M, Smalley KJ, Kavle EC, Bushman MC, Owen LR, Mozzoli MA, et al. A reappraisal of the caloric requirements of men. Am J Clin Nutr. 1987;46:875–885. doi: 10.1093/ajcn/46.6.875. [DOI] [PubMed] [Google Scholar]
- 32.Owen OE, Kavle E, Owen RS, Polansky M, Caprio S, Mozzoli MA, Kendrick ZV, Bushman MC, Boden G. A reappraisal of caloric requirements in healthy women. Am J Clin Nutr. 1986;44:1–19. doi: 10.1093/ajcn/44.1.1. [DOI] [PubMed] [Google Scholar]
- 33.Collaboration APCS. The burden of overweight and obesity in the Asia-Pacific region. Obes Rev. 2007;8:191–196. doi: 10.1111/j.1467-789X.2006.00292.x. [DOI] [PubMed] [Google Scholar]
- 34.Popkin BM. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr. 2006;84:289–298. doi: 10.1093/ajcn/84.1.289. [DOI] [PubMed] [Google Scholar]
- 35.He YH, Jiang GX, Yang Y, Huang HE, Li R, Li XY, Ning G, Cheng Q. Obesity and its associations with hypertension and type 2 diabetes among Chinese adults age 40 years and over. Nutrition. 2009;25:1143–1149. doi: 10.1016/j.nut.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 36.Weir JB. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9. doi: 10.1113/jphysiol.1949.sp004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Institutes of Health (NIH) conference. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med. 1991;115:956-61. [PubMed]
- 38.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 39.da Rocha EE, Alves VG, Silva MH, Chiesa CA, da Fonseca RB. Can measured resting energy expenditure be estimated by formulae in daily clinical nutrition practice? Curr Opin Clin Nutr Metab Care. 2005;8:319–328. doi: 10.1097/01.mco.0000165012.77567.1e. [DOI] [PubMed] [Google Scholar]
- 40.EFSA Panel on Dietetic Products NaAN. Scientific Opinion on Dietary Reference Values for energy. Parma, Italy: European Food Safety Authority; 2013.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.


