Abstract
Fibrosing mediastinitis is a rare condition defined by the presence of fibrotic mediastinal infiltrates that obliterate normal fat planes. It is a late complication of a previous granulomatous infection, such as histoplasmosis or tuberculosis (TB). Due to its rarity, fibrosing mediastinitis is often under-recognized, and the clinical presentation is variable and dependent on the extent of infiltration or encasement of structures within the mediastinum. We present a case of fibrosing mediastinitis in a man with a prior history of TB, who presented with progressive dyspnea and was found to have chronic mediastinal soft tissue opacities and pulmonary hypertension. His diagnosis was delayed due to the lack of recognition of this clinical/radiographic entity. Fibrosing mediastinitis is a rare entity usually caused by granulomatous disease. Most cases develop as a late complication of histoplasmosis or TB. The presence of calcified mediastinal soft tissue infiltrates on advanced chest imaging can be diagnostic of fibrosing mediastinitis in patients with a prior history of a granulomatous infection once active processes such as malignancy are excluded.
Keywords: Fibrosing mediastinitis, histoplasmosis, mediastinal fibrosis, sclerosing mediastinitis, tuberculosis

INTRODUCTION
Fibrosing mediastinitis, also known as sclerosing mediastinitis or mediastinal fibrosis, is a rare late sequela of a thoracic inflammatory process. Most cases arise from prior histoplasmosis infection, and less commonly from tuberculosis (TB).[1,2] Fibrosing mediastinitis is characterized by the development of dense mediastinal infiltrates that obliterate normal fat planes and is best viewed through advanced imaging modalities, such as computed tomography (CT) or magnetic resonance imaging (MRI).[1] Given the rarity of this clinical entity, some cases may go unrecognized and is often misdiagnosed. We present the case of a patient with TB-associated fibrosing mediastinitis whose diagnosis was delayed.
CASE REPORT
A 71-year-old man with a history of chronic obstructive pulmonary disease (COPD), pulmonary hypertension, and TB status posttreatment in 1985, presented for evaluation of chronic, progressive dyspnea. The patient had previously been seen at our institution for dyspnea and had been diagnosed with and treated for numerous COPD exacerbations. He had been treated with bronchodilators, corticosteroids, and occasional antibiotics without improvement. He had no history of tobacco use, significant alcohol consumption, or any illicit drug use.
On examination, the patient was in no significant distress and was able to speak in full sentences. His vital signs were normal except for a respiratory rate of 20 breaths/min and oxygen saturation of 90% on room air at rest. Cardiovascular examination was notable for jugular venous distension to the angle of the mandible. A parasternal heave, an accentuated P2, and an S3 were appreciated. Lung auscultation was notable for decreased breath sounds. The remainder of the examination was unremarkable.
Transthoracic echocardiography revealed right ventricular dilatation with flattening of the interventricular septum and an estimated pulmonary artery systolic pressure of 85 mmHg. Pulmonary function testing (PFT) demonstrated severe obstructive ventilatory defect with diffusion impairment.
Chest radiograph demonstrated bilateral perihilar soft tissue densities with right apical scarring, pleural thickening and volume loss [Figure 1]. Contrast-enhanced chest CT revealed ill-defined, infiltrative bilateral hilar soft tissue densities with calcifications, enlargement of the main and right pulmonary artery, and irregular narrowing of the right mainstem and upper lobe bronchi [Figure 2]. Positron emission tomography (PET) showed mild fluorodeoxyglucose uptake in the bilateral perihilar regions, right more prominent than left. Of note, the patient had undergone a non contrast-enhanced thoracic CT three years prior, which documented relative stability all the abnormal findings, including the bronchial narrowing and pulmonary artery dilation [Figure 3].
Figure 1.
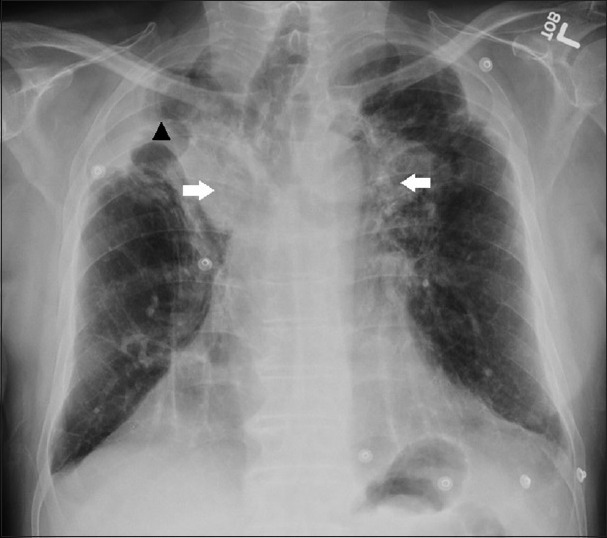
A 71-year-old man with a history of chronic obstructive pulmonary disease, pulmonary hypertension, and prior pulmonary tuberculosis infection presenting with progressive dyspnea, diagnosed with tuberculosis-associated fibrosing mediastinitis. Chest posteroanterior radiograph showing bilateral peri-hilar soft tissue densities (white arrows) with right apical, pleural thickening and volume loss (black arrow head).
Figure 2.
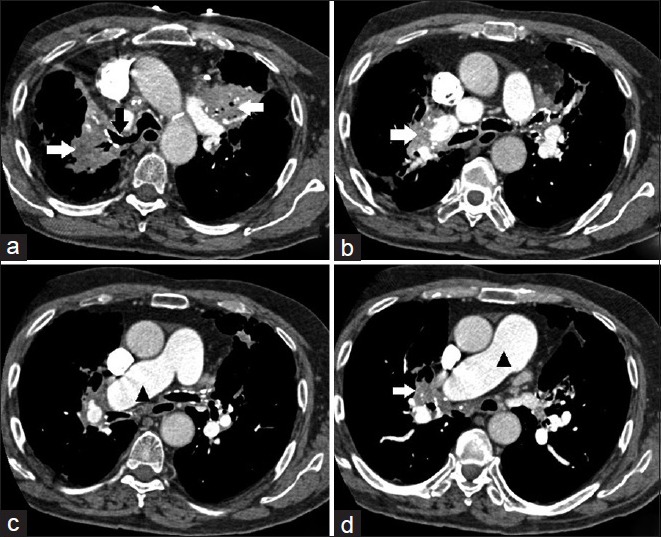
A 71-year-old man with a history of chronic obstructive pulmonary disease, pulmonary hypertension, and prior pulmonary tuberculosis infection presenting with progressive dyspnea, diagnosed with tuberculosis-associated fibrosing mediastinitis. Contrast-enhanced chest computed tomography, soft tissue window. (a-d) Demonstrates ill-defined, infiltrative bilateral hilar soft tissue densities with calcifications (white arrows); enlargement of the main and right pulmonary artery (black arrow heads); and irregular narrowing of the right mainstem and upper lobe bronchi (black arrow).
Figure 3.
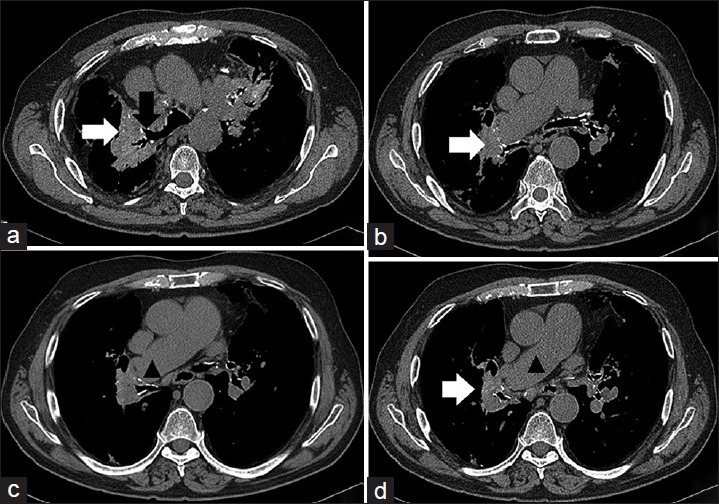
A 71-year-old man with a history of chronic obstructive pulmonary disease, pulmonary hypertension, and prior pulmonary tuberculosis infection presenting with progressive dyspnea, diagnosed with tuberculosis-associated fibrosing mediastinitis. Noncontrast enhanced computed tomography chest, soft tissue window, from 3-years prior. (a-d) Demonstrating ill-defined, infiltrative bilateral hilar soft tissue densities with calcifications (white arrows); enlargement of the main and right pulmonary artery (black arrow heads); and irregular narrowing of the right mainstem and upper lobe bronchi (black arrow).
The patient had previously undergone a bronchoscopy with bronchoalveolar lavage, brushings, and biopsies which were negative for fungal organisms and acid-fast bacilli.
The patient's known history of TB and findings of old granulomatous disease on imaging along and with negative bronchoscopy results established fibrosing mediastinitis as the likely cause of his mediastinal infiltrates. Although the PET scan showed mild uptake in the perihilar regions consistent with an active inflammatory process, the stability noted on imaging over a prolonged course was reassuring that the mediastinal and hilar infiltrates did not represent malignancy. The patient had compression of his pulmonary artery due to fibrosing mediastinitis and findings of pulmonary hypertension on the examination and by echocardiography. He also had tracheobronchial narrowing as a result of this entity as seen on chest imaging which likely manifested as obstruction on spirometry. The patient's respiratory symptoms stabilized on supportive medications, and no further interventions were required.
DISCUSSION
The pathophysiology of fibrosing mediastinitis is postulated to stem from the chronic inflammation and associated profound fibrotic changes of mediastinal structures from the adjacent primary granulomatous disease, either via direct infiltration from granuloma rupture or indirectly via local inflammatory processes within regional mediastinal lymph nodes.[3] The etiology of this inflammation includes granulomatous diseases (such as histoplasmosis, TB, sarcoidosis, and Behcet's disease), malignancy (such as bronchogenic cancer and lymphoma), trauma, and medication-induced (methysergide); however, a large number of cases remain idiopathic. A subset of idiopathic fibrosing mediastinitis now encompasses an emerging disease entity mediated by IgG-4, a presumed anti-inflammatory immunoglobulin whose exact role in inflammation modulation is yet to be elucidated but can manifest as retroperitoneal fibrosis with or without thyroiditis.
The development of fibrotic infiltrates/masses has the potential to encase and compromise mediastinal structures including the airway, esophagus, and/or major vessels. Airway involvement can vary widely ranging from hoarseness, if the laryngeal nerve is affected, to obstructive pneumonitis and/or atelectasis, and hemoptysis when erosion of the vascular bundle due to local inflammation into the pulmonary parenchyma occurs. Gastrointestinal involvement can include dysphagia and odynophagia through a direct mass effect. Vascular involvement can compromise any of the following: superior vena cava (SVC), aorta, pulmonary arteries, and veins through compression secondary to mass effect. Direct invasion can result in fistula formation. Clinically significant SVC syndrome and pulmonary hypertension can occur.[4] Of note, the insidious onset of vascular compromise often allows for the development of significant collaterals and the potential to remain asymptomatic.
The diagnosis of fibrosing mediastinitis is established via clinical impression and imaging, and must exclude other active infiltrative processes involving the mediastinum, particularly bronchogenic carcinoma and lymphoproliferative disorders.[5,6] Chest radiographs are usually nonspecific and often underestimate the extent of mediastinal disease. Therefore, advanced imaging modalities such as CT and MRI are preferred. Characteristic findings on CT or MRI include soft tissue obliteration of normal mediastinal fat planes with or without encasement and invasion of adjacent structures.
The management of fibrosing mediastinitis is largely directed toward symptom palliation, if present. There are currently, no medical therapies that have shown to prevent this sequela of granulomatous disease or alter it's natural progression. Although controlled trials have not been performed, glucocorticoids do not appear to be beneficial. Corticosteroids, however, may be effective in IgG-4 related fibrosing mediastinitis.[7] Treatment of any underlying infectious process is still warranted for patients’ well-being and public health purposes. Other management modalities can include percutaneous stenting of vascular structures such as the SVC to relieve obstruction, or placement of endoscopic stents in cases of airway obstruction and for the management of dysphagia.[8] Surgery has a limited benefit and generally leads to poor outcomes given the extent of the fibrosis, calcifications, and the presence of collaterals.[9]
Terminal outcomes with fibrosing mediastinitis include the development of cor pulmonale and respiratory compromise from recurrent infections, bronchial obstruction, or hemoptysis.[10]
CONCLUSIONS
Although rare, fibrosing mediastinitis should be considered in the differential diagnosis of an ill-defined, calcified soft tissue mass in the mediastinum. The clinical presentation and symptomatic involvement is directly proportional to the extent of infiltration of mediastinal structures. Fibrosing mediastinitis is a diagnosis of exclusion and is best established via advanced imaging modalities. It is most often a late sequela of granulomatous inflammation, however, active processes such as infection or malignancy must first be excluded. The management is primarily directed toward palliation of symptoms, if present, particularly as no medical therapy or surgical intervention has shown any benefit.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/32/188958
REFERENCES
- 1.Rossi SE, McAdams HP, Rosado-de-Christenson ML, Franks TJ, Galvin JR. Fibrosing mediastinitis. Radiographics. 2001;21:737–57. doi: 10.1148/radiographics.21.3.g01ma17737. [DOI] [PubMed] [Google Scholar]
- 2.Fijolek J, Wiatr E, Blasinska-Przerwa K, Roszkowski-Sliz K. Fibrosing mediastinitis as an untypical complication of tuberculosis: Case report. Pol Arch Med Wewn. 2009;119:752–5. [PubMed] [Google Scholar]
- 3.Goodwin RA, Nickell JA, Des Prez RM. Mediastinal fibrosis complicating healed primary histoplasmosis and tuberculosis. Medicine (Baltimore) 1972;51:227–46. doi: 10.1097/00005792-197205000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Zider, A, Kamangar N. An 80-year-old female with progressive shortness of breath and a mediastinal mass. Chest. 2016;150:19–22. doi: 10.1016/j.chest.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 5.McNeeley MF, Chung JH, Bhalla S, Godwin JD. Imaging of granulomatous fibrosing mediastinitis. AJR Am J Roentgenol. 2012;199:319–27. doi: 10.2214/AJR.11.7319. [DOI] [PubMed] [Google Scholar]
- 6.Koksal D, Bayiz H, Mutluay N, Koyuncu A, Demirag F, Dagli G, et al. Fibrosing mediastinitis mimicking bronchogenic carcinoma. J Thorac Dis. 2013;5:E5–7. doi: 10.3978/j.issn.2072-1439.2012.07.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peikert T, Colby TV, Midthun DE, Pairolero PC, Edell ES, Schroeder DR, et al. Fibrosing mediastinitis: Clinical presentation, therapeutic outcomes, and adaptive immune response. Medicine (Baltimore) 2011;90:412–23. doi: 10.1097/MD.0b013e318237c8e6. [DOI] [PubMed] [Google Scholar]
- 8.Kant S, Walsh GL. Fibrosingmediastinitis and consequent superior vena cava syndrome – A case report. J Thorac Dis. 2012;4:428–30. doi: 10.3978/j.issn.2072-1439.2012.01.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mathisen DJ, Grillo HC. Clinical manifestation of mediastinal fibrosis and histoplasmosis. Ann Thorac Surg. 1992;54:1053–7. doi: 10.1016/0003-4975(92)90069-g. [DOI] [PubMed] [Google Scholar]
- 10.Sherrick AD, Brown LR, Harms GF, Myers JL. The radiographic findings of fibrosing mediastinitis. Chest. 1994;106:484–9. doi: 10.1378/chest.106.2.484. [DOI] [PubMed] [Google Scholar]


