ABSTRACT
The effective treatment of adult and pediatric malignant glioma is a significant clinical challenge. In adults, glioblastoma (GBM) accounts for the majority of malignant glioma diagnoses with a median survival of 14.6 mo. In children, malignant glioma accounts for 20% of primary CNS tumors with a median survival of less than 1 y. Here, we discuss vaccine treatment for children diagnosed with malignant glioma, through targeting EphA2, IL-13Rα2 and/or histone H3 K27M, while in adults, treatments with RINTEGA, Prophage Series G-100 and dendritic cells are explored. We conclude by proposing new strategies that are built on current vaccine technologies and improved upon with novel combinatorial approaches.
Keywords: Cancer immunity, cancer vaccines, Dendritic cell vaccine, glioma, HSPPC-96, Immunosuppression, pediatric glioma, Rindopepimut
Introduction
Malignant glioma
Primary brain tumors have an annual incidence of ∼5 in 100,000 adults.1-3 Within the United States, it is estimated that there will be 24,790 newly diagnosed malignant brain cancer patients in the year 2016.4 Glioblastoma (GBM) is the most common primary malignant central nervous system (CNS) tumor in adults, accounting for ∼54% of all malignant glioma diagnoses.5,6 Despite the current standard of care regimen including maximum surgical resection, radiotherapy (RT) and chemotherapy, median overall survival (OS) remains at 14.6 mo with less than 26% of patients surviving at 2 y post-diagnosis.7-9 In the absence of therapy, OS is limited to 30–35 weeks.10-13 The poor outcome for GBM patients is largely due to the molecular and cellular heterogeneity of the cancer, which equips the tumor with multiple strategies for adapting to and overcoming the effects of therapy.14
Pediatric high-grade glioma (HGG) is clinically and biologically distinct from adult glioma. However, similar to adult GBM, these tumors are a major contributor toward cancer-related morbidity and mortality in infants, children, and adolescents, with long-term survival rates of only 10–15%.15 Pediatric HGG is found throughout the CNS, with those tumors localizing to the ventral pons of the brainstem possessing a particularly devastating prognosis. Commonly referred to as diffuse intrinsic pontine glioma (DIPG), these highly malignant tumors primarily affect young children with a peak incidence at 6 y of age and possess a high mortality rate when compared among all childhood solid cancers. Children diagnosed with DIPG possess a median survival of 9 mo and virtually all patients die within 2 y. Immunotherapy has been proposed as an approach for treating both pediatric and adult glioma. Here, we review targeted vaccination approaches for these tumors and discuss strategies for enhancing future therapeutic efficacy.
Immunosuppression
While the cellular composition and molecular profile of GBM varies, the immunosuppressive microenvironment is a consistent feature of these tumors. The accumulation of tumor-infiltrating myeloid-derived suppressor cells 16,17 and regulatory T cells (Treg; CD4+CD25+FoxP3+),18,19 the presence of IDO1,20,21 interleukin-10 (IL-10) and transforming growth factor-β (TGF-β), collectively contribute to the suppression of normal tumor surveillance.22-24 Additionally, PD-L1, a ligand highly expressed by GBM-infiltrating macrophages 25 and GBM cells,26 interacts with PD-1 on cytotoxic T cells, further contributing toward immunoevasion of antitumor immunity. Similarly, CTLA-4, a molecule constitutively expressed by Tregs, suppresses T cell cytotoxic activity,27 and is another mediator of immunotolerance.28,29 Beyond the immediate microenvironment of GBM, systemic lymphopenia is the result of cytotoxic therapy and coincident with a decreased expression of HLA-ABC, HLA-DR, CD86, ICAM-1 and TNFRII on peripheral blood monocytes.30 Decreased MHC expression on antigen-presenting cells (APCs) in lymphopenic patients further limits GBM-specific T cell activity and function. Therefore, the immunosuppressive properties of malignant glioma may well act synergistically with cytotoxic therapies to compromise the patient's immune-mediated antitumor response, with these combined effects providing additional impetus for testing numerous immune checkpoint blockade strategies in ongoing clinical trials.31
Much less is known about immunosuppressive mechanisms underlying malignant glioma in children, but this is an active area of preclinical research, currently ongoing within and external to our group. With advanced techniques that spare critical brain function during tumor biopsy becoming more common, in addition to the preclinical models that have recently been developed, more information about the novel immunosuppressive nature of pediatric HGG is likely to significantly increase during the next several years.
Antigenic targets
Glioma expresses a number of antigenic targets, including tumor-associated antigens (TAAs) that are not a direct result of mutagenic events, such as interleukin-13 receptor α 2 (IL-13Rα2). Additionally, they can also express tumor-specific antigens (TSAs) that are the result of mutant protein expression, such as epidermal growth factor receptor variant III (EGFRvIII). The select overexpression of wild-type epitopes, as well as the unique expression of mutant epitopes, has provided the solid foundation for vaccination approaches aimed at malignant glioma treatment.32-51 Recent work has helped distinguish pediatric HGG from adult GBM by characterizing unique epigenetic alterations that are exclusive to brain tumors in children.35 One classic example is the Lys27Met (K27M) missense mutation in genes encoding histone 3 isoforms, often found in midline malignant glioma and in up to 80% of DIPG patients 36-38; providing a novel tumor-specific vaccination target.
Vaccines for treatment of adult malignant glioma
RINTEGA/Rindopepimut
Whereas GBM is known to express several mutant proteins, EGFRvIII is the only TSA currently being investigated as a vaccine target in patients diagnosed with GBM (Fig. 1). EGFRvIII is the result of an in-frame deletion of 801 nucleotides (exons 2–7) of the wild-type gene. The mutation manifests as a shortened protein containing a novel glycine residue at the exon 1–8 in-frame junction.52 The mutant epitope is presented in the extracellular space, with the transmembrane and cytoplasmic portions of the altered receptor left intact. The occurrence of EGFRvIII in GBM is almost always in the context of corresponding mutant gene amplification, resulting in a high level of expression.53 In a preclinical GBM model, the ectopic expression of EGFRvIII caused increased tumor growth, following subcutaneous and intracranial engraftment of modified cells.54 Therapeutically, mice bearing established tumors and treated with the combination of rindopepimut, which consists of the EGFRvIII junction sequence conjugated to keyhole limpet hemocyanin (KLH) and complete Freund's adjuvant, showed an average survival increase of >120 d (p = 0.014): a 173% gain when compared to vehicle-treated mice.55 Clinically, the presence of EGFRvIII is independently prognostic for decreased OS56-59 Accordingly, Phase I and II clinical trials treating newly diagnosed GBM patients with RINTEGA, the tradename for rindopepimut, found an increase in median OS when compared to historical controls and was well tolerated (Table 1).60,61 ACTIII (n = 65), the largest of the Phase II studies utilizing RINTEGA, demonstrated a PFS of 12.3 mo and median OS of 24.6 mo in GBM patients.62 Recently, ACTIV, the first Phase III study investigating the benefits of RINTEGA in newly diagnosed GBM patients, was ended in accordance with a recommendation by the trial's independent Data Safety and Monitoring Board which concluded that the study would not reach statistical significance for OS.63 Notably, 43% of vaccine-treated patients showed evidence of a humoral response to EGFRvIII. Furthermore, at the time of tumor regrowth following treatment, 82% of the recurrent GBM demonstrated loss of EGFRvIII expression, suggesting that EGFRvIII-positive GBM evades the antitumor-mediated effects of RINTEGA by suppressing the expression of EGFRvIII.59
Figure 1.
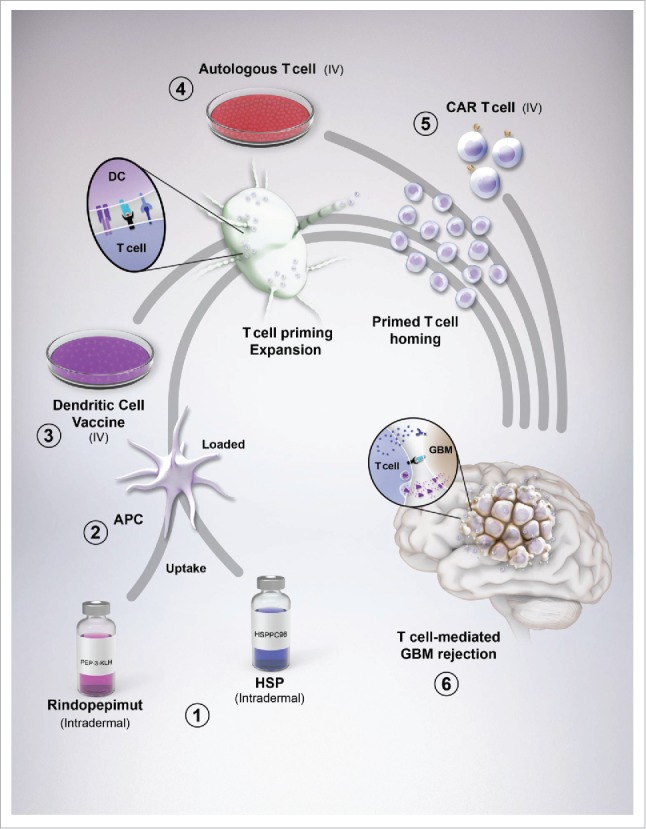
Glioblastoma (GBM) vaccines and their interaction with immunity. (1) Rindopepimut (RINTEGA), a synthetic peptide vaccine targeted at the EGFRvIII mutation, and HSPPC-96 (Prophage), an autologous-derived complex consisting of heat shock proteins complexed with GBM antigens, are intradermally injected for uptake by resident dendritic cells (DC). (2) The vaccines are co-administered with adjuvants, such as GM-CSF and keyhole limpet hemocyanin (with respect to RINTEGA) for stimulating DC uptake, antigen processing and upregulation of costimulatory molecules. (3) Peripheral blood mononuclear cells can be isolated from patient blood (not shown), expanded in culture, primed with autologous patient-derived GBM tumor lysate, followed by intravenous transfer back into the patient, bypassing the need for dermal injection of tumor antigens. Regardless of whether DCs are primed and loaded in culture, or a cutaneous route, DC drain to lymphoid tissue for subsequent T cell activation and expansion. (4) Similar to PBMC isolation for DC preparation, autologous T cells can also be isolated from this pool. These cells can be (re-)stimulated with plate-bound anti-human CD3ϵ, without anti-CD28, as to only (re-)engage the experience T cells that might respond to TAAs. This CD3ϵ-targeted stimulation can be further boosted by adding in cytokines that favor a proinflammatory/antitumor T cell subset such as IL-2, IL-12 and IL-15. (5) An alternative to simple autologous T cell isolation, (re-)priming and expansion, is by engineering the T cell to be highly specific to a GBM-expressed antigen, in the form of a chimeric antigen receptor-expressing T cell. This step provides a high level of stringency and targeting for all T cell adoptively transferred into the GBM patient. Ultimately, the goal of all vaccines is to eventually cause GBM-specific T cells to infiltrate the tumor and elicit immune-mediated rejection.
Table 1.
Clinical efficacy of vaccines for patients with newly diagnosed adult GBM or pediatric DIPG. *Trial closed ahead of stated objectives.
| Newly diagnosed adult GBM |
|||||||
|---|---|---|---|---|---|---|---|
| Therapeutic mediator(s) | Percent eligible | Trial (Phase) | n | PFS (weeks) | OS (weeks) | References | |
| Current standard (resection, radiation, temodar) | 29.6 | 62.6 | |||||
| RINTEGA (Rindopepimut) | 27–67 | ACTII (II) | 22 | 65.6 | 104.6 | 61 | |
| ACTIII (II) | 65 | 52.7 | 105.4 | NCT00458601 | |||
| ACTIVATE (II) | 18 | 60.9 | 105.4 | NCT00643097 | |||
| ACTIV (III) | Control Arm | 700 | 91.7 | 119 | |||
| Rintega Arm | 88.6 | ||||||
| Prophage series G-100 (HSPPC-96) | 60–65 | Prophage series G-100 (II) | 46 | 76.3 | 99.9 | NCT00905060 | |
| DCs | 60–65 | Tumor lysate (I) | 12 | 66.4 | 100.2 | 82 | |
| 100 | RT and TMZ with DCs (PGE2 and TNFα) (I) | 11 | 40.7 | 120 | 85 | ||
| 60–65 | ICT-107 (I) | 16 | 72.4 | 164.6 | 83 | ||
| ICT-107 (II) | Placebo | 43 | 9 | 16.7 | NCT01280552 | ||
| ICT-107 | 81 | 11.2 | 18.3 | ||||
| T cells | 100 | CAR T cell (I) | Ongoing | Ongoing | NCT01454596 | ||
| Recurrent adult GBM | |||||||
| Current standard (currently no effective therapy) | 9 | 35 | |||||
| RINTEGA (Rindopepimut) | 27–67 | ReACT | Ongoing | Ongoing | NCT01498328 | ||
| Prophage series G-100 | 60–65 | Phase I | 12 | 47 | 120 | ||
| Phase II | 41 | 19.1 | 42.6 | 69 | |||
| Pediatric malignant gliomas | |||||||
| Current standard (radiation) | 13–26 | 30.8–60.8 | |||||
| Peptide based | Phase I | 14 | 55.2 | 86 | |||
| DC | Phase I | 33 | 19 | 59 | 88 | ||
| Autologous lysate pulsed DCs (I) | 3 | 144.7 | 87 | ||||
| HSPPC-96 | Phase I | Ongoing | Ongoing | NCT02722512 | |||
Prophage series G-100/HSPPC-96
Prophage series G-100 is a clinical vaccine utilizing heat shock protein peptide complex 96 (HSPPC-96). The HSPPC-96 treatment strategy relies on heat shock protein (HSP) family member gp96 interactions with intracellular peptides in tumor and tumor-associated APCs. In 1986, Srivastava et al., demonstrated that tumor-derived gp96 facilitates intrinsic immunogenicity as a proof-of-concept vaccine in a model of fibrosarcoma 64 leading to priming of CD8+ 65 and CD4+ T cells 66 in wild-type Balb/c mice as a result of APC presentation of tumor-specific peptides by MHC I and II, respectively.67 In clinical trials for treating GBM, HSPPC-96-peptide complex is isolated from a patient's tumor, and then used as an autologous vaccine in treating the same patient.68 Based on the ability to induce a presumably multi-epitope specific immune response against a patient's resected tumor, HSPPC-96 vaccination is considered to be a form of personalized medicine.69 A preclinical model for HSPPC-96 vaccination in GBM does not yet exist, although this is an active area of investigation by our group.
A notable limitation to the HSPPC-96 approach for treating GBM is the requirement for a minimum of 7 g resected tumor tissue. Therefore, ∼35–40% of all GBM patients do not qualify for autologous HSPPC-96 vaccination due to insufficient resected tumor (Table 2).70,71 Nonetheless, a Phase II study of newly diagnosed GBM patients (n = 46), whose resected tumors were of appropriate mass, received Prophage Series G-100 and experienced PFS of 17.8 mo and median OS of 23.3 mo: both representing substantial improvements when compared to historical control values.72 Moreover, a phase II trial of recurrent GBM patients treated with HSPPC-96 yielded results showing PFS of 19.1 weeks and median OS of 42.6 weeks (n = 46). These values also represent substantial increases relative to historical controls (PFS of 9 weeks and an OS of 35 weeks). Interestingly, patients diagnosed with lymphopenia at the time of vaccination were associated with a poor survival outcome.69
Table 2.
Factors that limit patient selection for vaccine therapy.
| Therapeutic mediators | Vaccine | Limiting factors |
|---|---|---|
| RINTEGA (Rindopepimut) | Synthetic peptide |
|
| Prophage series G-100 (HSPPC-96) | Tumor lysate isolation |
|
| DCs | Tumor-lysate pulsed DCs |
|
| Lysate-pulsed DCs (PGE2 and TNFα) |
|
|
| Synthetic peptide-pulsed DCs |
|
|
| T Cells | CAR T cells |
|
Dendritic cells (DCs)
DCs are immunological sentinels that respond to tissue injury, inflammatory stimuli and/or changes of cellular homeostasis, such as hypoxia, acidity or osmolarity. DCs internalize, process and present antigens to T cells that facilitate epitope-specific immune responses.73,74 DCs can be expanded in vitro, for subsequent administration to cancer patients, using a variety of methods that include the isolation of circulating monocytes or bone-marrow-derived precursor cells that can differentiate, ex vivo, and become DCs.75-79 Pre-clinically, DCs treated with murine GL261 glioma lysates have been administered to C57BL6 mice, at one week post-intracranial injection of GL261 cells, with DC administration resulting in a reduction of tumor growth: 78.5 mm3 (control) to 39.9 mm3. An alternative approach has utilized DCs treated with a tumor extract-cationic liposome complex (synthetic small unilamellar vesicles), which results in a dramatic decrease in tumor volume relative to the control group of mice (p < 0.01).80 Similarly, in a rat glioma model, vaccination with bone-marrow-derived DCs, pulsed with acid-eluted peptides from syngeneic cells, results in an increased median OS from 16 (control) to 35 d (p = 0.027).81
Clinically, newly diagnosed GBM patients (n = 12) treated with autologous DCs and pulsed with acid-eluted tumor peptides demonstrates a PFS of 15.5 mo and median OS of 23.4 mo. In 4/12 patients, survival is >30 mo and tumors isolated at recurrence show robust CD3 T cell infiltration when compared to corresponding untreated tumor obtained at the time of initial surgery. In contrast, 4 of 12 patients that succumbed to tumor within 12 mo post-treatment initiation show decreased T cell infiltration of recurrent tumor, suggesting that T cell exclusion was an important determinant of therapeutic outcome.82 Another Phase I trial studying newly diagnosed GBM patients (n = 16) treated with DCs pulsed with HER2/neu, TRP-2, AIM-2, MAGE1 and IL13Rα2 antigens (ICT-107; Immunocellular Therapeutics Ltd.) yielded results showing PFS of 16.9 mo and median OS of 38.4 mo.83 In a recent randomized Phase II study of ICT-107 treatment in newly diagnosed GBM patients (n = 124), median PFS is 11.2 mo and median OS is 18.3 mo when compared to a PFS and OS of 9 mo (p = 0.01) and 16.7 mo, respectively, in patients treated with control dendritic cells.84 A Phase III study for ICT-107 is currently recruiting patients (NCT02546102). In yet another Phase II trial, GBM patients (n = 11) treated with radiation and temozolomide (TMZ), followed by vaccination with autologous tumor lysate-loaded DCs primed with PGE2 and TNF-α had a PFS of 9.5 mo and median OS of 28 mo. The frequency of CD4+ T cells in post-vaccination tumor tissue was significantly increased (p = 0.004) relative to pre-vaccination, whereas the frequency of CD8+ T cells was not significantly changed.85 Notably, a number of Phase II DC vaccine trials are ongoing, including studies whereby DCs are treated with: autogenic glioma stem-like cells (A2B5+) (NCT01567202), CMV RNA plus tetanus-diptheria toxoid (NCT02465268) and autologous tumor lysate plus resiquimod or adjuvant poly-ICLC (NCT01204684).
Vaccines for treatment of pediatric malignant glioma
Relative to vaccine attempts in the setting of adult GBM, analogous pursuits have been modest with respect to treating children diagnosed with malignant glioma. In a Phase I trial of newly diagnosed DIPG (n = 26), a peptide vaccine against the glioma-associated antigens, EphA2, IL-13Rα2 and survivin were targeted. In addition to safety aspects of the study, which were satisfactory in avoiding grade III or higher systemic toxicities, patients had an OS of 55.2 weeks, representing a substantial increase over historical control levels of 39–43 weeks. Inclusion in this trial required patients with HLA-A2-positive status and minimal or no dexamethasone usage at the time of enrollment.86 In a separate Phase I trial of newly diagnosed patients with HGG between the ages of 1 and 18, autologous tumor lysate-pulsed DCs were generated for 3/9 enrolled patients with 2 of the DC-treated individuals still alive at 40 and 51 mo post-surgery, respectively.87 Another Phase I trial using DCs treated with tumor lysate in 33 malignant glioma patients showed an average PFS of 19 weeks and OS of 59 weeks, with 7 patients surviving at the time of publication.88 A Phase I study utilizing the HSPPC-96 vaccine for treatment of pediatric malignant glioma recently opened at the Ann and Robert H. Lurie Children's Hospital of Chicago (NCT02722512). Also notable is an effort to leverage the presence of H3K27M mutations found in the high percentage of midline malignant glioma cases in the soon to open H3K27M peptide vaccine trial (S. Mueller, personal communication). Although no Phase II studies have reported results using vaccines in pediatric patients, preliminary results that address safety and tolerability indicate a high level of feasibility in the pediatric cohort with HGG.
Improving vaccine efficacy
Combinatorial approaches
Whereas vaccines aim to induce tumor-specific immune responses, effective immunotherapy against cancer requires the co-treatment against tumor-induced immune evasion. In patients diagnosed with GBM, as well as other cancers, spontaneous T cell infiltration has been associated with improved survival.89-94 However, the basis for this relationship has been difficult to describe comprehensively. One possibility is that the necrotic release of DNA from tumor cells leads to activation of the stimulator of interferon genes (STING) pathway, providing a mechanism for T cell recruitment to tumor.95 However, in malignancies with potent and active immunoevasive mechanisms, T cell infiltration, alone, is unlikely to change patient outcome.96 New strategies that engage STING, while simultaneously inhibiting a tumor's immunosuppressive activity, may help to recruit vaccine-conditioned cytotoxic T cells from the periphery to CNS, thereby promoting more effective tumor rejection that results in greater patient survival.
Future clinical studies should be designed to provide patients with multiple therapies to address the immunosuppressive phenotype present in adult GBM and pediatric HGG, while also aiming to improve T cell infiltration and T-cell-mediated killing of tumor cells. Although the optimal timing for administration of each treatment type (RT, chemotherapy, immunotherapy, vaccination, etc.) still requires further investigation. As shown in Fig. 2, it may be beneficial to treat malignant glioma with radio-/chemotherapy to (1) release TSA, (2) increase inflammatory cues responsible for immune cell recruitment and (3) facilitate the signals required for APC uptake and maturation. Therefore, vaccination in combination with standard of care therapies may promote a more effective antitumor T cell response with the benefit of improved survival.
Figure 2.
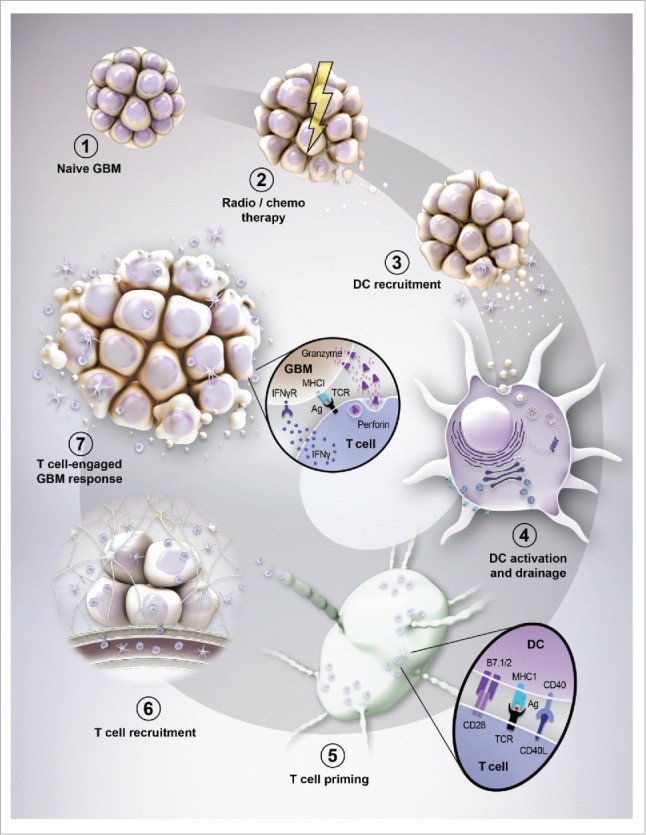
Evolution of brain tumor immunity. (1) The naive (newly diagnosed) brain tumor flourishes in the immunosuppressive environment of the central nervous system and is relatively non-immunogenic. (2) Standard of care for patients with brain tumors causes cancer cell death and the subsequent release of antigens. (3) The inflammation caused by cancer cell death triggers the recruitment of dendritic cells to the brain tumor microenvironment. (4) CD8α dendritic cells (DC) engulf the cancer-associated antigens and utilize the cross-presentation pathway to facilitate the loading of those epitopes onto major histocompatibility complex (MHC) I molecules. The CD8α-loaded DC subsequently emigrate out of the tumor microenvironment while simultaneously increasing costimulatory molecules that facilitate the future productive interaction(s) of naive CD8+ (and CD4+ T cells through MHCII) T cells. (5) After immigration into the lymph node, DC-mediated T cell priming and expansion occurs through MHC/antigen (Ag) expressed by DC and a high affinity T-cell receptor (TCR) expressed by T cells. (6) T cells that are now activated and specific to tumor-associated antigens then emigrate from the lymphoid tissue, back into the circulation. (7) To successfully penetrate the brain tumor, T cells must first come into contact with selectins and integrins (not shown) that facilitate the attachment to inflamed endothelium. Upon successful adhesion, T cells extravasate through the endothelial basement membrane, followed by the perivascular space and eventually through the parenchymal basement membrane whereby they can now come into direct contact with the CNS-resident tumor cells. (8) Productive T cell-mediated GBM rejection occurs when lymphocytes are reactivated by (re-)stimulation of T cell-expressed TCR with MHC/Ag expressed by brain tumor cells. This interaction facilitates the robust production and release of proinflammatory, interferon-gamma (IFNγ), in addition to the release of the pore forming complex, perforin, which facilitates the passive transfection of granzyme molecules (serine proteases) that cleave tumor-expressing procaspases into active molecules that trigger apoptosis.
Adoptive T cell therapy
An additional immunotherapeutic approach that negates the problems associated with suboptimal T cell activation in patients, is the ex vivo preparation of activated autologous T cells. Similarly, T cells can be engineered to express chimeric antigen receptors (CAR) specific to tumor antigens, while co-expressing genes that confer resistance to tumor-induced immune inhibitory signals.97 One such approach involves the fusion of intracellular γ or ζ subunits of the immunoglobulin or T-cell receptor (TCR) to the variable domain of the high-affinity monoclonal antibody, specific to the TAA.98 This strategy facilitates T cell activation through interaction of the chimeric TCR with the antigen on the surface of the tumor cell, overcoming the T cell's inability to recognize GBM cells with insufficient levels of MHC I/II for effective antigen presentation.99 Given the ability to rapidly generate CAR T cells in ∼2 weeks, preparation of adequate GBM-specific T cell levels can be achieved within reasonable time for therapeutic utilization.100 Currently, an ongoing clinical trial evaluating the safety and PFS in newly diagnosed GBM patients treated with CAR T cells engineered to target EGFRvIII has been announced but is not yet recruiting patients. (NCT02664363)
A novel strategy for generating high-affinity tumor-reactive T cells against autologous patient malignancy utilizes humanized mice. These mice gain their name by combining severely immunodeficient NOD-SCID-IL-2Rγnull (NSG) hosts, modified for constitutive expression of human stem cell factor (SCF), granulocyte-macrophage colony stimulating factor (GM-CSF) and interleukin-3 (IL-3) (SGM3) transgenes, with engrafted human fetal thymus and fetal liver-derived hematopoietic stem cells (BLT).101-103 These mice support the reconstitution of a human immune system 104 and can be used as hosts for patient tumor and immune system engraftment, followed by immune checkpoint blockade (anti-human CTLA-4, PD-(L)1 and/or IDO1 inhibition) to activate and expand a tumor-specific T cell response. Although current studies are aimed at optimizing mouse models for human cancers, in principle, memory lymphocytes could be isolated from the systemic immune cell repertoire of these mice, expanded in vitro, and adoptively transferred back into the patient for therapeutic benefit. Although it is possible that select T cells may also respond to mouse antigens, the predicted multiclonality of the T cell response to human antigens presented by human MHC is expected to supersede those T cells not directed toward relevant targets. Also, it is expected that mouse antigens will not be expressed in human patients, further diminishing this concern. However, these considerations will be necessary to address, should a humanized mouse bearing autologous immune system and tumor be utilized in this regard. This highly novel approach would also be considered an adaptation to, ‘personalized medicine’.
Conclusion
Early vaccine-based clinical trials have demonstrated promising results, though questions and concerns remain with respect to the durability of therapeutic efficacy and ultimate benefit from such cancer treatments. Recent data reporting disappointing results from the Phase III study of RINTEGA highlights the necessity for cautious optimism of early phase clinical trials that are limited to single arm approaches with small numbers of enrolled patients. This design has several restrictions that include a possible placebo effect, as well as the evolving standard of care that may incrementally increase in efficacy over time.105
Conceptually, an attractive antigenic target for GBM treatment is the human cytomegalovirus (CMV), first reported to be expressed by GBM in 2002.48 Since that initial study, a growing body of literature implicating CMV as a factor present in GBM has grown substantially.49-51 Notably, a Phase I clinical assessment of CMV-specific adoptive T cell therapy demonstrated PFS during the study period (175, 462, 1010, and 1447 d) in 4/10 GBM patients.106 Additionally, a Phase I randomized trial in newly diagnosed GBM (n = 12) whereby the vaccine site was pre-conditioned with tetanus/diphtheria (Td) toxoid and then vaccinated with CMV pp65 RNA-pulsed DCs, showed a median PFS of 10.8 mo and a median OS of 18.5 mo; similar to patients treated with standard of care in this study.107
Similar to targeting EGFRvIII, independent groups have developed vaccines against mutant isocitrate dehydrogenase 1 (mIDH1).108,109 This mutation occurs in 12% of total GBM patients, but is expressed prolifically in low-grade glioma (II and III). Interestingly, the presence of mIDH1 expression is associated with a favorable prognosis of GBM patients with a median OS of 3.8 y when compared to 1.1 y for GBM patients presenting with wild-type IDH1 (p < 0.001).110 Given that mIDH1 expression is associated with extended survival in GBM patients, the rationale for targeting this mutation and potentially selecting for a more aggressive GBM phenotype should be thoroughly considered.
In addition to targeting mutant peptide sequences, it is important to consider that cancer cells possess altered cellular surfaces with distinct carbohydrate modifications of cell membrane components.111-113 One glycosylation pattern, O-linked N-acetylgalactosamine (Tn antigen), has been shown to be selectively expressed in GBM,114 breast cancer,115 metastatic melanoma,116 as well as stomach, colon and pancreatic cancer.117 Brooks et al. demonstrated that targeting this carbohydrate moiety can result in striking tumor specificity.118 Further study of unique GBM posttranslational modifications that occur on the surface of the tumor cells may well reveal additional targets with vaccination potential.
There are some aspects of vaccine therapy which are unique to pediatric HGG. While adult GBM most often develops in the cerebral hemispheres, lending to neurosurgeons' ability to remove a significant amount of tumor en bloc for vaccine development, pediatric malignant glioma is often unresectable and only small amounts of tumor are possible to obtain during biopsy. The currently open HSPPC-96 vaccine trial will help to clarify the minimum of amount of tumor necessary for suitable vaccine development. Efforts directed against known TAAs that are available ‘off-the-shelf’ are attractive for pediatric patients. However, identification of appropriate antigens is still a challenge given the molecularly heterogeneity of histologically similar pediatric HGG and the relatively low mutational rate, when compared to adult GBM.
As vaccination therapies for patients with malignant glioma continue to be tested and refined, discussion(s) of how best to integrate standard-of-care therapy and other novel approaches will likely dominate in the future. The efficacy of combinatorial multi-modal treatments that include vaccine-induced immune responses will be influenced, in-part, by the timing of each administered modality. For instance, concurrent cytotoxic and vaccine regimens may substantially boost overall immune-mediated efficacy and OS, but at the cost of inducing significant and long-lasting adverse side effects in patients. Thus, one of the most significant hurdles going forward is how best to minimize immunotherapeutic-induced toxicity, without disabling therapeutic efficacy and immunological responsiveness. Toward this goal, increasing the study of humanized immunocompetent mice bearing HLA-matched intracranial adult and pediatric malignant glioma may prove especially informative.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Funding
C.D. James is supported by PHS grant numbers P50CA097257, R01CA159467, awarded by the NIH/NCI, as well as R01NS080619, awarded by the NIH/NINDS and D.A. Wainwright is supported by PHS grant number R00NS082381, awarded by the NIH/NINDS, US. Department of Health and Human Services; a Robert H. Lurie Comprehensive Cancer Center – Zell Scholar Program of the Zell Family Foundation Gift; and the Northwestern Brain Tumor Institute.
References
- 1.Ostrom QT, Gittleman H, Liao P, Rouse C, Chen Y, Dowling J, Wolinsky Y, Kruchko C, Barnholtz-Sloan J. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro Oncol 2014; 16 Suppl 4:iv1-63; PMID:25304271; http://dx.doi.org/ 10.1093/neuonc/nou223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 2013; 49(6):1374-403; PMID:23485231; http://dx.doi.org/ 10.1016/j.ejca.2012.12.027 [DOI] [PubMed] [Google Scholar]
- 3.Soerjomataram I, Lortet-Tieulent J, Parkin DM, Ferlay J, Mathers C, Forman D, Bray F. Global burden of cancer in 2008: a systematic analysis of disability-adjusted life-years in 12 world regions. Lancet 2012; 380(9856):1840-50; PMID:23079588; http://dx.doi.org/ 10.1016/S0140-6736(12)60919-2 [DOI] [PubMed] [Google Scholar]
- 4.2015 CBTRUS Fact Sheet 2015. [cited 2015December7]; Available from: http://www.cbtrus.org/factsheet/factsheet.html [Google Scholar]
- 5.Ostrom QT, Gittleman H, Stetson L, Virk SM, Barnholtz-Sloan JS. Epidemiology of gliomas. Cancer Treat Res 2015; 163:1-14; PMID:25468222; http://dx.doi.org/ 10.1007/978-3-319-12048-5_1 [DOI] [PubMed] [Google Scholar]
- 6.Wen PY, Kesari S. Malignant gliomas in adults. N Engl J Med 2008; 359(5):492-507; PMID:18669428; http://dx.doi.org/ 10.1056/NEJMra0708126 [DOI] [PubMed] [Google Scholar]
- 7.Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, Ludwin SK, Allgeier A, Fisher B, Belanger K et al.. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 2009; 10(5):459-66; PMID:19269895; http://dx.doi.org/ 10.1016/S1470-2045(09)70025-7 [DOI] [PubMed] [Google Scholar]
- 8.Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U et al.. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 2005; 352(10):987-96; PMID:15758009; http://dx.doi.org/ 10.1056/NEJMoa043330 [DOI] [PubMed] [Google Scholar]
- 9.Johnson DR, O'Neill BP. Glioblastoma survival in the United States before and during the temozolomide era. J Neurooncol 2012; 107(2):359-64; PMID:22045118; http://dx.doi.org/ 10.1007/s11060-011-0749-4 [DOI] [PubMed] [Google Scholar]
- 10.Eagan RT, Creagan ET, Bisel HF, Layton DD Jr, Groover RV, Herman RC Jr. Phase II studies of dianhydrogalactitol-based combination chemotherapy for recurrent brain tumors. Oncology 1981; 38(1):4-6; PMID:7443176; http://dx.doi.org/ 10.1159/000225511 [DOI] [PubMed] [Google Scholar]
- 11.Eagan RT, Dinapoli RP, Hermann RC Jr, Groover RV, Layton DD Jr, Scott M. Combination carmustine (BCNU) and dianhydrogalactitol in the treatment of primary brain tumors recurring after irradiation. Cancer Treat Rep 1982; 66(8):1647-9; PMID:7105055 [PubMed] [Google Scholar]
- 12.Eagan RT, Scott M. Evaluation of prognostic factors in chemotherapy of recurrent brain tumors. J Clin Oncol 1983; 1(1):38-44; PMID:6321671 [DOI] [PubMed] [Google Scholar]
- 13.Haid M, Khandekar JD, Christ M, Johnson CM, Miller SJ, Locker GY, Merrill JM, Reisel H, Hatfield A, Lanzotti V et al.. Aziridinylbenzoquinone in recurrent, progressive glioma of the central nervous system. A Phase II study by the Illinois Cancer Council. Cancer 1985; 56(6):1311-5; PMID:4027870; http://dx.doi.org/21135147 10.1002/1097-0142(19850915)56:6%3c1311::AID-CNCR2820560615%3e3.0.CO;2-V [DOI] [PubMed] [Google Scholar]
- 14.Prins RM, Soto H, Konkankit V, Odesa SK, Eskin A, Yong WH, Nelson SF, Liau LM. Gene expression profile correlates with T-cell infiltration and relative survival in glioblastoma patients vaccinated with dendritic cell immunotherapy. Clin Cancer Res 2011; 17(6):1603-15; PMID:21135147; http://dx.doi.org/ 10.1158/1078-0432.CCR-10-2563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lulla RR, Saratsis AM, Hashizume R. Mutations in chromatin machinery and pediatric high-grade glioma. Sci Adv 2016; 2(3):e1501354; PMID:27034984; http://dx.doi.org/ 10.1126/sciadv.1501354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodrigues JC, Gonzalez GC, Zhang L, Ibrahim G, Kelly JJ, Gustafson MP, Lin Y, Dietz AB, Forsyth PA, Yong VW et al.. Normal human monocytes exposed to glioma cells acquire myeloid-derived suppressor cell-like properties. Neuro Oncol 2010; 12(4):351-65; PMID:20308313; http://dx.doi.org/ 10.1093/neuonc/nop023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raychaudhuri B, Rayman P, Ireland J, Ko J, Rini B, Borden EC, Garcia J, Vogelbaum MA, Finke J. Myeloid-derived suppressor cell accumulation and function in patients with newly diagnosed glioblastoma. Neuro Oncol 2011; 13(6):591-9; PMID:21636707; http://dx.doi.org/ 10.1093/neuonc/nor042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El Andaloussi A, Han Y, Lesniak MS. Prolongation of survival following depletion of CD4+CD25+ regulatory T cells in mice with experimental brain tumors. J Neurosurg 2006; 105(3):430-7; PMID:16961139; http://dx.doi.org/ 10.3171/jns.2006.105.3.430 [DOI] [PubMed] [Google Scholar]
- 19.El Andaloussi A, Lesniak MS. An increase in CD4+CD25+FOXP3+ regulatory T cells in tumor-infiltrating lymphocytes of human glioblastoma multiforme. Neuro Oncol 2006; 8(3):234-43; PMID:16723631; http://dx.doi.org/ 10.1215/15228517-2006-006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wainwright DA, Nigam P, Thaci B, Dey M, Lesniak MS. Recent developments on immunotherapy for brain cancer. Expert Opin Emerg Drugs 2012; 17(2):181-202; PMID:22533851; http://dx.doi.org/ 10.1517/14728214.2012.679929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uyttenhove C, Pilotte L, Théate I, Stroobant V, Colau D, Parmentier N, Boon T, Van den Eynde BJ. Evidence for a tumoral immune resistance mechanism based on tryptophan degradation by indoleamine 2,3-dioxygenase. Nat Med 2003; 9(10):1269-74; PMID:14502282; http://dx.doi.org/ 10.1038/nm934 [DOI] [PubMed] [Google Scholar]
- 22.Zhang X, Wu A, Fan Y, Wang Y. Increased transforming growth factor-beta2 in epidermal growth factor receptor variant III-positive glioblastoma. J Clin Neurosci 2011; 18(6):821-6; PMID:21511480; http://dx.doi.org/ 10.1016/j.jocn.2010.09.024 [DOI] [PubMed] [Google Scholar]
- 23.Huettner C, Paulus W, Roggendorf W. Messenger RNA expression of the immunosuppressive cytokine IL-10 in human gliomas. Am J Pathol 1995; 146(2):317-22; PMID:7856743 [PMC free article] [PubMed] [Google Scholar]
- 24.Nitta T, Hishii M, Sato K, Okumura K. Selective expression of interleukin-10 gene within glioblastoma multiforme. Brain Res 1994; 649(1–2):122-8; PMID:7953624; http://dx.doi.org/ 10.1016/0006-8993(94)91055-3 [DOI] [PubMed] [Google Scholar]
- 25.Bloch O, Crane CA, Kaur R, Safaee M, Rutkowski MJ, Parsa AT. Gliomas promote immunosuppression through induction of B7-H1 expression in tumor-associated macrophages. Clin Cancer Res 2013; 19(12):3165-75; PMID:23613317; http://dx.doi.org/ 10.1158/1078-0432.CCR-12-3314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parsa AT, Waldron JS, Panner A, Crane CA, Parney IF, Barry JJ, Cachola KE, Murray JC, Tihan T, Jensen MC et al.. Loss of tumor suppressor PTEN function increases B7-H1 expression and immunoresistance in glioma. Nat Med 2007; 13(1):84-8; PMID:17159987; http://dx.doi.org/ 10.1038/nm1517 [DOI] [PubMed] [Google Scholar]
- 27.Thompson CB, Allison JP. The emerging role of CTLA-4 as an immune attenuator. Immunity 1997; 7(4):445-50; PMID:9354465; http://dx.doi.org/ 10.1016/S1074-7613(00)80366-0 [DOI] [PubMed] [Google Scholar]
- 28.Fecci PE, Ochiai H, Mitchell DA, Grossi PM, Sweeney AE, Archer GE, Cummings T, Allison JP, Bigner DD, Sampson JH. Systemic CTLA-4 blockade ameliorates glioma-induced changes to the CD4+ T cell compartment without affecting regulatory T-cell function. Clin Cancer Res 2007; 13(7):2158-67; PMID:17404100; http://dx.doi.org/ 10.1158/1078-0432.CCR-06-2070 [DOI] [PubMed] [Google Scholar]
- 29.Wainwright DA, Chang AL, Dey M, Balyasnikova IV, Kim CK, Tobias A, Cheng Y, Kim JW, Qiao J, Zhang L et al.. Durable therapeutic efficacy utilizing combinatorial blockade against IDO, CTLA-4 and PD-L1 in mice with brain tumors. Clin Cancer Res 2014; 20(20):5290-301; PMID:24691018; http://dx.doi.org/ 10.1158/1078-0432.CCR-14-0514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ogden AT, Horgan D, Waziri A, Anderson D, Louca J, McKhann GM, Sisti MB, Parsa AT, Bruce JN. Defective receptor expression and dendritic cell differentiation of monocytes in glioblastomas. Neurosurg 2006; 59(4):902-9; discussion 909-10; PMID:17038955; http://dx.doi.org/19387557 10.1227/01.NEU.0000233907.03070.7B [DOI] [PubMed] [Google Scholar]
- 31.Binder DC, Davis AA, Wainwright DA. Immunotherapy for cancer in the central nervous system: current and future directions. Onco Immunol 2015; 5(2):e1082027; PMID:27057463; http://dx.doi.org/19387557 10.1080/2162402X.2015.1082027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bullain SS, Sahin A, Szentirmai O, Sanchez C, Lin N, Baratta E, Waterman P, Weissleder R, Mulligan RC, Carter BS. Genetically engineered T cells to target EGFRvIII expressing glioblastoma. J Neurooncol 2009; 94(3):373-82; PMID:19387557; http://dx.doi.org/ 10.1007/s11060-009-9889-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu G, Ying H, Zeng G, Wheeler CJ, Black KL, Yu JS. HER-2, gp100, and MAGE-1 are expressed in human glioblastoma and recognized by cytotoxic T cells. Cancer Res 2004; 64(14):4980-6; PMID:15256472; http://dx.doi.org/ 10.1158/0008-5472.CAN-03-3504 [DOI] [PubMed] [Google Scholar]
- 34.Sahin U, Koslowski M, Türeci O, Eberle T, Zwick C, Romeike B, Moringlane JR, Schwechheimer K, Feiden W, Pfreundschuh M. Expression of cancer testis genes in human brain tumors. Clin Cancer Res 2000; 6(10):3916-22; PMID:11051238 [PubMed] [Google Scholar]
- 35.Scarcella DL, Chow CW, Gonzales MF, Economou C, Brasseur F, Ashley DM. Expression of MAGE and GAGE in high-grade brain tumors: a potential target for specific immunotherapy and diagnostic markers. Clin Cancer Res 1999; 5(2):335-41; PMID:10037183 [PubMed] [Google Scholar]
- 36.Kahlon KS, Brown C, Cooper LJ, Raubitschek A, Forman SJ, Jensen MC. Specific recognition and killing of glioblastoma multiforme by interleukin 13-zetakine redirected cytolytic T cells. Cancer Res 2004; 64(24):9160-6; PMID:15604287; http://dx.doi.org/ 10.1158/0008-5472.CAN-04-0454 [DOI] [PubMed] [Google Scholar]
- 37.Zhang JG, Eguchi J, Kruse CA, Gomez GG, Fakhrai H, Schroter S, Ma W, Hoa N, Minev B, Delgado C et al.. Antigenic profiling of glioma cells to generate allogeneic vaccines or dendritic cell-based therapeutics. Clin Cancer Res 2007; 13(2 Pt 1):566-75; PMID:17255279; http://dx.doi.org/ 10.1158/1078-0432.CCR-06-1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahmed N, Salsman VS, Kew Y, Shaffer D, Powell S, Zhang YJ, Grossman RG, Heslop HE, Gottschalk S. HER2-specific T cells target primary glioblastoma stem cells and induce regression of autologous experimental tumors. Clin Cancer Res 2010; 16(2):474-85; PMID:20068073; http://dx.doi.org/ 10.1158/1078-0432.CCR-09-1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu G, Yu JS, Zeng G, Yin D, Xie D, Black KL, Ying H. AIM-2: a novel tumor antigen is expressed and presented by human glioma cells. J Immunother 2004; 27(3):220-6; PMID:15076139; http://dx.doi.org/ 10.1097/00002371-200405000-00006 [DOI] [PubMed] [Google Scholar]
- 40.Ueda R, Yoshida K, Kawase T, Kawakami Y, Toda M. Preferential expression and frequent IgG responses of a tumor antigen, SOX5, in glioma patients. Int J Cancer 2007; 120(8):1704-11; PMID:17230535; http://dx.doi.org/ 10.1002/ijc.22472 [DOI] [PubMed] [Google Scholar]
- 41.Ueda R, Yoshida K, Kawakami Y, Kawase T, Toda M. Expression of a transcriptional factor, SOX6, in human gliomas. Brain Tumor Pathol 2004; 21(1):35-8; PMID:15696967; http://dx.doi.org/ 10.1007/BF02482175 [DOI] [PubMed] [Google Scholar]
- 42.Jin M, Komohara Y, Shichijo S, Harada M, Yamanaka R, Miyamoto S, Nikawa J, Itoh K, Yamada A. Identification of EphB6 variant-derived epitope peptides recognized by cytotoxic T-lymphocytes from HLA-A24+ malignant glioma patients. Oncol Rep 2008; 19(5):1277-83; PMID:18425388; http://dx.doi.org/ 10.3892/or.19.5.1277 [DOI] [PubMed] [Google Scholar]
- 43.Harada M, Ishihara Y, Itoh K, Yamanaka R. Kinesin superfamily protein-derived peptides with the ability to induce glioma-reactive cytotoxic T lymphocytes in human leukocyte antigen-A24+ glioma patients. Oncol Rep 2007; 17(3):629-36; PMID:17273744; http://dx.doi.org/ 10.3892/or.17.3.629 [DOI] [PubMed] [Google Scholar]
- 44.Friese MA, Platten M, Lutz SZ, Naumann U, Aulwurm S, Bischof F, Bühring HJ, Dichgans J, Rammensee HG, Steinle A et al.. MICA/NKG2D-mediated immunogene therapy of experimental gliomas. Cancer Res 2003; 63(24):8996-9006; PMID:14695218 [PubMed] [Google Scholar]
- 45.Wu A, Wiesner S, Xiao J, Ericson K, Chen W, Hall WA, Low WC, Ohlfest JR. Expression of MHC I and NK ligands on human CD133+ glioma cells: possible targets of immunotherapy. J Neurooncol 2007; 83(2):121-31; PMID:17077937; http://dx.doi.org/ 10.1007/s11060-006-9265-3 [DOI] [PubMed] [Google Scholar]
- 46.Castriconi R, Daga A, Dondero A, Zona G, Poliani PL, Melotti A, Griffero F, Marubbi D, Spaziante R, Bellora F et al.. NK cells recognize and kill human glioblastoma cells with stem cell-like properties. J Immunol 2009; 182(6):3530-9; PMID:19265131; http://dx.doi.org/ 10.4049/jimmunol.0802845 [DOI] [PubMed] [Google Scholar]
- 47.Hatano M, Eguchi J, Tatsumi T, Kuwashima N, Dusak JE, Kinch MS, Pollack IF, Hamilton RL, Storkus WJ, Okada H. EphA2 as a glioma-associated antigen: a novel target for glioma vaccines. Neoplasia 2005; 7(8):717-22; PMID:16207473; http://dx.doi.org/ 10.1593/neo.05277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cobbs CS, Harkins L, Samanta M, Gillespie GY, Bharara S, King PH, Nabors LB, Cobbs CG, Britt WJ. Human cytomegalovirus infection and expression in human malignant glioma. Cancer Res 2002; 62(12):3347-50; PMID:12067971 [PubMed] [Google Scholar]
- 49.Scheurer ME, Bondy ML, Aldape KD, Albrecht T, El-Zein R. Detection of human cytomegalovirus in different histological types of gliomas. Acta Neuropathol 2008; 116(1):79-86; PMID:18351367; http://dx.doi.org/ 10.1007/s00401-008-0359-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mitchell DA, Xie W, Schmittling R, Learn C, Friedman A, McLendon RE, Sampson JH. Sensitive detection of human cytomegalovirus in tumors and peripheral blood of patients diagnosed with glioblastoma. Neuro Oncol 2008; 10(1):10-8; PMID:17951512; http://dx.doi.org/ 10.1215/15228517-2007-035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lucas KG, Bao L, Bruggeman R, Dunham K, Specht C. The detection of CMV pp65 and IE1 in glioblastoma multiforme. J Neurooncol 2011; 103(2):231-8; PMID:20820869; http://dx.doi.org/ 10.1007/s11060-010-0383-6 [DOI] [PubMed] [Google Scholar]
- 52.Voldborg BR, Damstrup L, Spang-Thomsen M, Poulsen HS. Epidermal growth factor receptor (EGFR) and EGFR mutations, function and possible role in clinical trials. Ann Oncol 1997; 8(12):1197-206; PMID:9496384; http://dx.doi.org/ 10.1023/A:1008209720526 [DOI] [PubMed] [Google Scholar]
- 53.Brennan CW, Verhaak RG, McKenna A, Campos B, Noushmehr H, Salama SR, Zheng S, Chakravarty D, Sanborn JZ, Berman SH et al.. The somatic genomic landscape of glioblastoma. Cell 2013; 155(2):462-77; PMID:24120142; http://dx.doi.org/ 10.1016/j.cell.2013.09.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huang HS, Nagane M, Klingbeil CK, Lin H, Nishikawa R, Ji XD, Huang CM, Gill GN, Wiley HS, Cavenee WK. The enhanced tumorigenic activity of a mutant epidermal growth factor receptor common in human cancers is mediated by threshold levels of constitutive tyrosine phosphorylation and unattenuated signaling. J Biol Chem 1997; 272(5):2927-35; PMID:9006938; http://dx.doi.org/ 10.1074/jbc.272.5.2927 [DOI] [PubMed] [Google Scholar]
- 55.Heimberger AB, Crotty LE, Archer GE, Hess KR, Wikstrand CJ, Friedman AH, Friedman HS, Bigner DD, Sampson JH. Epidermal growth factor receptor VIII peptide vaccination is efficacious against established intracerebral tumors. Clin Cancer Res 2003; 9(11):4247-54; PMID:14519652 [PubMed] [Google Scholar]
- 56.Pelloski CE, Ballman KV, Furth AF, Zhang L, Lin E, Sulman EP, Bhat K, McDonald JM, Yung WK, Colman H et al.. Epidermal growth factor receptor variant III status defines clinically distinct subtypes of glioblastoma. J Clin Oncol 2007; 25(16):2288-94; PMID:17538175; http://dx.doi.org/ 10.1200/JCO.2006.08.0705 [DOI] [PubMed] [Google Scholar]
- 57.Shinojima N, Tada K, Shiraishi S, Kamiryo T, Kochi M, Nakamura H, Makino K, Saya H, Hirano H, Kuratsu J et al.. Prognostic value of epidermal growth factor receptor in patients with glioblastoma multiforme. Cancer Res 2003; 63(20):6962-70; PMID:14583498 [PubMed] [Google Scholar]
- 58.Heimberger AB, Hlatky R, Suki D, Yang D, Weinberg J, Gilbert M, Sawaya R, Aldape K. Prognostic effect of epidermal growth factor receptor and EGFRvIII in glioblastoma multiforme patients. Clin Cancer Res 2005; 11(4):1462-6; PMID:15746047; http://dx.doi.org/ 10.1158/1078-0432.CCR-04-1737 [DOI] [PubMed] [Google Scholar]
- 59.Sampson JH, Heimberger AB, Archer GE, Aldape KD, Friedman AH, Friedman HS, Gilbert MR, Herndon JE 2nd, McLendon RE, Mitchell DA et al.. Immunologic escape after prolonged progression-free survival with epidermal growth factor receptor variant III peptide vaccination in patients with newly diagnosed glioblastoma. J Clin Oncol 2010; 28(31):4722-9; PMID:20921459; http://dx.doi.org/ 10.1200/JCO.2010.28.6963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Choi BD, Archer GE, Mitchell DA, Heimberger AB, McLendon RE, Bigner DD, Sampson JH. EGFRvIII-targeted vaccination therapy of malignant glioma. Brain Pathol 2009; 19(4):713-23; PMID:19744042; http://dx.doi.org/ 10.1111/j.1750-3639.2009.00318.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sampson JH, Aldape KD, Archer GE, Coan A, Desjardins A, Friedman AH, Friedman HS, Gilbert MR, Herndon JE, McLendon RE et al.. Greater chemotherapy-induced lymphopenia enhances tumor-specific immune responses that eliminate EGFRvIII-expressing tumor cells in patients with glioblastoma. Neuro Oncol 2011; 13(3):324-33; PMID:21149254; http://dx.doi.org/ 10.1093/neuonc/noq157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schuster J, Lai RK, Recht LD, Reardon DA, Paleologos NA, Groves MD, Mrugala MM, Jensen R, Baehring JM, Sloan A et al.. A phase II, multicenter trial of rindopepimut (CDX-110) in newly diagnosed glioblastoma: the ACT III study. Neuro Oncol 2015; 17(6):854-61; PMID:25586468; http://dx.doi.org/ 10.1093/neuonc/nou348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Celldex Glioblastoma Candidate Rintega Fails Phase III Trial 2016. March-07-2016. [cited 2016March-16-2016]; Available from: http://www.genengnews.com/gen-news-highlights/celldex-ends-phase-iii-trial-of-glioblastoma-candidate-rintega/81252448/ [Google Scholar]
- 64.Srivastava PK, DeLeo AB, Old LJ. Tumor rejection antigens of chemically induced sarcomas of inbred mice. Proc Natl Acad Sci U S A 1986; 83(10):3407-11; PMID:3458189; http://dx.doi.org/ 10.1073/pnas.83.10.3407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Udono H, Levey LJ, Srivastava PK. Cellular requirements for tumor-specific immunity elicited by heat shock proteins: tumor rejection antigen gp96 primes CD8+ T cells in vivo. Proc Natl Acad Sci U S A 1994; 91(8):3077-81; PMID:7909157; http://dx.doi.org/ 10.1073/pnas.91.8.3077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chandawarkar RY, Wagh MS, Srivastava PK. The dual nature of specific immunological activity of tumor-derived gp96 preparations. J Exp Med 1999; 189(9):1437-42; PMID:10224283; http://dx.doi.org/ 10.1084/jem.189.9.1437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Binder RJ, Srivastava PK. Essential role of CD91 in re-presentation of gp96-chaperoned peptides. Proc Natl Acad Sci U S A 2004; 101(16):6128-33; PMID:15073331; http://dx.doi.org/ 10.1073/pnas.0308180101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lindquist S, Craig EA. The heat-shock proteins. Annu Rev Genet 1988; 22:631-77; PMID:2853609; http://dx.doi.org/ 10.1146/annurev.ge.22.120188.003215 [DOI] [PubMed] [Google Scholar]
- 69.Bloch O, Parsa AT. Heat-shock protein peptide complex-96 vaccination for recurrent glioblastoma: a phase II, single-arm trial. Neuro Oncol 2014; 16(2):274-9; PMID:24335700; http://dx.doi.org/ 10.1093/neuonc/not203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fazeny-Dorner B, Wenzel C, Veitl M, Piribauer M, Rössler K, Dieckmann K, Ungersböck K, Marosi C. Survival and prognostic factors of patients with unresectable glioblastoma multiforme. Anticancer Drugs 2003; 14(4):305-12; PMID:12679735; http://dx.doi.org/ 10.1097/00001813-200304000-00008 [DOI] [PubMed] [Google Scholar]
- 71.Stewart LA. Chemotherapy in adult high-grade glioma: a systematic review and meta-analysis of individual patient data from 12 randomised trials. Lancet 2002; 359(9311):1011-8; PMID:11937180; http://dx.doi.org/ 10.1016/S0140-6736(02)08091-1 [DOI] [PubMed] [Google Scholar]
- 72.Agenus Agenus Reports Positive Follow-on Phase 2 Results for Brain Cancer Vaccine in Newly Diagnosed Patients. 2013. [cited 2015October29]; Available from: http://www.agenusbio.com/docs/press-releases/2013/positive-phase-2-brain-cancer-vaccine.php [Google Scholar]
- 73.Constant S, Sant'Angelo D, Pasqualini T, Taylor T, Levin D, Flavell R, Bottomly K. Peptide and protein antigens require distinct antigen-presenting cell subsets for the priming of CD4+ T cells. J Immunol 1995; 154(10):4915-23; PMID:7730604 [PubMed] [Google Scholar]
- 74.Levin D, Constant S, Pasqualini T, Flavell R, Bottomly K. Role of dendritic cells in the priming of CD4+ T lymphocytes to peptide antigen in vivo. J Immunol 1993; 151(12):6742-50; PMID:7903097 [PubMed] [Google Scholar]
- 75.Inaba K, Inaba M, Romani N, Aya H, Deguchi M, Ikehara S, Muramatsu S, Steinman RM. Generation of large numbers of dendritic cells from mouse bone marrow cultures supplemented with granulocyte/macrophage colony-stimulating factor. J Exp Med 1992; 176(6):1693-702; PMID:1460426; http://dx.doi.org/ 10.1084/jem.176.6.1693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Campbell JD, Piechaczek C, Winkels G, Schwamborn E, Micheli D, Hennemann S, Schmitz J. Isolation and generation of clinical-grade dendritic cells using the Clini MACS system. Methods Mol Med 2005; 109:55-70; PMID:15585913; http://dx.doi.org/ 10.1385/1-59259-862-5:055 [DOI] [PubMed] [Google Scholar]
- 77.Mu LJ, Gaudernack G, Saebøe-Larssen S, Hammerstad H, Tierens A, Kvalheim G. A protocol for generation of clinical grade mRNA-transfected monocyte-derived dendritic cells for cancer vaccines. Scand J Immunol 2003; 58(5):578-86; PMID:14629630; http://dx.doi.org/ 10.1046/j.1365-3083.2003.01333.x [DOI] [PubMed] [Google Scholar]
- 78.Sorg RV, Ozcan Z, Brefort T, Fischer J, Ackermann R, Müller M, Wernet P. Clinical-scale generation of dendritic cells in a closed system. J Immunother 2003; 26(4):374-83; PMID:12843800; http://dx.doi.org/ 10.1097/00002371-200307000-00010 [DOI] [PubMed] [Google Scholar]
- 79.Tuyaerts S, Noppe SM, Corthals J, Breckpot K, Heirman C, De Greef C, Van Riet I, Thielemans K. Generation of large numbers of dendritic cells in a closed system using Cell Factories. J Immunol Methods 2002; 264(1–2):135-51; PMID:12191517; http://dx.doi.org/ 10.1016/S0022-1759(02)00099-6 [DOI] [PubMed] [Google Scholar]
- 80.Aoki H, Mizuno M, Natsume A, Tsugawa T, Tsujimura K, Takahashi T, Yoshida J. Dendritic cells pulsed with tumor extract-cationic liposome complex increase the induction of cytotoxic T lymphocytes in mouse brain tumor. Cancer Immunol Immunother 2001; 50(9):463-8; PMID:11761440; http://dx.doi.org/ 10.1007/s002620100220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liau LM, Black KL, Prins RM, Sykes SN, DiPatre PL, Cloughesy TF, Becker DP, Bronstein JM. Treatment of intracranial gliomas with bone marrow-derived dendritic cells pulsed with tumor antigens. J Neurosurg 1999; 90(6):1115-24; PMID:10350260; http://dx.doi.org/ 10.3171/jns.1999.90.6.1115 [DOI] [PubMed] [Google Scholar]
- 82.Liau LM, Prins RM, Kiertscher SM, Odesa SK, Kremen TJ, Giovannone AJ, Lin JW, Chute DJ, Mischel PS, Cloughesy TF et al.. Dendritic cell vaccination in glioblastoma patients induces systemic and intracranial T-cell responses modulated by the local central nervous system tumor microenvironment. Clin Cancer Res 2005; 11(15):5515-25; PMID:16061868; http://dx.doi.org/ 10.1158/1078-0432.CCR-05-0464 [DOI] [PubMed] [Google Scholar]
- 83.Phuphanich S, Wheeler CJ, Rudnick JD, Mazer M, Wang H, Nuño MA, Richardson JE, Fan X, Ji J, Chu RM, Bender JG et al.. Phase I trial of a multi-epitope-pulsed dendritic cell vaccine for patients with newly diagnosed glioblastoma. Cancer Immunol Immunother 2013; 62(1):125-35; PMID:22847020; http://dx.doi.org/ 10.1007/s00262-012-1319-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Siegelin MD, Siegelin Y, Habel A, Rami A, Gaiser T. KAAD-cyclopamine augmented TRAIL-mediated apoptosis in malignant glioma cells by modulating the intrinsic and extrinsic apoptotic pathway. Neurobiol Dis 2009; 34(2):259-66; PMID:19385057; http://dx.doi.org/ 10.1016/j.nbd.2009.01.012 [DOI] [PubMed] [Google Scholar]
- 85.Fadul CE, Fisher JL, Hampton TH, Lallana EC, Li Z, Gui J, Szczepiorkowski ZM, Tosteson TD, Rhodes CH, Wishart HA et al.. Immune response in patients with newly diagnosed glioblastoma multiforme treated with intranodal autologous tumor lysate-dendritic cell vaccination after radiation chemotherapy. J Immunother 2011; 34(4):382-9; PMID:21499132; http://dx.doi.org/ 10.1097/CJI.0b013e318215e300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pollack IF, Jakacki RI, Butterfield LH, Hamilton RL, Panigrahy A, Potter DM, Connelly AK, Dibridge SA, Whiteside TL, Okada H. Antigen-specific immune responses and clinical outcome after vaccination with glioma-associated antigen peptides and polyinosinic-polycytidylic acid stabilized by lysine and carboxymethylcellulose in children with newly diagnosed malignant brainstem and nonbrainstem gliomas. J Clin Oncol 2014; 32(19):2050-8; PMID:24888813; http://dx.doi.org/ 10.1200/JCO.2013.54.0526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lasky JL 3rd, Panosyan EH, Plant A, Davidson T, Yong WH, Prins RM, Liau LM, Moore TB. Autologous tumor lysate-pulsed dendritic cell immunotherapy for pediatric patients with newly diagnosed or recurrent high-grade gliomas. Anticancer Res 2013; 33(5):2047-56; PMID:23645755 [PMC free article] [PubMed] [Google Scholar]
- 88.Ardon H, De Vleeschouwer S, Van Calenbergh F, Claes L, Kramm CM, Rutkowski S, Wolff JE, Van Gool SW. Adjuvant dendritic cell-based tumour vaccination for children with malignant brain tumours. Pediatr Blood Cancer 2010; 54(4):519-25; PMID:19852061; http://dx.doi.org/ 10.1002/pbc.22319 [DOI] [PubMed] [Google Scholar]
- 89.Azimi F, Scolyer RA, Rumcheva P, Moncrieff M, Murali R, McCarthy SW, Saw RP, Thompson JF. Tumor-infiltrating lymphocyte grade is an independent predictor of sentinel lymph node status and survival in patients with cutaneous melanoma. J Clin Oncol 2012; 30(21):2678-83; PMID:22711850; http://dx.doi.org/ 10.1200/JCO.2011.37.8539 [DOI] [PubMed] [Google Scholar]
- 90.Kreike B, van Kouwenhove M, Horlings H, Weigelt B, Peterse H, Bartelink H, van de Vijver MJ. Gene expression profiling and histopathological characterization of triple-negative/basal-like breast carcinomas. Breast Cancer Res 2007; 9(5):R65; PMID:17910759; http://dx.doi.org/ 10.1186/bcr1771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mahmoud SM, Paish EC, Powe DG, Macmillan RD, Grainge MJ, Lee AH, Ellis IO, Green AR. Tumor-infiltrating CD8+ lymphocytes predict clinical outcome in breast cancer. J Clin Oncol 2011; 29(15):1949-55; PMID:21483002; http://dx.doi.org/ 10.1200/JCO.2010.30.5037 [DOI] [PubMed] [Google Scholar]
- 92.Rusakiewicz S, Semeraro M, Sarabi M, Desbois M, Locher C, Mendez R, Vimond N, Concha A, Garrido F, Isambert N et al.. Immune infiltrates are prognostic factors in localized gastrointestinal stromal tumors. Cancer Res 2013; 73(12):3499-510; PMID:23592754; http://dx.doi.org/ 10.1158/0008-5472.CAN-13-0371 [DOI] [PubMed] [Google Scholar]
- 93.Herold-Mende C, Mossermann J, Jungk C, Ahmadi R, Capper D, von Deimling A, Unterberg A, Beckhove P. Spontaneous immune responses in gbm patients after complete tumor resection are associated with an improved survival. Neuro-Oncology 2014; 16(suppl 3):iii42; http://dx.doi.org/ 10.1093/neuonc/nou209.1 [DOI] [Google Scholar]
- 94.Kmiecik J, Poli A, Brons NH, Waha A, Eide GE, Enger PØ, Zimmer J, Chekenya M. Elevated CD3+ and CD8+ tumor-infiltrating immune cells correlate with prolonged survival in glioblastoma patients despite integrated immunosuppressive mechanisms in the tumor microenvironment and at the systemic level. J Neuroimmunol 2013; 264(1–2):71-83; PMID:24045166; http://dx.doi.org/ 10.1016/j.jneuroim.2013.08.013 [DOI] [PubMed] [Google Scholar]
- 95.Ohkuri T, Ghosh A, Kosaka A, Zhu J, Ikeura M, David M, Watkins SC, Sarkar SN, Okada H. STING contributes to antiglioma immunity via triggering type I IFN signals in the tumor microenvironment. Cancer Immunol Res 2014; 2(12):1199-208; PMID:25300859; http://dx.doi.org/ 10.1158/2326-6066.CIR-14-0099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Woo SR, Corrales L, Gajewski TF. The STING pathway and the T cell-inflamed tumor microenvironment. Trends Immunol 2015; 36(4):250-6; PMID:25758021; http://dx.doi.org/ 10.1016/j.it.2015.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Miao H, Choi BD, Suryadevara CM, Sanchez-Perez L, Yang S, De Leon G, Sayour EJ, McLendon R, Herndon JE, Healy P et al.. EGFRvIII-specific chimeric antigen receptor T cells migrate to and kill tumor deposits infiltrating the brain parenchyma in an invasive xenograft model of glioblastoma. PLoS One 2014; 9(4):e94281; PMID:24722266; http://dx.doi.org/ 10.1371/journal.pone.0094281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Eshhar Z, Waks T, Gross G, Schindler DG. Specific activation and targeting of cytotoxic lymphocytes through chimeric single chains consisting of antibody-binding domains and the gamma or zeta subunits of the immunoglobulin and T-cell receptors. Proc Natl Acad Sci U S A 1993; 90(2):720-4; PMID:8421711; http://dx.doi.org/ 10.1073/pnas.90.2.720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sadelain M, Riviere I, Brentjens R. Targeting tumours with genetically enhanced T lymphocytes. Nat Rev Cancer 2003; 3(1):35-45; PMID:12509765; http://dx.doi.org/ 10.1038/nrc971 [DOI] [PubMed] [Google Scholar]
- 100.Pule M, Finney H, Lawson A. Artificial T-cell receptors. Cytotherapy 2003; 5(3):211-26; PMID:12850789; http://dx.doi.org/ 10.1080/14653240310001488 [DOI] [PubMed] [Google Scholar]
- 101.Wege AK, Ernst W, Eckl J, Frankenberger B, Vollmann-Zwerenz A, Männel DN, Ortmann O, Kroemer A, Brockhoff G. Humanized tumor mice–a new model to study and manipulate the immune response in advanced cancer therapy. Int J Cancer 2011; 129(9):2194-206; PMID:21544806; http://dx.doi.org/ 10.1002/ijc.26159 [DOI] [PubMed] [Google Scholar]
- 102.Brehm MA, Wiles MV, Greiner DL, Shultz LD. Generation of improved humanized mouse models for human infectious diseases. J Immunol Methods 2014; 410:3-17; PMID:24607601; http://dx.doi.org/ 10.1016/j.jim.2014.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Aryee KE, Shultz LD, Brehm MA. Immunodeficient mouse model for human hematopoietic stem cell engraftment and immune system development. Methods Mol Biol 2014; 1185:267-78; PMID:25062635; http://dx.doi.org/ 10.1007/978-1-4939-1133-2_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Billerbeck E, Barry WT, Mu K, Dorner M, Rice CM, Ploss A. Development of human CD4+FoxP3+ regulatory T cells in human stem cell factor-, granulocyte-macrophage colony-stimulating factor-, and interleukin-3-expressing NOD-SCID IL2Rgamma(null) humanized mice. Blood 2011; 117(11):3076-86; PMID:21252091; http://dx.doi.org/ 10.1182/blood-2010-08-301507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Evans SR. Clinical trial structures. J Exp Stroke Transl Med 2010; 3(1):8-18; PMID:21423788; http://dx.doi.org/ 10.6030/1939-067X-3.1.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Schuessler A, Smith C, Beagley L, Boyle GM, Rehan S, Matthews K, Jones L, Crough T, Dasari V, Klein K et al.. Autologous T-cell therapy for cytomegalovirus as a consolidative treatment for recurrent glioblastoma. Cancer Res 2014; 74(13):3466-76; PMID:24795429; http://dx.doi.org/ 10.1158/0008-5472.CAN-14-0296 [DOI] [PubMed] [Google Scholar]
- 107.Mitchell DA, Batich KA, Gunn MD, Huang MN, Sanchez-Perez L, Nair SK, Congdon KL, Reap EA, Archer GE, Desjardins A et al.. Tetanus toxoid and CCL3 improve dendritic cell vaccines in mice and glioblastoma patients. Nature 2015; 519(7543):366-9; PMID:25762141; http://dx.doi.org/ 10.1038/nature14320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Schumacher T, Bunse L, Wick W, Platten M. Mutant IDH1: An immunotherapeutic target in tumors. Oncoimmunology 2014; 3(12):e974392; PMID:25964867; http://dx.doi.org/ 10.4161/2162402X.2014.974392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Schumacher T, Bunse L, Pusch S, Sahm F, Wiestler B, Quandt J, Menn O, Osswald M, Oezen I, Ott M et al.. A vaccine targeting mutant IDH1 induces antitumour immunity. Nature 2014; 512(7514):324-7; ; http://dx.doi.org/ 10.1038/nature13387 [DOI] [PubMed] [Google Scholar]
- 110.Parsons DW, Jones S, Zhang X, Lin JC, Leary RJ, Angenendt P, Mankoo P, Carter H, Siu IM, Gallia GL et al.. An integrated genomic analysis of human glioblastoma multiforme. Science 2008; 321(5897):1807-12; PMID:18772396; http://dx.doi.org/ 10.1126/science.1164382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Dennis JW, Laferté S, Waghorne C, Breitman ML, Kerbel RS. Beta 1–6 branching of Asn-linked oligosaccharides is directly associated with metastasis. Science 1987; 236(4801):582-5; PMID:2953071; http://dx.doi.org/ 10.1126/science.2953071 [DOI] [PubMed] [Google Scholar]
- 112.Sell S. Cancer-associated carbohydrates identified by monoclonal antibodies. Hum Pathol 1990; 21(10):1003-19; PMID:2210723; http://dx.doi.org/ 10.1016/0046-8177(90)90250-9 [DOI] [PubMed] [Google Scholar]
- 113.Kobata A, Amano J. Altered glycosylation of proteins produced by malignant cells, and application for the diagnosis and immunotherapy of tumours. Immunol Cell Biol 2005; 83(4):429-39; PMID:16033539; http://dx.doi.org/ 10.1111/j.1440-1711.2005.01351.x [DOI] [PubMed] [Google Scholar]
- 114.Lou YW, Wang PY, Yeh SC, Chuang PK, Li ST, Wu CY, Khoo KH, Hsiao M, Hsu TL, Wong CH. Stage-specific embryonic antigen-4 as a potential therapeutic target in glioblastoma multiforme and other cancers. Proc Natl Acad Sci U S A 2014; 111(7):2482-7; PMID:24550271; http://dx.doi.org/ 10.1073/pnas.1400283111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Freire T, Bay S, von Mensdorff-Pouilly S, Osinaga E. Molecular basis of incomplete O-glycan synthesis in MCF-7 breast cancer cells: putative role of MUC6 in Tn antigen expression. Cancer Res 2005; 65(17):7880-7; PMID:16140958; http://dx.doi.org/ 10.1158/0008-5472.CAN-04-3746 [DOI] [PubMed] [Google Scholar]
- 116.Kanitakis J, al-Rifai I, Faure M, Claudy A. Differential expression of the cancer associated antigens T (Thomsen-Friedenreich) and Tn to the skin in primary and metastatic carcinomas. J Clin Pathol 1998; 51(8):588-92; PMID:9828816; http://dx.doi.org/ 10.1136/jcp.51.8.588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ohshio G, Imamura T, Imamura M, Yamabe H, Sakahara H, Nakada H, Yamashina I. Distribution of Tn antigen recognized by an anti-Tn monoclonal antibody (MLS128) in normal and malignant tissues of the digestive tract. J Cancer Res Clin Oncol 1995; 121(4):247-52; PMID:7751324; http://dx.doi.org/ 10.1007/BF01366970 [DOI] [PubMed] [Google Scholar]
- 118.Brooks CL, Schietinger A, Borisova SN, Kufer P, Okon M, Hirama T, Mackenzie CR, Wang LX, Schreiber H, Evans SV. Antibody recognition of a unique tumor-specific glycopeptide antigen. Proc Natl Acad Sci U S A 2010; 107(22):10056-61; PMID:20479270; http://dx.doi.org/ 10.1073/pnas.0915176107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Inman S. Rintega (Rindopepimut) Misses Survival Endpoint in Phase 3 Glioblastoma Trial. Brain Cancer Cure 2016. March-10-2016. [cited 2016April-19-2016]; Available from: http://www.curetoday.com/articles/rintega-misses-survival-endpoint-in-phase-3-glioblastoma-trial [Google Scholar]
- 120.Crane CA, Han SJ, Ahn B, Oehlke J, Kivett V, Fedoroff A, Butowski N, Chang SM, Clarke J, Berger MS et al.. Individual patient-specific immunity against high-grade glioma after vaccination with autologous tumor derived peptides bound to the 96 KD chaperone protein. Clin Cancer Res 2013; 19(1):205-14; PMID:22872572; http://dx.doi.org/ 10.1158/1078-0432.CCR-11-3358 [DOI] [PubMed] [Google Scholar]
- 121.Gedeon PC, Choi BD, Sampson JH, Bigner DD. Rindopepimut: anti-EGFRvIII peptide vaccine, oncolytic. Drugs Future 2013; 38(3):147-155; PMID:25663738; http://dx.doi.org/ 10.1358/dof.2013.038.03.1933992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ahmed KA, Sawa T, Ihara H, Kasamatsu S, Yoshitake J, Rahaman MM, Okamoto T, Fujii S, Akaike T. Regulation by mitochondrial superoxide and NADPH oxidase of cellular formation of nitrated cyclic GMP: potential implications for ROS signalling. Biochem J 2012; 441(2):719-30; PMID:21967515; http://dx.doi.org/ 10.1042/BJ20111130 [DOI] [PubMed] [Google Scholar]


