ABSTRACT
Arenaviruses are responsible for severe and often fatal hemorrhagic disease. In the absence of effective antiviral therapies and vaccines, these viruses pose serious threats to public health and biodefense. Arenaviruses enter the host cell by fusion of the viral and endosomal membranes, a process mediated by the virus envelope glycoprotein GPC. Unlike other class I viral fusion proteins, GPC retains its stable signal peptide (SSP) as an essential third subunit in the mature complex. SSP spans the membrane twice and is myristoylated at its cytoplasmic N terminus. Mutations that abolish SSP myristoylation have been shown to reduce pH-induced cell-cell fusion activity of ectopically expressed GPC to ∼20% of wild-type levels. In order to examine the role of SSP myristoylation in the context of the intact virus, we used reverse genetics to generate Junín viruses (Candid #1 isolate) in which the critical glycine-2 residue in SSP was either replaced by alanine (G2A) or deleted (ΔG2). These mutant viruses produced smaller foci of infection in Vero cells and showed an ∼5-fold reduction in specific infectivity, commensurate with the defect in cell-cell fusion. However, virus assembly and GPC incorporation into budded virions were unaffected. Our findings suggest that the myristate moiety is cryptically disposed in the prefusion GPC complex and may function late in the fusion process to promote merging of the viral and cellular membranes.
IMPORTANCE Hemorrhagic fever arenaviruses pose significant threats to public health and biodefense. Arenavirus entry into the host cell is promoted by the virus envelope glycoprotein GPC. Unlike other viral envelope glycoproteins, GPC contains a myristoylated stable signal peptide (SSP) as an essential third subunit. Myristoylation has been shown to be important for the membrane fusion activity of recombinantly expressed GPC. Here, we use reverse genetics to study the role of SSP myristoylation in the context of the intact virion. We find that nonmyristoylated GPC mutants of the Candid #1 strain of Junín virus display a commensurate deficiency in their infectivity, albeit without additional defects in virion assembly and budding. These results suggest that SSP myristoylation may function late in the fusion process to facilitate merging of the viral and cellular membranes. Antiviral agents that target this novel aspect of GPC membrane fusion may be useful in the treatment of arenavirus hemorrhagic fevers.
INTRODUCTION
The mammarenaviruses comprise a diverse genus of enveloped negative-strand RNA viruses whose members have diversified in association with their respective murid hosts (1). Some arenavirus species can be transmitted to humans to cause severe life-threatening hemorrhagic fevers. Lassa virus (LASV) is endemic in western Africa and can be exported by infected travelers (2–4). Five New World species cause fatal disease in the Americas, including the Argentine hemorrhagic fever virus Junín (JUNV). Frequent reports of new pathogenic isolates suggest a wider diversity of arenavirus species (5, 6). In the face of this challenge, there are no arenavirus-specific therapeutics and no licensed vaccines to protect against infection. Therefore, the hemorrhagic fever arenaviruses are recognized to pose significant threats to public health and biodefense and are classified as category A priority pathogens (7). Intervention strategies that aim to block arenavirus entry into its target cells hold promise for preventing viral infection and disease (8–11).
Arenaviruses enter the host cell through pH-dependent fusion of the viral and endosomal membranes, a process mediated by the virus envelope glycoprotein GPC (12). As a class I viral fusion protein (13–16), GPC is synthesized as a glycoprotein precursor that assembles to form a trimer. Proteolytic cleavage by the cellular S1P/SKI-1 protease generates the mature receptor-binding and transmembrane fusion subunits, GP1 and GP2, respectively. In addition, GPC retains a unique stable signal peptide (SSP) as a third subunit in the mature complex (17, 18). SSP is required for GPC exit from the endoplasmic reticulum (ER) (19) and thus for proteolytic maturation in the Golgi compartment (20, 21) and transit to the cell surface for virion assembly and budding. The 58-amino-acid residue SSP contains two hydrophobic regions that span the membrane in an antiparallel manner to form a hairpin structure (22). The cytoplasmic N terminus of SSP is myristoylated at glycine-2 (18), and the C terminus forms an intersubunit zinc finger with the cytoplasmic domain of GP2 (23, 24). The central ectodomain loop of SSP interacts with GP2 to modulate the pH at which membrane fusion is activated in the maturing endosome (25).
Myristoylation is a common modification of N-terminal glycine residues, present in nearly 1% of the eukaryotic cell proteome and in a number of viral proteins (26, 27). In many myristoylated proteins, the myristate moiety can exist in two states, either sequestered within a hydrophobic pocket of the protein or exposed to interact with membrane. This so-called myristoyl switch is typically triggered by ligand binding and promotes a range of biologically significant changes in protein activity, protein-protein interactions, and membrane localization (26, 27). In ectopically expressed GPC, the G2A mutation that abolishes myristate addition to SSP has been shown to reduce cell-cell fusion activity to ∼20% of the wild-type level, without affecting GPC biosynthesis and trafficking (18, 28) or its accumulation into discrete detergent-soluble membrane microdomains on the cell surface (29). The molecular basis for this fusion deficiency is unclear, and it is unknown whether GPC is similarly impacted when incorporated into virions. Furthermore, it is possible that GPC myristoylation promotes interactions with other viral or cellular proteins throughout the viral life cycle. For example, GPC has been reported to interact with the arenavirus Z matrix protein (30), which is itself myristoylated (31, 32). This shared membrane-targeting mechanism may be important for virion assembly and budding. Therefore, we utilized a recently developed reverse genetics system (33) to investigate the role of GPC myristoylation in the morphogenesis and infectivity of the attenuated Candid #1 strain of JUNV.
MATERIALS AND METHODS
Molecular reagents, cells, and antibodies.
Reverse genetics plasmids and protocols for generating recombinant Candid #1 (rCan) viruses (33) were kindly provided by Juan Carlos de la Torre (Scripps Research Institute, La Jolla, CA) and Slobodan Paessler (University of Texas Medical Branch, Galveston, TX). Plasmids mPol-I-Sag (number 30) and mPol-I-Lag (number 35) express the entire S and L genomic RNAs, respectively, in an antigenomic orientation under the control of the mouse polymerase I (mPol I) promoter. Plasmids pC-L and pC-NP encode the multifunctional RNA-dependent RNA polymerase (L) and the nucleoprotein (NP), respectively. Recombinant viruses are generated upon cotransfection of these four plasmids into BHK-21 cells (ATCC). GPC from the pathogenic MC2 isolate of JUNV (34) was ectopically expressed in Vero-76 cells (ATCC) using the minimal bacteriophage T7 promoter in pcDNA3.1-based plasmids. T7 polymerase is provided by concurrent infection with the vTF7-3 vaccinia virus (35) as previously described (18, 36). In these studies, plasmids encoding SSP and the GP1/GP2 precursor (fused to the conventional signal peptide of human CD4) were cotransfected and expressed in trans to reconstitute the intact GPC (18, 37). All mutants were generated using QuikChange mutagenesis (Stratagene), and changes were confirmed by DNA sequence analysis using an ABI 3130 genetic analyzer (Applied Biosystems).
Monoclonal antibodies (MAbs) directed to JUNV GP1 (BF11) and NP (AG12 and AA10) (38) were obtained through the NIAID Biodefense and Emerging Infections Research Program (BEI Resources). The GP2-directed MAbs G3 and G5 (39) were kindly provided by the Public Health Agency of Canada (Winnipeg, MB, Canada).
Reverse genetics methodology.
Recombinant Candid #1 viruses were generated using published reverse genetics procedures (33). A laboratory protocol was kindly provided by Juan Carlos de la Torre (Scripps Research Institute, La Jolla, CA). In brief, BHK-21 cells were transfected with the two reverse genetics plasmids mPol-I-Sag (number 30) and mPol-I-Lag (number 35) and with pC-L and pC-NP to initiate replication of the transcribed genomic RNAs. After 3 days, the cell culture supernatant containing the rescued rCan virus was transferred to permissive Vero-76 cells, and the virus was expanded for an additional 3 days. At this point, a virus stock was prepared from freeze-thawed cells and culture supernatant. In some derivations, additional expansion of the virus was necessary to obtain a high-titer stock. All studies using recombinant Candid #1 viruses were approved by the University of Montana Institutional Biosafety Committee and performed using biosafety level 2+ (BSL2+) operations.
The original rCan stock was characterized in detail and used in serial passage studies to identify genetic changes that might compensate for the lack of myristoylation. At each passage, 1 ml of cell culture supernatant was transferred onto fresh Vero-76 cells in a 10-cm culture dish. This process was repeated every 3 to 4 days (twice per week) until such time as phenotypic changes were observed (G2A-GPC rCan) or through passage 30 (p30; ΔG2-GPC rCan).
Virus growth curves.
Vero-76 cells, grown in 6-cm culture dishes with Dulbecco's modified Eagle medium (DMEM) containing 10% fetal bovine serum (FBS), were infected with virus at a multiplicity of infection (MOI) of 0.01. The inoculated virus was removed after 1 h, and cultures were maintained in DMEM–2% FBS. Over the course of 72 h, individual dishes were harvested to measure viral growth. Cell culture supernatants were used to assess infectious virus production (focus-forming units) and NP content (NP enzyme-linked immunosorbent assay [ELISA]) as described below. Cell monolayers were fixed with methanol-acetone and immunochemically stained using MAb AG12, a horseradish peroxidase (HRP)-conjugated secondary antibody and diaminobenzidine substrate in order to qualitatively assess viral spread in the culture.
Viral titers and focal growth morphology were determined by incubating serial dilutions of the virus in duplicate with Vero cell monolayers prepared in six-well culture dishes with DMEM–2% FBS. Following a 1-h incubation, the medium was removed and replaced with a 1:1 mix of 2× minimal essential medium (MEM) without phenol red (Life Technologies) and 1% low-melting-point (LMP) agarose (Life Technologies). Cultures were continued for 4 to 5 days and subsequently fixed by the addition of Dulbecco's phosphate-buffered saline (DPBS) containing 4% paraformaldehyde (2% final). Upon removal of the agarose overlay, dishes were immunochemically stained using MAb AG12.
Virion NP content was quantitated by sandwich ELISA using MAb AG12 for capture and the noncompeting biotinylated MAb AA10 for detection (40). MAb AA10 was biotinylated using EZ-Link Sulfo-NHS-LC-biotin (sulfosuccinimidyl-6-biotinamido-hexanoate; Life Technologies) and detected with NeutrAvidin-HRP (Pierce) and Sure Blue reagent (KPL). Optical densities were measured at 450 nm using a V-Max microplate reader (Molecular Devices). The assay is linear with respect to NP concentration to optical densities of ≥3.0.
Immunoblot analysis.
Virions were partially purified from cleared cell culture supernatants by centrifugation through a cushion of 20% sucrose in DPBS. For immunoblot analysis, virion pellets were dissolved in NuPAGE lithium dodecyl sulfate (LDS) sample buffer with reducing agent (Life Technologies), and proteins were resolved by SDS-polyacrylamide gel electrophoresis (SDS-PAGE) using 4 to 12% NuPAGE gels (Life Technologies). Infected cell lysates were prepared by solubilizing the cell pellet in 50 mM Tris, pH 7.5, and 150 mM NaCl containing 1% Triton X-100 and protease inhibitors (36). Cleared lysates were then denatured and reduced in NuPAGE LDS sample buffer and subjected to NuPAGE analysis as described for purified virions. Following gel electrophoresis, proteins were transferred to Novex polyvinylidene difluoride (PVDF) membranes (Life Technologies) and probed using either MAbs G3 and G5 (GPC) or MAb AG12 (NP). Bands were visualized via a secondary HRP-conjugated anti-mouse IgG antibody and ECL 2 Western blotting substrate (Pierce). Chemifluorescence was quantitated using a Fuji FLA 3000G imager and ImageGauge software (Fuji).
Characterization of ectopically expressed GPC.
GPC was expressed through Lipofectamine 2000 (Life Technologies)-mediated transfection of Vero-76 cells using pcDNA3.1-based plasmids encoding SSP and the GP1/GP2 precursor, which was directed to the ER via the signal peptide of human CD4. Expression was driven by T7 polymerase provided by concurrent infection with vTF7-3 (35) as previously described (18, 36). Cells expressing GPC were metabolically labeled using [35S]methionine-cysteine (EasyTag Express; Perkin-Elmer), and radioimmunoprecipitation was performed using the GP1-directed MAb BF11 (36). Proteins were resolved by reducing SDS-PAGE using NuPAGE 4 to 12% Bis-Tris gels (Life Technologies). A vaccinia virus-based β-galactosidase fusion reporter assay was used as previously described (41, 42) to assess the cell-cell fusion activity of ectopically expressed GPC. In brief, Vero-76 cells expressing SSP and the GP1/GP2 precursor in trans under the control of the vTF7-3 vaccinia virus T7 polymerase were mixed with Vero cells infected with the vCB21R-lacZ vaccinia virus carrying the β-galactosidase gene under the control of a T7 promoter (43). The cells were treated with cytosine arabinoside (araC) and/or rifampin to block vaccinia virus production and cross-infection (41, 42). Cell-cell fusion was initiated by exposing the coculture to medium buffered either to pH 5.0 in the standard assay or to a range of pHs (4.5 to 7.0) to assess the pH profile for fusion activity (41, 42). Fusion-induced expression of the β-galactosidase reporter was assessed by chemiluminescence using Galactolite Plus substrate (Applied Biosystems) and a SpectraMax L microplate luminometer (Molecular Devices).
RNA extraction and RT-PCR.
Virion and infected cell RNAs were prepared using TRIzol reagent (Ambion). Oligonucleotide primers used in reverse transcription-PCR (RT-PCR) to confirm retention of the G2A and ΔG2 mutations are rCan 5UTR (5′-GGGGATCCTAGGCGATTTTGGTTACGC) and rCan GPC 2 (5′-CCTTCTGTCTTTGCACGGTTCC). These primers span amino acids 1 to 165 in GPC. Superscript III reverse transcriptase and Platinum Taq DNA polymerase (Life Technologies) were used to generate the respective cDNA and PCR products. Sanger sequencing of gel-purified PCR fragments was performed using an ABI 3130 genetic analyzer (Applied Biosystems).
Next-generation sequencing of virion RNAs.
Virion RNA was prepared from cell culture supernatants and provided to the Yale Center for Genome Analysis (Yale School of Medicine) for library construction and deep sequencing using an Illumina HiSeq 2000 instrument. In brief, RNA was depleted of rRNA molecules using a Ribo-Zero Gold kit (Epicentre) and then sheared by incubation at 94°C. Following first-strand synthesis with random primers, second-strand synthesis was performed with dUTP for generating a strand-specific sequencing library. The library was then end repaired and A tailed, and adapters were ligated prior to second-strand digestion using uracil-DNA glycosylase. Libraries were quantified by quantitative RT-PCR (qRT-PCR; Kapa Biosystems), and the insert size distribution was determined with LabChip GX. Samples were multiplexed (8×) and loaded onto Illumina version 3 flow cells at a concentration that yields 170 to 200 million passing filter clusters per lane. Samples were sequenced using a 75-bp paired-end strategy on an Illumina HiSeq 2000 according to Illumina protocols. Signal intensities were converted to individual base calls during the run using the system's real-time analysis (RTA) software.
The raw data were provided as fastq files to Sijung Yun (Yotta Biomed, LLC) for bioinformatics analysis. Read qualities were checked using FastQC software (44). The reads were aligned to the reference Candid #1 S and L RNA genomes (GenBank accession numbers AY746353.1 and AY746354.1, respectively) using the Burrows-Wheeler Aligner (BWA) (version 0.7.8-r455) with the BWA maximal exact match (BWA-MEM) algorithm (45). Variants were called using SAMtools mpileup and bcftools (46). The Broad Institute Integrated Genomics Viewer (IGV) (47) was used for further review and analysis of sequence variation. DNA sequences of the original reverse genetics plasmids mPol-I-Sag (number 30) and mPol-I-Lag (number 35) were kindly provided by Juan Carlos de la Torre (Scripps Research Institute, La Jolla, CA) to confirm preexisting variations from the reference sequences.
RESULTS
Recombinant G2A-GPC rCan recapitulates the phenotype of G2A GPC.
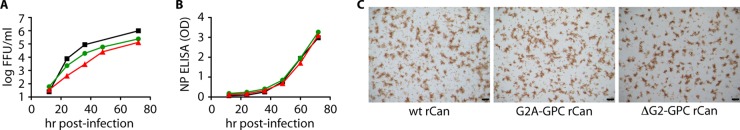
The attenuated Candid #1 strain of JUNV is used for vaccination in regions of endemicity in Argentina (48, 49) but is not licensed for use in the United States. Unlike its highly pathogenic parent, Candid #1 can be used in the laboratory under biosafety level 2 containment (50). To examine the role of SSP myristoylation in the intact Candid #1 virion, we used reverse genetics (33) to generate a recombinant virus (rCan) bearing the G2A mutation in GPC. A single nucleotide substitution converted the glycine-2 codon (GGG) to alanine (GCG). In this reverse genetics system, BHK-21 cells are transfected with plasmids containing the complete L and S RNA segments of the bipartite Candid #1 genome in an antigenomic orientation, under transcriptional control of the mouse RNA polymerase I (Pol I) promoter (33). Replication of the transcribed genomic RNAs is initiated through cotransfection with plasmids encoding the viral RNA-dependent RNA polymerase (L protein) and nucleoprotein (NP). The cell culture supernatant is then transferred onto permissive Vero cells for amplification of the rescued virus. Infectious virions were readily detected by immunochemical staining of Vero cells on the initial transfer, and a high-titer stock of G2A-GPC rCan was prepared through two additional expansions. RT-PCR sequencing confirmed retention of the G2A mutation in the rescued virus. Notably, the foci of infected cells produced in Vero cells after 5 days of growth under agarose were significantly smaller than those of the wild-type virus (Fig. 1).
FIG 1.
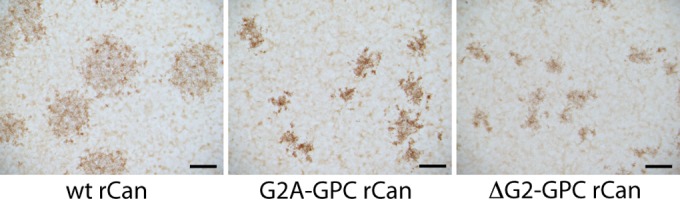
G2A-GPC and ΔG2-GPC rCan produce small foci in Vero cells. Photomicrographs of rCan foci after 4 days of growth under agarose. Infected cells were immunochemically stained using the anti-NP MAb AG12 (38). Scale bar, 600 μm. wt, wild type.
To investigate the apparent defect in focal spread, we compared the kinetics of virus production over 72 h in Vero cells infected at a low multiplicity of infection (MOI of 0.01). Indeed, accumulation of infectious G2A-GPC rCan in the cell culture supernatant was significantly reduced relative to that of wild-type rCan at all times over the course of infection (Fig. 2A). In contrast to the reduction in infectious particles, the kinetics and extent of NP accumulation in the cell culture supernatant were similar to those of wild-type rCan (Fig. 2B). Thus, virion particle production was largely unaffected by the lack of myristoylation. By using NP levels as a surrogate for the number of virion particles, we could compare the specific infectivities of the wild-type and mutant viruses (focus-forming units per optical density unit in NP ELISA). In two independent growth experiments, the specific infectivity of G2A-GPC rCan virus harvested at 72 h postinfection was ∼20% (22% and 17%) that of wild-type rCan, consistent with the deficit in cell-cell fusion activity by the ectopically expressed mutant (18, 28).
FIG 2.
Growth kinetics of G2A-GPC and ΔG2-GPC rCan in Vero cells. Separate 6-cm culture dishes were infected at a multiplicity of infection (MOI) of 0.01, and culture supernatants were harvested at the indicated times. Accumulations of infectious particles (A) and NP (B) were determined, respectively, by using a plaque assay and NP ELISA as described in Materials and Methods. The results presented are representative of two independent growth experiments. Black squares, wild-type rCan; green circles, G2A-GPC rCan; red triangles, ΔG2-GPC rCan. (C) Infected cell monolayers were immunochemically stained at the 36-h time point with MAb AG12 to illustrate the comparable extent of virus spread through the cultures, in agreement with results from the NP ELISA. At later time points, infection is too widespread to visually judge the proportion of infected cells. Scale bar, 200 μm. OD, optical density; FFU, focus-forming units.
In light of the smaller foci and diminished specific infectivity, the spread of G2A-GPC rCan infection throughout the culture might be expected to be less efficient than with wild-type rCan, thus producing smaller amounts of NP. However, not only were NP levels comparable (Fig. 2B), but immunochemical staining of the monolayers also revealed roughly similar proportions of infected cells over time (Fig. 2C). To reconcile these observations, we suggest that high multiplicities of infection at later time points can compensate for the reduced infectivity of individual viral particles to promote efficient spread. This mechanism may be less significant in focal spread.
Although the specific infectivity of G2A-GPC rCan is numerically consistent with the deficit in cell-cell fusion activity by the ectopically expressed protein, myristoylation may also be important for GPC incorporation into the budding virion. The fact that the Z matrix protein is also myristoylated (31, 32) raises the possibility that colocalization of Z and GPC at the site of virion assembly may be promoted by this shared modification. Therefore, we investigated the composition of purified G2A-GPC rCan virions. Immunoblot analysis using monoclonal antibodies directed to either GPC or NP (Fig. 3 and Table 1) revealed similar ratios of the two virion proteins in the wild-type and G2A-GPC rCan viruses, indicating that GPC incorporation into G2A-GPC rCan virions is not impaired by the lack of myristoylation. Furthermore, the wild-type and mutant GPCs were expressed and proteolytically processed with similar efficiencies in the infected cells, and only the mature GPC complex was incorporated into virions (Fig. 3 and Table 1). The extent of virion budding was likewise comparable, as judged by the relative amounts of the viral proteins in virion particles versus those in infected cells (Fig. 3 and Table 1). Taken together, our results indicate that the absence of SSP myristoylation does not impair virion assembly and budding. Thus, the reduction in specific infectivity in G2A-GPC rCan is likely wholly attributable to the defect in the intrinsic membrane fusion activity of the mutant GPC.
FIG 3.
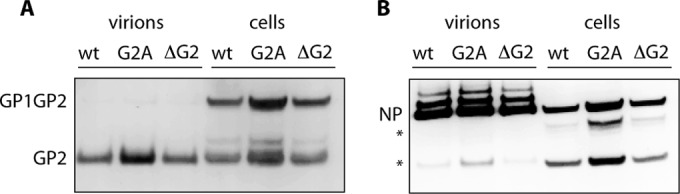
Immunoblot analysis of purified virions and infected cells. Vero cells were infected with wild-type, G2A-GPC, or ΔG2-GPC rCan virus (MOI of 0.1) for 48 h, and virions were purified from cell culture supernatants by centrifugation through 20% sucrose solution. Both the purified virions and infected cell monolayers were solubilized and subjected to SDS-PAGE and immunoblot analysis using GP2-directed MAbs G3 and G5 (39) (A) or NP-directed MAb AG12 (38) (B). The higher-molecular-size NP species may represent phosphorylated isoforms (73); the absence of these species in infected cell lysates could reflect errant phosphatase activity. The lower-molecular-size NP bands (*) are common degradation products. None of the identified species is present in lysates of uninfected cells. This experiment is representative of four independent virus growths, and average GPC and NP compositions are shown in Table 1.
TABLE 1.
GPC and NP in virions and infected cellsa
| Virus | GP2/GPC in cells | GP2/NP in virions | GPC/NP in cells | GPC in virions/GPC in cells |
|---|---|---|---|---|
| Wild-type rCan | 0.52 | 0.28 | 1.46 | 0.62 |
| G2A-GPC rCan | 0.49 | 0.36 | 1.33 | 0.57 |
| ΔG2-GPC rCan | 0.50 | 0.30 | 1.27 | 0.56 |
Immunoblots of GP2, GP1/GP2 precursor (GPC is the sum of GP1/GP2 and GP2), and all forms of NP were quantitated using ImageGauge software (Fuji). Ratios represent averages from four independent infections (including that represented in Fig. 3).
In keeping with its reduced fitness, serial passage of G2A-GPC rCan resulted in the emergence of wild-type revertants. This was evident in the appearance of larger, wild-type foci (data not shown). DNA sequence analysis documented a mixed population of G2A and revertant viruses in passages 5 to 7 and complete reversion to the wild-type glycine by p8 (Fig. 4). Facile reversion precluded further efforts to derive complementing second-site mutations that might provide additional insight into the role of myristoylation throughout the virus life cycle.
FIG 4.
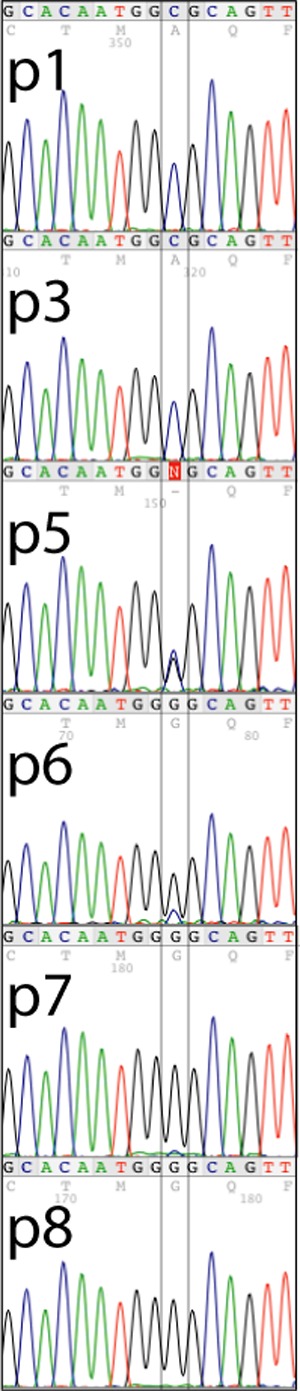
Reversion of G2A-GPC rCan detected by Sanger DNA sequencing. Viral RNA was prepared from cell culture supernatants of Vero cells throughout early serial passages of G2A-GPC rCan, and RT-PCR products of the GPC open reading frame were subjected to Sanger sequencing. Chromatograms flanking the G2A mutation (GCG) are shown, and the position of the C→G nucleotide change is boxed. Reversion to the wild-type glycine (GGG) is complete by passage 8 (p8).
The lack of myristoylation does not alter the pH required for cell-cell fusion activity by ectopically expressed GPC.
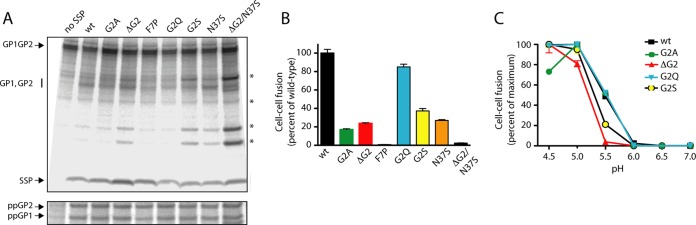
In order to identify myristoylation mutants with a reduced likelihood of reversion, we first characterized a series of additional SSP mutations in a plasmid-based GPC expression construct. Substitution of two nucleotides in the glycine-2 codon yielded G2S (TCG) and G2Q (CAG) GPC. We also deleted the entire G2 codon (ΔG2) to make reconstitution of the core myristoylation motif [GX3(S/T)] all but impossible. In addition, we generated an F7P (TTC→CCC) mutant, as proline residues are not tolerated immediately adjacent to the core myristoylation motif (51). Characterization of the GPC mutants revealed that all were expressed, assembled, and proteolytically processed similarly to wild-type GPC and the original G2A mutant (Fig. 5A) (18). Importantly, G2S and ΔG2 GPCs displayed a deficiency in cell-cell fusion comparable to that of the G2A mutant (Fig. 5B). G2Q GPC showed more robust activity, suggesting that the larger uncharged glutamine side chain may in some manner compensate for the lack of the myristate moiety. In contrast, the F7P mutation abolished cell-cell fusion activity (Fig. 5B), likely due to the nonconservative nature of the proline substitution. On the whole, these findings bolster the presumption that the fusion deficiency in G2A GPC is not due to the specific amino acid substitution but rather to the absence of myristoylation.
FIG 5.
Biochemical and functional characterization of myristoylation mutants in ectopically expressed GPC. (A) Vero cells expressing the wild-type and mutant GPCs were metabolically labeled, and lysates were subjected to immunoprecipitation using the GP1-directed MAb BF11 (38). In these studies, the mutant SSPs were expressed in trans with the wild-type GP1/GP2 precursor (fused to the conventional signal peptide of human CD4) to reconstitute native GPC (18, 37). Proteins were resolved by SDS-PAGE, and incorporated [35S]methionine-cysteine was imaged using a Fuji FLA 3000G imager. In addition to the indicated mutants, a sample in which SSP was omitted from the transfection (no SSP) is included to draw attention to SSP association and the presence of the mature GP1 and GP2 subunits in the mutant GPCs. The GP1/GP2 precursor is not proteolytically cleaved in the absence of SSP. The positions of the GP1/GP2 precursor, SSP, and the comigrating GP1 and GP2 subunits are marked. Additional bands of unknown origin are indicated by asterisks (*). In the bottom panel, the immunoprecipitated protein was deglycosylated using peptide N-glycosidase F (New England BioLabs) to resolve the GP1 and GP2 polypeptides (ppGP1 and ppGP2, respectively). (B) The relative cell-cell fusion activities of the GPC mutants were determined using a vaccinia virus-based β-galactosidase fusion reporter assay as described in Materials and Methods. Fusion was induced by exposing the cell monolayer to medium adjusted to pH 5.0, the optimal pH for wild-type GPC fusion. (C) The pH profile for cell-cell fusion was determined by varying the pH of the acidic medium, as indicated. All curves were normalized to the maximum extent of fusion by each GPC (100%).
The molecular basis for the defect in membrane fusion activity is unknown. It is possible that the absence of the myristate moiety might alter the intrinsic metastability of GPC to overly stabilize or destabilize the complex. In many instances, the stability of viral envelope glycoproteins can be probed by assessing the pH at which membrane fusion is activated (25, 52). In wild-type GPC, cell-cell fusion activity is optimally triggered at pH 5.0 (25). By varying the pH to which GPC-expressing cells were exposed, we determined that the optimal pH for cell-cell fusion by the G2A and G2Q mutants was comparable to that of the wild-type and modestly reduced in the G2S and ΔG2 mutants (Fig. 5C). This minor shift in the pH profile is insufficient to account for the magnitude of the observed fusion deficiency at pH 5.0. Retention of the wild-type pH for optimal activation of cell-cell fusion suggests that the functional stability of the prefusion GPC trimer is largely unaffected by the lack of the myristate moiety.
ΔG2-GPC rCan behaves similarly to G2A-GPC rCan.
We chose to introduce the ΔG2 mutation into a reverse genetics-derived rCan virus in order to minimize the likelihood of reversion to a functional myristoylation motif. This virus was readily rescued and, like G2A-GPC rCan, produced small foci (Fig. 1A). ΔG2-GPC rCan also displayed similar growth properties, producing wild-type amounts of virion particles (Fig. 2B) with reduced specific infectivity (15% and 8% of the wild-type rCan in two independent experiments). Purified ΔG2-GPC rCan virions also contained wild-type ratios of NP and GPC (Fig. 3 and Table 1). Thus, ΔG2-GPC rCan was similar to, albeit somewhat more debilitated than, G2A-GPC rCan. Deletion of the N-terminal glycine residue may account for the incremental deficit in ΔG2-GPC rCan. Notably, these findings reinforce the conclusion that the lack of myristoylation, while directly responsible for the observed reduction in specific infectivity, does not adversely affect virion assembly and budding.
Serial passage of ΔG2-GPC rCan fails to generate complementing mutations.
In contrast to G2A-GPC rCan, serial passage of ΔG2-GPC rCan did not result in the emergence of larger wild-type foci (data not shown). This is in keeping with the design of the nonrevertable deletion mutation. To identify any second site mutations that might contribute to viral fitness without an apparent increase in focus size, we used transcriptome sequencing (RNA-Seq) to determine the genetic makeup of the virus population at passage 30. Virion RNA was isolated from cell culture supernatants of Vero cells infected with either the original ΔG2-GPC rCan stock or the passaged virus and provided to the Yale Center for Genome Analysis (Yale School of Medicine) for library construction and deep sequencing using an Illumina HiSeq 2000 instrument. Reads were aligned to reference Candid #1 genome sequences (GenBank accession numbers AY746353.1 and AY746354.1) using the BWA algorithm (45). Both genomic and antigenomic strands were represented. Coverage of the Candid #1 S and L genomic RNAs was complete, with the exception of eight nucleotides at the 5′ terminus of the S RNA, and averaged well over 3,000 reads per nucleotide. This analysis revealed that, other than the ΔG2 mutation, the consensus sequence of the original ΔG2-GPC rCan virus was identical to that of the reverse genetics plasmids and differed from the reference Candid #1 sequences at previously noted sites (J. C. de la Torre, personal communication) (Table 2, italics). We also identified a nonconservative change in the NP open reading frame (K162E) present in 42% of the reads (Table 2) and a silent mutation at amino acid residue 30 in the L protein (9% of reads). Other variants were present at frequencies of <1% and likely reflect sporadic sequencing errors. These results attest to the robust nature of the reverse genetics system. Importantly, sequence analysis of the p30 virus confirmed the absolute retention of the ΔG2 mutation. In addition to variants present in the reverse genetics plasmids, we identified 13 novel nucleotide changes that accumulated to levels of ≥20% in the p30 ΔG2-GPC rCan quasispecies (Table 2). None of these variants emerged upon deep sequencing of wild-type rCan virus, which retained its original sequence through passage 10, at which point serial passage was discontinued. The genetic stability of wild-type rCan in cell culture likely reflects the fact that Candid #1 is typically propagated in Vero cells. Of the 13 mutations in p30 ΔG2-GPC rCan, all but one were within open reading frames, and 10 encoded nonsynonymous substitutions, consistent with a response to selective pressure.
TABLE 2.
Nucleotide changes in p30 ΔG2-GPC rCan
| RNA nucleotide position | Nucleotide change (% of reads)a | Amino acid changea |
|---|---|---|
| S RNA | ||
| 1–8 | Missing | 5′ UTR |
| 9 | A→ C (93) | 5′ UTR |
| 92–94 | Missing | SSP ΔG2 mutation |
| 198 | A → G (77) | SSP N37S |
| 273 | T → A (21) | GP1 F62Y |
| 285 | T → A (36) | GP1 L66Q |
| 462 | T → C (29) | GP1 I125T |
| 488 | T → C (25) | GP1 W134R |
| 590 | G → A (35) | GP1 A168T |
| 2067 | G → A (100) | NP silent |
| 2070 | A → G (100) | NP silent |
| 2178 | G → A (24) | NP silent |
| 2849 | T → C (42, 76)b | NP K162E |
| 3406 | A → T (56) | 3′ UTR |
| L RNA | ||
| 22 | T → A (100) | 5′ UTR |
| 367–368 | tAG → tGA (100) | Z stop (silent) |
| 452 | T → C (100) | L stop (silent) |
| 1634 | A → G (100) | L silent |
| 2891 | C → A (100) | L L1398F |
| 4305 | C → T (100) | L G927E |
| 4682 | T → G (100) | L silent |
| 4688 | G → A (100) | L silent |
| 4803 | C → T (100) | L R761K |
| 4856 | T → C (49) | L silent |
| 4940 | G → A (100) | L silent |
| 5032 | C → T (55) | L D685N |
| 5296 | G → A (100) | L R597W |
| 5321 | G → A (100) | L silent |
| 6045 | T → A (58) | L N347I |
| 6295 | A → T (57) | L S264T |
| 6814 | G → A (100) | L L91F |
| 7107 | C → T (69) | 3′ UTR |
Included are changes present in ≥20% of reads relative to Candid #1 S and L RNA reference genomes (GenBank accession numbers AY746353.1 and AY746354.1, respectively). Changes in the reverse genetics plasmids relative to the reference sequence (J.C. de la Torre, personal communication) are italicized.
Percentages of reads in original and p30 populations, respectively.
In the p30 ΔG2-GPC open reading frame, the sole nucleotide change present in a majority of reads (77%) encodes an N37S mutation within the ectodomain loop of SSP. Additional changes were found in a minority of GP1 sequences: F62Y (21%), L66Q (36%), I125T (29%) W134R (25%), and A168T (35%). Curiously, the A168T variant recreates the functional N-linked glycosylation sequon found in the pathogenic XJ13 isolate of JUNV from which Candid #1 was derived, a change that is reported to be unrelated to Candid #1 attenuation (53, 54) but may influence utilization of the virus receptor, transferrin receptor 1 (55). No amino acid changes were noted in the GP2 fusion subunit. The nonconservative K162E change in NP increased in frequency upon passage to 76% of reads. This region of NP is reported to be involved in ribonucleoprotein formation (56–60), and thus any potential effect of this early arising mutation relative to GPC myristoylation is likely to be indirect. Three nonsynonymous substitutions were also found in the open reading frame of the large, multifunctional L protein: S264T (57% of reads), N347I (58%), and D685N (55%). These mutations lie within the N-terminal domain of the multifunctional L protein, a region that encodes the capping endonuclease and is important for mRNA transcription but not for genome replication (61–63). The silent change at leucine-30 noted in the original virus stock was not retained in the p30 virus. The relationship of these variants in NP and L to viral fitness (as well as that of the variant in the 3′ untranslated region [UTR] of the S RNA) is unclear, and any compensatory effect relative to the lack of GPC myristoylation is likely to be indirect. No changes were noted in the Z matrix protein, which could plausibly interact with GPC in virion assembly and budding.
Of the variants in p30 ΔG2-GPC rCan, only the N37S mutation in the SSP loop was sufficiently frequent in the population and appropriately located to directly influence the fusion deficiency resulting from the lack of myristoylation. However, introduction of the N37S mutation into ectopically expressed wild-type GPC significantly depressed cell-cell fusion activity, which was further reduced to <5% of wild-type levels by the addition of the ΔG2 mutation (Fig. 5B). Clearly, the N37S mutation does not favorably complement the deficiency in cell-cell fusion activity. Despite the low intrinsic fusogenicity of ΔG2/N37S GPC, we were readily able to rescue rCan virus bearing the two mutations. However, the foci produced by this virus were comparable in size to those of ΔG2-GPC rCan (data not shown), suggesting that the N37S mutation is unlikely to have provided a significant growth advantage to the passaged virus. Hence, the relationship, if any, between the N37S mutation and the lack of myristoylation is obscure. Collectively, the absence of phenotypic change upon 30 serial passages of ΔG2-GPC rCan and the dearth of plausible complementing mutations suggest that the virus was unable to directly mitigate the specific defect arising from the lack of myristoylation.
DISCUSSION
In addition to its conventional role in targeting the GPC precursor to the ER, SSP has evolved to fulfill a number of novel functions in the tripartite GPC complex. Importantly, SSP interacts with the GP2 fusion subunit to sense acidic pH and trigger conformational changes leading to membrane fusion. This activity is modulated by amino acid residues within the ectodomain loop and first membrane-spanning region of SSP (25, 64) and by the N-terminal addition of myristate. Ectopically expressed mutants of GPC in which myristoylation is abolished by replacing the critical glycine-2 with alanine were previously shown to support membrane fusion at a level ∼20% that of the wild-type GPC (18, 28). We find that GPC mutants in which glycine is replaced by serine or simply deleted are similarly compromised, reaffirming the importance of myristoylation for membrane fusion activity. The key finding in this report is that this phenotype is exactly recapitulated in the context of the intact Candid #1 virion: the specific infectivities of the G2A-GPC and ΔG2-GPC rCan mutants are reduced 5- to 10-fold, and no additional defects were noted. The numerical concordance between the reduction in cell-cell fusion activity and virus specific infectivity is consistent with a common underlying defect in membrane fusion.
Given the fundamental role of myristoylation in regulating the biological activities of other proteins (26, 27), it is perhaps telling that we were unable to detect additional defects in the mutant viruses. Myristoylation of the Z matrix protein, by contrast, is essential for its trafficking to the membrane, association with GPC, and budding activity (30–32). Notably, serial passage of ΔG2-GPC rCan did not select for compensatory changes in Z. Our negative finding is consistent with the notion that the myristate moiety does not interact with other virion or host cell proteins during virion assembly and budding, perhaps due to sequestration within the GPC trimer.
Despite the substantial fitness cost associated with the lack of GPC myristoylation, we were unable to detect phenotypic reversion of the ΔG2-GPC rCan virus upon 30 passages in cell culture. The fact that 10 of 13 nucleotide substitutions that did arise during passage were nonsynonymous suggests that selection had been active during passage, but the adaptive significance of these changes is difficult to discern. The N37S mutation in GPC was found to be detrimental to cell-cell fusion activity and did not result in an increase in focus size when reintroduced into ΔG2-GPC rCan. Mutations in NP and L could indirectly contribute toward mitigating the fusion deficiency through subtle changes in the rate of viral replication, which might have been missed in our analysis. Importantly, none of the emerged changes appear directly related to the specific defect in GPC membrane fusion.
In the absence of structural information, the molecular basis for the intrinsic defect in fusion activity remains unknown. Our finding that the pH of fusion activation is largely unchanged in the nonmyristoylated mutants suggests that the fusion deficiency does not arise from gross structural alterations in the prefusion GPC trimer. Furthermore, we have shown that G2A GPC is proteolytically cleaved and trafficked to nonraft microdomains on the cell surface comparably to wild-type GPC (29). Nor does the lack of myristoylation significantly perturb the recruitment and incorporation of GPC into rCan viruses. Collectively, our findings suggest that myristoylation is largely unimportant in the context of the prefusion GPC complex.
Rather, we hypothesize that the myristate moiety may function primarily during the fusogenic transitions that lead to the merger of the viral and cellular membranes. Based on analogies from other proteins that undergo a myristate switch as part of their biological function (27, 65), we speculate that the pH-induced structural reorganization in GPC results in expulsion of the myristate moiety from the GPC trimer. This enables the acylated N terminus of SSP to associate with the inner leaflet of the viral membrane, potentially destabilizing the hemifusion diaphragm and promoting fusion pore formation (66). In this model of GPC membrane fusion, the lack of myristoylation would favor fusion arrest at the hemifusion intermediate, much as reported for engineered fusion proteins lacking a full-length transmembrane domain (67–72). This functional defect may be difficult to rescue through simple amino acid substitution and could provide the basis for generating genetically stable attenuated viruses as potential vaccines to protect against arenaviral hemorrhagic fevers.
ACKNOWLEDGMENTS
We are grateful to Juan Carlos de la Torre (Scripps Research Institute, La Jolla, CA) and Slobodan Paessler (University of Texas Medical Branch, Galveston, TX) for providing the Candid #1 reverse genetics plasmids, laboratory protocols, unpublished DNA sequence information, and advice throughout the studies. We are also grateful to Kaya Bilguvan and Christopher Castaldi at the Yale Center for Genome Analysis (Yale School of Medicine) and Sijung Yun (Yotta Biomed, LLC, Potomac, MD) for next-generation sequencing and bioinformatics analysis, respectively. J.H.N. thanks Brian Gowen (Utah State University, Logan, UT) and Yuying Liang (University of Minnesota, Twin Cities, MN) for advice on assessing viral growth kinetics. Monoclonal antibodies used in the studies were kindly provided by BEI Resources (NIAID Biodefense and Emerging Infections Research Program) and the Public Health Agency of Canada (Winnipeg, MB, Canada).
This work was funded in part by a National Institutes of Health (NIH) subaward from grant AI065357 (Rocky Mountain Regional Center of Excellence for Biodefense and Emerging Infectious Diseases grant to J. Belisle, Colorado State University).
REFERENCES
- 1.Salazar-Bravo J, Ruedas LA, Yates TL. 2002. Mammalian reservoirs of arenaviruses. Curr Top Microbiol Immunol 262:25–63. [DOI] [PubMed] [Google Scholar]
- 2.Hirabayashi Y, Oka S, Goto H, Shimada K, Kurata T, Fisher-Hoch SP, McCormick JB. 1989. The first imported case of Lassa fever in Japan. Nihon Rinsho 47:71–75. (In Japanese.) [PubMed] [Google Scholar]
- 3.Haas WH, Breuer T, Pfaff G, Schmitz H, Köhler P, Asper M, Emmerich P, Drosten C, Gölnitz U, Fleischer K, Günther S. 2003. Imported Lassa fever in Germany: surveillance and management of contact persons. Clin Infect Dis 36:1254–1258. doi: 10.1086/374853. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. 2015. Lassa fever confirmed in death of U.S. traveler returning from Liberia. Centers for Disease Control and Prevention, Atlanta, GA: http://www.cdc.gov/media/releases/2015/p0525-lassa.html. [Google Scholar]
- 5.Delgado S, Erickson BR, Agudo R, Blair PJ, Vallejo E, Albariño CG, Vargas J, Comer JA, Rollin PE, Ksiazek TG, Olson JG, Nichol ST. 2008. Chapare virus, a newly discovered arenavirus isolated from a fatal hemorrhagic fever case in Bolivia. PLoS Pathog 4:e1000047. doi: 10.1371/journal.ppat.1000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Briese T, Paweska JT, McMullan LK, Hutchison SK, Street C, Palacios G, Khristova ML, Weyer J, Swanepoel R, Egholm M, Nichol ST, Lipkin WI. 2009. Genetic detection and characterization of Lujo virus, a new hemorrhagic fever-associated arenavirus from southern Africa. PLoS Pathog 5:e1000455. doi: 10.1371/journal.ppat.1000455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NIAID. 25 January 2016. NIAID Category A, B, and C priority pathogens. National Institutes of Health, Bethesda, MD: https://www.niaid.nih.gov/topics/biodefenserelated/biodefense/pages/cata.aspx Accessed 29 June 2016. [Google Scholar]
- 8.Bolken TC, Laquerre S, Zhang Y, Bailey TR, Pevear DC, Kickner SS, Sperzel LE, Jones KF, Warren TK, Amanda Lund S, Kirkwood-Watts DL, King DS, Shurtleff AC, Guttieri MC, Deng Y, Bleam M, Hruby DE. 2006. Identification and characterization of potent small molecule inhibitor of hemorrhagic fever New World arenaviruses. Antiviral Res 69:86–89. doi: 10.1016/j.antiviral.2005.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larson RA, Dai D, Hosack VT, Tan Y, Bolken TC, Hruby DE, Amberg SM. 2008. Identification of a broad-spectrum arenavirus entry inhibitor. J Virol 82:10768–10775. doi: 10.1128/JVI.00941-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee AM, Rojek JM, Spiropoulou CF, Gundersen AT, Jin W, Shaginian A, York J, Nunberg JH, Boger DL, Oldstone MBA, Kunz S. 2008. Unique small molecule entry inhibitors of hemorrhagic fever arenaviruses. J Biol Chem 283:18734–18742. doi: 10.1074/jbc.M802089200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahmutovic S, Clark L, Levis SC, Briggiler AM, Enria DA, Harrison SC, Abraham J. 2015. Molecular basis for antibody-mediated neutralization of New World hemorrhagic fever mammarenaviruses. Cell Host Microbe 18:705–713. doi: 10.1016/j.chom.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buchmeier MJ. 2002. Arenaviruses: protein structure and function. Curr Top Microbiol Immunol 262:159–173. [DOI] [PubMed] [Google Scholar]
- 13.York J, Agnihothram SS, Romanowski V, Nunberg JH. 2005. Genetic analysis of heptad-repeat regions in the G2 fusion subunit of the Junin arenavirus envelope glycoprotein. Virology 343:267–279. doi: 10.1016/j.virol.2005.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eschli B, Quirin K, Wepf A, Weber J, Zinkernagel R, Hengartner H. 2006. Identification of an N-terminal trimeric coiled-coil core within arenavirus glycoprotein 2 permits assignment to class I viral fusion proteins. J Virol 80:5897–5907. doi: 10.1128/JVI.00008-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Igonet S, Vaney MC, Vonhrein C, Bricogne G, Stura EA, Hengartner H, Eschli B, Rey FA. 2011. X-ray structure of the arenavirus glycoprotein GP2 in its postfusion hairpin conformation. Proc Natl Acad Sci U S A 108:19967–19972. doi: 10.1073/pnas.1108910108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parsy ML, Harlos K, Huiskonen JT, Bowden TA. 2013. Crystal structure of Venezuelan hemorrhagic fever virus fusion glycoprotein reveals a class 1 postfusion architecture with extensive glycosylation. J Virol 87:13070–13075. doi: 10.1128/JVI.02298-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eichler R, Lenz O, Strecker T, Garten W. 2003. Signal peptide of Lassa virus glycoprotein GP-C exhibits an unusual length. FEBS Lett 538:203–206. doi: 10.1016/S0014-5793(03)00160-1. [DOI] [PubMed] [Google Scholar]
- 18.York J, Romanowski V, Lu M, Nunberg JH. 2004. The signal peptide of the Junín arenavirus envelope glycoprotein is myristoylated and forms an essential subunit of the mature G1-G2 complex. J Virol 78:10783–10792. doi: 10.1128/JVI.78.19.10783-10792.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agnihothram SS, York J, Nunberg JH. 2006. Role of the stable signal peptide and cytoplasmic domain of G2 in regulating intracellular transport of the Junin virus envelope glycoprotein complex. J Virol 80:5189–5198. doi: 10.1128/JVI.00208-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lenz O, ter Meulen J, Klenk H-D, Seidah NG, Garten W. 2001. The Lassa virus glycoprotein precursor GP-C is proteolytically processed by subtilase SKI-1/S1P. Proc Natl Acad Sci U S A 98:12701–12705. doi: 10.1073/pnas.221447598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beyer WR, Popplau D, Garten W, von Laer D, Lenz O. 2003. Endoproteolytic processing of the lymphocytic choriomeningitis virus glycoprotein by the subtilase SKI-1/S1P. J Virol 77:2866–2872. doi: 10.1128/JVI.77.5.2866-2872.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agnihothram SS, York J, Trahey M, Nunberg JH. 2007. Bitopic membrane topology of the stable signal peptide in the tripartite Junín virus GP-C envelope glycoprotein complex. J Virol 81:4331–4337. doi: 10.1128/JVI.02779-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.York J, Nunberg JH. 2007. A novel zinc-binding domain is essential for formation of the functional Junín virus envelope glycoprotein complex. J Virol 81:13385–13391. doi: 10.1128/JVI.01785-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Briknarova K, Thomas CJ, York J, Nunberg JH. 2011. Structure of a zinc-binding domain in the Junin virus envelope glycoprotein. J Biol Chem 286:1528–1536. doi: 10.1074/jbc.M110.166025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.York J, Nunberg JH. 2006. Role of the stable signal peptide of the Junín arenavirus envelope glycoprotein in pH-dependent membrane fusion. J Virol 80:7775–7780. doi: 10.1128/JVI.00642-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maurer-Stroh S, Eisenhaber F. 2004. Myristoylation of viral and bacterial proteins. Trends Microbiol 12:178–185. doi: 10.1016/j.tim.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 27.Resh MD. 2006. Trafficking and signaling by fatty-acylated and prenylated proteins. Nat Chem Biol 2:584–590. doi: 10.1038/nchembio834. [DOI] [PubMed] [Google Scholar]
- 28.Saunders AA, Ting JP, Meisner J, Neuman BW, Perez M, de la Torre JC, Buchmeier MJ. 2007. Mapping the landscape of the lymphocytic choriomeningitis virus stable signal peptide reveals novel functional domains. J Virol 81:5649–5657. doi: 10.1128/JVI.02759-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agnihothram SS, Dancho B, Grant KW, Grimes ML, Lyles DS, Nunberg JH. 2009. Assembly of arenavirus envelope glycoprotein GPC in detergent-soluble membrane microdomains. J Virol 83:9890–9900. doi: 10.1128/JVI.00837-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Capul AA, Perez M, Burke E, Kunz S, Buchmeier MJ, de la Torre JC. 2007. Arenavirus Z-GP association requires Z myristoylation but not functional RING or L domains. J Virol 81:9451–9460. doi: 10.1128/JVI.00499-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perez M, Greenwald DL, de la Torre JC. 2004. Myristoylation of the RING finger Z protein is essential for arenavirus budding. J Virol 78:11443–11448. doi: 10.1128/JVI.78.20.11443-11448.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Strecker T, Maisa A, Daffis S, Eichler R, Lenz O, Garten W. 2006. The role of myristoylation in the membrane association of the Lassa virus matrix protein Z. Virol J 3:93. doi: 10.1186/1743-422X-3-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Emonet SF, Seregin AV, Yun NE, Poussard AL, Walker AG, de la Torre JC, Paessler S. 2011. Rescue from cloned cDNAs and in vivo characterization of recombinant pathogenic Romero and live-attenuated Candid #1 strains of Junin virus, the causative agent of Argentine hemorrhagic fever disease. J Virol 85:1473–1483. doi: 10.1128/JVI.02102-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ghiringhelli PD, Rivera-Pomar RV, Lozano ME, Grau O, Romanowski V. 1991. Molecular organization of Junin virus S RNA: complete nucleotide sequence, relationship with other members of the Arenaviridae and unusual secondary structures. J Gen Virol 72:2129–2141. doi: 10.1099/0022-1317-72-9-2129. [DOI] [PubMed] [Google Scholar]
- 35.Fuerst TR, Niles EG, Studier FW, Moss B. 1986. Eukaryotic transient-expression system based on recombinant vaccinia virus that synthesizes bacteriophage T7 RNA polymerase. Proc Natl Acad Sci U S A 83:8122–8126. doi: 10.1073/pnas.83.21.8122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.York J, Nunberg JH. 2007. Distinct requirements for signal peptidase processing and function of the stable signal peptide (SSP) subunit in the Junin virus envelope glycoprotein. Virology 359:72–81. doi: 10.1016/j.virol.2006.08.048. [DOI] [PubMed] [Google Scholar]
- 37.Eichler R, Lenz O, Strecker T, Eickmann M, Klenk HD, Garten W. 2003. Identification of Lassa virus glycoprotein signal peptide as a trans-acting maturation factor. EMBO Rep 4:1084–1088. doi: 10.1038/sj.embor.7400002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sanchez A, Pifat DY, Kenyon RH, J PC, McCormick JB, Kiley MP. 1989. Junin virus monoclonal antibodies: characterization and cross-reactivity with other arenaviruses. J Gen Virol 70:1125–1132. doi: 10.1099/0022-1317-70-5-1125. [DOI] [PubMed] [Google Scholar]
- 39.York J, Berry JD, Ströher U, Li Q, Feldmann H, Lu M, Trahey M, Nunberg JH. 2010. An antibody directed against the fusion peptide of Junin virus envelope glycoprotein GPC inhibits pH-induced membrane fusion. J Virol 84:6119–6129. doi: 10.1128/JVI.02700-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baird NL, York J, Nunberg JH. 2012. Arenavirus infection induces discrete cytosolic structures for RNA replication. J Virol 86:11301–11310. doi: 10.1128/JVI.01635-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.York J, Dai D, Amberg SA, Nunberg JH. 2008. pH-induced activation of arenavirus membrane fusion is antagonized by small-molecule inhibitors. J Virol 82:10932–10939. doi: 10.1128/JVI.01140-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.York J, Nunberg JH. 2009. Intersubunit interactions modulate pH-induced activation of membrane fusion by the Junin virus envelope glycoprotein GPC. J Virol 83:4121–4126. doi: 10.1128/JVI.02410-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nussbaum O, Broder CC, Berger EA. 1994. Fusogenic mechanisms of enveloped-virus glycoproteins analyzed by a novel recombinant vaccinia virus-based assay quantitating cell fusion-dependent reporter gene activation. J Virol 68:5411–5422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Andrews S. 2014. FastQC: a quality control tool for high throughput sequence data. Babraham Institute, Cambridge, United Kingdom: http://www.bioinformatics.babraham.ac.uk/projects/fastqc/. [Google Scholar]
- 45.Li H, Durbin R. 2009. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25:1754–1760. doi: 10.1093/bioinformatics/btp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, Marth G, Abecasis G, Durbin R. 2009. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25:2078–2079. doi: 10.1093/bioinformatics/btp352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Robinson JT, Thorvaldsdottir H, Winckler W, Guttman M, Lander ES, Getz G, Mesirov JP. 2011. Integrative genomics viewer. Nat Biotechnol 29:24–26. doi: 10.1038/nbt.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Maiztegui JI, McKee KT Jr, Barrera Oro JG, Harrison LH, Gibbs PH, Feuillade MR, Enria DA, Briggiler AM, Levis SC, Ambrosio AM, Halsey NA, Peters CJ. 1998. Protective efficacy of a live attenuated vaccine against Argentine hemorrhagic fever. AHF Study Group. J Infect Dis 177:277–283. doi: 10.1086/514211. [DOI] [PubMed] [Google Scholar]
- 49.Ambrosio A, Saavedra M, Mariani M, Gamboa G, Maiza A. 2011. Argentine hemorrhagic fever vaccines. Hum Vaccin 7:694–700. doi: 10.4161/hv.7.6.15198. [DOI] [PubMed] [Google Scholar]
- 50.Centers for Disease Control and Prevention. 2009. Biosafety in microbiological and biomedical laboratories, 5th ed Centers for Disease Control and Prevention, Atlanta, GA. [Google Scholar]
- 51.Towler DA, Gordon JI, Adams SP, Glaser L. 1988. The biology and enzymology of eukaryotic protein acylation. Annu Rev Biochem 57:69–99. doi: 10.1146/annurev.bi.57.070188.000441. [DOI] [PubMed] [Google Scholar]
- 52.Steinhauer DA, Martin J, Lin YP, Wharton SA, Oldstone MB, Skehel JJ, Wiley DC. 1996. Studies using double mutants of the conformational transitions in influenza hemagglutinin required for its membrane fusion activity. Proc Natl Acad Sci U S A 93:12873–12878. doi: 10.1073/pnas.93.23.12873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Albariño CG, Bird BH, Chakrabarti AK, Dodd KA, Flint M, Bergeron E, White DM, Nichol ST. 2011. The major determinant of attenuation in mice of the Candid1 vaccine for Argentine hemorrhagic fever is located in the G2 glycoprotein transmembrane domain. J Virol 85:10404–10408. doi: 10.1128/JVI.00856-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Seregin AV, Yun NE, Miller M, Aronson J, Smith JK, Walker AG, Smith JN, Huang C, Manning JT, de la Torre JC, Paessler S. 2015. The glycoprotein precursor gene of Junin virus determines the virulence of the Romero strain and the attenuation of the Candid #1 strain in a representative animal model of Argentine hemorrhagic fever. J Virol 89:5949–5956. doi: 10.1128/JVI.00104-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Droniou-Bonzom ME, Reignier T, Oldenburg JE, Cox AU, Exline CM, Rathbun JY, Cannon PM. 2011. Substitutions in the glycoprotein (GP) of the Candid #1 vaccine strain of Junin virus increase dependence on human transferrin receptor 1 for entry and destabilize the metastable conformation of GP. J Virol 85:13457–13462. doi: 10.1128/JVI.05616-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hastie KM, Liu T, Li S, King LB, Ngo N, Zandonatti MA, Woods VL Jr, de la Torre JC, Saphire EO. 2011. Crystal structure of the Lassa virus nucleoprotein-RNA complex reveals a gating mechanism for RNA binding. Proc Natl Acad Sci U S A 108:19365–19370. doi: 10.1073/pnas.1108515108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brunotte L, Kerber R, Shang W, Hauer F, Hass M, Gabriel M, Lelke M, Busch C, Stark H, Svergun DI, Betzel C, Perbandt M, Gunther S. 2011. Structure of the Lassa virus nucleoprotein revealed by X-ray crystallography, small-angle X-ray scattering, and electron microscopy. J Biol Chem 286:38748–38756. doi: 10.1074/jbc.M111.278838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.D'Antuono A, Loureiro ME, Foscaldi S, Marino-Buslje C, Lopez N. 2014. Differential contributions of tacaribe arenavirus nucleoprotein N-terminal and C-terminal residues to nucleocapsid functional activity. J Virol 88:6492–6505. doi: 10.1128/JVI.00321-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Levingston Macleod JM, D'Antuono A, Loureiro ME, Casabona JC, Gomez GA, Lopez N. 2011. Identification of two functional domains within the arenavirus nucleoprotein. J Virol 85:2012–2023. doi: 10.1128/JVI.01875-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ortiz-Riano E, Cheng BY, de la Torre JC, Martinez-Sobrido L. 2012. Self-association of lymphocytic choriomeningitis virus nucleoprotein is mediated by its N-terminal region and is not required for its anti-interferon function. J Virol 86:3307–3317. doi: 10.1128/JVI.05503-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lelke M, Brunotte L, Busch C, Günther S. 2010. An N-terminal region of Lassa virus L protein plays a critical role in transcription but not replication of the virus genome. J Virol 84:1934–1944. doi: 10.1128/JVI.01657-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Morin B, Coutard B, Lelke M, Ferron F, Kerber R, Jamal S, Frangeul A, Baronti C, Charrel R, de Lamballerie X, Vonrhein C, Lescar J, Bricogne G, Günther S, Canard B. 2010. The N-terminal domain of the arenavirus L protein is an RNA endonuclease essential in mRNA transcription. PLoS Pathog 6:e1001038. doi: 10.1371/journal.ppat.1001038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wallat GD, Huang Q, Wang W, Dong H, Ly H, Liang Y, Dong C. 2014. High-resolution structure of the N-terminal endonuclease domain of the Lassa virus L polymerase in complex with magnesium ions. PLoS One 9:e87577. doi: 10.1371/journal.pone.0087577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Messina EL, York J, Nunberg JH. 2012. Dissection of the role of the stable signal peptide of the arenavirus envelope glycoprotein in membrane fusion. J Virol 86:6138–6145. doi: 10.1128/JVI.07241-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ames JB, Tanaka T, Stryer L, Ikura M. 1996. Portrait of a myristoyl switch protein. Curr Opin Struct Biol 6:432–438. doi: 10.1016/S0959-440X(96)80106-0. [DOI] [PubMed] [Google Scholar]
- 66.Melikyan GB, Brener SA, Ok DC, Cohen FS. 1997. Inner but not outer membrane leaflets control the transition from glycosylphosphatidylinositol-anchored influenza hemagglutinin-induced hemifusion to full fusion. J Cell Biol 136:995–1005. doi: 10.1083/jcb.136.5.995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Weiss CD, White JM. 1993. Characterization of stable Chinese hamster ovary cells expressing wild-type, secreted, and glycosylphosphatidylinositol-anchored human immunodeficiency virus type 1 envelope glycoprotein. J Virol 67:7060–7066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Salzwedel K, Johnston PB, Roberts SJ, Dubay JW, Hunter E. 1993. Expression and characterization of glycophospholipid-anchored human immunodeficiency virus type 1 envelope glycoproteins. J Virol 67:5279–5288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kemble GW, Danieli T, White JM. 1994. Lipid-anchored influenza hemagglutinin promotes hemifusion, not complete fusion. Cell 76:383–391. doi: 10.1016/0092-8674(94)90344-1. [DOI] [PubMed] [Google Scholar]
- 70.Melikyan GB, White JM, Cohen FS. 1995. GPI-anchored influenza hemagglutinin induces hemifusion to both red blood cell and planar bilayer membranes. J Cell Biol 131:679–691. doi: 10.1083/jcb.131.3.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Armstrong RT, Kushnir AS, White JM. 2000. The transmembrane domain of influenza hemagglutinin exhibits a stringent length requirement to support the hemifusion to fusion transition. J Cell Biol 151:425–437. doi: 10.1083/jcb.151.2.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li Z, Blissard GW. 2008. Functional analysis of the transmembrane (TM) domain of the Autographa californica multicapsid nucleopolyhedrovirus GP64 protein: substitution of heterologous TM domains. J Virol 82:3329–3341. doi: 10.1128/JVI.02104-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gimenez HB, Boersma DP, Compans RW. 1983. Analysis of polypeptides in Tacaribe virus-infected cells. Virology 128:469–473. doi: 10.1016/0042-6822(83)90272-6. [DOI] [PubMed] [Google Scholar]