Abstract
Objective:
To determine the delay in diagnosis of various types of congenital heart defects in children and factors associated with such delay.
Patients and Methods:
For this observational study, 354 patients having congenital heart disease (CHD) presenting for the first time to the Department of Cardiology, Children’s Hospital, Lahore, Pakistan, between January 1, 2015 and June 30, 2015, were enrolled after obtaining informed verbal consent from the guardian of each child. Demographical profile and various factors under observation were recorded.
Results:
Among the 354 enrolled children (M: F 1.7:1) with age ranging from 1 to 176 months (median 24 months), 301 (85.1%) had delayed diagnosis of CHD (mainly acyanotic 65.3%), with median delay (8 months). Main factors for delay were delayed first consultation to a doctor (37.2%) and delayed diagnosis by a health professional (22.5%). Other factors included delayed referral to a tertiary care hospital (13.3%), social taboos (13.0%), and financial constraints (12.3%). Most children were delivered outside hospital settings (88.7%). Children with siblings less than two (40%) were less delayed than those having two or more siblings (60%, P < 0.001).
Conclusion:
Diagnosis of congenital heart defect was delayed in majority of patients. Multiple factors such as lack of adequately trained health system and socioeconomic constraints were responsible for the delay. There is a need to develop an efficient referral system and improve public awareness in developing countries for early diagnosis and management of such children.
Keywords: Congenital heart defect, delayed diagnosis, Pakistan
INTRODUCTION
The incidence of moderate-to-severe form of congenital heart disease (CHD) is estimated to be about 6/1000 live births.[1] Incidence of CHD is much higher (19/1000 to 75/1000) if potentially significant bicuspid aortic valve and tiny muscular ventricular septal defects are also included. As a result, CHD constitutes a major cause of infant mortality across the globe.[2] With remarkable improvements in diagnostic and management options in recent years, a significant proportion of children born with CHD are expected to lead a normal, productive life.[3] Among various other factors, early identification of CHD and timely intervention is extremely important for final prognosis in these children.[4,5] Antenatal detection of CHD is now considered standard of care in developed countries, improving the final outcome. In most low and middle-income countries, however, such facilities are few and far, and majority of patients from developing countries present late. Such delay results in suboptimal management and poor outcome as complications may have already set in. Comorbidities especially undernutrition seriously compromise the results of any intervention in these children.[6]
In this study, we aimed to examine the pattern of CHD in children presenting to a tertiary care hospital, trends in timing of diagnosis of various CHD, and various factors associated with delayed presentation hence delayed diagnosis. The identification of such factors would help in planning focused screening program and awareness strategies for an early detection of CHD.
MATERIALS AND METHODS
This cross-sectional observational study was conducted at the Department of Cardiology, The Children Hospital and Institute of Child Health, Lahore, Pakistan, over a period of 6 months (January 2015 to June 2015). This is the sole public sector, tertiary care pediatric cardiac center for the entire province of Punjab with a population of over 100 million.[7,8] Two adult cardiology centers in the province provide some pediatric service but do not operate children less than 10 kg in weight. Institutional Review Board of the hospital approved the study protocol. All patients presenting to the hospital for the first time and diagnosed as CHD were evaluated for inclusion in the study. After obtaining informed consent from patient’s parents, evaluation was performed with confirmation of diagnosis through echocardiography. Any patient with acquired heart disease including acute viral myocarditis/postviral cardiomyopathy and rheumatic heart disease were excluded from study.
Demographical profile and socioeconomic status, poverty, illiteracy, improper referral, inadequate health facilities, and social issues were recorded on specially designed questionnaire through interview-based information by the author (UR) from direct caregiver including mother, father, or the guardian. Any child with cyanotic heart disease diagnosed after discharge from birth clinic was labeled as having a delayed diagnosis. Patients with acyanotic CHD were considered having delayed diagnosis, in case the defect was diagnosed at an age when elective cardiac repair should have already been performed, according to contemporary standards of pediatric cardiology.[9] Socioeconomic status was evaluated using scale developed by Mughal et al.[10] Poverty was defined in absolute terms of low income as less than US$2 a day.[11] Illiterate person was described as someone who cannot, with understanding, read and write a short, simple statement of their own in everyday life.[12] Improper referral was defined as a process in which a health worker at one level of the health system, having insufficient resources (drugs, equipment, skills) to manage a clinical condition, does not seek the assistance of a better or differently resourced facility.[13] Inadequate health facilities were described as lack of required diagnostic tools, drugs, equipments, and skills at a given health facility to optimally manage a child with heart condition. Social issues included discrepancy between the elements of culture or society, which endanger the lives of social groups.[14]
Statistical analysis
Data was entered in SPSS version 18 (Stata) and analyzed using its statistical package. The sample size calculation was done with 80% power of test and 5% level of significance, taking incidence of CHD as 6/1000 live birth using nonprobability purposive sampling. Frequency was calculated for qualitative variable including sex, type of CHD, various factors associated with delayed diagnosis, and parental education. Mean and standard deviation were calculated for quantitative variables such as age, weight, and number of siblings. Median with range was calculated for variables with nonnormal distribution. χ2 test was applied as test of significance for any significant difference between various factors resulting in delayed diagnosis of various type of CHD. Univariate and multivariate analyses were performed to determine significance of various factors causing delay in diagnosis, and their odds ratios were calculated. P < 0.05 was considered as significant.
RESULTS
A total of 354 new patients with confirmed CHD were included in the study. There were 224 boys (63.3%) with boy to girl ratio of 1.7:1. Median age was 24 month (range 3 days to 14.8 years). The patients had a median weight of 13 kg (2.8-32 kg) with majority of the patients weighing below the 3rd centile for age (201/354, 56.8%). Nearly 60% children came from rural areas. About 66% (n = 234) belonged to poor socioeconomic class with additional 30% (n = 107) from middle-income group. Illiteracy rate in parents was higher in fathers than mothers (73% vs. 54% respectively, P < 0.001). Median number of siblings was three per family ranging from one to seven. Only eight mothers (2%) had a fetal echocardiography performed. Most babies were delivered at home or local maternity centers (n = 273, 77%). Median distance the patient had to travel to reach the cardiac center was 100 km (range 3-650 km) with 32% (n = 112) traveling more than 100 km. Two hundred and thirty one children (65.3%) had acyanotic CHD.
Out of 354 children, 301 (85.1%) had a delayed diagnosis of CHD. The median delay in diagnosis was 8 months (range 1-168 months) [Table 1]. There was no significant difference in delay in diagnosis between male and female children, P = 0.1. The delay in diagnosis varied according to underlying diseases. There was a median delay of 18.5 months (range 3-120 months) in large unrestricted ventricular septal defect (VSD), 98 months (range 72-168 months) in atrial septal defect (ASD) with right ventricular volume overload, 24 months (range 4-144 months) in Tetralogy of Fallot, and 4 months (range 2-6 months) in transposition of great arteries with intact septum [Table 2, Figure 1]. Diagnosis of CHD in most patients was delayed because of delayed first consultation with a doctor (n = 112, 37.2%), delayed diagnosis by a health professional (n = 68, 22.5%), delayed referral to a tertiary care hospital (n = 40, 13.3%), social taboos leading to delayed diagnosis (n = 39, 13.0%), financial constraints (n = 37, 12.3%), and religious beliefs (n = 5, 1.7%). Children having acyanotic CHD (n = 205) had a significantly longer delay in diagnosis than cyanotic CHD (n = 96), odds ratio = 2.0, P = 0.01. Children living in rural area were significantly more delayed in diagnosis (n = 183/207) than those living in urban area (n = 118/147) (odds ratio = 1.9; P = 0.04). Children belonging to lower socioeconomic status (n = 217) had more delayed diagnosis of CHD than middle and upper socioeconomic status (n = 84) (P < 0.001; odds ratio = 5.0). Parental illiteracy (n = 258) was significantly associated with delayed diagnosis compared with maternal illiteracy (n = 192) (P = 0.01; odds ratio = 6.4). Children having more than two siblings (n = 181) were more delayed in presentation than those having two or less siblings (n = 120), (P = 0.001; odds ratio = 2.9). Among patients with delayed diagnosis, children living in an area >50 km from tertiary care hospital (65.3%) were more delayed than living within 50 km (P < 0.001; odds ratio = 4.3). None of the children with delayed diagnosis had fetal echocardiography done (P < 0.001). Children delivered at a hospital (23%) were less likely to have a delayed diagnosis than children delivered at home or a maternity clinic (77%) (odds ratio = 49; P < 0.001). Children with delayed diagnosis were significantly more undernourished with weight <3rd centile (60.7%) than children presenting early (39.3%) (P < 0.001). The referral pattern included 112 (31.6%) patients referred by a general practitioner, 171 (48.3%) by a pediatrician, 43 (12.2%) by an adult cardiologist, and 28 (7.9%) by a hospital practitioner. Children referred by a general practitioner (delayed referral 108 vs. optimal referral 4) were more delayed than a pediatrician (delayed referral 134 vs. optimal referral 37) (P < 0.001) [Table 1].
Table 1.
Frequency of qualitative data
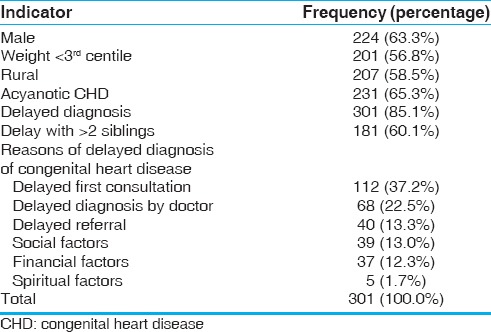
Table 2.
Pattern of CHD and delay in diagnosis according to disease subgroups
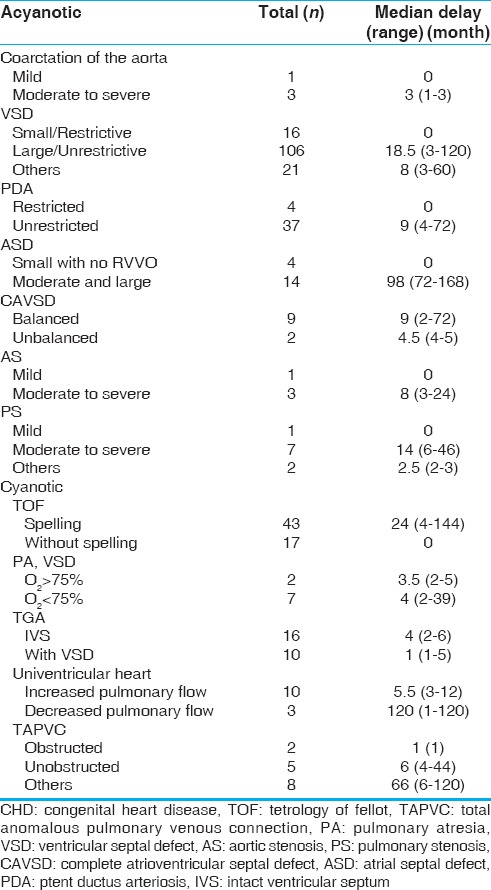
Figure 1.
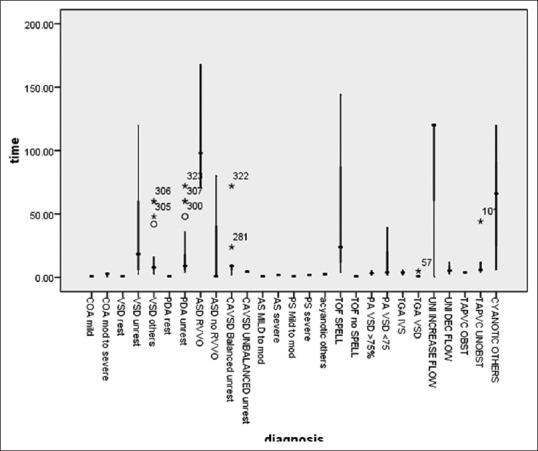
Delay in diagnosis according to disease subgroups
DISCUSSION
Unrecognized CHD carries a serious risk of avoidable mortality, morbidity, and permanent handicap.[9] Furthermore, failure to thrive, recurrent infections, and undernutrition adversely affects the long-term health of these children. Limitations in daily activities also have a significant impact on social development of these children. The economic and social impacts on families are also significant in the absence of state-sponsored social support.
In our study, the distribution of CHD was quite similar to the previously documented data. Male predominance found in our study has been documented in previous regional studies.[6] This may highlight a possible change in genetic substrate in South Asian population resulting in higher incidence in males rather than equal gender distribution in Western population. Another factor is cultural wherein a male gets more attention and is more likely to be brought to attention earlier than a female child. Children with CHD in our study were diagnosed at an older age (median 24 month, range 1 month to 14.8 year) than most of the previous studies from developed countries with well-established healthcare screening and referral programs. The mean age of diagnosis from various developing countries has been recorded much higher (median 4 years) emphasizing the need for proper screening programs in developing countries.[15] Such programs can be cost effective in broader view as early detection could prevent various permanent deficits requiring lifelong treatment with financial implications and poor productivity by the affected individual.
Almost 60% children belonged to rural areas, a figure consistent with the general population, figures of rural population of Pakistan (62%) as well as South Asia (65%).[16] This finding reiterates the fact that CHD is equally distributed in urban and rural populations and highlights the importance of provision of screening facilities in rural areas as well as early detection.
Nearly two-third of all children with CHD were having severe malnutrition with no significant difference between children with cyanotic and acyanotic CHD (P = 0.5). The incidence of malnutrition with weight below third centile was much higher than international literature. Malnutrition is prevalent in the region (26%), however, our data suggests a significantly higher prevalence in children with CHD.[17] Delayed diagnosis and late management not only compromised the optimal timing for intervention but also compounded by malnutrition that was significantly higher in children with delayed presentation when compared with normal population in this part of the world.[18] This puts these patients at an added risk of morbidity and mortality from congenital heart surgery.[19] This fact emphasizes additional need for nutritional and social support for these children as well as early interventions to prevent secondary complications from malnutrition itself.
In our study, acyanotic children had a much more delayed diagnosis than cyanotic children. This finding was similar to the previous local data.[20] This difference could partly be due to obvious finding of bluish discoloration of the child with CHD leading to earlier medical consultation by the parents or the attending doctor. On the other hand, acyanotic CHD with increased pulmonary blood flow were frequently misdiagnosed as pneumonia and accordingly managed until alternate diagnosis of CHD was established.
Parental education is an important determinant of delayed diagnosis of CHD. Literacy rate among mothers of children with CHD was only 54%. Mother’s illiteracy was significantly associated with delayed diagnosis of children (179 vs. 13, P < 0.001). Interestingly, literacy rate among fathers was much lower than the national statistics (27% vs. 69%). This low literacy rate was probably related to socioeconomic status of the family as more than two-third belonged to poor socioeconomic class and further 30% to the middle class. Delayed presentation in children with CHD was significantly associated with father’s literacy (P < 0.001). This factor has also been reported in the previous studies.[21] In our study, parental illiteracy (n = 238) was significantly associated with delayed diagnosis compared with maternal illiteracy. This finding was because of the prevalent social setup of the country with male-dominated society and decision-making powers of male partner. Hence, universal education for all is of utmost importance as literacy is equally important for mothers as well as fathers for proper care of their children and general awareness.[22]
Family planning goes hand in hand with better child health. It was also a factor in our study as delay was more common in families with more than two siblings and dependents (180 vs. 120, P < 0.001). This fact has been documented in a number of studies with smaller family size having a positive effect on better upbringing and optimal development of children.[23] Evidently, families with larger number of children cannot concentrate socially or financially on one child while neglecting others.[10]
Home deliveries or deliveries through untrained birth attendants are a major obstacle in screening children with CHD. High percentage of deliveries outside the hospital setting either because of financial constraints, nonavailability of adequate health facility nearby, or social taboos.[21] Home deliveries by untrained birth attendants accounted for 77.1% of all deliveries and amounted to 88.6% of all children with delayed diagnosis. Almost all patients delivered at home (97%) had a delayed diagnosis. With limited resources, providing additional hospital services may not be an option in short term but training birth attendants to identify and refer such patients for consultation can be very helpful in avoiding delays in diagnosis.[24]
Distance from medical facility was an important factor in timely diagnosis of these children. This fact has been documented in the previous studies.[25] Providing advanced diagnostic health facility at doorstep may not be feasible in a resource-constraint setting. However, proper planning and employing of telemedicine including transfer of echocardiography images may be an interim solution to avoid delaying critical diagnosis.
Antenatal diagnosis by fetal echocardiography is a useful screening tool for recognizing an early CHD and thus preventing neonatal morbidity and mortality. Antenatal diagnosis is getting universal in developed countries.[26] In our study, only 2% of mother had the antenatal diagnosis of CHD by fetal echocardiography and all of these had a timely referral with subsequent optimal management. Training the sonographers in a standard four-chamber and great vessels view on routine antenatal scans can increase the yield of a possible CHD significantly.[3]
We report one of the highest ratios of delayed diagnosis reported in the literature in recent times (85.1%). Although this is still a very high incidence of delayed diagnosis, the situation is better than data from a decade ago in a local study wherein it was 97%.[27] Most common reason for delayed diagnosis of CHD was delayed first consultation with a doctor (37.2%). This delay was mainly caused by difficult approach to a physician as most children with delayed diagnosis were residents of rural areas (60%) and belonged to poor socioeconomic strata (66%). This is a common problem in developing countries where many families in rural and semiurban areas seek advice from unqualified, self proclaimed quacks because of common beliefs and myths as well as illiteracy and socioeconomic constraints.[21]
Second major reason for delay was a delayed diagnosis by a health professional (22.5%). This results in a large proportion of children getting to a physician and yet having costly delay in diagnosis of CHD. Professional training and awareness was lacking in general practitioners and, to some extent, pediatricians, about the proper time for referral of the patients. Lack of awareness among primary care medical professionals has been highlighted; additional training advocated time and again avoiding missing such children in the previous studies.[24,28] Such training courses would be very beneficial in identifying these children with CHD early. Following an initial diagnosis, many children still did not reach an appropriate medical facility in time. This delay was again multifactorial. Saxena et al.[21] also reported poverty, difficult access to tertiary care facility, and large family size as some of the factors responsible for delayed treatment of CHD in India.
Although there was more delay in acyanotic CHD than cyanotic CHD but the median delay was different in different subset of patients with CHD. Nine patients with large VSD and a delayed diagnosis developed Eisenmenger syndrome and 4 (9.3%) patients with Tetralogy of Fallot developed neurological disability, which will definitely impact on surgical outcome of these patients. Such delay in diagnosis of this subset of children leads to irreversible damage and early demise of these patients. Such complications not only frequently necessitate hospital admissions but also further drain on family and health system resources.
Study limitations
There is considerable inherent ambiguity as far as definition of delay is concerned. It is really hard to label an absolute definition given the vast spectrum of disease severity and extraordinary variety of CHDs. The decision about optimal time for intervention was based on collective expert opinion and prevalent best practices guidelines. Second, data was collected from a single tertiary care hospital setting and that was also a study limitation. It only included patients who did reach a tertiary care facility and could not account for critical conditions and could not make it to such facility.
CONCLUSIONS
Acyanotic CHD was the most common lesion and had a significantly longer delay in diagnosis than cyanotic CHD. Many factors including poverty, illiteracy, inadequate health facilities, inappropriately trained health professionals at primary care level, lack of antenatal and immediate postnatal screening program, improper referral system, and social and financial issues were identified as causes of delayed diagnosis of CHD in our setup. Improving the basic socioeconomic indicators and establishing a proper screening and referral healthcare delivery system could save such children from avoidable morbidity and mortality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890–900. doi: 10.1016/s0735-1097(02)01886-7. [DOI] [PubMed] [Google Scholar]
- 2.Bjornard K, Riehle-Colarusso T, Gilboa SM, Correa A. Patterns in the prevalence of congenital heart defects, metropolitan Atlanta, 1978 to 2005. Birth Defects Res A Clin Mol Teratol. 2013;97:87–94. doi: 10.1002/bdra.23111. [DOI] [PubMed] [Google Scholar]
- 3.Rychik J, Ayres N, Cuneo B, Gotteiner N, Hornberger L, Spevak PJ, et al. American Society of Echocardiography guidelines and standards for performance of the fetal echocardiogram. J Am Soc Echocardiogr. 2004;17:803–10. doi: 10.1016/j.echo.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 4.Brown KL, Ridout DA, Hoskote A, Verhulst L, Ricci M, Bull C. Delayed diagnosis of congenital heart disease worsens preoperative condition and outcome of surgery in neonates. Heart. 2006;92:1298–302. doi: 10.1136/hrt.2005.078097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peterson C, Dawson A, Glidewell J, Garg LF, Braun KVN, Knapp MM, et al. Hospitalizations, costs, and mortality among infants with critical congenital heart disease: How important is timely detection? Birth Defects Res A Clin Mol Teratol. 2013;97:664–72. doi: 10.1002/bdra.23165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shirazi H, Haider N, Hassan M. Pattern of heart diseases in children. Ann Pak Inst Med Sci. 2008;4:50–5. [Google Scholar]
- 7.World Health Organization. Country Cooperation Strategy for WHO and Pakistan 2011–2017. Available at: http://www.who.int/countryfocus/cooperation_strategy/ccs_pak_en.pdf .
- 8.Pakistan Bureau of Statistics. Population size and growth of major cities. 1998 [Google Scholar]
- 9.Massin MM, Dessy H. Delayed recognition of congenital heart disease. Postgrad Med J. 2006;82:468–70. doi: 10.1136/pgmj.2005.044495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mughal AR, Sadiq M, Hyder SN, Qureshi AU, A Shah SS, Khan MA, Nasir JA. Socioeconomic status and impact of treatment on families of children with congenital heart disease. J Coll Physicians Surg Pak. 2011;21:398–402. [PubMed] [Google Scholar]
- 11.World Health Organization. Health topics: Poverty. Available at: http://www.who.int/topics/poverty/en .
- 12.Adult literacy. EFA global monitoring report 2015. 2nd ed. Paris: UNESCO; 2015. p. 135. Available at: unesdoc.unesco.org/images/0023/002322/232205e . [Google Scholar]
- 13.Referral systems – A summary of key processes to guide health services managers; improper referral. pp. 1–9. Available at: www.who.int/management/Referralnotes.doc .
- 14.Social education material: Social issues. Available at: http://culturesocial.blogspot.com/2011/08/definition-types-and-social-problem.html .
- 15.Mocumbi AO, Lameira E, Yaksh A, Paul L, Ferreira MB, Sidi D. Challenges on the management of congenital heart disease in developing countries. Int J Cardiol. 2011;148:285–8. doi: 10.1016/j.ijcard.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Rural population (% of total population) Available at: data.worldbank.org/indicator/SP.RUR.TOTL.ZS .
- 17.Shah SM, Selwyn BJ, Luby S, Merchant A, Bano R. Prevalence and correlates of stunting among children in rural Pakistan. Pediatr Int. 2003;45:49–53. doi: 10.1046/j.1442-200x.2003.01652.x. [DOI] [PubMed] [Google Scholar]
- 18.Vaidyanathan B, Nair SB, Sundaram KR, Babu UK, Shivaprakasha K, Rao SG, Kumar RK. Malnutrition in children with congenital heart disease (CHD) determinants and short-term impact of corrective intervention. Indian Pediatr. 2008;45:541–6. [PubMed] [Google Scholar]
- 19.Panni RZ. Earlier surgical intervention in congenital heart disease results in better outcome and resource utilization. BMC Health Services Res. 2011;11:353. doi: 10.1186/1472-6963-11-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khan IU, Muhammad A, Muhammad T. Pattern of congenital heart disease at Lady Reading Hospital, Peshawar. Gomel J Med Sci. 2011;9:174–7. [Google Scholar]
- 21.Saxena A. Congenital heart disease in India: A status report. Indian J Pediatr. 2005;72:595–8. doi: 10.1007/BF02724185. [DOI] [PubMed] [Google Scholar]
- 22.Children's HeartLink. Linked by a common purpose: Global efforts for improving pediatric heart health; A report by Children's HeartLink. 2007. Retrieved from: http://www.childrensheartlink.org/docs/globalreport .
- 23.Juhn C. The quantity-quality trade-off and the formation of cognitive and non-cognitive skills: National Bureau of Economic Research. 2015 [Google Scholar]
- 24.Liberman RF, Getz KD, Lin AE, Higgins CA, Sekhavat S, Markenson GR, Anderka M. Delayed diagnosis of critical congenital heart defects: Trends and associated factors. Pediatrics. 2014;134:e373–81. doi: 10.1542/peds.2013-3949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guy R, Donald J, Bijoy K, Eric R, Walter J, James B, et al. Remote telemedical interpretation of neonatal echocardiograms: Impact on clinical management in a primary care setting. JACC. 34;1;99:241–5. doi: 10.1016/s0735-1097(99)00182-5. [DOI] [PubMed] [Google Scholar]
- 26.Brown KL, Ridout DA, Hoskote A, Hoskote A, Verhulst L, Ricci M, et al. Delayed diagnosis of congenital heart disease worsens preoperative condition and outcome of surgery in neonates. Heart. 2006;92:1298–302. doi: 10.1136/hrt.2005.078097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sadiq M, Roshan B, Khan A, Latif F, Bashir I, Sheikh S, et al. Pattern of pediatric heart diseases in Pakistan. J Coll Physicians Surg Pak. 2002;12:149–53. [Google Scholar]
- 28.Schultz AH, Localio AR, Clark BJ, Ravishankar C, Videon N, Kimmel SE, et al. Epidemiologic features of the presentation of critical congenital heart disease: Implications for screening. Pediatrics. 2008;121:751. doi: 10.1542/peds.2007-0421. [DOI] [PubMed] [Google Scholar]


