Abstract
There are more than 10 million prisoners worldwide, and the prevalence of all investigated mental disorders is higher than general population comparisons. Although the extent to which prison increases the incidence of mental disorders is uncertain, there is considerable evidence of low rates of identification and treatment of psychiatric disorders. Prisoners are also at increased risk of all-cause mortality, suicide, self-harm, violence, and victimization, and research has outlined some modifiable risk factors. High quality treatment trials for psychiatric disorders in prisoners have been limited. Despite this, it has been shown in trials that opiate substitution treatments reduce substance misuse relapse and possibly reoffending. The mental health needs of women and older adults in prison are distinct, and national policies should be developed to meet these. Clinical, research, and policy recommendations to improve prison mental healthcare are presented. National attempts to meet these recommendations should be annually surveyed.
Introduction
There are more than 10 million individuals in prison at any given time with more than 30 million circulating through each year. Research has consistently shown that prisoners have high rates of psychiatric disorders, and in some countries there are more people with severe mental illness in prisons than psychiatric hospitals. Despite the high level of need, these disorders are frequently underdiagnosed and poorly treated. In this structured review, we provide an overview of the epidemiology of psychiatric disorders in prison, summarise information on rates of suicide and violence victimisation and risk factors for these outcomes, and outlineevidence-based interventions for mental health. Based on this, we propose a series of clinical, research, and policy recommendations. The aim is to provide a broad synthesis of the main issues relating to the mental health of adult prisoners, and highlight gaps in evidence and practice. Two special populations are briefly discussed, namely women and older adults. Juveniles in prison have distinct mental health needs, and an overview of these is outside the scope of this review.
In this review, we have used the terms jails and prisons interchangeably and include those who have received a criminal sentence and are detained pretrial (but not individuals in police custody or detained for non-criminal reasons,such as immigration centres).
Search strategy and selection criteria
We conducted a structured search for systematic reviews on prisoner mental health over 2003-2015. We supplemented the search by identifying large primary studies on individual psychiatric disorders, rates and risk factors for adverse outcomes, and interventions for mental health problems. We scanned reference lists of papers identified. Search terms and selection criteria are presented in the Panel.
Prevalence
Many primary studies and reviews have documented the high prevalence of most psychiatric disorders in prisoners (Table 1); however caution is warranted when interpreting these data. First, published studies may overestimate prevalence. Self-report approaches to clinical diagnosis are problematic. In addition, prisoners assessed by lay interviewers have been associated with higher prevalences compared to diagnostic interviews conducted by clinically trained psychiatrists or psychologists.1 Certain disorders may be particularly prone to overestimation. One example is ADHD; heterogeneity between the primary research studies on prevalence is substantial. One systematic review reported that 26% of adult prisoners have an ADHD diagnosis,2 in contrast to two recent high quality studies using self-report measures and diagnostic instruments with reported prevalence rates of 17%3 and 11%4, respectively. This disparity suggests that the choice of statistical models when pooling prevalence estimates needs careful consideration. In particular, random effects models should be used with caution as they weight smaller studies similarly to the larger ones. If used, they should be complemented with a fixed effects model, and examination of individual study quality. For some diagnoses, large high quality studies should be prioritised over many smaller investigations that may reflect publication bias. Furthermore, the heterogeneity of prevalence estimates may reflect real differences related to variations in community rates for individual disorders around the world, how the police and courts approach mental illness, incarceration rates for different crimes, and provision of prison healthcare. Where variations between countries is large, pooling estimates may not be meaningful and prevalence ranges should be provided.
Table 1. Prevalence of different psychiatric diagnoses in adult prisoners based on systematic reviews.
Some prevalence studies of personality disorders in prisoners are problematic for similar reasons. Large high quality studies using clinically-based diagnoses have reported prevalences between 7-10%5,6 compared to the 65% found in reviews of studies that have used diagnostic instruments.1 The discrepancy may be partly explained due to the inclusion of antisocial personality disorder, the most common personality disorder in prisoners, for which diagnostic criteria overlap with the reasons for entering prison and diagnostic instruments will score. Three of these criteria (disregarding norms and rules, low threshold for aggression or violence, and inability to profit from experience) are together highly correlated with criminogenic factors.
A second problem is that many diagnostic instruments currently used have not been validated in prisons, and include items that may not be specific. For example, the MINI diagnostic interview isextensively used in newer prison studies, and without modification canlead to overestimating rates of mania and obsessive-compulsive disorder.7 In addition, screening tools may be particularly susceptible to false positives. For example, in a recent investigation to identify autism spectrum disorders in Scottish prisoners, only 6% of those that screened positive were clinically diagnosed with such disorders.8 As a result, case identification is poor.9
Despite these caveats, a number of prevalence findings are consistent. The evidence for major depression and psychotic illnesses is the strongest. A 2012 systematic reviewof around 33,000 prisoners and over 100 studies found very similar findings to a previous 2002 review (Table 1). According to these reviews, one in seven prisoners has major depression or psychosis, with little change in rates over the last three decades.10 Another consistent theme, including in low and middle income (LMI) countries, is the high rate of substance misuse. Recent research has also demonstrated high rates of comorbidity between mental illness and substance misuse.11 Such comorbidity worsens the prognosis of the individual psychiatric disorders, and has been shown to increase repeat offending and premature mortality following release.12 A further finding consistently reported is the higher rate of psychiatric disorders, particularly depression10 and drug dependence13, in female prisoners. Future prevalence research should focus on special populations, prisoners in LMI countries, and investigating comorbidities. The new problem of novel psychoactive agents, which is common in many prisons, requires more research, and whether it exacerbates mental health problems and other risks. In England and Wales, the Inspectorate of Prisons stated that these substances, particularly synthetic cannabinoids, have led to increased violence in prison as a direct result of drug intoxication or increased bullying due to drug debts.14 The difficulties, however, of reliable detection and disincentives to self-report their use mean that innovative designs are required.
A key issue in this field is the direction of causality for the high prevalences of psychiatric disorders, namely whether the excess in rates is caused by prison or whether they are imported into prison.There is evidence for the importation hypothesis since severe mental illnesses are associated with criminality,15,16 but more longitudinal studies are needed following entry into prison (See Research Recommendations). One prospective study in English prisons found that symptoms of depression decreased in the months following arrival in prison, but psychotic symptoms remained stable.17 Although the study was underpowered for categorical psychiatric diagnoses, it suggested that the stresses secondary to criminal conviction and prison entry are not the only explanations for high rates of mental disorder. Self-report data from a national survey of Australian prisoners found that around half those interviewed reported that their mental health improved during their imprisonment.18
In the subsequent section, we will review adverse outcomes that are associated with psychiatric disorders.
Adverse Outcomes
Suicide and Self-harm
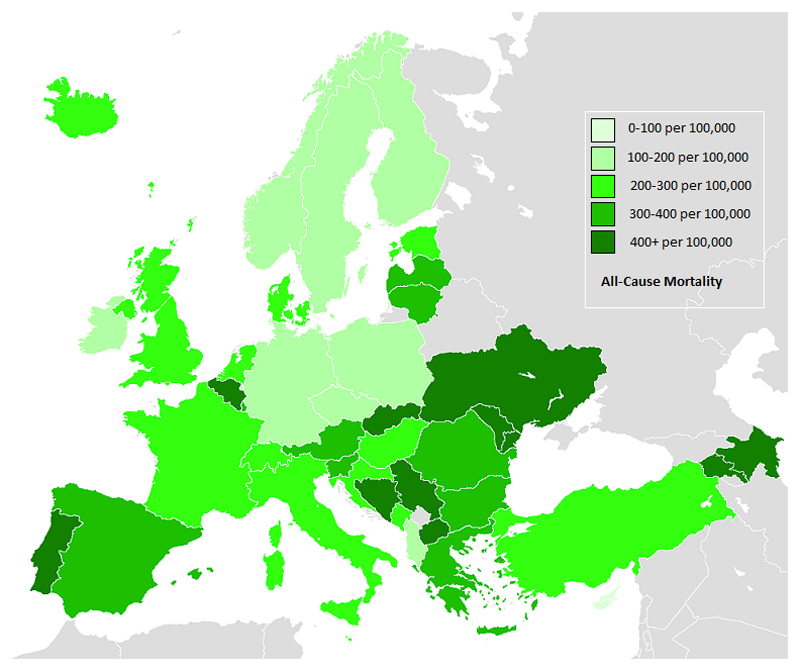
Suicide and self-harm are more common in prisoners than community-based persons of similar age and gender. Where studied, the relative risks of suicide in male prisoners are around 3-6 compared to the general population, and higher risks in women prisoners (with relative risks typically more than 6). Explanations for the differences in relative risks between countries is not clear and is not correlated with incarceration rates or general population suicide rates.19 More widely, suicide numbers are difficult to validate due to misclassification of suicides as accidents, unknown or natural deaths, and reluctance in some countries to characterise self-inflicted deaths in custody as suicides. For this reason, we suggest that all-cause mortality in prison may be a better proxy than official suicide ratesfor international comparisons when including countries where suicide reporting in prisons has not been validated. Using data routinely collected in the European Union, we have calculated three-year all-cause mortality rates in EU countries with at least two years of data (presented in Figure 1).20,22 These show some notable differences between Western and Eastern Europe which may be explained by higher rates of death from infectious diseases in the latter. However, in Western Europe, higher rates of all-cause mortality in prison for Belgium and Portugal need further examination. When looking specifically at suicide, France is an outlier with a reported suicide rate of 179 per 100,000 prisoners23 whereas most countries report around 100-150 per 100,000. Interestingly, another outlier is the US where suicide rates in local jails are 41 per 100,000, and in state prisons 16 per 100,000.24 One possible explanation is the higher proportion of African American and Hispanic prisoners there, who have lower suicide rates, but even in white prisoners, suicide rates appear to be lower than in many European countries (80 per 100,000 in U.S. local jails and 25 per 100,000 in U.S. state prisons).24
Figure 1. Mean annual all-cause mortality rates in European Union countries during 2011-201320–22.
Self-harm is a substantial cause of morbiditybut less studied than suicide. A recent epidemiological study in English and Welsh prisons found that in the previous 12 months in custody, 5-6% of men and 20-24% of women self-harmed.25 Risk factors include younger age and short sentences, and there is evidence that self-harm clusters in certain prison settings. A summary of risk factors for suicide, near-lethal self-harm, and self-harm are presented in Table 2. Near-lethal self-harm has been shown to be a valid proxy for completed suicide in prisons, and has advantages over psychological autopsy approaches because it allows for a broader and deeper range of risk factors to be evaluated.26
Table 2. Risk factors for suicide, near-lethal self-harm, self-harm, violence, and victimisation in prisoners.
| Suicide78 | Near-lethal self-harm 7,79 | Self-harm 25 | Prison Violence 41 | Physical Victimisation 81– 84 |
|---|---|---|---|---|
| Risk Factors | Risk Factors | Risk factors | Risk Factors | Risk Factors |
| Suicidal ideation | White ethnicity | Young age | Younger age | Mental disorder |
| Single cell occupancy | No educational qualifications | White ethnicity | Minority ethnic group | Younger age |
| History of attempted suicide | Prior prison spell | Sentence length <12 months | Less formal education | White ethnicity |
| Current psychiatric diagnosis | Less than 30 days in prison | Life sentence | Shorter sentence | Sexual offence |
| Psychotropic medication | Mood disorders | Detainee/remand status | Gang affiliation | Past victimisation |
| Detainee/remand status | Anxiety disorders | Previous violent offence (women only) | Prior arrests | Gang involvement |
| Life sentence | Psychoses | Prior incarceration | Dissatisfaction with officers | |
| Murder/manslaughter offence | Drug use disorder | Prior poor incarceration adjustment | ||
| Violent offence | Past psychiatric treatment | Aggression | ||
| Alcohol use problems | Previous self-harm in prison | Psychopathology | ||
| Past contact with mental health services79 | Previous self-harm outside prison | Less social support | ||
| Being married before prison | Two or more psychiatric disorders | Major mental illness | ||
| Protective Factors | Psychopathy | |||
| Black race/ethnicity | Substance misuse | |||
| Length of sentence <18 months | Dual diagnosis (mental illness and substance misuse) | |||
| Sentenced | Protective Factors | Protective Factors | ||
| Older age | Involvement in work programmes | |||
| Sexual Victimisation 34 | ||||
| Risk Factors | ||||
| Mental disorder | ||||
| Female | ||||
| Minority ethnic group |
In terms of interventions for the management of suicide and self-harmin prison, a number have been reviewed,27 ranging from screening on reception, staff training, treatment, appropriate supervision of at-risk prisoners, and improvements to the safety of the physical environment and social support. Overall, the studies have indicated the importance of adequate screening for suicide risk with comprehensive care planning based on identified risk on arrival to prison. However, this research is difficult to appraise as most report many simultaneous changes within a prison system, so independent effects cannot be reliably determined. For example in England and Wales, the suicide prevention and management strategyfor prisons was amended in 2004 by improving identification and risk assessment,28 and there was a subsequent reduction in prison suicide rates over 2004 to 2006, although rates have increased since 2012.29,30Screening tools for identifying prisoners at risk of suicide and self-harm were reviewed in 2010.31 Sensitivity and specificity varied widely between tools, but since none of the studies were prospective, limited conclusions can be drawnand more research is needed on screens that have high specificities (see Research Recommendations). Another recommended intervention has been training of suicide risk assessment and management, often focusing on communication skills. Evaluations of training programmes have not been sufficiently robust to show an effect on suicide outcomes, but have reported that these approaches are acceptable to staff.27
Guidelines for suicide prevention have recommended early screening of prisoners at first reception to custody, actions taken in response to positive screening, and ongoing risk monitoring.32 Multidisciplinary information sharing and decision-making are emphasised along with appropriate mental health treatment (see Clinical Recommendations). Finally staff training and environmental safety (e.g., removal of potential risks such as ligature suspension points) are recommended.
Violence and Victimisation
Other adverse outcomes that may arise as a result of psychiatric disorders are violence and victimisation within prison. While violence is common in many prisons, little research exists on its prevalence. Some studies have estimated the rates of physical assault are 13 to 27 times higher than the general population.33,35 Non-lethal prisoner-on-prisoner physical assault is the most frequently seen form of violence in prison, though homicides are reported.36 One recent study involving 7,528 US prisoners found a six-month prevalence rate of 205 per 1000 for inmate-on-inmate physical violence and 246 per 1000 for staff-on-inmate physical violence.33 US official statistics suggest that the rate of violent assaults on prison staff (155 per 1000 persons) is more than double that of mental health staff.37 UK data for 2015 showed that per 1000 prisoners, there were 198 incidents of assault on a prisoner, and 46 of assault on staff.38 Again, methodological problems mean that exact figures should be interpreted with caution; official statistics underestimate violence prevalence and base rates of violence can vary due to differences in violence definition and measurement.
Research aimed at understanding violence within prisons has investigated individual pre-incarceration characteristics and contextual factors. A meta-analysis of 90 studies (published between 1996 and 2012) of institutional infractions found that strong contextual predictors of infractions were higher levels of gang activity, larger prison populations, and a higher security level of the institution or proportion of high-security inmates. In contrast, modestly lower infractions rates were found in settings with a greater level of employment inside prison. The strongest socio-demographic predictor of prison misconduct was a younger age, whereas being black, unmarried, and with a low education level were weaker correlates. In terms of criminological characteristics, the presence of prior infractions was the strongest predictor, while conviction for a violent offence was not a significant predictor.39 Early deviant behaviours (i.e., a more extensive criminal history, a younger age when first arrested, and prior incarcerations) have also been associated with management difficulties while incarcerated. Finally, clinical variables such as aggressiveness, impulsiveness, antisocial traits, and psychopathy are robust predictors of institutional infractions.40,41
Prisoners with mental health disorders are disproportionately involved in prison infractions and violent incidents,41,42 and are more likely to be charged with violating prison rules than other prisoners, and twice as likely to be injured in a fight.43 Mentally disordered offenders with a history of violence are at even greater risk.44
In terms of victimisation, official estimates under-represent its extent in prisons as there are socio-cultural disincentives to reporting and a particular reluctance of prisoners to report staff victimisation.45 Prisoners who have characteristics making them more likely victims of physical assault (e.g., transgender, intellectual disability) may be systematically over- or underrepresented, while victimisation by staff may be under-reported. Physical violence is only one form of victimisation and should be considered alongside property theft, emotional and psychological victimisation, intimidation, and sexual victimisation.
A summary of risk factors (Table 2) demonstrates that psychiatric disorder is associated with violence and victimisation outcomes in prison. This is corroborated by a large US regional survey of state prisons with a total of 7,528 individuals, where one in 12 male prisoners with a mental disorder reported at least one incident of sexual victimisation by another prisoner over a six-month period, compared with one in 33 male prisoners without a mental disorder, and sexual victimisation was three times as high among female prisoners (23%) as among male prisoners (8%).34 Mental disorder also increased risks of physical victimisation. Men in prison with any mental disorder were 1.6 times (prisoner-on-prisoner) and 1.2 times (staff-on-prisoner) higher than men with no mental disorder to be physically victimized. Female prisoners with mental disorder were 1.7 times more likely to report being physically victimized by another prisoner than their non-mentally disorderedpeers.33
Overall, we have demonstrated the confluence of adverse outcomes that mentally disordered are at increased risk of. These include self-harm, suicide, violence and victimization in prison, and premature mortality and reoffending on release. The risk factors have little specificity, and also few are shared across these outcomes. Two that are shared are mental illness and substance misuse. But without further clarification of modifiable risk factors, development of effective interventions will be limited. Environmental risk factors need to be considered, such as staffing, overcrowding, policies, and the extent and nature of daytime activities, and considered alongside individual-level factors.
Interventions
Mental Illness
Many interventions aimed at prisoner mental health have been evaluated, though mostly on a small scale. The small sample size, and heterogeneity of prisoners and settings makes synthesis of the research difficult. The lack of research conducted in prisons compared to community settings is secondary to a combination of organisational difficulties (such as obtaining permissions and running interventions alongside mandated programmes), a lack of specific research funding, and a perceived division of prisoner health from public health in general (see Research Recommendations).
The number of medication trials conducted in prisons is particularly low. Some small RCTs have found evidence for ADHD medications in Swedish prisoners, including improved global functioning46 and increased likelihood of abstinence from amphetamine after release (as measured by negative urine samples).47 Work with other medications is limited. Another study found that, in women with bipolar disorder, following an evidence-based pharmacological treatment algorithm was no better than treatment as usual (where medication decisions were taken by the treating clinician)48 for reducing symptoms and improving medication adherence. More psychopharmacology research in prison settings is required, particularly for commonly prescribed psychotropic medications (see Research Recommendations).
Compared with medication, there are more controlled trials of psychological therapies in prisoners, but these are typically small and involve a wide variety of interventions (e.g., cognitive behavioural [CBT], interpersonal, dialectical behavioural [DBT], meditation-based, and group therapies) with inconsistent findings. Larger trials include a study of yoga amongst 167 prisoners, where participants randomised to yoga had lower self-rated psychological distress and improved cognitive performance than controls who kept an exercise diary.49 In another study, 120 Iranian prisoners were randomised to receive individual CBT, combined individual and group CBT, or placed on a waiting list. The study reported improvements in psychological well-being symptom scores for the sample receiving combined therapy relative to controls.50 Another study included 63 prisoners who received a modified form of DBT and were then randomised into receiving eight weeks of further DBT or case management.51 Those receiving further DBT showed a reduction in psychopathological symptoms at six months compared with the case management group but not at twelve months.
In summary, there is some evidence for these psychological interventions, but their effect sizes are not large, whether they would hold in better quality designs (e.g. using active controls and not waiting list or treatment as usual controls), and it is uncertain whether any improvements are sustained. While there are further psychological treatment trials involving female prisoners and individuals with substance misuse (see below), there is a lack of high quality large trials. Thus, theeffectivenessof commonly used psychological interventions to treat mental health problemsneeds further clarification (see Research Recommendations). Furthermore, in the absence of good quality treatment trials in prisons, treatments developed in the community need to be imported and evaluated (see Clinical Recommendations). The prison environment, in particular the increased structures, different rules, housing, and access to drugs create unique challenges, which may explain why psychological treatments do not generalise well. It also suggests that tailored interventions for prisoners, particularly for substance misuse, are required.
Substance Misuse
Research into prisoners with substance misuse includes trials of pharmacological and psychological interventions. Differences in study design, sample size, and a variety of heterogeneous outcome measures make synthesis of the data difficult. Nevertheless, it is possible to provide some principles of treatment.
Alcohol and opiates are the two most common and problematic substances for detoxification management in prisons although provision of such treatment services is variable. One survey found that only 34% of US jails offer any detoxification treatment52 equating to about one million arrestees annually being at risk of untreated withdrawal from alcohol, including delirium tremens and its associated high mortality.53 A 2010 Cochrane review summarizing evidence from 64 RCTs in community settings found that benzodiazepines are effective against alcohol withdrawal seizures compared to placebo, and are protective for many outcomes compared to alternative drugs.54
The management of opiate withdrawal in prison is generally symptomatic, and mostly based on detoxification rather than maintenance. A systematic review identified 23 controlled trials with 2467 adult opioid userswhich included samples with criminal histories.55 Participants were randomised to receive methadone or another pharmacological agent, with evidence finding slow tapering with long-acting opioids reduced withdrawal severity, though relapse was common.55 One exemplar included in this review is the Leeds Evaluation of Efficacy of Detoxification Study (LEEDS), an open-label RCT of 306 prisoners in three English prisons. This trial compared methadone and buprenorphine detoxification and found equivalent clinical effectiveness. A further RCT from this group compared dihydrocodeine and buprenorphine demonstrating comparable effectiveness for acute opiate detoxification.56 On the basis of this evidence, all prisoners should be offered acute detoxification on arrival (see Clinical Recommendations).
Psychological treatments for substance misuse include therapeutic communities (TC), CBT, and motivational interviewing (MI). A meta-analysis of prison-based TCs suggests that participation increases treatment success, with those TCs followed by aftercare in the community most effective at reducing relapse and re-incarceration.57 A meta-analysis of Moral Reconation Therapy, which focuses on moral reasoning and originally a component of TC, generally supported success in reducing recidivism.58
A variety of CBT-based therapies studied in prison populations with substance misuse demonstrate effectiveness compared to drug and alcohol education or no treatment. However, design limitations prevent clear generalizability, and study outcomes generally focus on rate of re-incarceration as a proxy for relapse.58 Reasoning and Rehabilitation (R&R), a 35-session CBT program focusingon prosocial attitudes, emotion regulation and self-control, and interpersonal problem solving, has demonstrated reductions in recidivism.59
MI is regarded as an evidence-based treatment, particularly for alcohol misuse. One RCT of adolescents incarcerated for driving while intoxicated found lower rates of re-offence with MI compared to relaxation training.60
Apart from psychological treatments, there is good evidence for the treatment of opiateand alcohol misuse with medication assisted therapy (MAT), which combines pharmacological treatments (including methadone, buprenorphine and naltrexone) and psychological approaches. A recent extensive literature search of MAT found 15 methodologically rigorous evaluations from six European countries, containing 3953 participants. There were significant positive outcomes of treatment on reoffending (d=0.47) and drug use (d=0.38).61 Using slightly different criteria, a Cochrane review of MAT for offenders with substance misuse found 11 studies met criteria for inclusion; overall results reflect that MAT reduces drug use in this population.62
Methadone maintenance therapy (MMT) has been implemented in many countries. A recent Cochrane review showed that MMT decreases heroin use and enhances treatment retention compared to non-pharmacologic treatments.63
Starting methadone prior to release is significantly more effective for treatment retention, reduced drug use, and reduced reoffending than either counselling alone or simple referral to MMT upon release.64,65 An RCT conducted at a US prison compared MMT plus counselling, counselling and community referral, and counselling alone for 204 individuals demonstrated increased post release treatment retention and decreased drug abuse with persisting benefits at 6 months and twelve months post-release for those in MMT.66 Another RCT compared MMT versus monitored withdrawal found that higher rates returned to treatment in the community upon release in the MMT sample.67
A number of program evaluations have demonstrated reduction in opiate use following release when individuals were started during incarceration. One RCT conducted in New York City compared MMT to buprenorphine and found equivalence in self-reported relapse, but superiority for buprenorphine treated patients for post-release treatment engagement.68 Another RCT with 211 offenders compared buprenorphine treatment to counselling initiated pre-release demonstrated increased community treatment entry for those randomized to buprenorphine.69 Some RCT evidence supports the use of intramuscular naltrexone as an alternative to methadone.70
In summary, the evidence supports the use of MMT in the offender population, and further research with intramuscular naltrexone and oral buprenorphine is warranted. Additionally, there is a relative paucity of studies treating alcohol misuse in prisoners. Nevertheless, on the basis of evidence we have reviewed, opiate substitution and CBT-based relapse prevention therapies should be made available to all prisoners (see Clinical Recommendations).
Women in Prison
Most prisons across the world are separated by gender, and research has shown that the demographic, health, and criminal characteristics of female prisoners are different to males. In this section, we review some specificareas of prison research. Some trauma-focused interventions for female prisoners have been developed. However, most are small and have reported non-significant findings, which may represent inadequate power. ‘Seeking Safety’, a trauma-focused CBT intervention, has not been demonstrated to have improved outcomes compared with treatment as usual (i.e., 180-240 hours of individual and group treatment).71 Another RCT comparing trauma affect regulation with supportive group therapy was also not associated with differences in recovery between groups.72 Despite disappointing results to date, larger studies are needed to fully evaluate the efficacy of trauma-focused therapies (see Research Recommendations). There is a lack of RCTs for other interventions amongst women prisoners including CBT, mindfulness, and DBT.
In addition, a small number of studies have focused on psychiatric morbidity in prisoners at specialised mother and baby units.73
Older Adults in Prison
The number and proportion of older adults in prison is rising in high income countries. In several prison populations, those over 60 are now the fastest-growing age group, and the number is expected to continue rising as the population ages. Much of the research on older prisoners has described demographic, criminal and health characteristics,74 supplemented with newer research on health, social and custodial needs.75 There have been very few intervention studies despite their increased chronic physical health problems, depression, and functional ability.
Conclusions
Mental disorders are overrepresented in prisoners. The strongest evidence is for serious mental disorders, where surveys have estimated that around one in seven prisoners are diagnosed with psychosis or clinical depression. Substance abuse is also increased many fold in prisoners. For many other disorders, the picture is complicated by self-reported approaches to diagnosis which overestimate rates, and meta-analyses relying on random effects models that weigh small studies similarly to larger higher quality investigations. Further research should move beyond simple prevalence studies and examine the contribution of prison to these excess rates, and the extent, consequences and patterns of novel psychoactive substance use. Individuals in prison with mental health problems are at increased risk of suicide, self-harm, violence and victimisation. There is little specificity in risk factors for these outcomes and few are shared across them, limiting development of effective interventions. Thus, interventions will mostly have to rely on evidence from non-prison settings, although some prison-specific research has suggested that the pharmacological treatment of ADHD, and CBT-based treatments for depression, may improve outcomes. High quality RCT evidence exists on methadone maintenance and opioid substitution treatments, but little on how to treat alcohol misuse. A number of special groups in prison including women and older prisoners appear to have specific mental health needs and may need tailored treatments. Justice departments should collaborate with researchers as addressing the paucity of treatment research will need concerted action by government, funding agencies, and researchers.
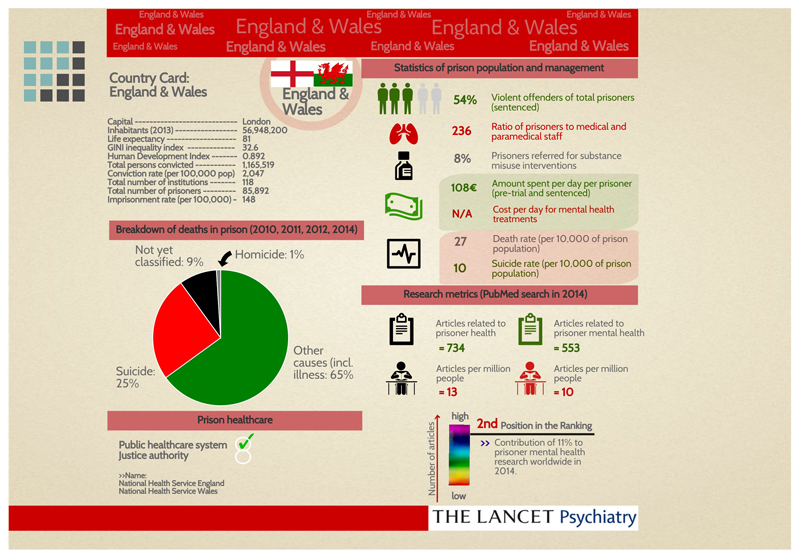
On the basis of this review, we have outlined a number of recommendations relevant to clinical practice and research (Panel 2). In addition, we have included policy recommendations incorporating several outlined by the World Health Organisation.76 Relevant to these recommendations is surveillance of key indicators on a regular basis. We have suggested a format for the presentation of these key indicators for England and Wales (Figure 2) and for 13 other Western European, North American, and Australasian countries (Supplemental eFigures) which would allow comparison between different countries, including the extent of prison-based health research. The choice of these countries was determined by those with populations of over 5 million and GDP’s in the top half ($35,000 per head according to the World Bank 2011-2014).
Figure 2. Country card outlining selected prison metrics for England and Wales in 2014.
Note: References and other country cards for 13 other high-income countries included in online supplement
Supplementary Material
Panel 1. Search strategy and selection criteria.
We searched PubMed and Web of Knowledgefor articles published from1 January 2003 to 31 December 2015. Search terms included (prison* or jail* or offender* or criminal* or inmate* or correction* or penitentiar*) and (RCT* or trial*or randomi* or control*) for intervention studies supplemented with searches based on (mental* or psychiatr* or drug* or alcohol or substance*) for prevalence and interventions, with (suicid* or (self and (harm* or injur* or inflict*)) and (violen* or infraction* or assault* or victim* or bullying or bullie*) for adverse outcomes. Searches also included citations to studies selected for inclusion. We preferentially includedrecent systematic reviews and meta-analyses, unselected prisoner samples for prevalence research, and RCTs with 50 or more participants for the sections on interventions. Unlike a systematic review, reference lists were not manually checked, nor was a meta-analysis considered.
Panel 2.
Clinical Recommendations
-
-
All prisons should have systems in place for the identification of those with serious mental health problems, including case finding on arrival to prison and allocation to appropriate level of service (i.e. primary/secondary/transfer to hospital)
-
-
All prisons should have a suicide prevention strategy that includes accurate screening and monitoring of risk after arrival into prison, multi-disciplinary management of high risk prisoners, and staff training.
-
-
Evidence-based psychological and pharmacological mental health treatments that are available in the community or developed for prison settings should be provided
-
-
There should be monitoring of substance dependent prisoners, and provision of drug and alcohol acute detoxification on arrival to all prisons
-
-
Methadone or alternative (e.g. buprenorphine) maintenance therapy should be available in all prisons with systems in place to link prisoners with appropriate services to continue treatment on release if indicated
-
-
Provision of CBT for relapse prevention of substance misuse
-
-
Prisons should consider provision of trauma-focused and gender-specific interventions to prisoners, particularly if unmet needs are identified
-
-
Minimum standards for meaningful daytime activity (education/courses/training) should be developed that include the amount and range of these activities
Research Recommendations
-
-
More prevalence studies should not be prioritised as there have been more than 100 high quality ones with little variation between and within countries for the severe mental disorders
-
-
Longitudinal studies of mental health in prisoners and the use of novel psychoactive agents are required
-
-
Screening tools for suicide risk and identification of severe mental illness are required that have false positive rates that will not overwhelm prison health services
-
-
Funding bodies should consider prison-specific research calls
-
-
Clarification of the most effective pharmacological treatments for common mental disorders in prison (such as PTSD, anxiety disorders, depression)
-
-
More evidence is required to determine which psychological therapies are most effective for mental health problems in prison, and whether they can be provided in a group-based formats. More research is required for trauma-based treatments in women prisoners
-
-
Research on treatment for alcohol use disorders in prisoners, and also intramuscular naltrexone and oral buprenorphine as opiate substitution therapies
-
-
Evidence-based approaches to diversion of mentally ill offenders from prison, particularly women and young people
-
-
Development of prediction rules/tools that will enable prisons to stratify prisoners into risk groups, particularly for mentally disordered individuals in prison
Policy Recommendations (including WHO recommendations)76
-
-
Adherence to basic principles of human and prison rights
-
-
Equivalence of health care services in prison to those available in the community
-
-
Equity of funding for mental and physical health services (including ensuring that mental health services receive at least the same proportion of funding as they receive in the community)
-
-
Consideration of the social needs of prisoners in addition to health
-
-
Management of prison health by public health systems, particularly in relation to employment of healthcare staff
-
-
National prison services should have a strategy for their management of health and social needs of older prisoners
-
-
National systems need to be instituted that collect annual information on deaths in prison including by suicide, overcrowding rates, prisoner-prisoner and prisoner-staff assault rates, self-harm rates by gender, availability of methadone maintenance therapy, and research activity (see Figure 2 for England and Wales, and country cards for 11other high-income countries in the online Supplementary material and references in the online Appendix)
Acknowledgments
Funding source: SF is funded by a Wellcome Trust Senior Research Fellowship in Clinical Science (095806).
Footnotes
Author contributions: SF and AH completed the literature search. SF drafted the sections on prevalence of psychiatric disorders, suicide risk, and recommendations, MC on violence and victimization, RT on treatment for substance misuse, and AH on interventions for suicide risk and mental health, and special populations. KB compiled infographic cards. All authors contributed to final manuscript.
Conflict of interest: None declared.
Ethics committee approval: Not required.
Publication Statement: The authors confirm that the paper has not been submitted to another journal, and has not been published in whole or in part elsewhere previously.
Contributor Information
Prof Seena Fazel, Department of Psychiatry, University of Oxford, Warneford Hospital, Oxford, United Kingdom, OX3 7JX.
Dr Adrian J Hayes, Department of Psychiatry, University of Oxford, Warneford Hospital, Oxford, United Kingdom, OX3 7JX.
Katrina Bartellas, Department of Psychiatry, University of Oxford, Warneford Hospital, Oxford, OX3 7JX, United Kingdom.
Dr Massimo Clerici, School of Medicine and Surgery, University of Milano-Bicocca, Piazza dell'AteneoNuovo, 1 - 20126 Milan, Italy.
Prof Robert Trestman, Correctional Managed Health Care, University of Connecticut Health Center, 263 Farmington Ave, Farmington, CT 06030, United States.
References
- 1.Fazel S, Danesh J. Serious mental disorder in 23 000 prisoners: a systematic review of 62 surveys. Lancet. 2002;359:545–50. doi: 10.1016/S0140-6736(02)07740-1. [DOI] [PubMed] [Google Scholar]
- 2.Young S, Moss D, Sedgwick O, Fridman M, Hodgkins P. A meta-analysis of the prevalence of attention deficit hyperactivity disorder in incarcerated populations. Psychol Med. 2015;45:247–58. doi: 10.1017/S0033291714000762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Usher AM, Stewart LA, Wilton G. Attention deficit hyperactivity disorder in a Canadian prison population. Int J Law Psychiatry. 2013;36:311–5. doi: 10.1016/j.ijlp.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Gaiffas A, Galera C, Mandon V, Bouvard MP. Attention-defecit/hyperactivity disorder in young French male prisoners. J Forensic Sci. 2014;59:1016–19. doi: 10.1111/1556-4029.12444. [DOI] [PubMed] [Google Scholar]
- 5.Gunn J, Maden A, Swinton M. Treatment needs of prisoners with psychiatric disorders. BMJ. 1991;303:338–41. doi: 10.1136/bmj.303.6798.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Birmingham L, Mason D, Grubin D. Prevalence of mental disorder in remand prisoners: Consecutive case study. BMJ. 1996;313:1521–4. doi: 10.1136/bmj.313.7071.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rivlin A, Hawton K, Marzano L, Fazel S. Psychiatric disorders in male prisoners who made near-lethal suicide attempts: case-control study. Br J Psychiatry. 2010;197:313–9. doi: 10.1192/bjp.bp.110.077883. [DOI] [PubMed] [Google Scholar]
- 8.Robinson L, Spencer MD, Thomson LDG, Stanfield AC, Owens DGC, Hall J, Johnstone EC. Evaluation of a screening instrument for autism spectrum disorders in prisoners. PLoS One. 2012;7:e36078. doi: 10.1371/journal.pone.0036078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Senior J, Birmingham L, Harty MA, Hassan L, Hayes AJ, Kendall K, King C, Lathlean J, Lowthian C, Mills A, Webb R, et al. Identification and management of prisoners with severe psychiatric illness by specialist mental health services. Psychol Med. 2013;43:1511–20. doi: 10.1017/S0033291712002073. [DOI] [PubMed] [Google Scholar]
- 10.Fazel S, Seewald K. Severe mental illness in 33 588 prisoners worldwide: systematic review and meta-regression analysis. Br J Psychiatry. 2012;200:364–73. doi: 10.1192/bjp.bp.111.096370. [DOI] [PubMed] [Google Scholar]
- 11.Butler T, Indig D, Allnutt S, Mamoon H. Co-occurring mental illness and substance use disorder among Australian prisoners. Drug Alcohol Rev. 2011;30:188–94. doi: 10.1111/j.1465-3362.2010.00216.x. [DOI] [PubMed] [Google Scholar]
- 12.Chang Z, Lichtenstein P, Larsson H, Fazel S. Substance use disorders, psychiatric disorders, and mortality after release from prison: a nationwide longitudinal cohort study. Lancet Psychiatry. 2015;2:422–30. doi: 10.1016/S2215-0366(15)00088-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Binswanger IA, Merrill JO, Krueger PM, White MC, Booth RE, Elmore JG. Gender differences in chronic medical, psychiatric, and substance-dependence disorders among jail inmates. Am J Public Health. 2010;100:476–82. doi: 10.2105/AJPH.2008.149591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.HM Chief Inspector of Prisons for England and Wales. Annual Report 2014–15. London: 2015. [Google Scholar]
- 15.Fazel S, Wolf A, Palm C, Lichtenstein P. Violent crime, suicide, and premature mortality in patients with schizophrenia and related disorders: a 38-year total population study in Sweden. Lancet Psychiatry. 2014;1:44–54. doi: 10.1016/S2215-0366(14)70223-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fazel S, Wolf A, Chang Z, Larsson H, Goodwin GM, Lichtenstein P. Depression and violence: a Swedish population study. Lancet Psychiatry. 2015;2:224–32. doi: 10.1016/S2215-0366(14)00128-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hassan L, Birmingham L, Harty MA, Jones P, King C, Lathlean J, Lowthian C, Mills A, Senior J, Thornicroft G, Webb R, et al. Prospective cohort study of mental health during imprisonment. Br J Psychiatry. 2011;198:37–42. doi: 10.1192/bjp.bp.110.080333. [DOI] [PubMed] [Google Scholar]
- 18.Australian Institute of Health and Welfare. The health of Australia’s prisoners. Canberra: Australian Institute of Health and Welfare; 2015. [Google Scholar]
- 19.Fazel S, Grann M, Kling B, Hawton K. Prison suicide in 12 countries: an ecological study of 861 suicides during 2003-2007. Soc Psychiatry Psychiatr Epidemiol. 2011;46:191–5. doi: 10.1007/s00127-010-0184-4. [DOI] [PubMed] [Google Scholar]
- 20.Aebi MF, Delgrande N. Survey 2011. Strasbourg: Council of Europe; 2013. SPACE I - Council of Europe Annual Penal Statistics: Prison populations. [Google Scholar]
- 21.Aebi MF, Delgrande N. Survey 2012. Strasbourg: Council of Europe; 2014. SPACE I - Council of Europe Annual Penal Statistics: Prison populations. [Google Scholar]
- 22.Aebi MF, Delgrande N. Survey 2013. Strasbourg: Council of Europe; 2015. SPACE I - Council of Europe Annual Penal Statistics: Prison populations. [Google Scholar]
- 23.Duthé G, Hazard A, Kensey A, Pan Ké Shon J-L. Suicide among male prisoners in France: A prospective population-based study. Forensic Sci Int. 2013;233:273–7. doi: 10.1016/j.forsciint.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 24.Bureau of Justice Statistics. Mortality in Local Jails and State Prisons, 2000–2013 - Statistical Tables. Washington DC: Bureau of Justice Statistics; 2015. [Google Scholar]
- 25.Hawton K, Linsell L, Adeniji T, Sariaslan A, Fazel S. Self-harm in prisons in England and Wales: an epidemiological study of prevalence, risk factors, clustering, and subsequent suicide. Lancet. 2014;383:1147–54. doi: 10.1016/S0140-6736(13)62118-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rivlin A, Fazel S, Marzano L, Hawton K. Studying survivors of near-lethal suicide attempts as a proxy for completed suicide in prisons. Forensic Sci Int. 2012;220:19–26. doi: 10.1016/j.forsciint.2012.01.022. [DOI] [PubMed] [Google Scholar]
- 27.Barker E, Kolves K, De Leo D. Management of suicidal and self-harming behaviors in prisons: Systematic literature review of evidence-based activities. Arch Suicide Res. 2014;18:227–40. doi: 10.1080/13811118.2013.824830. [DOI] [PubMed] [Google Scholar]
- 28.Humber N, Hayes A, Senior J, Fahy T, Shaw J. Identifying, monitoring and managing prisoners at risk of self-harm/suicide in England and Wales. J Forens Psychiatry Psychol. 2011;22:22–51. [Google Scholar]
- 29.Ministry of Justice. Assaults and Self-harm to March 2015. London: Ministry of Justice; 2015. Safety in Custody Statistics England and Wales: Deaths in prison custody to June 2015. [Google Scholar]
- 30.Humber N, Piper M, Appleby L, Shaw J. Characteristics of and trends in subgroups of prisoner suicides in England and Wales. Psychol Med. 2011;41:2275–85. doi: 10.1017/S0033291711000705. [DOI] [PubMed] [Google Scholar]
- 31.Perry AE, Marandos R, Coulton S, Johnson M. Screening tools assessing risk of suicide and self-harm in adult offenders: A systematic review. Int J Offender Ther Comp Criminol. 2010;54:803–28. doi: 10.1177/0306624X09359757. [DOI] [PubMed] [Google Scholar]
- 32.Konrad N, Daigle MS, Daniel AE, Dear GE, Frottier P, Hayes LM, Kerkhof A, Liebling A, Sarchiapone M. Preventing suicide in prisons, part I - Recommendations from the International Association for Suicide Prevention Task Force on Suicide in Prisons. Crisis. 2007;28:113–21. doi: 10.1027/0227-5910.28.3.113. [DOI] [PubMed] [Google Scholar]
- 33.Blitz CL, Wolff N, Shi J. Physical victimization in prison: The role of mental illness. Int J Law Psychiatry. 2008;31:385–393. doi: 10.1016/j.ijlp.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wolff N, Blitz CL, Shi J. Rates of Sexual Victimization in Prison for Inmates With and Without Mental Disorders. Psychiatr Serv. 2007;58:1087–94. doi: 10.1176/appi.ps.58.8.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Teplin LA, McClelland GM, Abram KM, Weiner DA. Crime victimization in adults with severe mental illness - Comparison with the national crime victimization survey. Arch Gen Psychiat. 2005;62:911–21. doi: 10.1001/archpsyc.62.8.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stephan JJ, Karberg JC. Census of state and federal correctional facilities 2000 (No. NCJ 198272) Washington, DC: Bureau of Justice Statistics, U.S. Department of Justice; 2003. [Google Scholar]
- 37.Duhart DT. Violence in the workplace, 1993–99. Washington D.C: U.S. Department of Justice, Office of Justice Programs; 2001. [Google Scholar]
- 38.Ministry of Justice. Deaths in prison custody to June 2015 Assaults and Self-harm to March 2015. London: Ministry of Justice; 2015. Safety in Custody Statistics England and Wales. [Google Scholar]
- 39.Goncalves LC, Goncalves RA, Martins C, Dirkzwager AJE. Predicting infractions and health care utilization in prison: A Meta-Analysis. Crim Justice Behav. 2014;41:921–42. [Google Scholar]
- 40.Campbell MA, French S, Gendreau P. The prediction of violence in adult offenders: A meta-analytic comparison of instruments and methods of assessment. Crim Justice Behav. 2009;36:567–90. [Google Scholar]
- 41.Schenk AM, Fremouw WJ. Individual characteristics related to prison violence: A critical review of the literature. Aggress Violent Behav. 2012;17:430–42. [Google Scholar]
- 42.Houser KA, Welsh W. Examining the association between co-occurring disorders and seriousness of misconduct by female prison inmates. Crim Justice Behav. 2014;41:650–66. [Google Scholar]
- 43.James JD, Glaze LE. Mental health problems of prison and jail inmates (NCJ 213600) Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2006. [Google Scholar]
- 44.Walters GD, Crawford G. Major mental illness and violence history as predictors of institutional misconduct and recidivism: Main and interaction effects. Law Hum Behav. 2014;38:238–47. doi: 10.1037/lhb0000058. [DOI] [PubMed] [Google Scholar]
- 45.Gilligan J. Violence: Reflections on a national epidemic. New York: Vintage Books; 1997. [Google Scholar]
- 46.Ginsberg Y, Lindefors N. Methylphenidate treatment of adult male prison inmates with attention-deficit hyperactivity disorder: randomised double-blind placebo-controlled trial with open-label extension. Br J Psychiatry. 2012;200:68–73. doi: 10.1192/bjp.bp.111.092940. [DOI] [PubMed] [Google Scholar]
- 47.Konstenius M, Jayaram-Lindstroem N, Guterstam J, Beck O, Philips B, Franck J. Methylphenidate for attention deficit hyperactivity disorder and drug relapse in criminal offenders with substance dependence: a 24-week randomized placebo-controlled trial. Addict. 2014;109:440–9. doi: 10.1111/add.12369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ehret MJ, Shelton D, Barta W, Trestman R, Maruca A, Kamath J, Golay L. Medication Adherence Among Female Inmates With Bipolar Disorder: Results From a Randomized Controlled Trial. Psychol Serv. 2013;10:106–14. doi: 10.1037/a0031433. [DOI] [PubMed] [Google Scholar]
- 49.Bilderbeck AC, Farias M, Brazil IA, Jakobowitz S, Wikholm C. Participation in a 10-week course of yoga improves behavioural control and decreases psychological distress in a prison population. J Psychiatr Res. 2013;47(10):1438–45. doi: 10.1016/j.jpsychires.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 50.Khodayarifard M, Shokoohi-Yekta M, Hamot GE. Effects of individual and group cognitive-behavioral therapy for male prisoners in Iran. Int J Offender Ther Comp Criminol. 2010;54:743–55. doi: 10.1177/0306624X09344840. [DOI] [PubMed] [Google Scholar]
- 51.Shelton D, Sampl S, Kesten KL, Zhang WL, Trestman RL. Treatment of impulsive aggression in correctional settings. Behav Sci Law. 2009;27:787–800. doi: 10.1002/bsl.889. [DOI] [PubMed] [Google Scholar]
- 52.Oser CB, Knudsen HK, Staton-Tindall M, Taxman F, Leukefeld C. Organizational-level correlates of the provision of detoxification services and medication-based treatments for substance abuse in correctional institutions. Drug Alcohol Depend. 2009;103:S73–S81. doi: 10.1016/j.drugalcdep.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States - Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 54.Amato L, Minozzi S, Vecchi S, Davoli M. Benzodiazepines for alcohol withdrawal. Cochrane Database Syst Rev. 2010;3:CD005063. doi: 10.1002/14651858.CD005063.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Amato L, Davoli M, Minozzi S, Ferroni E, Ali R, Ferri M. Methadone at tapered doses for the management of opioid withdrawal. Cochrane Database Syst Rev. 2013;2:CD003409. doi: 10.1002/14651858.CD003409.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sheard L, Wright NMJ, El-Sayeh HG, Adams CE, Li R, Tompkins CNE. The Leeds Evaluation of Efficacy of Detoxification Study (LEEDS) prisons project: a randomised controlled trial comparing dihydrocodeine and buprenorphine for opiate detoxification. Subst Abuse Treat Prev Policy. 2009;4:1. doi: 10.1186/1747-597X-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mitchell O, Wilson DB, MacKenzie DL. Does incarceration-based drug treatment reduce recidivism? A meta-analytic synthesis of the research. J Exp Criminol. 2007;3:353–75. [Google Scholar]
- 58.Ferguson LM, Wormith JS. A meta-analysis of moral reconation therapy. Int J Offender Ther Comp Criminol. 2013;57:1076–106. doi: 10.1177/0306624X12447771. [DOI] [PubMed] [Google Scholar]
- 59.Tong LSJ, Farrington DP. How effective is the "Reasoning and Rehabilitation" programme in reducing reoffending? A meta-analysis of evaluations in four countries. Psychol Crime Law. 2006;12:3–24. [Google Scholar]
- 60.Stein LAR, Colby SM, Barnett NP, Monti PM, Golembeske C, Lebeau-Craven R. Effects of motivational interviewing for incarcerated adolescents on driving under the influence after release. Am J Addict. 2006;15:50–7. doi: 10.1080/10550490601003680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Koehler JA, Humphreys DK, Akoensi TD, de Ribera OS, Loesel F. A systematic review and meta-analysis on the effects of European drug treatment programmes on reoffending. Psychol Crime Law. 2014;20:584–602. [Google Scholar]
- 62.Perry AE, Neilson M, Martyn-St James M, Glanville JM, McCool R, Duffy S, Godfrey C, Hewitt C. Pharmacological interventions for drug-using offenders. Cochrane Database Syst Rev. 2013;12:CD010862. doi: 10.1002/14651858.CD010862. [DOI] [PubMed] [Google Scholar]
- 63.Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev. 2009;3:CD002209. doi: 10.1002/14651858.CD002209.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gordon MS, Kinlock TW, Schwartz RP, O'Grady KE. A randomized clinical trial of methadone maintenance for prisoners: findings at 6 months post-release. Addict. 2008;103:1333–42. doi: 10.1111/j.1360-0443.2008.002238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.McKenzie M, Zaller N, Dickman SL, Green TC, Parihk A, Friedmann PD, Rich JD. A randomized trial of methadone initiation prior to release from incarceration. Subst Abuse. 2012;33:19–29. doi: 10.1080/08897077.2011.609446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kinlock TW, Gordon MS, Schwartz RP, Fitzgerald TT, O'Grady KE. A randomized clinical trial of methadone maintenance for prisoners: Results at 12 months postrelease. J Subst Abuse Treat. 2009;37:277–85. doi: 10.1016/j.jsat.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rich JD, McKenzie M, Larney S, Wong JB, Tran L, Clarke J, Noska A, Reddy M, Zaller N. Methadone continuation versus forced withdrawal on incarceration in a combined US prison and jail: a randomised, open-label trial. Lancet. 2015;386:350–9. doi: 10.1016/S0140-6736(14)62338-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Magura S, Lee JD, Hershberger J, Joseph H, Marsch L, Shropshire C, Rosenblum A. Buprenorphine and methadone maintenance in jail and post-release: A randomized clinical trial. Drug Alcohol Depend. 2009;99:222–30. doi: 10.1016/j.drugalcdep.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gordon MS, Kinlock TW, Schwartz RP, Fitzgerald TT, O'Grady KE, Vocci FJ. A randomized controlled trial of prison-initiated buprenorphine: Prison outcomes and community treatment entry. Drug Alcohol Depend. 2014;142:33–40. doi: 10.1016/j.drugalcdep.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lobmaier PP, Kunoe N, Gossop M, Katevoll T, Waal H. Naltrexone implants compared to methadone: Outcomes six months after prison release. Eur Addict Res. 2010;16:139–45. doi: 10.1159/000313336. [DOI] [PubMed] [Google Scholar]
- 71.Zlotnick C, Johnson J, Najavits LM. Randomized controlled pilot study of Cognitive-Behavioral Therapy in a sample of incarcerated women with substance use disorder and PTSD. Behav Ther. 2009;40:325–36. doi: 10.1016/j.beth.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ford JD, Chang R, Levine J, Zhang W. Randomized clinical trial comparing affect regulation and supportive group therapies for victimization-related PTSD with incarcerated women. Behav Ther. 2013;44:262–76. doi: 10.1016/j.beth.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 73.Mukherjee S, Pierre-Victor D, Bahelah R, Madhivanan P. Mental health issues among pregnant women in correctional facilities: A systematic review. Women Health. 2014;54:816–42. doi: 10.1080/03630242.2014.932894. [DOI] [PubMed] [Google Scholar]
- 74.Fazel S, Hope T, O'Donnell I, Piper M, Jacoby R. Health of elderly male prisoners: worse than the general population, worse than younger prisoners. Age Ageing. 2001;30:403–7. doi: 10.1093/ageing/30.5.403. [DOI] [PubMed] [Google Scholar]
- 75.Hayes AJ, Burns A, Turnbull P, Shaw JJ. The health and social needs of older male prisoners. Int J Geriatr Psychiatry. 2012;27:1155–62. doi: 10.1002/gps.3761. [DOI] [PubMed] [Google Scholar]
- 76.Enggist SM, Lars, Galea Gauden, Udesen Caroline. Prisons and Health. Copenhagen: World Health Organisation; 2014. [Google Scholar]
- 77.Fazel S, Bains P, Doll H. Substance abuse and dependence in prisoners: a systematic review. Addict. 2006;101:181–91. doi: 10.1111/j.1360-0443.2006.01316.x. [DOI] [PubMed] [Google Scholar]
- 78.Fazel S, Cartwright J, Norman-Nott A, Hawton K. Suicide in prisoners: A systematic review of risk factors. J Clin Psychiatry. 2008;69:1721–31. [PubMed] [Google Scholar]
- 79.Rivlin A, Hawton K, Marzano L, Fazel S. Psychosocial characteristics and social networks of suicidal prisoners: Towards a model of suicidal behaviour in detention. PLoS One. 2013;8:e68944. doi: 10.1371/journal.pone.0068944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Humber N, Webb R, Piper M, Appleby L, Shaw J. A national case-control study of risk factors among prisoners in England and Wales. Soc Psychiatry Psychiatr Epidemiol. 2013;48:1177–85. doi: 10.1007/s00127-012-0632-4. [DOI] [PubMed] [Google Scholar]
- 81.Wolff N, Shi J. Victimisation and feelings of safety among male and female inmates with behavioural health problems. J Forens Psychiatry Psychol. 2009;20:S56–S77. [Google Scholar]
- 82.Huebner BM. Administrative determinants of inmate violence: A multilevel analysis. J Crim Justice. 2003;31:107–17. [Google Scholar]
- 83.Wolff N, Shi J, Siegel J. Understanding physical victimization inside prisons: Factors that Predict Risk. Justice Q. 2009;26:445–75. [Google Scholar]
- 84.Perez DM, Gover AR, Tennyson KM, Santos SD. Individual and Institutional Characteristics Related to Inmate Victimization. International Journal of Offender Therapy and Comparative Criminology. 2010;54(3):378–94. doi: 10.1177/0306624X09335244. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.