Abstract
Background
In recent years, measurement of cerebral regional oxygen saturation (rSO2) has attracted attention during resuscitation. However, serial changes of cerebral rSO2 in pre-hospital settings are unclear. The objective of this study was to clarify serial changes in cerebral rSO2 of patients with out-of-hospital cardiac arrest (OHCA) in the pre-hospital setting.
Methods
We recently developed a portable rSO2 monitor that is small (170 × 100 × 50 mm in size and 600 g in weight) enough to carry in pre-hospital settings. The sensor is attached to the patient’s forehead by the ELT (Emergency Life-saving Technician), and it monitors rSO2 continuously.
Results
From June 2013 through August 2014, serial changes in cerebral rSO2 in seven patients were evaluated. According to the results of the serial changes in rSO2, four patterns of rSO2 change were found, as follows. Type 1: High rSO2 (around about 60 %) type (n = 1). Initial electrocardiogram was ventricular fibrillation and ROSC (return of spontaneous circulation) could be diagnosed in pre-hospital setting. Her outcome at discharge was Good Recovery (GR). Type 2: Low rSO2 (around about 45–50 %) type (n = 3). They did not get ROSC even once. Type 3: Gradually decreasing rSO2 type (n = 2): ROSC could be diagnosed in hospital, but not in pre-hospital setting. Their outcomes at discharge were not GR. Type 4: other type (n = 1). In this patient with ROSC when ELT started cerebral rSO2 measurement, cerebral rSO2 was 67.3 % at measurement start, it dropped gradually to 54.5 %, and then rose to 74.3 %. The cerebral oxygenation was impaired due to possible cardiac arrest again, and after that, ROSC led to the recovery of cerebral blood flow.
Conclusion
We could measure serial changes in cerebral rSO2 in seven patients with OHCA in the pre-hospital setting. Our data suggest that pre-hospital monitoring of cerebral rSO2 might lead to a new resuscitation strategy.
Electronic supplementary material
The online version of this article (doi:10.1186/s13104-016-2239-4) contains supplementary material, which is available to authorized users.
Keywords: Regional oxygen saturation, Out-of-hospital cardiac arrest, Pre-hospital, Emergency life-saving technician, Portable rSO2 monitor
Background
In recent years, measurement of cerebral regional oxygen saturation (rSO2) by near-infrared spectroscopy (NIRS) has attracted attention in many fields [1–4]. We thought that it might be useful for the development of a new resuscitation strategy. Some research groups have reported that cerebral rSO2 on hospital arrival can predict neurological outcome in patients with out-of-hospital cardiac arrest (OHCA) [5, 6], but we thought this might not be correct because the values of rSO2 always change depending on the patient’s situation at the time cerebral rSO2 is measured [7]. Some research groups have reported that serial changes of cerebral rSO2 in hospital cardiac arrest patients may reflect high-quality cardiopulmonary resuscitation (CPR) [8, 9]. We hypothesised that rather than measuring one rSO2 value at one time point, measurement of serial changes in the values of rSO2 would be important. To prove this hypothesis, pre-hospital measurement of rSO2 in patients was needed. We recently developed a portable rSO2 monitor that is small enough to carry in pre-hospital settings. In this study, we tried to detect the serial changes of rSO2 measured by the Emergency Life-saving Technician (ELT) in earlier phase after out-of-hospital cardiac arrest. The objective of this study was to clarify serial changes in cerebral rSO2 of patients with out-of-hospital cardiac arrest in the pre-hospital setting.
Methods
Study design and data collection
The subjects were all cardiopulmonary arrest (CPA) patients who were transferred to the National Hospital Organization Osaka National Hospital (Osaka, Japan) by ELTs based at Chuo Fire Station. The ELTs performed CPR according to recommendations of the Japan Resuscitation Council Guidelines 2010, which are based on the guidelines of the American Heart Association and the International Liaison Committee on Resuscitation [10]. The rSO2 sensor is attached to the patient’s forehead by the ELT (Fig. 1a). Medical staff did not change patient treatment according to rSO2 data.
Fig. 1.
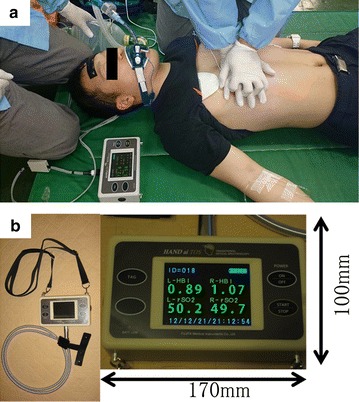
Photograph showing rSO2 measurement in a mock patient by ELTs and the portable near-infrared spectroscopy unit (portable rSO2 monitor). a The detector consists of two sensors that monitor the bilateral frontal lobes. The ELT can carry the portable rSO2 monitor (HAND ai TOS®; TOSTEC CO., Tokyo, Japan) and perform cardiopulmonary resuscitation without difficulty in the pre-hospital setting. b The portable rSO2 monitor is 170 × 100 × 50 mm in size and 600 g in weight. It can be carried easily by hanging it around the neck, and it can be used even in severe pre-hospital environments such as heavy rain and strong sunlight. rSO 2 regional saturation of oxygen; ELT emergency life-saving technician
The pre-hospital portable monitoring of cerebral rSO2 in CPA patients with OHCA was approved by the Ethics Committee of Osaka University Graduate School of Medicine (No. 12446), and the institutional review board waived the need for informed consent because the subjects were all in CPA.
Portable NIRS rSO2 monitoring system
We developed a portable rSO2 monitor (HAND ai TOS®; TOSTEC CO., Tokyo, Japan) (Fig. 1b). The HAND ai TOS was not approved by Medicines and Healthcare Products Regulatory Agency (MHRA) and Food and Drug Administration (FDA). The HAND ai TOS system measures oxygen saturation based on the Beer-Lambert law by using three different wavelengths of near-infrared LED light, which have specific absorbance to oxyhaemoglobin and deoxyhaemoglobin. The lights pass through the skin to a depth of approximately 3 cm, and the reflected lights are sensed by a photodiode. The reflected lights represent the haemoglobin information mainly in the cerebral cortex. The system can measure rSO2 data every second without the necessity of arterial pulsation, so it is possible to carry out continuous monitoring in CPA patients. Two rSO2 values, left side and right side, are acquired continuously, and then the average of the two values is calculated. The normal range of cerebral rSO2 was previously determined from 15 healthy adult volunteers to be 71.2 ± 3.9 % (on room air) (n = 15, 10 men and 5 women, 43.2 ± 8.9 years) [7].
Statistical analysis
All data are represented as mean ± standard deviation (SD). All statistical analyses were performed with JMP Pro 10 for Windows (SAS Institute Inc., Cary, NC, USA).
Results
Patient characteristics
From June 2013 through August 2014, serial changes in cerebral rSO2 in seven patients were evaluated. Characteristics, outcome, and rSO2 data of the OHCA patients are shown in Table 1. According to the results of the serial changes in rSO2, four patterns of rSO2 change were found, as follows.
Table 1.
Characteristics, outcome, and rSO2 data of out-of-hospital cardiac arrest patients
| No. | Age (years) | Witness | Bystander CPR | Initial ECG | ROSC | rSO2 at the start of measurement (%) | Outcome (GOS at discharge) |
|---|---|---|---|---|---|---|---|
| 1 | 51 | Yes | Yes | VF | Yes (pre-hospital) | 60.1 | GR |
| 2 | 74 | No | No | VF | Yes (after application of ECMO) | 55.3 | D |
| 3 | 86 | Yes | No | Unknown | Yes (before ELT contact) | 66.1 | VS |
| 4 | 65 | Yes | No | Asystole | Yes (in-hospital) | 53.9 | D |
| 5 | 45 | Yes | No | Asystole | No | 45.3 | D |
| 6 | 27 | No | Yes | Asystole | No | 49.7 | D |
| 7 | 86 | No | No | Asystole | No | 52.9 | D |
rSO 2 regional oxygen saturation, CPR cardiopulmonary resuscitation, ECG electrocardiogram, ROSC return of spontaneous circulation, GOS Glasgow outcome scale, VF ventricular fibrillation, ECMO extracorporeal membrane oxygenation, ELT emergency life-saving technician, GR good recovery, VS vegetative state, D death
Type 1: high rSO2 type (Table 1; patient #1)
Type 1 [high rSO2 type (n = 1)] is shown in Fig. 2a. The patient’s initial electrocardiogram (ECG) was ventricular fibrillation (VF). The rSO2 values remained at around 60 %. Return of spontaneous circulation (ROSC) was diagnosed 4 min after ELT contact in the pre-hospital setting. On hospital arrival, the patient’s consciousness was impaired (Glasgow Coma Scale [GCS], 1–2–5). Hypothermia therapy (34 °C) was performed for brain protection. Her outcome according to the Glasgow Outcome Scale (GOS) at discharge was good recovery. The etiology of CPA was considered cardiac arrhythmia.
Fig. 2.
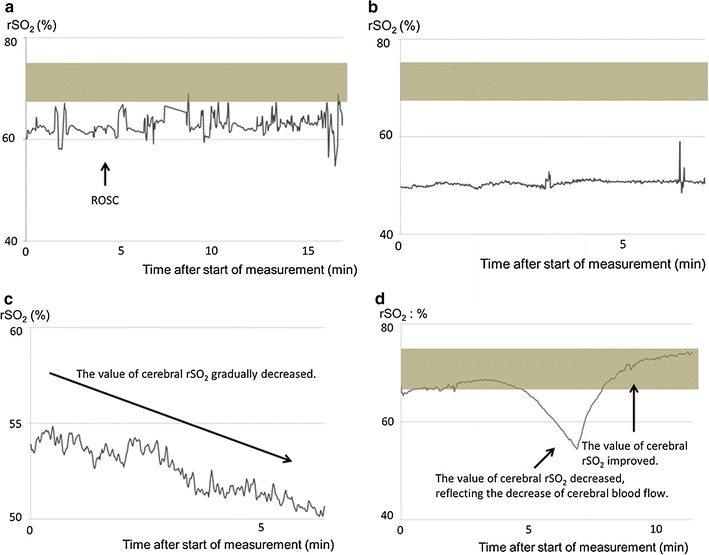
Serial changes in cerebral rSO2 (representative cases). a Type 1: High rSO2 type (around 60 %). One patient (51-year-old woman; patient #1) showed this type. Her initial electrocardiogram was ventricular fibrillation, and ROSC was diagnosed in the pre-hospital setting. Her outcome at discharge was good recovery. b Type 2: Low rSO2 type (around 45-50 %). Three patients (52.7 ± 30.2 years, 1 man and 2 women) showed this type. This graph shows the serial changes in cerebral rSO2 of patient #6. A similar pattern was observed in patients #5 and #7. None attained ROSC even once. c Type 3: gradually decreasing rSO2 type. Two patients (69.5 ± 6.4 years, 2 men) showed this type. Serial changes in cerebral rSO2 from patient #4 are shown. The rSO2 value gradually decreased. ROSC was diagnosed in-hospital 35 min after the start of measurement. His outcome was death. A similar pattern was also observed in patient #2. Both patients attained ROSC, which was diagnosed in hospital but not in the pre-hospital setting. Their outcomes at discharge were death. d Type 4: other type. One patient (86-year-old woman; patient #3) showed this type. In this patient with ROSC, when the ELT started cerebral rSO2 measurement, the cerebral rSO2 was 67.3 %. It dropped gradually to 54.5 % and then rose to 74.3 %. Cerebral oxygenation was impaired due to possible return of cardiac arrest, but after that, ROSC led to the recovery of cerebral blood flow. The shaded area represents the normal cerebral rSO2 range measured from healthy adults. rSO 2 regional saturation of oxygen, ROSC return of spontaneous circulation, ELT emergency life-saving technician
Type 2: low rSO2 type (Table 1; patients #5, 6, 7)
Type 2 (low rSO2 type [n = 3]) is shown in Fig. 2b (Table 1; patient #6). Her initial ECG was asystole. The rSO2 values remained at around 50 %. Her GOS outcome at discharge was death. A similar rSO2 pattern was observed in patients #5 and #7 (Table 1; Additional file 1: Figure S1B, C), whose ECGs also showed asystole. The mean value of cerebral rSO2 at the start of measurement was 49.3 ± 3.8 %. None of these patients attained ROSC even once.
Type 3: gradually decreasing rSO2 type (Table 1; patients #2, 4)
Type 3 [gradually decreasing rSO2 type (n = 2)] is shown in Fig. 2c (Table 1; patient #4). This man’s initial ECG was asystole. His rSO2 values gradually decreased. ROSC was diagnosed in-hospital at 35 min after the start of measurement. His GOS outcome at discharge was death. A similar rSO2 pattern was observed in patient #2 (Table 1, Additional file 1: Figure S1A). ROSC was diagnosed in-hospital in patient #2 but not in the pre-hospital setting. The GOS outcome of patient #2 was also death.
Type 4: other type (Table 1; #3)
Type 4 (other type [n = 1]) is shown in Fig. 2d. In this patient with ROSC when the ELTs started cerebral rSO2 measurement, cerebral rSO2 at measurement start was 67.3 % (almost normal range), it dropped gradually to 54.5 %, and it then rose to 74.3 %. Her cerebral oxygenation was impaired due to possible return of cardiac arrest, and after that, ROSC led to the recovery of cerebral blood flow. Her GOS outcome at discharge was vegetative state.
Discussion
In this report, we showed the pre-hospital serial changes of cerebral rSO2 in patients with OHCA. The values of cerebral rSO2 in the patients with OHCA dramatically changed in the very early phase after cardiac arrest.
Our data showed several advantages of the pre-hospital measurement of cerebral rSO2. First, we might be able to predict the neurological outcome of patients with VF. The initial ECGs of patients #1 and #2 both showed VF, but the initial rSO2 value of patient #1 was higher than that of patient #2 (Table 1; Fig. 2a, c). In terms of neurological outcome, patient #1 experienced good recovery, whereas that of patient #2 was death (Table 1). Our report suggested that a patient who maintained a high cerebral rSO2 value might have a good neurological prognosis, and the type of serial change in the pre-hospital cerebral rSO2 data might lead to the prediction of neurological outcome in patients with VF.
Second, the pre-hospital cerebral rSO2 data might allow the estimation of the time after cardiac arrest in unwitnessed cases. Presence of a witness is one of the factors of good neurological prognosis [11, 12], but if witness information is absent, we might treat CPA patients as those for whom considerable time had passed after CPA. We could detect gradually decreasing cerebral rSO2 in two patients (Fig. 2c). We thought that the gradually decreasing rSO2 type probably indicated that little time had passed since CPA. To better understand the relation between time and cerebral rSO2, it will be necessary to accumulate data from more witnessed CPA patients.
Third, a portable rSO2 monitoring system would be very useful, similar to ECG monitoring, for ELTs in the pre-hospital setting. As shown in Fig. 2d, dynamic changes of cerebral rSO2 can be revealed. When the value of cerebral rSO2 decreased in Fig. 2d, the ECG showed QRS waves. We determined that pulseless electrical activity could be diagnosed at that time. The ELTs cannot always check the patient’s pulse in the pre-hospital setting, especially when they are transporting the patient on stairs or into the ambulance, because they must transfer the patient to hospital quickly. By using our portable rSO2 monitor, ELTs can always check cerebral blood flow without actually having to check the pulse.
Finally, the presence of a continuous low rSO2 type might predict poor neurological outcome and high mortality.
Our report has some limitations. First, rSO2 monitoring was not performed in a blind fashion. Therefore, rSO2 value may influence CPR procedures. Second, the validation of HAND ai TOS about low rSO2 value (<60 %) had been demonstrated in vitro but not in vivo. Third, sample size is small. To generalize this results, we need further study in a larger population.
Conclusion
We could measure serial changes in cerebral rSO2 in seven patients with OHCA in the pre-hospital setting. Further evaluation of the validity of pre-hospital monitoring of cerebral rSO2 may lead to a new resuscitation strategy in the pre-hospital setting.
Authors' contributions
TH, TS and MO conceived the study, and participated in its design. JN, YH, KS, and KK conducted the case. JN, YH, KS, KK, NE, AW and MO collected and generated the data. TH wrote the first draft. TH, TS and MO analyzed the data. TS, KS, SH, DS, and TS helped to draft the manuscript. All the authors read and approved the final manuscript.
Acknowledgements
We gratefully acknowledge the devoted cooperation of the Osaka Municipal Fire Department.
Competing interests
The authors declare that they have no competing interests.
Availability of data and material
All data generated or analysed during this study are included in this published article and its supplementary information files.
Consent for publication
We could not obtain consent from all patients because the subjects were all in CPA.
Ethics approval and consent to participate
The pre-hospital portable monitoring of cerebral rSO2 in CPA patients with OHCA was approved by the Ethics Committee of Osaka University Graduate School of Medicine (No. 12446), and the institutional review board waived the need for informed consent because the subjects were all in CPA and this rSO2 monitor was non-invasive for patients.
Funding
This work was supported by Grants-in-aid for scientific research from the Ministry of Education, Culture, Sports, Science, and Technology in Japan (no.JP15H05007).
Abbreviations
- rSO2
regional oxygen saturation
- ELT
emergency life-saving technician
- ROSC
return of spontaneous circulation
- OHCA
out-of-hospital cardiac arrest
- NIRS
near-infrared spectroscopy
- CPR
cardiopulmonary resuscitation
- GOS
Glasgow outcome scale
- GR
good recovery
- VS
vegetative state
- D
death
- ECG
electrocardiogram
- VF
ventricular fibrillation
- GCS
Glasgow coma scale
- ECMO
extracorporeal membrane oxygenation
- PEA
pulseless electrical activity
Additional file
10.1186/s13104-016-2239-4 Serial changes in cerebral rSO2 (non-representative cases). Serial changes in cerebral rSO2 (non-representative cases). (A) 74-year-old man; patient #2. His initial electrocardiogram was ventricular fibrillation, and the values of cerebral rSO2 gradually decreased after start of measurement. ROSC was diagnosed in the hospital setting after application of ECMO. Her outcome at discharge was Dead. (B) 45-year-old woman; patient #5. This patient showed the low rSO2 type. None attained ROSC even once. (C) 86-year-old man; patient #7. This patient showed the low rSO2 type. None attained ROSC even once. rSO2, regional saturation of oxygen; ROSC, return of spontaneous circulation; ECMO: extracorporeal membrane oxygenation.
Contributor Information
Tomoya Hirose, Phone: +81-6-6879-5707, Email: htomoya1979@hp-emerg.med.osaka-u.ac.jp.
Tadahiko Shiozaki, Email: shiozaki@hp-emerg.med.osaka-u.ac.jp.
Junji Nomura, Email: j-nomura@city.osaka.lg.jp.
Yasuto Hamada, Email: ya-hamada@city.osaka.lg.jp.
Keiichi Sato, Email: k-satou@fasd.or.jp.
Kazuya Katsura, Email: k-katsura@city.osaka.lg.jp.
Naoki Ehara, Email: ehaehaeha@hotmail.com.
Akinori Wakai, Email: gogowakasama@gmail.com.
Kentaro Shimizu, Email: shimizu507@gmail.com.
Mitsuo Ohnishi, Email: mohnishi@hp-emerg.med.osaka-u.ac.jp.
Sumito Hayashida, Email: s-hayashida@city.osaka.lg.jp.
Daikai Sadamitsu, Email: dsada@onh.go.jp.
Takeshi Shimazu, Email: shimazu@hp-emerg.med.osaka-u.ac.jp.
References
- 1.Murkin JM, Adams SJ, Novick RJ, Quantz M, Bainbridge D, Iglesias I, et al. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg. 2007;104:51–58. doi: 10.1213/01.ane.0000246814.29362.f4. [DOI] [PubMed] [Google Scholar]
- 2.Goldman S, Sutter F, Ferdinand F, Trace C. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg. Forum. 2004;7:E376–E381. doi: 10.1532/HSF98.20041062. [DOI] [PubMed] [Google Scholar]
- 3.Slater JP, Guarino T, Stack J, Vinod K, Bustami RT, Brown JM, et al. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg. 2009;87:36–44. doi: 10.1016/j.athoracsur.2008.08.070. [DOI] [PubMed] [Google Scholar]
- 4.Gottlieb EA, Fraser CD, Jr, Andropoulos DB, Diaz LK. Bilateral monitoring of cerebral oxygen saturation results in recognition of aortic cannula malposition during pediatric congenital heart surgery. Paediatr Anaesth. 2006;16:787–789. doi: 10.1111/j.1460-9592.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 5.Ito N, Nishiyama K, Callaway CW, Orita T, Hayashida K, Arimoto H, et al. Noninvasive regional cerebral oxygen saturation for neurological prognostication of patients with out-of-hospital cardiac arrest: a prospective multicenter observational study. Resuscitation. 2014;85:778–784. doi: 10.1016/j.resuscitation.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 6.Hayashida K, Nishiyama K, Suzuki M, Abe T, Orita T, Ito N, et al. Estimated cerebral oxyhemoglobin as a useful indicator of neuroprotection in patients with post-cardiac arrest syndrome: a prospective, multicenter observational study. Crit Care. 2014;18:500. doi: 10.1186/s13054-014-0500-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakahori Y, Hirose T, Shiozaki T, Ogawa Y, Ohnishi M, Fujimi S, et al. Serial changes in values of cerebral regional saturation of oxygen (rSO2) during resuscitation in patients with out-of-hospital cardiac arrest. Nihon Kyukyu Igakukai Zasshi. 2013;24:774–780. doi: 10.3893/jjaam.24.774. [DOI] [Google Scholar]
- 8.Parnia S, Nasir A, Ahn A, Malik H, Yang J, Zhu J, et al. A feasibility study of cerebral oximetry during in-hospital mechanical and manual cardiopulmonary resuscitation. Crit Care Med. 2014;42:930–933. doi: 10.1097/CCM.0000000000000047. [DOI] [PubMed] [Google Scholar]
- 9.Ibrahim AW, Trammell AR, Austin H, Barbour K, Onuorah E, House D, et al. Cerebral oximetry as a real-time monitoring tool to assess quality of in-hospital cardiopulmonary resuscitation and post cardiac arrest care. J Am Heart Assoc. 2015;4:e001859. doi: 10.1161/JAHA.115.001859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hazinski MF, Nolan JP, Billi JE, Bottiger BW, Bossaert L, de Caen AR, et al. Part 1: executive summary: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2010;122(16 Suppl 2):S250–S275. doi: 10.1161/CIRCULATIONAHA.110.970897. [DOI] [PubMed] [Google Scholar]
- 11.Goto Y, Maeda T, Nakatsu-Goto Y. Neurological outcomes in patients transported to hospital without a prehospital return of spontaneous circulation after cardiac arrest. Crit Care. 2013;17:R274. doi: 10.1186/cc13121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]


