Abstract
Background:
The number of grown ups with congenital heart diseases (GUCHs) is steadily increasing.
Aims:
To analyze factors predicting early cardiac morbidity following cardiac surgery in GUCH at a tertiary care center.
Setting and Design:
Retrospective study at a multispeciality tertiary referral center.
Methods:
Between January 2004 and December 2014, 1432 patients ≥13 years of age (acyanotic defects: 843, cyanotic defects: 589) underwent surgery for congenital heart defects. Factors associated with early cardiac morbidity were analyzed.
Statistical Analysis:
Univariable and multivariable analysis of all factors affecting outcomes.
Results:
On multivariate analysis, previous sternotomy, aortic cross-clamp time >45 min, cyanosis, and emergency procedure were independent predictors of early morbidity with respective odds ratios (ORs) of 12.4, 3.6, 2.6, and 8.1. For more precise estimation, a risk score was generated. Taking the log odds with each of these four as respective weights, a score was generated. The variables were previous sternotomy (2.5), aortic cross-clamp >45 min (1.3), emergency procedure (2.1), and cyanosis (0.9), if the respective condition is present, zero otherwise. The score ranged from 0 to 4.5. The average value of the score based on the four variables was significantly higher in cases with morbidity (1.85 ± 1.17) vs. (0.75 ± 0.88), P < 0.001. Distribution of scores was significantly different between patients with and without morbidity. Sixty-seven percent patients without any morbidity had score <1 compared to 24.6% with morbidity. Only 0.9% patients without morbidity had score of ≥3 compared to 16.4% patients with morbidity. Compared with patients having score <1, patients with scores 1-2 had OR of 3.4, 2-3 had OR of 6.0, and >3 had OR of 48.7.
Conclusion:
GUCH can be safely operated when adequate caution is taken in the presence of independent predictors such as previous sternotomy, aortic clamp time >45 min, cyanosis, and emergency procedure.
Keywords: Congenital heart disease in adults, delayed diagnosis, grown up congenital heart disease, reoperations
INTRODUCTION
Although the number of grown ups with congenital heart disease (GUCH) has steadily risen, their needs have not been addressed in most parts of the world.[1] Morbidity following surgery is relatively frequent and is generally associated with multiple preoperative, intraoperative, and postoperative factors. We therefore decided to review our experience with the management of GUCH over the past 10 years and attempted to analyze the factors related to early morbidity following cardiac surgery in a tertiary referral unit.
PATIENTS AND METHODS
Data of 1432 patients, 13 years of age or older with congenital heart disease (CHD), who underwent 1650 procedures during a 10-year period between January 2004 and January 2014, was retrospectively collected from available records. Ethics Committee clearance was obtained before performing this study. The patients were broadly divided into two categories: Those who had acyanotic CHD (n = 843) and cyanotic CHD (n = 589). Surgical procedures were divided into two groups, namely, repair procedures wherein anatomic correction was performed that restored separate pulmonary and systemic connections, and palliative procedures that improved patients' clinical status and longevity without restoration of normal anatomy. All preoperative, intraoperative, and postoperative variables were accumulated and analyzed in detail. Early morbidity was defined as occurrence of low cardiac output syndrome, new-onset postoperative arrhythmia, prolonged pleural drainage (>7 days), need for prolonged ventilator support, reexploration, revision of the procedure, tracheostomy, need for repeat cardiac catheterization, and requirement of permanent pacemaker implantation occurring in the index hospital admission or within 30 days of the operation if the patient had been discharged from the hospital. To elucidate the results further, the patients were divided into two surgical eras: January 2004 to December 2008 (n = 622) and January 2009 to December 2014 (n = 810).
Followup was performed through patients attending outpatient department (OPD) as a part of follow-up visit, through phone, or mail, and patients underwent clinical examination, chest X-rays, and echocardiography, if needed. Adverse events recorded were late death (cardiac or noncardiac), reoperation, interventional procedure, or worsening of symptoms.
Statistical analysis
All analysis was carried out using Stata version 12.1 software (Stata Corp, College Station, Texas, USA). Quantitative variables were compared between groups such as cyanotic CHD and acyanotic CHD with and without early cardiac morbidity using Student’s t test. Qualitative variables were compared between groups using a χ2 test/Fisher’s exact test. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated for early cardiac morbidity, using logistic regression analysis. Quantitative variables were categorized for ease of clinical interpretation. A stepwise multivariable logistic regression was carried out using the promising variables showing significant association with early morbidity in the univariable analysis. Using the significant variables found in the multivariable analysis, a risk score was generated for early morbidity. The number of significant factors present in each patient was also used as a risk indicator and ORs were calculated. A P value of <0.05 was considered to be statistically significant.
RESULTS
As GUCH includes both adolescents and adults,[2] age of our study group ranged from 13 to 65 years (mean 24.0 ± 10.3, median 21 years). On the basis of clinical presentation, 589 (41.2%) were cyanotic and 843 (58.9%) were acyanotic with 841 being male. The list of diagnosis and procedures done are presented in Tables 1 and 2.
Table 1.
Diagnostic spectrum of studied patients
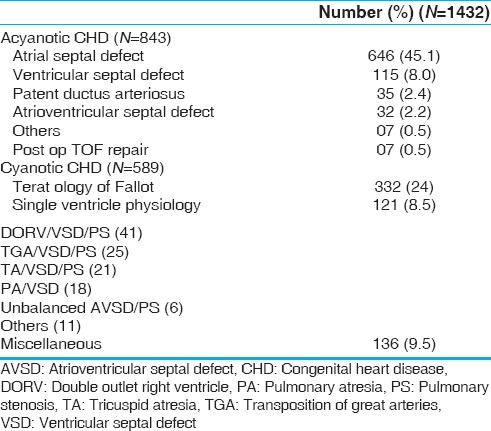
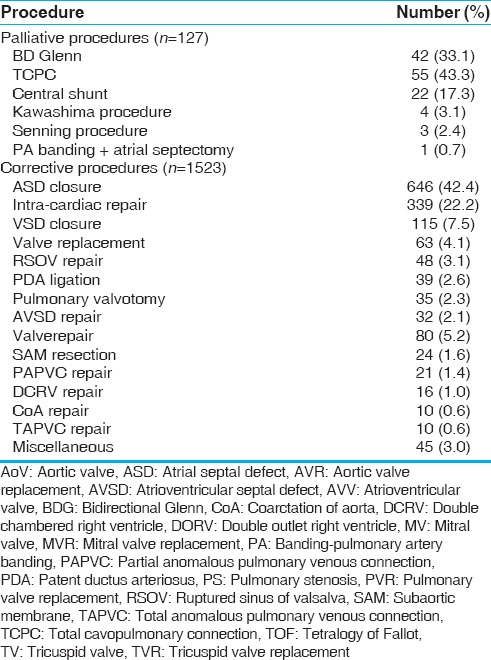
Table 2.
Details of procedures performed
Out of the 1432 patients, majority [1078 (75.4%)] were of New York Heart Association class II. One thousand three hundred and thirty-six patients (93.7%) were in normal sinus rhythm preoperatively. Arrhythmias included atrial fibrillation in 37 patients (2.5%), supraventricular tachycardia in 13 patients (0.9%), bundle branch block in 12 patients (0.8%), atrial flutter in 2, ventricular premature complexes in 3, and complete AV block in 2 patients. No data were available for 27 patients.
The preoperative diagnostic tool in the majority consisted of only transthoracic echocardiography (TTE) in 60% of patients (N = 854), whereas cardiac catheterization with cine-angiography was also performed along with TTE in 39% of patients (N = 578) to evaluate pulmonary artery pressures (n = 150), major aortopulmonary collateral arteries (n = 90), and coronaries (n = 80), and complete the diagnosis (n = 258). Cardiac magnetic resonance imaging was performed in 15 patients (1.0%) as a part of preoperative evaluation of right ventricle volume and function in Ebstein’s anomaly and postoperative patients with Tetralogy of Fallot (TOF) to aid decision making prior to pulmonary valve replacement. Preoperative and intraoperative characteristics are tabulated in Tables 3 and 4, respectively.
Table 3.
Preoperative characteristics of cyanotics and acyanotics
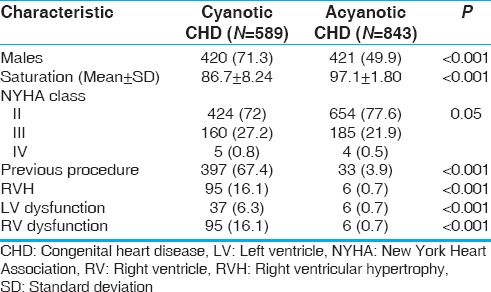
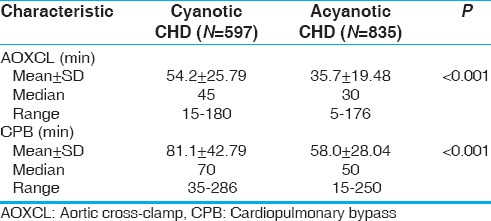
Table 4.
Intraoperative parameters of cyanotic and acyanotic congenital heart disease (CHD)
Sixteen cyanotic (4%) and 18 acyanotic (1.3%) who had undergone previous procedures in early infancy and childhood required a resternotomy and reoperations as GUCH. Seven patients underwent pulmonary valve replacement following intracardiac repair of TOF and were classified as acyanotics apart from five other patients who were cyanotic and required pulmonary valve replacement. Others included redo intracardiac repair (n = 7) for residual ventricular septal defect/pulmonary stenosis (VSD/PS), redo conduit repair for conduit degeneration/calcification (n = 2), and redo central shunt (n = 2). Among acyanotic patients also, valve replacement (n = 5) occupied the most common cause followed by previous valve repair. Others included residual VSD closure (n = 3) and redo valve repair (n = 3).
Of the 314 patients with TOF who underwent repair, majority had an anatomy amenable to repair through the right atrium. Only 52 patients needed transannular patching, 5 patients required associated pulmonary artery plasty, 5 patients needed conduit repair, 5 patients required associated aortic or tricuspid valve repair, 4 patients required pulmonary valve replacement because of absent pulmonary valve, and 2 patients required associated partial anomalous pulmonary venous connection repair.
There were 21 (1.5%) early deaths, 14 (2.3%) in cyanotic group and 7 (0.8%) in acyanotic group. The most common causes of death were low cardiac output syndrome (n = 7), sepsis (n = 5), bleeding (n = 3), unexplained sudden cardiac arrest (n = 3), and multiorgan dysfunction syndrome (n = 3). Overall, early postoperative morbidity was 74/1432 (5.2%, 95% CI: 4.1-6.4%). Of the 835 acyanotic patients, 21 (2.5%, 95% CI: 1.6-3.8%) experienced significant morbidity. Of the 597 cyanotic patients, 53 (8.9%, 95% CI: 6.7-11.5%) patients experienced early morbidity [Table 5].
Table 5.
Postoperative parameters of cyanotic and acyanotic congenital heart disease
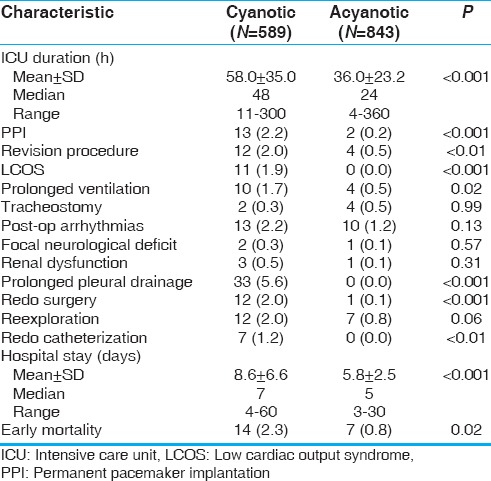
Mean ICU stay for all patients was 44.9 ± 29.8 h (range 4-360, median 42 h). Mean ICU stay was 58.0 ± 35.0 h (median = 48 h) in cyanotic patients, whereas it was 36.0 ± 23.20 h (median = 24 h) in acyanotic patients. Mean hospital stay was 8.6 ± 6.6 days (median = 7 days) in cyanotic patients, whereas 5.8 ± 2.4 days (median = 5 days) in acyanotic patients.
Postoperative complications occurred in 74 patients (5.2%) [Table 5]. Factors associated with early cardiac morbidity were analyzed by univariable logistic regression analysis and are listed in Table 6. On multivariable analysis, only four variables emerged as significant independent predictors of early cardiac morbidity. These were previous sternotomy (OR = 10.54), aortic cross-clamp time ≥45 min (OR = 3.74), cyanotic disease (OR = 2.26), and emergency procedure (OR = 8.01).
Table 6.
Predictors of early cardiac morbidity among GUCH
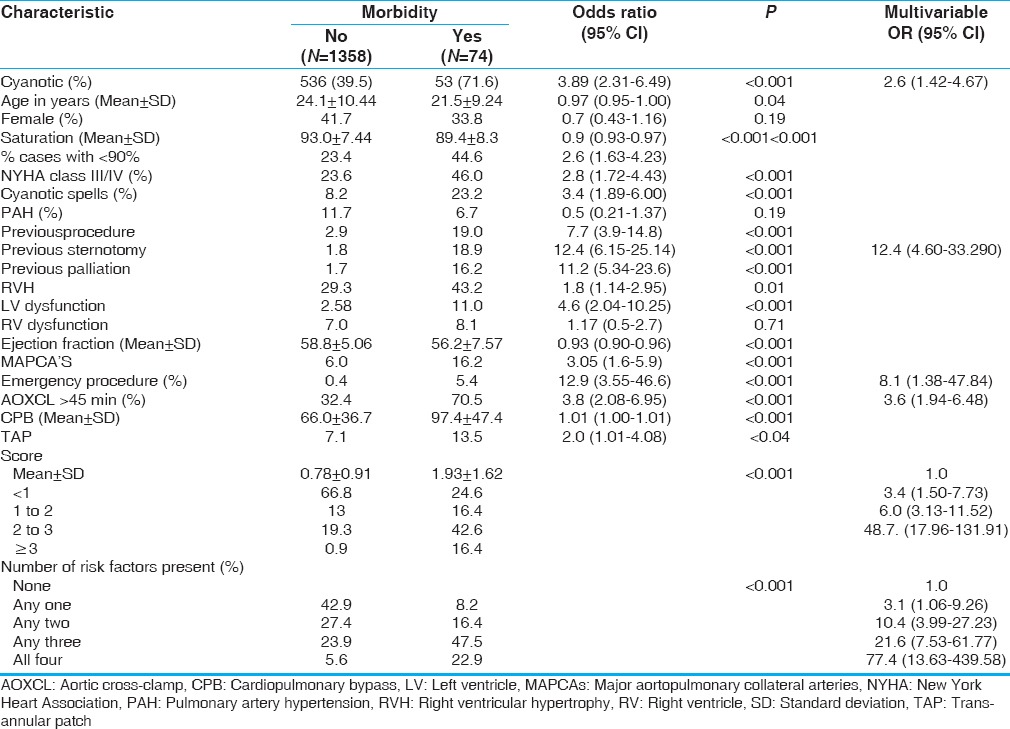
Taking the log odds of these four significant predictors as weights for the presence and zero for the absence of the respective predictors, a score was generated for each patient. The weights of previous sternotomy, emergency procedure, aortic cross-clamp time >45 min, and cyanosis were 2.4, 2.1, 1.3, and 0.8, respectively. The score ranged from 0 to 4.5. There was a significant difference in the average score and the distribution of the scores between those with and without early cardiac morbidity [Table 6]. Nearly 67% of cases in this study without any morbidity had a score of less than 1. Fifteen percent of cases in this study with morbidity had a score of more than 3. Compared with patients having a score of <1, patients with a score between 1 and 2 had an OR of 3.5; between 2 and 3 had an OR of 6.3; and >3 had an OR of 32.1 for cardiac morbidity [Table 7]. We also examined the risk associated with the four significant predictors in a simpler way. Compared to those patients with none of the four factors present, the risk of early morbidity increased as the number of risk factors present in a patient [Figure 1].
Table 7.
Analysis of the scores generated with and without morbidity
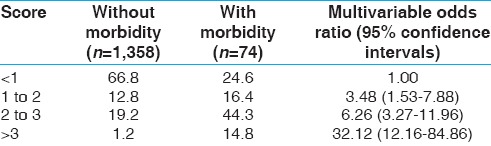
Figure 1.
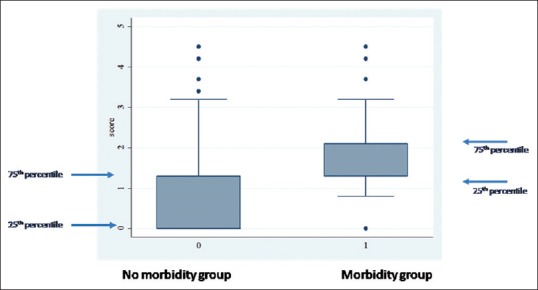
Box plot showing pattern of scores between patients without and with morbidity. The median value of the score among the group with no morbidity is close to zero, compared with 1.4 in the group with morbidity. The 75th percentile (which is the top of the box) among the group with no morbidity is lower than the 25th percentile (which is the bottom of the box) among the group with morbidity
FOLLOWUP
Followup ranged from 1 month to 10 years (mean 18.15 ± 16.13 months, median 12 months) and was 86% (1230/1432) complete. Most of the patients among atrial septal defect (ASD) operated in the initial study period were lost to followup. Late cardiac deaths were noticed in two cyanotic patients and late noncardiac-related death was noticed in one acyanotic patient. Most common reoperations included completion Fontan procedure (n = 15) and pulmonary valve replacement for severe pulmonary regurgitation in operated TOF patients (n = 12), aortic valve or mitral valve replacement following valve repair (n = 5), or correction of residual lesions (n = 12). During follow up most common adverse events noticed were due to arrhythmias (n = 23), pleural (n = 17) or pericardial (n = 5) effusions. Interventions in the form of embolization of major aortopulmonary collaterals for severe hemoptysis in three patients among cyanotic group and device closure of antegrade flow after total cavopulmonary connection (TCPC) in one surgically high-risk patient were performed.
DISCUSSION
The present study reviews our experience with a large population of GUCH, with the aim of determining risk factors for morbidity after surgery in GUCH population.
In this series, 5.3% were reoperations and the most common cause was pulmonary valve replacement for severe pulmonary regurgitation in patients who had undergone previous intracardiac repair of TOF. Although reoperations have become safer, we observed a higher mortality and morbidity in this group. The possible reasons cited in the literature for this are difficulties of surgical exposure because of adhesions, advanced age, and myocardial dysfunction.[3]
We also observed a higher operative mortality (2.3%) in the cyanotic group. As has been documented in the literature,[3,4] this is because of combined effects of long-term cyanosis on hemostasis, renal, and immune functions, preoperative lung or liver disease, prolonged cardiopulmonary bypass and aortic cross-clamp times, postoperative requirement of higher inotropic support, and presence of preoperative or postoperative cardiac dysfunction.
The median duration of ICU stay in our series was 1.8 days that was comparable to the results of Putman et al.[5](1.9 days), but lower when compared with Padalino et al.[6](2.3 days), European study[7](2.4 days), and Mello et al.[8](3.9 days). This reflects in our lower mean hospital stay also, which was for about 7 days. However, the latter was reported to be 10.5 days by Mello et al.[8], and 14.4 days by Putman et al.[5] and the European study.[7] The mortality rate in our study was 1.4%, which was comparable to the results of Putman et al.[5](1.5%) but lower than the results of the European study[7](2.0%), Mello et al.[8](2.5%), and Padalino et al.[6](3.1%). However, one must exercise caution when comparing our results with these published series as our patients were much younger and the number of reoperations was less. The larger number of patients with ASD may also have skewed the results.
The complication rate in our study was only 3.3%, when compared with 28, 29, and 33% in the studies by Padalino et al.,[6] Mello et al.,[8] and Putman et al.,[5] respectively. This lower complication rate might be because a majority of patients in our study were preoperatively in good clinical condition and patients with ASD constituted the majority.
The most common single precipitating factor for death in patients with GUCH is reoperation,[2,6,9] although in our study reoperation was a significant predictor of early cardiac morbidity rather than mortality. Reoperations in GUCH are mostly performed because of RVOT lesions and have been associated with low mortality rate if performed in a center with meticulous approach and considerable experience with a dedicated GUCH program. Only a few studies have addressed this issue and varied results have been reported.[10,11] In this study, the factors associated with early cardiac morbidity were analyzed by univariable regression analysis and factors, as listed in Table 5, and were found to be relevant. However, in the final analysis, the only four significant independent predictors identified were previous sternotomy, emergency procedure, aortic cross-clamp time >45 min, and cyanosis with respective ORs of 10.5, 8.0, 3.7, and 2.3, respectively. These four factors could together discriminate 77% of all procedures correctly as to their immediate postoperative cardiac morbidity.
The proportion of patients with complex CHD increased from 28% (177/622) in January 2004 to December 2008 to 39% (316/810) in January 2009-2014. Pulmonary valve replacements in operated TOF increased from four cases in January 2004 to December 2008 to eight cases in January 2009-2014. Conduit replacement increased from one case to seven cases and double switch operation from zero to six cases. Increased number of off-pump TCPC (18/56) was being performed from January 2009 to 2014 when compared with none performed between 2004 and 2008. The percentage of repeat operations increased from 1.4% (11/622) in January 2004 to December 2008 to 4.0% (32/810) in January 2009-2014. Out of the 21 deaths, 8 occurred in the first era and 13 occurred in the second era. We observed that the operations had increased in complexity because of both the increased incidence of repeat operations and by increased use of technically demanding procedures such as double switch operation, redo conduit repair, and others. This increased cardiopulmonary bypass and aortic cross-clamp times, ICU and hospital stay, and morbidity. Nevertheless, mortality did not increase reflecting our growing experience with this patient subset.
Giamberti et al.[10] studied 164 reoperated patients with GUCH and identified cardiopulmonary bypass (CPB) duration, timing of reoperation and cyanosis, congestive cardiac failure, and number of previous operations as major causes of morbidity among patients with GUCH. They concluded that CPB duration was the most important independent predictor of morbidity as it implies the complexity of the procedure. This is similar to our data. Preoperative cyanosis is an important risk factor for early and mid-term outcome of patients with GUCH.[5,11,4] Long-standing cyanosis is associated with complex congenital cardiac disorders, major aortopulmonary collaterals, bleeding disorders, and cardiac dysfunction.[3]
In a study of 66 patients, Berdat et al.,[11] identified cyanosis, poor ventricular function, prolonged CPB time, and aortic cross-clamp time as risk factors for adverse outcomes which is similar to our findings. Thus, timely intervention before onset of ventricular dysfunction is recommended to reduce the risk of early morbidity and improve outcome. Recently, a consensus-based risk stratification model has been developed by a 11-member panel of pediatric cardiologists and cardiac surgeons (RACHS - 1 Risk Adjustment for Congenital Heart surgery Score) to stratify in-hospital mortality risk in patients with CHD by age, diagnosis, and surgical procedure. It was found that single ventricle anatomy, younger age and presence of major non-cardiac structural anomalies increases the risk of mortality.[12,4] Our findings are similar to these reports although all factors failed to reach statistical significance on multivariate analysis. We believe that for developing a validated risk-adjustment score, multi-institutional studies are needed.
Abarbanell et al.[4] reviewed 234 patients with GUCH and concluded that prolonged CPB and aortic cross-clamp times were significant predictors of mortality along with other factors such as preoperative lung or liver disease, elevated inotropic score, and serum lactate. This supports the present study that also identified prolonged cross-clamp time as one of the independent predictors of early cardiac morbidity in GUCH population.
Mascio et al.[13] analyzed 5265 patients from the Society of Thoracic Surgeons congenital heart surgery database and reported 2.1% in-hospital mortality and 5 days median length of hospital stay that was comparable with the present study (1.5% in-hospital mortality and 7 days median hospital stay). The mortality and morbidity were higher in the Fontan conversion group in view of associated comorbidities with this group.
STUDY LIMITATIONS
This is a retrospective study limited to a single center. As most of the patients come from rural areas, loss of followup is not uncommon especially if patients have no symptoms. Therefore, follow-up completeness of this study is only 86%. Only surgically palliated patients are included in this study. Those who had undergone percutaneous interventions were not included. Ideally, a study should include all forms of therapy in such patients. The other limitation is that a variety of simple lesions may have skewed the results.
CONCLUSION
The outcome of surgical management of GUCH is encouraging. Our analysis predicts a good mid-term outcome that encourages surgeons to be relatively optimistic in managing this difficult category of patients. Identified independent predictors of early morbidity are previous sternotomy, emergency procedure, aortic cross-clamp time >45 min, and cyanosis. However, further studies are required to develop a robust risk stratification model for this emerging GUCH population. As GUCH population continues to grow in number over the coming years, with an expected increase in number of complex diseases, continued clinical vigilance will be required to maintain or improve outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Webb GD. Care of adults with congenital heart disease. A challenge for the new millennium. Thorac Cardiovasc Surg. 2001;49:30–4. doi: 10.1055/s-2001-9918. [DOI] [PubMed] [Google Scholar]
- 2.Somerville J. Grown-up congenital heart disease – Medical demands look back, look forward 2000. Thorac Cardiovasc Surg. 2001;49:21–6. doi: 10.1055/s-2001-9911. [DOI] [PubMed] [Google Scholar]
- 3.Dore A, Glancy DL, Stone S, Menashe VD, Somerville J. Cardiac surgery for grown-up congenital heart patients: Survey of 307 consecutive operations from 1991 to 1994. Am J Cardiol. 1997;80:906–13. doi: 10.1016/s0002-9149(97)00544-4. [DOI] [PubMed] [Google Scholar]
- 4.Abarbanell GL, Goldberg CS, Devaney EJ, Ohye RG, Bove EL, Charpie JR. Early surgical morbidity and mortality in adults with congenital heart disease: The University of Michigan experience. Congenit Heart Dis. 2008;3:82–9. doi: 10.1111/j.1747-0803.2008.00170.x. [DOI] [PubMed] [Google Scholar]
- 5.Putman LM, vanGameren M, Meijboom FJ, de Jong PL, Roos-Hesselink JW, Witsenburg M, et al. Seventeen years of adult congenital heart surgery: A single centre experience. Eur J Cardiothoracic Surg. 2009;36:96–104. doi: 10.1016/j.ejcts.2009.01.046. [DOI] [PubMed] [Google Scholar]
- 6.Padalino MA, Speggiorin S, Rizzoli G, Crupi G, Vida VL, Bernabei M, et al. Midterm results of surgical intervention for congenital heart disease in adults: An Italian multicentre study. J Thorac Cardiovasc Surg. 2007;134:106–13. doi: 10.1016/j.jtcvs.2007.01.080. [DOI] [PubMed] [Google Scholar]
- 7.Vida VL, Berggren H, Brawn WJ, Daenen W, Di Carlo D, Di Donato R, et al. Risk of surgery for congenital heart disease in the adult: A multicentered European study. Ann Thorac Surg. 2007;83:161–8. doi: 10.1016/j.athoracsur.2006.07.045. [DOI] [PubMed] [Google Scholar]
- 8.Mello GA, Carvalho JL, Baucia JA, MagalhaesFilho J. Adults with congenital heart disease undergoing first surgery: Prevalence and outcomes at a tertiary hospital. Rev Bras Cir Cardiovasc. 2012;27:529–34. doi: 10.5935/1678-9741.20120094. [DOI] [PubMed] [Google Scholar]
- 9.Somerville J. Near misses and disasters in the treatment of grownup congenital heart patients. J R Soc Med. 1997;90:124–7. doi: 10.1177/014107689709000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giamberti A, Chessa M, Abella R, Butera G, Carlucci C, Nuri H, et al. Morbidity and mortality risk factors in adults with congenital heart disease undergoing cardiac reoperations. Ann Thorac Surg. 2009;88:1284–9. doi: 10.1016/j.athoracsur.2009.05.060. [DOI] [PubMed] [Google Scholar]
- 11.Berdat PA, Immer F, Pfammatter JP, Carrel T. Reoperations in adults with congenital heart disease: Analysis of early outcome. Int J Cardiol. 2004;93:239–45. doi: 10.1016/j.ijcard.2003.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002;123:110–8. doi: 10.1067/mtc.2002.119064. [DOI] [PubMed] [Google Scholar]
- 13.Mascio CE, Pasquali SK, Jacobs JP, Jacobs ML, Austin EH. Outcomes in adult congenital heart surgery: Analysis of the Society of Thoracic Surgeons (STS) database. J Thorac Cardiovasc Surg. 2011;142:1090–97. doi: 10.1016/j.jtcvs.2011.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]


